Modification of Pronated Foot Posture after a Program of Therapeutic Exercises
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments and Procedure
- (1)
- Walking on their heel and forefoot. In upright position, subjects must walk (a) with the sole support of their heel and (b) with the support of metatarsal heads and phalanges. Feet must be aligned with the legs.
- (2)
- Walking on medial and lateral border of the foot. Subjects must walk with the sole support of (a) medial longitudinal arch and (b) lateral longitudinal arch.
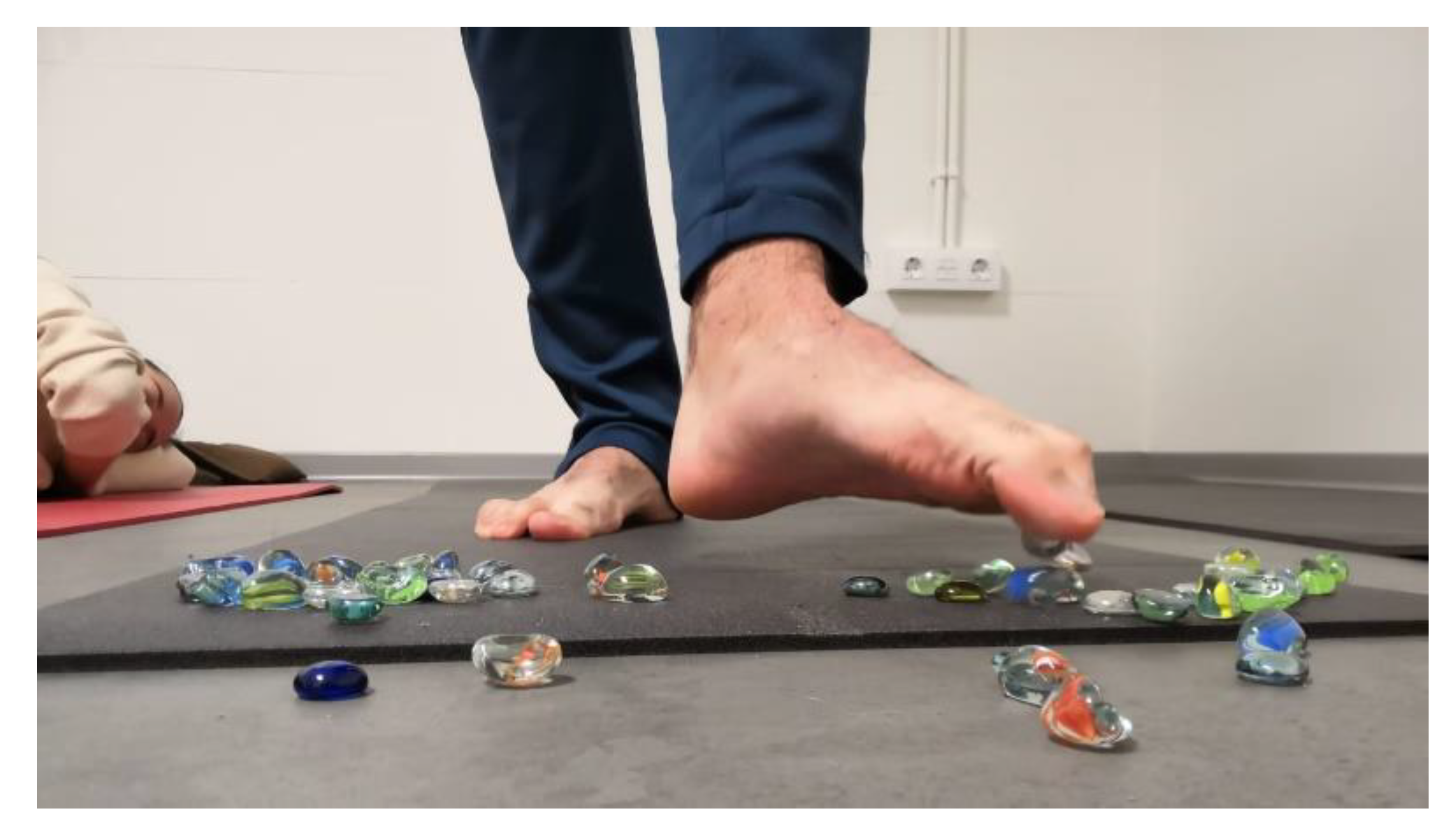
- (3)
- Picking up small objects with the toes. In standing position subjects must pick up little stones with the toes, and release them in other places (Figure 1).
