Boosting Psychological Well-Being through a Social Mindfulness-Based Intervention in the General Population
Abstract
1. Introduction
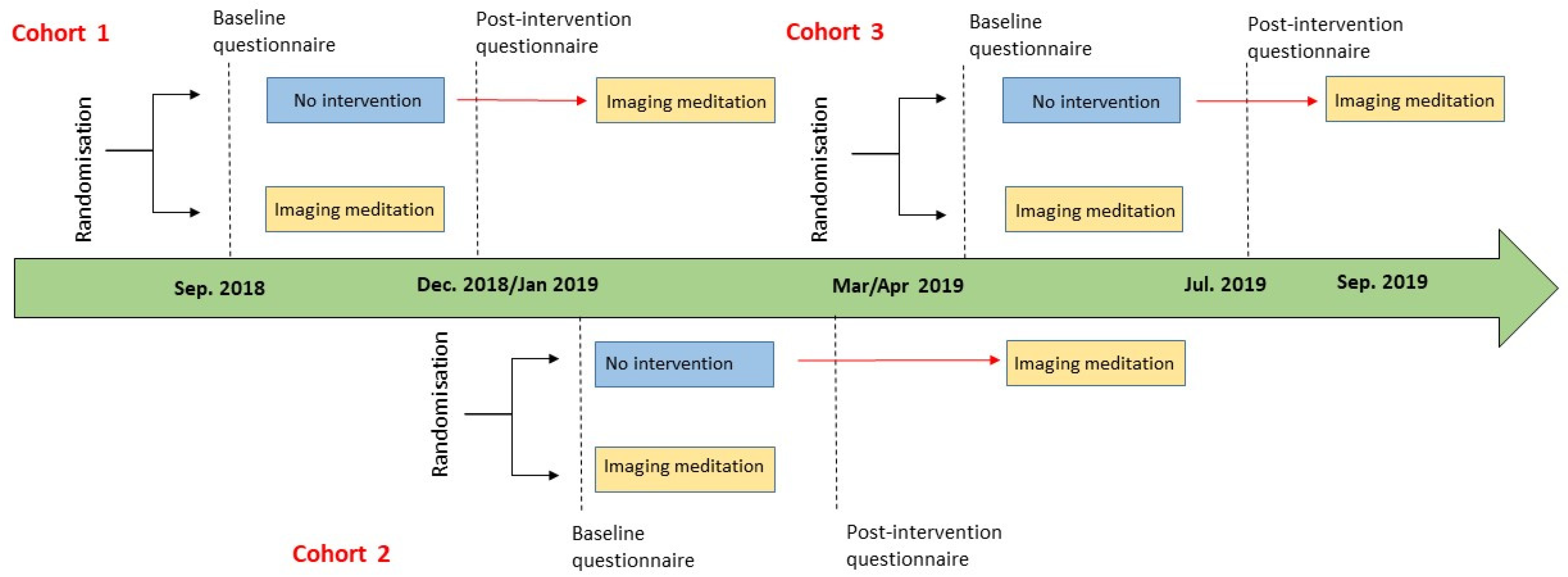
2. Materials and Methods
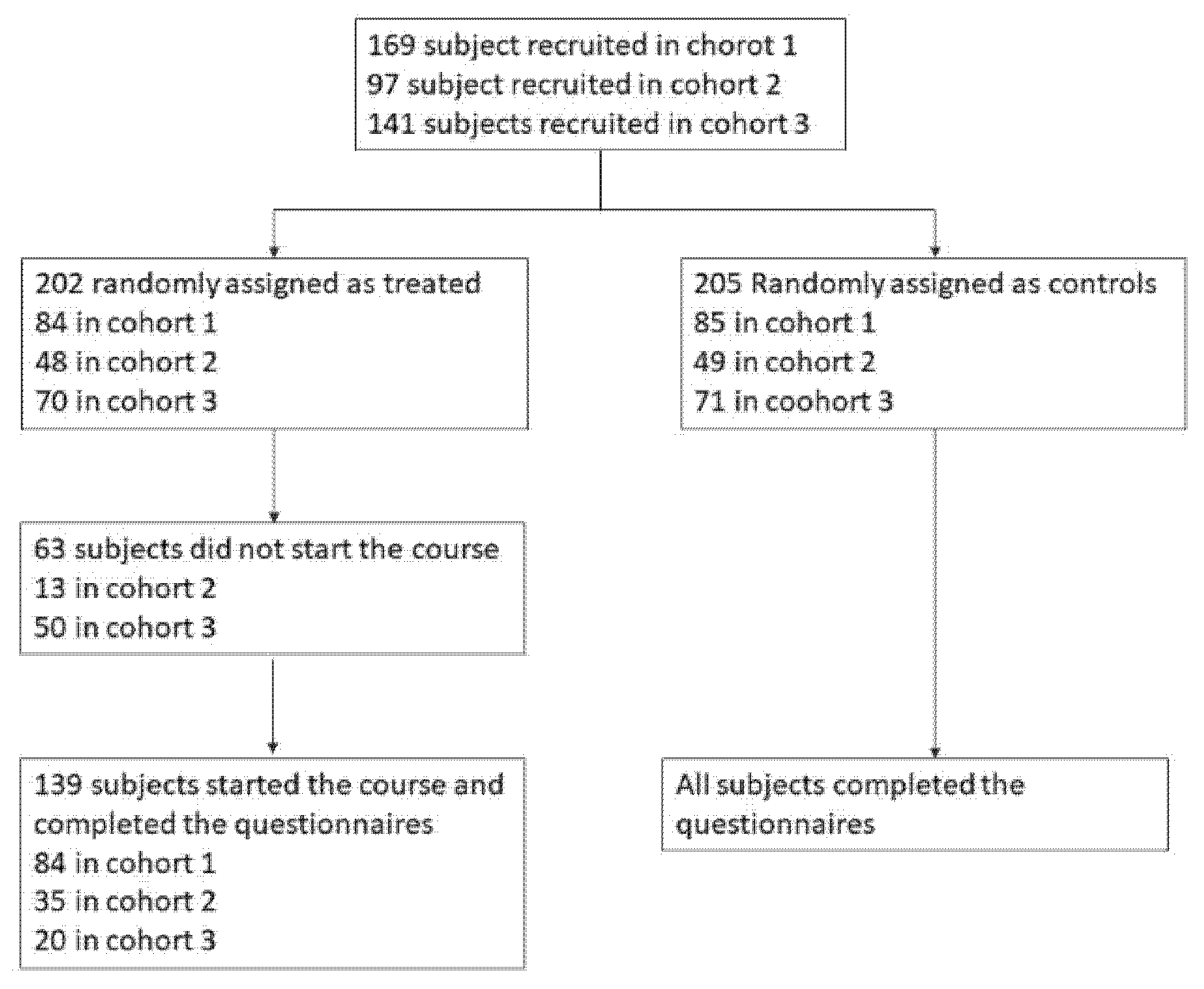
2.1. Participants
2.2. Recruitment Process
2.3. Intervention
2.4. Measures
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chiesa, A.; Fazia, T.; Bernardinelli, L.; Morandi, G. Citation patterns and trends of systematic reviews about mindfulness. Complement. Ther. Clin. Pract. 2017, 28, 26–37. [Google Scholar] [CrossRef]
- Tang, Y.Y.; Leve, L.D. A translational neuroscience perspective on mindfulness meditation as a prevention strategy. Transl. Behav. Med. 2016, 6, 63–72. [Google Scholar] [CrossRef]
- Galante, J.; Dufour, G.; Vainre, M.; Wagner, A.P.; Stochl, J.; Benton, A.; Lathia, N.; Howarth, E.; Jones, P.B. A mindfulness-based intervention to increase resilience to stress in university students (the Mindful Student Study): A pragmatic randomised controlled trial. Lancet Public Health 2018, 3, e72–e81. [Google Scholar] [CrossRef]
- Creswell, J.D. Mindfulness Interventions. Annu. Rev. Psychol. 2017, 68, 491–516. [Google Scholar] [CrossRef]
- Arias, A.J.; Steinberg, K.; Banga, A.; Trestman, R.L. Systematic review of the efficacy of meditation techniques as treatments for medical illness. J. Altern. Complement. Med. 2006, 12, 817–832. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, S. Health Benefits of Meditation: What the Newest Research Shows. Altern. Complement. Ther. 2010, 16, 223–228. [Google Scholar] [CrossRef]
- Keng, S.L.; Smoski, M.J.; Robins, C.J. Effects of mindfulness on psychological health: A review of empirical studies. Clin. Psychol. Rev. 2011, 31, 1041–1056. [Google Scholar] [CrossRef]
- Gotink, R.A.; Meijboom, R.; Vernooij, M.W.; Smits, M.; Hunink, M.G.M. 8-week Mindfulness Based Stress Reduction induces brain changes similar to traditional long-term meditation practice—A systematic review. Brain Cogn. 2016, 108, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Garland, E.L.; Hanley, A.; Farb, N.A.; Froeliger, B.E. State Mindfulness during Meditation Predicts Enhanced Cognitive Reappraisal. Mindfulness 2015, 6, 234–242. [Google Scholar] [CrossRef]
- Jain, S.; Shapiro, S.L.; Swanick, S.; Roesch, S.C.; Mills, P.J.; Bell, I.; Schwartz, G.E.R. A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Ann. Behav. Med. 2007, 33, 11–21. [Google Scholar] [CrossRef]
