Long-Term Effect of Income Level on Mortality after Stroke: A Nationwide Cohort Study in South Korea
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Data Source
2.3. Study Population
2.4. Variables
- <3 months from the first stroke event
- 3–12 months after the first stroke event
- 13–36 months after the first stroke event
- >36 months after the first stroke event.
2.5. Statistical Analysis
2.6. Ethics Statement
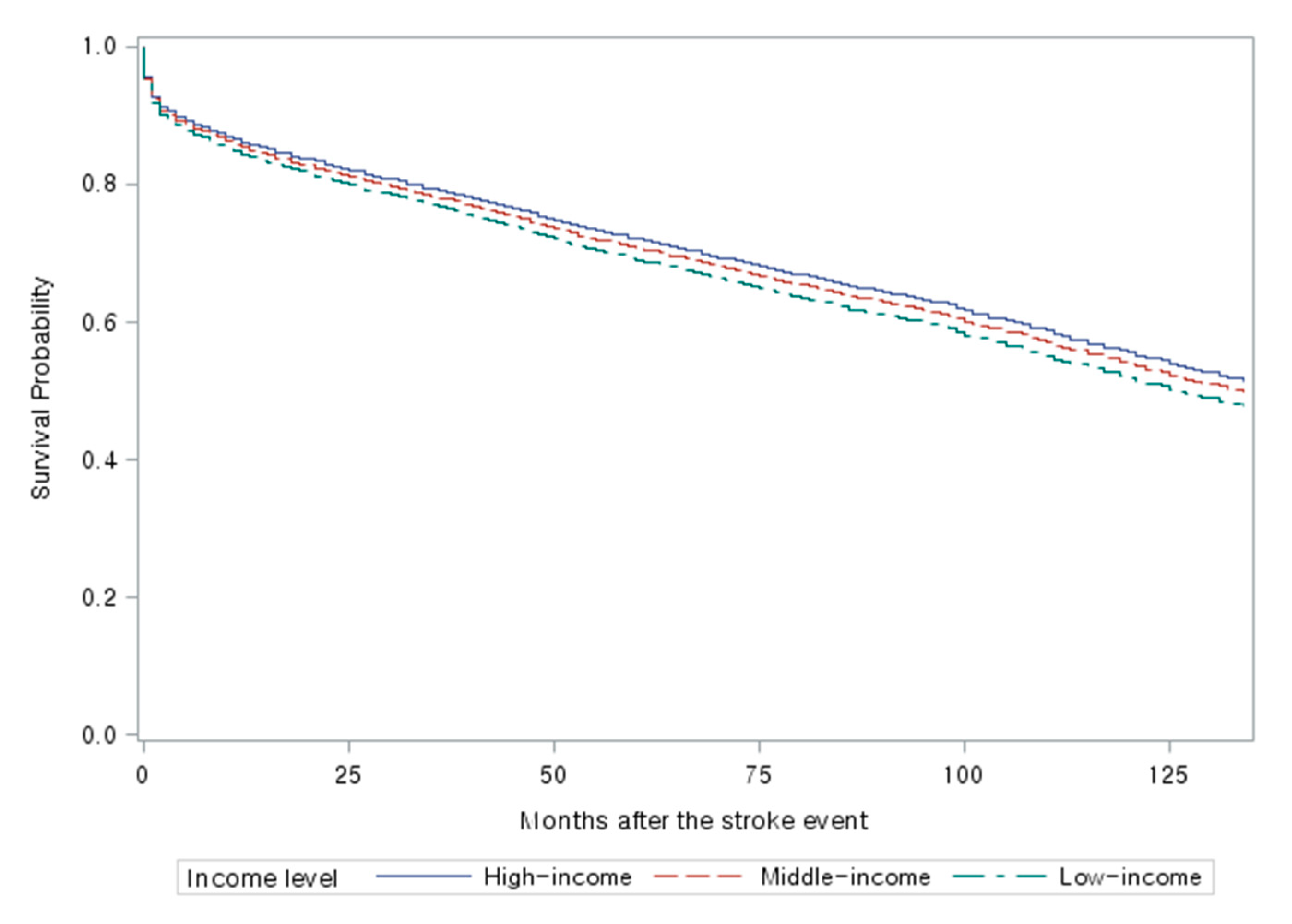
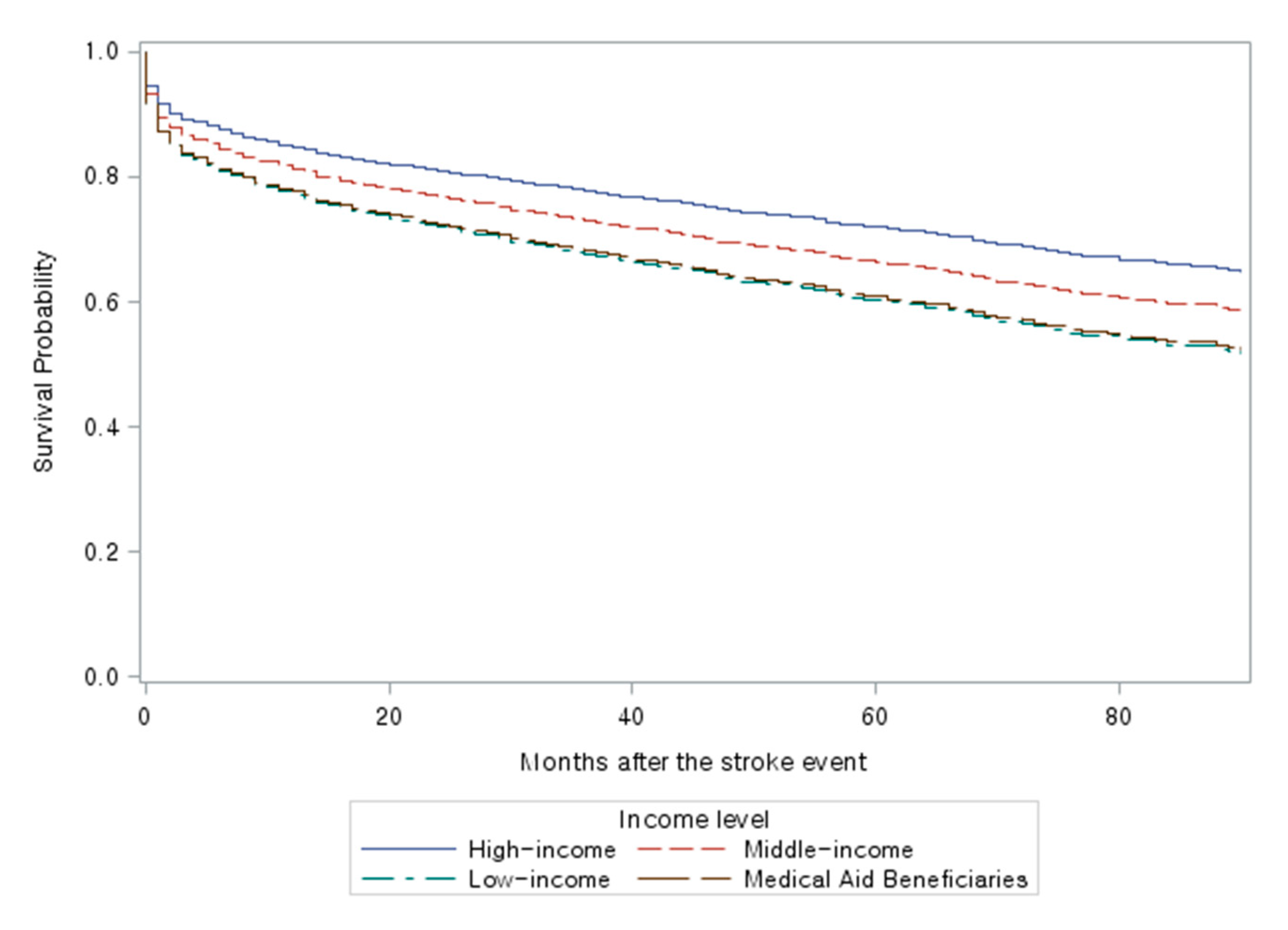
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mansfield, A.; Inness, E.L.; McIlroy, W.E. Stroke. Handb. Clin. Neurol. 2018, 159, 205–228. [Google Scholar] [CrossRef]
- Marshall, I.J.; Wang, Y.; Crichton, S.L.; McKevitt, C.J.; Rudd, A.G.; Wolfe, C.D.A. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. 2015, 14, 1206–1218. [Google Scholar] [CrossRef]
- Zhou, G.; Liu, X.; Xu, G.; Liu, X.; Zhang, R.; Zhu, W. The effect of socioeconomic status on three-year mortality after first-ever ischemic stroke in Nanjing, China. BMC Public Health 2006, 6, 227. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bray, B.D.; Paley, L.; Hoffman, A.; James, M.; Gompertz, P.; Wolfe, C.D.A.; Hemingway, H.; Rudd, A.G. Socioeconomic disparities in first stroke incidence, quality of care, and survival: A nationwide registry-based cohort study of 44 million adults in England. Lancet Public Health 2018, 3, e185–e193. [Google Scholar] [CrossRef]