- (4)
- Resistive inversion and eversion with an elastic band. While seated with a straight leg, subjects must move the foot in eversion and inversion with the resistance of an elastic band (Figure 2).
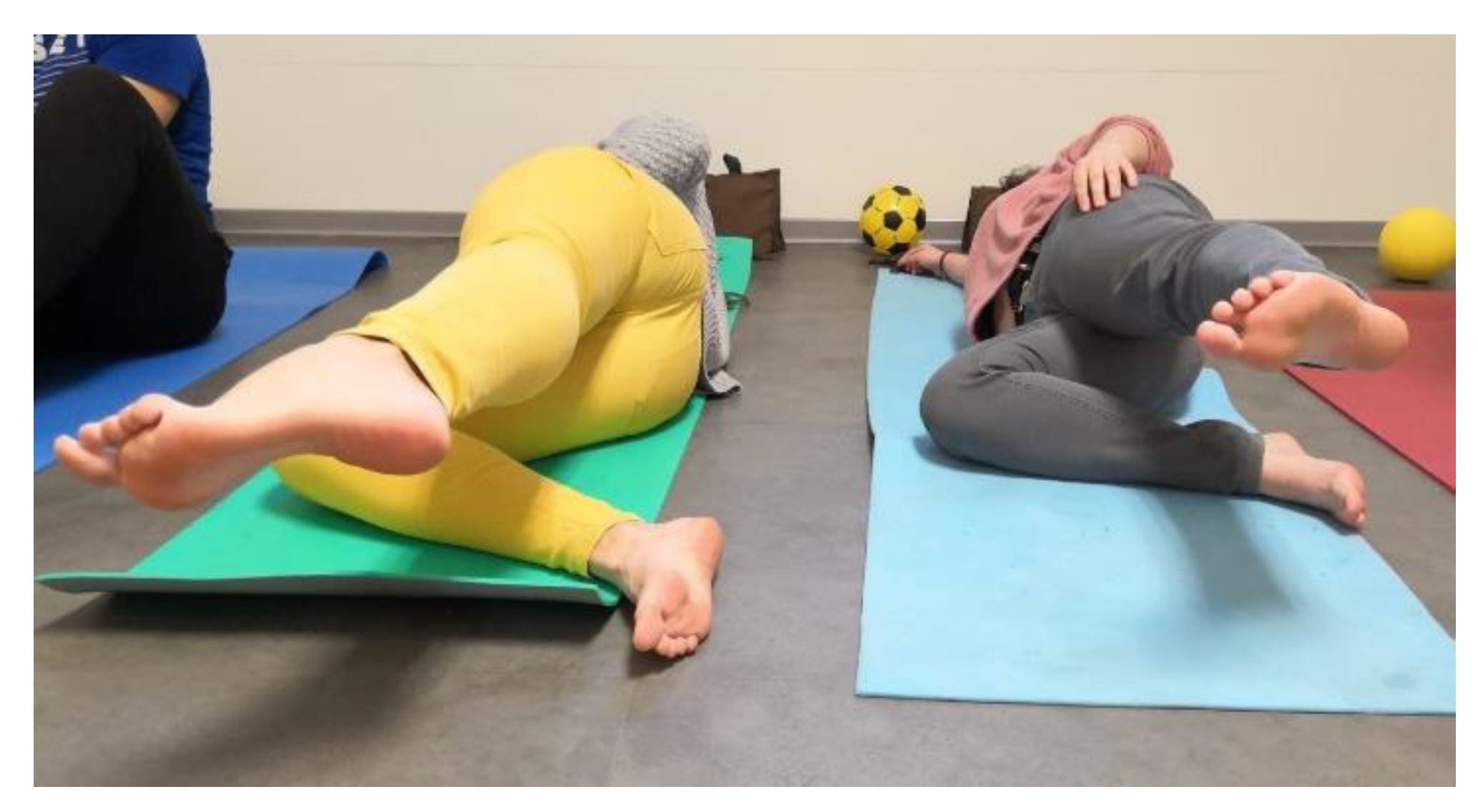
- (5)
- Hip abduction. In the lateral position, the leg in contact with the ground is bent. The contralateral leg will be aligned with the trunk. Subjects must contract 8 s moving away the leg from the other, and 8 s of muscle relaxation when lowering it again (Figure 3).