- Basso, J.C.; McHale, A.; Ende, V.; Oberlin, D.J.; Suzuki, W.A. Brief, daily meditation enhances attention, memory, mood, and emotional regulation in non-experienced meditators. Behav. Brain Res. 2019, 356, 208–220. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Singh, S.; Sibinga, E.M.S.; Gould, N.F.; Rowland-Seymour, A.; Sharma, R.; Berger, Z.; Sleicher, D.; Maron, D.D.; Shihab, H.M.; et al. Meditation Programs for Psychological Stress and Well-being. JAMA Intern. Med. 2014, 174, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Greeson, J.M. Mindfulness Research Update: 2008. Complement. Health Pract. Rev. 2009, 14, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Hölzel, B.K.; Lazar, S.W.; Gard, T.; Schuman-Olivier, Z.; Vago, D.R.; Ott, U. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action from a Conceptual and Neural Perspective. Perspect. Psychol. Sci. 2011, 6, 537–559. [Google Scholar] [CrossRef] [PubMed]
- Burzler, M.A.; Voracek, M.; Hos, M.; Tran, U.S. Mechanisms of Mindfulness in the General Population. Mindfulness 2019, 10, 469–480. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness; Delacorte Press: New York, NY, USA, 1990; ISBN 0385303122. [Google Scholar]
- Kabat-Zinn, J. Mindfulness-Based Interventions in Context: Past, Present, and Future. Clin. Psychol. Sci. Pract. 2006, 10, 144–156. [Google Scholar] [CrossRef]
- Segal, Z.V.; Williams, M.G.; Teasdale, J.D. Mindfulness Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse; Guilford Press: New York, NY, USA, 2002. [Google Scholar]
- Beck, A.T.; Rush, A.J.; Shaw, B.F.; Emery, G. Cognitive Therapy of Depression; Guilford Press: New York, NY, USA, 1979; ISBN 0898629195. [Google Scholar]
- Sharma, M.; Rush, S.E. Mindfulness-Based Stress Reduction as a Stress Management Intervention for Healthy Individuals. J. Evid. Based Complement. Altern. Med. 2014, 19, 271–286. [Google Scholar] [CrossRef]
- Carmody, J.; Baer, R.A.; Lykins, E.L.B.; Olendzki, N. An empirical study of the mechanisms of mindfulness in a mindfulness-based stress reduction program. J. Clin. Psychol. 2009, 65, 613–626. [Google Scholar] [CrossRef]
- Bowen, S.; Chawla, N.; Witkiewitz, K. Mindfulness-based relapse prevention for addictive behaviors. In Mindfulness-Based Treatment Approaches: Clinician’s Guide to Evidence Base and Applications, 2nd ed.; Academic Press: Cambridge, MA, USA, 2014; pp. 141–157. [Google Scholar]
- Jha, A.P.; Krompinger, J.; Baime, M.J. Mindfulness training modifies subsystems of attention. Cogn. Affect. Behav. Neurosci. 2007, 7, 109–119. [Google Scholar] [CrossRef]
- Vieten, C.; Astin, J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: Results of a pilot study. Arch. Womens Ment. Health 2008, 11, 67–74. [Google Scholar] [CrossRef]