- Jaja, B.N.; Saposnik, G.; Nisenbaum, R.; Schweizer, T.A.; Reddy, D.; Thorpe, E.K.; Macdonald, R.L.; Shigematsu, T.; Fujinaka, T.; Yoshimine, T.; et al. Effect of socioeconomic status on inpatient mortality and use of postacute care after subarachnoid hemorrhage. Stroke 2013, 44, 2842–2847. [Google Scholar] [CrossRef]
- Oza, R.; Rundell, K.; Garcellano, M. Recurrent ischemic stroke: Strategies for prevention. Am. Fam. Physician 2017, 96, 436–440. [Google Scholar]
- Langhorne, P.; Stott, D.J.; Robertson, L.; Macdonald, J.; Jones, L.; McAlpine, C.; Dick, F.; Taylor, G.S.; Murray, G. Medical complications after stroke. Stroke 2000, 31, 1223–1229. [Google Scholar] [CrossRef]
- Langagergaard, V.; Palnum, K.H.; Mehnert, F.; Ingeman, A.; Krogh, B.R.; Bartels, P.; Johnsen, S.P. Socioeconomic differences in quality of care and clinical outcome after stroke. Stroke 2011, 42, 2896–2902. [Google Scholar] [CrossRef]
- Kapral, M.; Fang, J.; Chan, C.; Alter, D.A.; Bronskill, S.E.; Hill, M.D.; Manuel, D.G.; Tu, J.V.; Anderson, G.M. Neighborhood income and stroke care and outcomes. Neurology 2012, 79, 1200–1207. [Google Scholar] [CrossRef]
- Wang, S.; Shen, B.; Wei, L.; Wu, M.; Wang, J. Association between socioeconomic status and prognosis after ischemic stroke in South China. Neurol. Res. 2019, 41, 916–922. [Google Scholar] [CrossRef]