- (6)
- Strength of the erector spinae. With the subject in the prone position, extended upper limbs in prolongation of the body. Subjects must perform a slight elevation of the trunk. A total of 8 s of contraction and 8 s of muscle relaxation.
- (7)
- Strength of the abdomen. With the subject in the supine position, and knees flexed, slightly separated and aligned with the feet, hip elevation. On the abdomen there will be a weights 2 kg, and a ball, which they have to stabilize with the pelvis.
- (8)
- Strength of the obliques of the abdomen. With the subject in the supine position and knees flexed, slightly separated and aligned with the feet, flexed trunk the right arm must touch the left knee, left arm and right knee, respectively. A total of 8 s of contraction and 8 s of muscle relaxation.
- (9)
- Ball in the legs. With the subject in the supine position, with flexed knees and a ball between the legs contracting the adductors (8 s of contraction and 8 s of muscle relaxation).
- (10)
- Balance on an unstable base. In the standing position subjects must move in eversion and inversion, supporting in the toes and also the heel.
- (11)
- Balance on an unstable base and destabilization. In the standing position a couple of subjects must maintain balance bouncing a ball between them.
2.3. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fiolkowski, P.; Brunt, D.; Bishop, M.; Woo, R.; Horodyski, M. Intrinsic pedal musculature support of the medial longitudinal arch: An electromyography study. J. Foot Ankle Surg. 2003, 42, 327–333. [Google Scholar] [CrossRef]
- Jung, D.-Y.; Kim, M.-H.; Koh, E.-K.; Kwon, O.-Y.; Cynn, H.-S.; Lee, W.-H. A comparison in the muscle activity of the abductor hallucis and the medial longitudinal arch angle during toe curl and short foot exercises. Phys. Ther. Sport 2011, 12, 30–35. [Google Scholar] [CrossRef]
- Koura, G.M.; Elimy, D.A.; Hamada, H.A.; Fawaz, H.E.; Elgendy, M.H.; Saab, I.M. Impact of foot pronation on postural stability: An observational study. J. Back Musculoskelet. Rehabil. 2017, 30, 1327–1332. [Google Scholar] [CrossRef]
- Chung, K.A.; Lee, E.; Lee, S. The effect of intrinsic foot muscle training on medial longitudinal arch and ankle stability in patients with chronic ankle sprain accompanied by foot pronation. Phys. Ther. Rehabil. Sci. 2016, 5, 78–83. [Google Scholar] [CrossRef]
- Sánchez-Rodríguez, R.; Martínez-Nova, A.; Escamilla-Martínez, E.; Pedrera-Zamorano, J.D. Can the Foot Posture Index or their individual criteria predict dynamic plantar pressures? Gait Posture 2012, 36, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Nova, A.; Sánchez-Rodríguez, R.; Pérez-Soriano, P.; Llana-Belloch, S.; Leal-Muro, A.; Pedrera-Zamorano, J.D. Plantar pressures determinants in mild Hallux Valgus. Gait Posture 2010, 32, 425–427. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, W.; Takahashi, M.; Iwamoto, Y.; Shinakoda, K. Coordination among Shank, Rearfoot, Midfoot, and Forefoot Kinematic Movement During Gait in Individuals With Hallux Valgus. J. Appl. Biomech. 2019, 35, 44–51. [Google Scholar] [CrossRef]
- Lee, J.-H.; Yoon, J.; Cynn, H.-S. Foot exercise and taping in patients with patellofemoral pain and pronated foot. J. Bodyw. Mov. Ther. 2017, 21, 216–222. [Google Scholar] [CrossRef]