- Griffith, G.M.; Bartley, T.; Crane, R.S. The Inside Out Group Model: Teaching Groups in Mindfulness-Based Programs. Mindfulness 2019, 10, 1315–1327. [Google Scholar] [CrossRef]
- Crane, R.S.; Brewer, J.; Feldman, C.; Kabat-Zinn, J.; Santorelli, S.; Williams, J.M.G.; Kuyken, W. What defines mindfulness-based programs? The warp and the weft. Psychol. Med. 2017, 47, 990–999. [Google Scholar] [CrossRef] [PubMed]
- Fazia, T.; Bubbico, F.; Iliakis, I.; Salvato, G.; Berzuini, G.; Bruno, S.; Bernardinelli, L. Short-Term Meditation Training Fosters Mindfulness and Emotion Regulation: A Pilot Study. Front. Psychol. 2020, 11, 2828. [Google Scholar] [CrossRef]
- Evans, C.; Mellor-Clark, J.; Margison, F.; Barkham, M.; Audin, K.; Connell, J.; McGrath, G. CORE: Clinical Outcomes in Routine Evaluation. J. Ment. Health 2000, 9, 247–255. [Google Scholar] [CrossRef]
- Palmieri, G.; Evans, C.; Hansen, V.; Brancaleoni, G.; Ferrari, S.; Porcelli, P.; Reitano, F.; Rigatelli, M. Validation of the Italian version of the clinical outcomes in routine evaluation outcome measure (CORE-OM). Clin. Psychol. Psychother. 2009, 16, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Baer, R.A.; Smith, G.T.; Hopkins, J.; Krietemeyer, J.; Toney, L. Using Self-Report Assessment Methods to Explore Facets of Mindfulness. Assessment 2006, 13, 27–45. [Google Scholar] [CrossRef] [PubMed]
- Giovannini, C.; Giromini, L.; Bonalume, L.; Tagini, A.; Lang, M.; Amadei, G. The Italian Five Facet Mindfulness Questionnaire: A Contribution to its Validity and Reliability. J. Psychopathol. Behav. Assess. 2014, 36, 415–423. [Google Scholar] [CrossRef]
- Diener, E.; Emmons, R.A.; Larsem, R.J.; Griffin, S. The Satisfaction with Life Scale. J. Personal. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Di Fabio, A.; Gori, A. Measuring Adolescent Life Satisfaction. J. Psychoeduc. Assess. 2016, 34, 501–506. [Google Scholar] [CrossRef]
- Crawford, J.R.; Henry, J.D. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2004, 43, 245–265. [Google Scholar] [CrossRef]
- Terracciano, A.; McCrae, R.R.; Costa, P.T., Jr. Factorial and construct validity of the Italian Positive and Negative Affect Schedule (PANAS). Eur. J. Psychol. Assess. 2003, 19, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Mondo, M.; Sechi, C.; Cabras, C. Psychometric evaluation of three versions of the Italian Perceived Stress Scale. Curr. Psychol. 2019. [Google Scholar] [CrossRef]