- Lindmark, A.; Glader, E.-L.; Asplund, K.; Norrving, B.; Eriksson, M.; Riks-Stroke Collaboration. Socioeconomic disparities in stroke case fatality–Observations from riks-stroke, the Swedish Stroke Register. Int. J. Stroke 2014, 9, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.J. The South Korean health care system. Jpn. Med. Assoc. J. 2009, 52, 206–209. [Google Scholar]
- Kim, J.-H.; Kim, N.R.; Park, E.-C.; Han, K.-T.; Choi, Y.; Lee, S.G. Impact of continuous medical aid utilisation on healthcare utilisation: Unique insight using the 2008–2012 Korean Welfare Panel Study (KOWEPS). BMJ Open 2016, 6, e008583. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hwang, K.-T.; Ju, Y.W.; A Kim, Y.; Kim, J.; Oh, S.; Jung, J.; Chai, Y.J.; Choi, I.S.; Oh, S.W. Prognostic influence of Korean public medical insurance system on breast cancer patients. Ann. Surg. Treat. Res. 2019, 96, 58–69. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.S.; Park, S.-H.; Shin, S.A.; Kim, K. Cohort profile: The National Health Insurance Service–National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2017, 46, 1–8. [Google Scholar] [CrossRef]
- Jung, C.; Kwon, H.; Nahm, J. The equity of the national health insurance contribution in Korea-The equity of the national health insurance contribution in Korea. Korean Soc. Secur. Stud. 2014, 30, 317–344. Available online: http://www.riss.kr/link?id=A100037639 (accessed on 11 November 2020).