- Yazdani, F.; Razeghi, M.; Karimi, M.T.; Bani, M.S.; Bahreinizad, H. Foot hyperpronation alters lumbopelvic muscle function during the stance phase of gait. Gait Posture 2019, 74, 102–107. [Google Scholar] [CrossRef]
- Maharaj, J.N.; Cresswell, A.G.; Lichtwark, G.A. Subtalar Joint Pronation and Energy Absorption Requirements during Walking Are Related to Tibialis Posterior Tendinous Tissue Strain. Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef]
- Telfer, S.; Abbott, M.; Steultjens, M.; Rafferty, D.; Woodburn, J. Dose–response effects of customised foot orthoses on lower limb muscle activity and plantar pressures in pronated foot type. Gait Posture 2013, 38, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Taşpınar, Ö.; Kabayel, D.D.; Ozdemir, F.; Tuna, H.; Keskin, Y.; Mercimek, O.B.; Süt, N.; Yavuz, S.; Tuna, F. Comparing the efficacy of exercise, internal and external shoe modification in pes planus: A clinical and pedobarographic study. J. Back Musculoskelet. Rehabil. 2017, 30, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Ford, S.E.; Scannell, B.P. Pediatric Flatfoot. Foot Ankle Clin. 2017, 22, 643–656. [Google Scholar] [CrossRef] [PubMed]
- Mulligan, E.P.; Cook, P.G. Effect of plantar intrinsic muscle training on medial longitudinal arch morphology and dynamic function. Man. Ther. 2013, 18, 425–430. [Google Scholar] [CrossRef]
- Sulowska, I.; Oleksy, Ł.; Mika, A.; Bylina, D.; Sołtan, J. The Influence of Plantar Short Foot Muscle Exercises on Foot Posture and Fundamental Movement Patterns in Long-Distance Runners, a Non-Randomized, Non-Blinded Clinical Trial. PLoS ONE 2016, 11, e0157917. [Google Scholar] [CrossRef]
- Pabón-Carrasco, M.; Castro-Méndez, A.; Vilar, S.; Jiménez-Cebrián, A.M.; García-Paya, I.; Palomo-Toucedo, I. Randomized Clinical Trial: The Effect of Exercise of the Intrinsic Muscle on Foot Pronation. Int. J. Environ. Res. Public Health 2020, 17, 4882. [Google Scholar] [CrossRef]
- Yoon, S.-D.; Sung, D.-H.; Park, G.D. The effect of active core exercise on fitness and foot pressure in Taekwondo club students. J. Phys. Ther. Sci. 2015, 27, 509–511. [Google Scholar] [CrossRef]
- McKeon, P.O.; Hertel, J.; Bramble, D.; Davis, I. The foot core system: A new paradigm for understanding intrinsic foot muscle function. Br. J. Sports Med. 2014, 49, 290. [Google Scholar] [CrossRef]
- Gijon-Nogueron, G.; Alguacil, J.M.; Alfageme-García, P.; Cervera-Marin, J.A.; Asencio, J.M.; Martínez-Nova, A. Establishing normative foot posture index values for the paediatric population: A cross-sectional study. J. Foot Ankle Res. 2016, 9, 24. [Google Scholar] [CrossRef]
- Redmond, A.; Crosbie, J.; Ouvrier, R.A. Development and validation of a novel rating system for scoring standing foot posture: The Foot Posture Index. Clin. Biomech. 2006, 21, 89–98. [Google Scholar] [CrossRef]
- Menz, H.B. Two feet, or one person? Problems associated with statistical analysis of paired data in foot and ankle medicine. Foot 2004, 14, 2–5. [Google Scholar] [CrossRef]
- De Blaiser, C.; De Ridder, R.; Willems, T.; Bossche, L.V.; Danneels, L.; Roosen, P. Impaired Core Stability as a Risk Factor for the Development of Lower Extremity Overuse Injuries: A Prospective Cohort Study. Am. J. Sports Med. 2019, 47, 1713–1721. [Google Scholar] [CrossRef] [PubMed]