- Neff, K.D. The Development and Validation of a Scale to Measure Self-Compassion. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Veneziani, C.A.; Fuochi, G.; Voci, A. Self-compassion as a healthy attitude toward the self: Factorial and construct validity in an Italian sample. Personal. Individ. Differ. 2017, 119, 60–68. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Dinburgh mental well-being scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5. [Google Scholar] [CrossRef]
- Gremigni, P.; Stewart-Brown, S. Measuring mental well-being: Italian validation of the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS). G. Ital. Psicol. 2011, 38, 485–505. [Google Scholar] [CrossRef]
- Lyubomirsky, S.; Lepper, H.S. A measure of subjective happiness: Preliminary reliability and construct validation. Soc. Indic. Res. 1999, 46, 137–155. [Google Scholar] [CrossRef]
- Iani, L.; Lauriola, M.; Layous, K.; Sirigatti, S. Happiness in Italy: Translation, Factorial Structure and Norming of the Subjective Happiness Scale in a Large Community Sample. Soc. Indic. Res. 2014, 118, 953–967. [Google Scholar] [CrossRef]
- Cicchetti, D.V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 1994, 6, 284–290. [Google Scholar] [CrossRef]
- Pinheiro, J.C.; Bates, D.M. Mixed-Effects Models in S and S-PLUS; Springer: Berlin/Heidelberg, Germany, 2000; ISBN 1441903178. [Google Scholar]
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017. [Google Scholar]
- Imel, Z.; Baldwin, S.; Bonus, K.; MacCoon, D. Beyond the individual: Group effects in mindfulness-based stress reduction. Psychother. Res. 2008. [Google Scholar] [CrossRef] [PubMed]
- Kumlander, S.; Lahtinen, O.; Turunen, T.; Salmivalli, C. Two is more valid than one, but is six even better? The factor structure of the Self-Compassion Scale (SCS). PLoS ONE 2018, 13, e0207706. [Google Scholar] [CrossRef] [PubMed]
- López, A.; Sanderman, R.; Smink, A.; Zhang, Y.; Eric, V.S.; Ranchor, A.; Schroevers, M.J. A reconsideration of the self-compassion scale’s total score: Self-compassion versus self-criticism. PLoS ONE 2015, 10, e0132940. [Google Scholar] [CrossRef]
- Petrocchi, N.; Ottaviani, C.; Couyoumdjian, A. Dimensionality of self-compassion: Translation and construct validation of the self-compassion scale in an Italian sample. J. Ment. Health 2014, 23, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Sperduti, M.; Martinelli, P.; Piolino, P. A neurocognitive model of meditation based on activation likelihood estimation (ALE) meta-analysis. Conscious. Cogn. 2012, 21, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, N. Self-reports: How the questions shape the answers. Am. Psychol. 1999, 54, 93–105. [Google Scholar] [CrossRef]