- Rha, J.-H.; Koo, J.; Cho, K.H.; Kim, E.-G.; Oh, G.S.; Lee, S.J.; Cha, J.K.; Oh, J.-J.; Ham, G.-R.; Seo, H.-S.; et al. Two-Year direct medical costs of stroke in Korea: A multi-centre incidence-based study from hospital perspectives. Int. J. Stroke 2012, 8, 186–192. [Google Scholar] [CrossRef]
- Thygesen, S.K.; Christiansen, C.; Christensen, S.; Lash, T.L.; Sorensen, H.T. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med. Res. Methodol. 2011, 11, 2–7. [Google Scholar] [CrossRef]
- Lindholt, J.S.; Juul, S.; Fasting, H.; Henneberg, E.W. Screening for abdominal aortic aneurysms: Single centre randomised controlled trial. BMJ 2005, 330, 750–752. [Google Scholar] [CrossRef]
- Persson, I. Essays on the Assumption of Proportional Hazards in Cox Regression. Ph.D. Thesis, Uppsala University, Uppsala, Sweden, 2002. [Google Scholar]
- Zhang, Z.; Reinikainen, J.; Adeleke, K.A.; Pieterse, M.E.; Groothuis-Oudshoorn, C.G.M. Time-varying covariates and coefficients in Cox regression models. Ann. Transl. Med. 2018, 6, 121. [Google Scholar] [CrossRef]
- Stecksén, A.; Glader, E.-L.; Asplund, K.; Norrving, B.; Eriksson, M. Education Level and Inequalities in Stroke Reperfusion Therapy: Observations in the Swedish Stroke Register. Stroke 2014, 45, 2762–2768. [Google Scholar] [CrossRef] [PubMed]
- Sjölander, M.; Eriksson, M.; Asplund, K.; Norrving, B.; Glader, E.-L. Socioeconomic inequalities in the prescription of oral anticoagulants in stroke patients with atrial fibrillation. Stroke 2015, 46, 2220–2225. [Google Scholar] [CrossRef] [PubMed]
- Samet, J.M. Tobacco smoking: The leading cause of preventable disease worldwide. Thorac. Surg. Clin. 2013, 23, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Specter, S.E. Poverty and obesity: The role of energy density and energy costs. Am. J. Clin. Nutr. 2004, 79, 6–16. [Google Scholar] [CrossRef]
- Chen, R.; McKevitt, C.; Rudd, A.G.; Wolfe, C.D. Socioeconomic deprivation and survival after stroke: Findings from the prospective South London Stroke Register of 1995 to 2011. Stroke 2014, 45, 217–223. [Google Scholar] [CrossRef]
- Park, J.M. Equity of access under Korean universal health insurance. Asia Pac. J. Public Health 2012, 27, NP914–NP924. [Google Scholar] [CrossRef]
- Sohn, M.; Che, X.; Park, H.-J. Unmet healthcare needs, catastrophic health expenditure, and health in South Korea’s universal healthcare system: Progression towards improving equity by NHI type and income level. Healthcare 2020, 8, 408. [Google Scholar] [CrossRef]