- Mucha, M.D.; Caldwell, W.; Schlueter, E.L.; Walters, C.; Hassen, A. Hip abductor strength and lower extremity running related injury in distance runners: A systematic review. J. Sci. Med. Sport 2017, 20, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Emami, F.; Yoosefinejad, A.K.; Razeghi, M. Correlations between core muscle geometry, pain intensity, functional disability and postural balance in patients with nonspecific mechanical low back pain. Med. Eng. Phys. 2018, 60, 39–46. [Google Scholar] [CrossRef]
- Grieve, R.; Goodwin, F.; AlFaki, M.; Bourton, A.-J.; Jeffries, C.; Scott, H. The immediate effect of bilateral self myofascial release on the plantar surface of the feet on hamstring and lumbar spine flexibility: A pilot randomised controlled trial. J. Bodyw. Mov. Ther. 2015, 19, 544–552. [Google Scholar] [CrossRef]
- Gijon-Nogueron, G.; Sanchez-Rodriguez, R.; Lopezosa-Reca, E.; Cervera-Marin, J.A.; Martinez-Quintana, R.; Martinez-Nova, A. Normal values of the foot posture index in a young adult Spanish population a cross-sectional study. J. Am. Podiatr. Med. Assoc. 2015, 105, 42–46. [Google Scholar] [CrossRef]

| Gender | n | Mean | SD | p | |
|---|---|---|---|---|---|
| Weight | Men | 15 | 77.6 | 7.5 | <0.001 |
| Women | 21 | 58.7 | 9.8 | ||
| Height | Men | 15 | 175.1 | 6.3 | <0.001 |
| Women | 21 | 161.1 | 6.4 | ||
| BMI | Men | 15 | 25.3 | 1.9 | 0.002 |
| Women | 21 | 22.3 | 2.9 | ||
| Years | Men | 15 | 24.3 | 6.3 | 0.099 |
| Women | 21 | 21.3 | 1.6 |
| Men | Women | p | ||
|---|---|---|---|---|
| FPI Experimental | PRE | 8.3 ± 1.7 | 8 ±1.8 | 0.887 |
| POST | 7 ± 2.3 | 6.1 ± 2.1 | 0.457 | |
| FPI | PRE | 7.7 ± 1.4 | 8.2 ± 1.1 | 0.430 |
| Control | POST | 7.7 ± 1.4 | 8.2 ± 1.1 | 0.430 |
| Neutral | Pronated | Highly Pronated | TOTAL | |
|---|---|---|---|---|
| FPI Pre | 0 | 15 | 3 | 18 |
| FPI Post | 6 | 11 | 1 | 18 |
| p | 0.001 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-Rodríguez, R.; Valle-Estévez, S.; Fraile-García, P.A.; Martínez-Nova, A.; Gómez-Martín, B.; Escamilla-Martínez, E. Modification of Pronated Foot Posture after a Program of Therapeutic Exercises. Int. J. Environ. Res. Public Health 2020, 17, 8406. https://doi.org/10.3390/ijerph17228406
Sánchez-Rodríguez R, Valle-Estévez S, Fraile-García PA, Martínez-Nova A, Gómez-Martín B, Escamilla-Martínez E. Modification of Pronated Foot Posture after a Program of Therapeutic Exercises. International Journal of Environmental Research and Public Health. 2020; 17(22):8406. https://doi.org/10.3390/ijerph17228406
Chicago/Turabian StyleSánchez-Rodríguez, Raquel, Sandra Valle-Estévez, Peñas Albas Fraile-García, Alfonso Martínez-Nova, Beatriz Gómez-Martín, and Elena Escamilla-Martínez. 2020. "Modification of Pronated Foot Posture after a Program of Therapeutic Exercises" International Journal of Environmental Research and Public Health 17, no. 22: 8406. https://doi.org/10.3390/ijerph17228406
APA StyleSánchez-Rodríguez, R., Valle-Estévez, S., Fraile-García, P. A., Martínez-Nova, A., Gómez-Martín, B., & Escamilla-Martínez, E. (2020). Modification of Pronated Foot Posture after a Program of Therapeutic Exercises. International Journal of Environmental Research and Public Health, 17(22), 8406. https://doi.org/10.3390/ijerph17228406