- Lavrakas, P. Respondent Fatigue. In Encyclopedia of Survey Research Methods; Sage Publications Inc.: Thousand Oaks, CA, USA, 2013. [Google Scholar]
| Variables | Mean (SD) Controls | Mean (SD) Treated | p-Value a |
|---|---|---|---|
| Age | 41.52 (13.91) | 42.64 (13.44) | 0.46 |
| N (%) controls | N (%) treated | ||
| Sex | |||
| Male | 29 (8%) | 17 (5%) | 0.72 |
| Female | 176 (51%) | 122 (36%) | |
| Nationality | |||
| Italian | 195 (57) | 136 (39%) | 0.31 |
| Non-Italian | 10 (3%) | 3 (1%) | |
| Marital status | |||
| Cohabitant/married | 87 (25%) | 56 (16%) | 0.37 |
| Unmarried/single | 94 (27%) | 59 (17%) | |
| Separated/Divorced | 20 (6%) | 22 (6%) | |
| Widowed | 3 (1%) | 2 (<1%) | |
| Number of children | |||
| 0 | 131 (38%) | 80 (23%) | 0.29 |
| 1 | 33 (10%) | 33 (10%) | |
| 2 | 37 (11%) | 25 (7%) | |
| ≥3 | 4 (1%) | 1 (<1%) | |
| Dependent children/family members | |||
| No | 156 (45%) | 107 (31%) | 0.76 |
| Yes | 49 (14%) | 30 (9%) | |
| Unpaid loans | |||
| No | 164 (48%) | 110 (32%) | 0.77 |
| Yes | 37 (11%) | 28 (8%) | |
| Education | |||
| Middle school | 8 (2%) | 4 (1%) | 0.93 |
| High school | 80 (23%) | 57 (17%) | |
| Degree | 90 (26%) | 62 (18%) | |
| Post-graduate course (e.g., Ph.D.) | 27 (%) | 16 (%) | |
| Job | |||
| Public or private employee | 89 (26%) | 69 (20%) | 0.67 |
| Freelance (e.g., lawyer, doctor etc.) | 30 (9%) | 19 (6%) | |
| Student | 50 (14%) | 28 (8%) | |
| Unemployed or looking for a job | 9 (3%) | 7 (2%) | |
| Housewife | 6 (2%) | 4 (1%) | |
| Retired | 14 (4%) | 6 (2%) | |
| Other | 6 (2%) | 6 (2%) | |
| Type of employment agreement | |||
| Undetermined term | 26 (8%) | 23 (7%) | 0.10 |
| Fixed term | 94 (27%) | 68 (20%) | |
| Not applicable | 58 (17%) | 25 (7%) | |
| Employee satisfaction | |||
| No | 60 (18%) | 48 (14%) | 0.27 |
| Yes | 140 (41%) | 84 (24%) | |
| Sport | |||
| No | 48 (14%) | 27 (8%) | 0.45 |
| Yes | 157 (46%) | 112 (33%) | |
| Time spent on sport activities | |||
| Every day | 15 (4%) | 6 (2%) | 0.37 |
| 3 times a week | 50 (14%) | 31 (9%) | |
| 2 times a week | 58 (17%) | 52 (15%) | |
| Rarely | 44 (13%) | 24 (7%) | |
| Never | 37 (11%) | 26 (8%) | |
| Smoker | |||
| Yes | 30 (9%) | 17 (5%) | 0.64 |
| No | 174 (51%) | 121 (35%) | |
| Favourite music genre | |||
| All | 45 (13%) | 38 (11%) | 0.01 |
| No one in particular | 31 (9%) | 14 (4%) | |
| Rock | 42 (12%) | 22 (6%) | |
| Pop | 45 (13%) | 23 (7%) | |
| Jazz | 7 (2%) | 13 (4%) | |
| Classic | 14 (4%) | 21 (6%) | |
| Other | 21 (6%) | 7 (2%) | |
| Knowledge about meditation | |||
| Clear idea | 75 (22%) | 64 (19%) | 0.19 |
| Vague idea | 105 (30%) | 62 (18%) | |
| Just heard of | 23 (7%) | 11 (3%) | |
| Never heard of | 2 (1%) | 0 (0%) | |
| Previous meditation experience | |||
| Yes | 108 (31%) | 80 (23%) | 0.45 |
| No | 97 (28%) | 59 (17%) | |
| Religious | |||
| No | 114 (33%) | 61 (18%) | 0.04 |
| Yes | 87 (25%) | 76 (22%) | |
| Number of books read in a year | |||
| 0–1 | 14 (4%) | 8 (2%) | 0.92 |
| 2–3 | 51 (15%) | 35 (10%) | |
| >3 | 139 (40%) | 96 (28%) | |
| Member of a cultural/sportive association | |||
| No | 136 (40%) | 86 (25%) | 0.49 |
| Yes | 67 (19%) | 51 (15%) | |
| Diet | |||
| Mediterranean | 173 (50%) | 112 (32%) | 0.34 |
| Vegetarian | 19 (5%) | 20 (6%) | |
| Vegan | 5 (1%) | 1 (<1%) | |
| Other | 7 (2%) | 5 (1%) | |
| Use of biological product | |||
| No | 126 (37%) | 83 (24%) | 0.96 |
| Yes | 79 (23%) | 54 (16%) | |
| Disease/disability | |||
| No | 175 (51%) | 118 (34%) | 1 |
| Yes | 30 (9%) | 21 (6%) | |
| Addiction | |||
| No | 189 (55%) | 127 (37%) | 1 |
| Yes | 14 (4%) | 10 (3%) | |
| Have you ever gone to a psychologist | |||
| No | 96 (28%) | 73 (21%) | 0.35 |
| Yes | 109 (32%) | 66 (19%) | |
| Currently treated by a psychologist | |||
| No | 178 (52%) | 116 (34%) | 0.57 |
| Yes | 27 (8%) | 22 (6%) |
| Questionnaire | Mean (SD) Controls t0 | Mean (SD) Treated t0 | Mean (SD) Controls t1 | Mean (SD) Treated t1 | Internal Consistency t0 | Internal Consistency t1 |
|---|---|---|---|---|---|---|
| CORE-OM | ||||||
| All Items | 1.18 (0.56) | 1.07 (0.48) | 1.09 (0.57) | 0.84 (0.47) | 0.93 | 0.94 |
| Subjective well-being | 1.52 (0.90) | 1.53 (0.82) | 1.55 (0.92) | 1.19 (0.77) | 0.78 | 0.81 |
| Life functioning | 1.20 (0.56) | 1.16 (0.47) | 1.19 (0.61) | 0.95 (0.50) | 0.77 | 0.84 |
| Symptoms/problems | 1.40 (0.76) | 1.32 (0.70) | 1.31 (0.73) | 1.00(0.63) | 0.69 | 0.78 |
| Risk to self and other | 0.13 (0.27) | 0.09 (0.22) | 0.13 (0.31) | 0.08 (0.23) | 0.89 | 0.89 |
| FFMQ | ||||||
| All Items | 3.32 (0.53) | 3.33 (0.52) | 3.29 (0.54) | 3.50 (0.52) | 0.92 | 0.93 |
| Observing | 3.30 (0.66) | 3.33 (0.72) | 3.24 (0.73) | 3.54 (0.75) | 0.79 | 0.83 |
| Describing | 3.60 (0.75) | 3.51 (0.72) | 3.56 (0.79) | 3.68 (0.72) | 0.91 | 0.93 |
| Acting with awareness | 3.23 (0.77) | 3.30 (0.82) | 3.22 (0.76) | 3.40 (0.74) | 0.90 | 0.90 |
| Non-judging of inner experience | 3.49 (0.83) | 3.57 (0.78) | 3.51 (0.86) | 3.69 (0.78) | 0.88 | 0.90 |
| Non reactivity to inner experience | 2.90 (0.66) | 2.89 (0.67) | 2.84 (0.66) | 3.13 (0.72) | 0.81 | 0.85 |
| SWLS | ||||||
| All Items | 20.35 (7.23) | 20.31 (6.72) | 20.42 (7.25) | 21.73 (6.56) | 0.90 | 0.91 |
| PANAS | ||||||
| Positive | 33.45 (6.25) | 33.29 (5.57) | 32.69 (6.51) | 34.55 (5.42) | 0.84 | 0.86 |
| Negative | 24.67 (7.66) | 23.91 (7.51) | 24.34 (7.35) | 21.94 (7.10) | 0.89 | 0.89 |
| PSS | ||||||
| All Items | 19.17 (7.26) | 19.19 (6.94) | 18.99 (7.58) | 16.01 (6.40) | 0.89 | 0.91 |
| SCS | ||||||
| All Items | 3.08 (0.66) | 3.12 (0.69) | 3.10 (0.68) | 3.24 (0.66) | 0.95 | 0.95 |
| Self-kindness | 2.77 (0.54) | 2.86 (0.55) | 2.79 (0.57) | 2.92 (0.59) | 0.90 | 0.92 |
| Self-judgment | 3.20 (0.88) | 3.28 (0.89) | 3.25 (0.92) | 3.43 (0.90) | 0.85 | 0.88 |
| Common humanity | 2.94 (0.89) | 2.93 (0.90) | 2.97 (0.91) | 3.12 (0.83) | 0.79 | 0.80 |
| Isolation | 3.54 (0.96) | 3.54 (0.94) | 3.50 (0.99) | 3.65 (0.88) | 0.84 | 0.86 |
| Mindfulness | 3.04 (0.86) | 2.99 (0.86) | 3.00 (0.78) | 3.13 (0.82) | 0.82 | 0.80 |
| Over identification | 3.05 (0.86) | 3.12 (0.85) | 3.13 (0.88) | 3.22 (0.84) | 0.79 | 0.81 |
| WEMWBS | ||||||
| All Items | 48.96 (8.85) | 48.48 (7.23) | 48.12 (9.06) | 51.97 (7.31) | 0.91 | 0.93 |
| SHS | ||||||
| All Items | 4.30 (1.30) | 4.35 (1.32) | 4.25 (1.39) | 4.59 (1.21) | 0.84 | 0.86 |
| Questionnaire | β Time X Group [95%CI] | p-Value |
|---|---|---|
| CORE-OM | ||
| All Items | −0.20 [−0.30;−0.10] | 0.0002 * |
| Subjective well-being | −0.37 [−0.55;−0.19] | <0.0001 * |
| Life functioning | −0.20 [−0.31;−0.09] | 0.0003 * |
| Symptoms/problems | −0.23 [−0.37;−0.09] | 0.001 * |
| Risk to self and others | −0.02 [−0.08;0.03] | 0.46 |
| FFMQ | ||
| All Items | 0.20 [0.12;0.28] | <0.0001 * |
| Observing | 0.27 [0.16;0.38] | <0.0001 * |
| Describing | 0.22 [0.11;0.33] | <0.0001 * |
| Acting with awareness | 0.11 [−0.02;0.24] | 0.08 |
| Non-judging of inner experience | 0.10 [−0.04;0.23] | 0.16 |
| Non-reactivity to inner experience | 0.30 [0.18;0.43] | <0.0001 * |
| SWLS | ||
| All Items | 1.43 [0.42;2.45] | 0.006 * |
| PANAS | ||
| Positive | 1.99 [0.95;3.04] | 0.0002 * |
| Negative | −1.67 [−2.92;−0.43] | 0.009 * |
| PSS | ||
| All Items | −2.98 [−4.25;−1.71] | <0.0001 * |
| SCS | ||
| All Items | 0.10 [−0.004;0.21] | 0.06 |
| Self-kindness | 0.05 [−0.06;0.16] | 0.37 |
| Self-judgment | 0.11 [−0.06;0.27] | 0.20 |
| Common humanity | 0.15 [−0.01;0.31] | 0.08 |
| Isolation | 0.14 [−0.30;0.31] | 0.12 |
| Mindfulness | 0.17 [0.02;0.33] | 0.03 |
| Over identification | 0.03 [−0.13;0.18] | 0.74 |
| WEMWBS | ||
| All Items | 4.38 [2.93;5.83] | <0.0001 * |
| SHS | ||
| All Items | 0.29 [0.10;0.48] | 0.003 * |
| Questionnaire | β Days [95% CI] | p-Value |
|---|---|---|
| CORE-OM | ||
| All Items | −0.05 [−0.08;−0.02] | 0.0002 * |
| Subjective well-being | −0.03 [−0.08; 0.01] | 0.173 |
| Life functioning | −0.06 [−0.09;−0.03] | <0.0001 * |
| Symptoms/problems | −0.02 [−0.10;−0.03] | 0.0003 * |
| Risk to self and others | −0.01 [−0.03;0.004] | 0.14 |
| FFMQ | ||
| All Items | 0.03 [0.01;0.05] | 0.002 * |
| Observing | 0.02 [−0.01;0.05] | 0.23 |
| Describing | 0.02 [−0.002;0.05] | 0.07 |
| Acting with awareness | 0.04 [0.002;0.8] | 0.04 |
| Non-judging of inner experience | 0.06 [0.02;0.10] | 0.001 * |
| Non-reactivity to inner experience | 0.01 [−0.02;0.04] | 0.5 |
| SWLS | ||
| All Items | 0.54 [0.25;0.84] | 0.0004 * |
| PANAS | ||
| Positive | 0.05 [−0.21;0.31] | 0.72 |
| Negative | −0.31 [−0.67;0.05] | 0.09 |
| PSS | ||
| All Items | −0.29 [−0.62;0.04] | 0.08 |
| SCS | ||
| All Items | 0.02 [−0.005;0.05] | 0.11 |
| Self-kindness | −0.002 [−0.3;0.03] | 0.91 |
| Self-judgment | 0.06 [0.02;0.10] | 0.005 * |
| Common humanity | 0.002 [−0.04;0.05] | 0.94 |
| Isolation | 0.01 [−0.03;0.06] | 0.48 |
| Mindfulness | 0.02 [−0.01;0.06] | 0.23 |
| Over identification | 0.03 [−0.009;0.07] | 0.13 |
| WEMWBS | ||
| All Items | 0.31 [−0.08;0.69] | 0.12 |
| SHS | ||
| All Items | 0.05 [−0.008;0.11] | 0.09 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fazia, T.; Bubbico, F.; Salvato, G.; Berzuini, G.; Bruno, S.; Bottini, G.; Bernardinelli, L. Boosting Psychological Well-Being through a Social Mindfulness-Based Intervention in the General Population. Int. J. Environ. Res. Public Health 2020, 17, 8404. https://doi.org/10.3390/ijerph17228404
Fazia T, Bubbico F, Salvato G, Berzuini G, Bruno S, Bottini G, Bernardinelli L. Boosting Psychological Well-Being through a Social Mindfulness-Based Intervention in the General Population. International Journal of Environmental Research and Public Health. 2020; 17(22):8404. https://doi.org/10.3390/ijerph17228404
Chicago/Turabian StyleFazia, Teresa, Francesco Bubbico, Gerardo Salvato, Giovanni Berzuini, Salvatore Bruno, Gabriella Bottini, and Luisa Bernardinelli. 2020. "Boosting Psychological Well-Being through a Social Mindfulness-Based Intervention in the General Population" International Journal of Environmental Research and Public Health 17, no. 22: 8404. https://doi.org/10.3390/ijerph17228404
APA StyleFazia, T., Bubbico, F., Salvato, G., Berzuini, G., Bruno, S., Bottini, G., & Bernardinelli, L. (2020). Boosting Psychological Well-Being through a Social Mindfulness-Based Intervention in the General Population. International Journal of Environmental Research and Public Health, 17(22), 8404. https://doi.org/10.3390/ijerph17228404