- Elfassy, T.; Grasset, L.; Glymour, M.M.; Swift, S.; Zhang, L.; Howard, G.; Howard, V.J.; Flaherty, M.; Rundek, T.; Osypuk, T.L.; et al. Sociodemographic disparities in long-term mortality among stroke survivors in the United States. Stroke 2019, 50, 805–812. [Google Scholar] [CrossRef]
- Kleindorfer, D.; Lindsell, C.J.; Broderick, J.P.; Flaherty, M.L.; Woo, D.; Ewing, I.; Schmit, P.; Moomaw, C.; Alwell, K.; Pancioli, A.; et al. Community socioeconomic status and prehospital times in acute stroke and transient ischemic attack: Do poorer patients have longer delays from 911 call to the emergency department? Stroke 2006, 37, 1508–1513. [Google Scholar] [CrossRef]
- Sheifer, S.E.; Rathore, S.S.; Gersh, B.J.; Weinfurt, K.P.; Oetgen, W.J.; Breall, J.A.; Schulman, K.A. Time to Presentation with acute myocardial infarction in the elderly. Circulation 2012, 102, 1651–1656. [Google Scholar] [CrossRef]
- Park, Y.H.; Kang, G.H.; Song, B.G.; Chun, W.J.; Lee, J.H.; Hwang, S.Y.; Oh, J.H.; Park, K.; Kim, Y.D. Factors related to prehospital time delay in acute ST-segment elevation myocardial infarction. J. Korean Med. Sci. 2012, 27, 864–869. [Google Scholar] [CrossRef] [PubMed]
- Seifi, A.; Elliott, R.-J.; Elsehety, M.A. Impact of patients’ income on stroke prognosis. J. Stroke Cerebrovasc. Dis. 2016, 25, 2308–2311. [Google Scholar] [CrossRef] [PubMed]
| Demographic Characteristics | Employees | Self-Employed and Medical Aid Beneficiaries | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | High-Income | Middle-Income | Low-Income | Total | High-Income | Middle-Income | Low-Income | Medical Aid Beneficiaries | |
| Total n (%) | 7720 (100) | 2534 (100) | 2964 (100) | 2222 (100) | 3948 (100) | 799 (100) | 1826 (100) | 553 (100) | 770 (100) |
| Gender n (%) | |||||||||
| Male | 4109 (53.2) | 1268 (50.0) | 1596 (53.9) | 1245 (56.0) | 2074 (52.5) | 439 (54.9) | 1071 (58.7) | 238 (43.0) | 326 (42.3) |
| Female | 3611 (46.8) | 1266 (50.0) | 1368 (46.1) | 977 (44.0) | 1874 (47.5) | 360 (45.1) | 755 (41.4) | 315 (57.0) | 444 (57.7) |
| Age n (%) | |||||||||
| 18–44 years | 694 (9.0) | 167 (6.6) | 304 (10.3) | 223 (10.0) | 362 (9.2) | 70 (8.8) | 195 (10.7) | 51 (9.2) | 46 (6.0) |
| 45–64 years | 2715 (35.2) | 573 (22.6) | 1055 (35.6) | 1087 (48.9) | 1563 (39.6) | 352 (44.1) | 815 (44.6) | 165 (29.8) | 231 (30.0) |
| 65–80 years | 3303 (42.8) | 1305 (51.5) | 1290 (43.5) | 708 (31.9) | 1517 (38.4) | 295 (36.9) | 652 (35.7) | 226 (40.9) | 344 (44.7) |
| >80 years | 1008 (13.0) | 489 (19.3) | 315 (10.6) | 204 (9.2) | 506 (12.8) | 82 (10.3) | 164 (9.0) | 111 (20.1) | 149 (19.4) |
| Physical Disability Status n (%) | |||||||||
| Severe | 164 (2.1) | 63 (2.5) | 65 (2.2) | 36 (1.6) | 166 (4.2) | 14 (1.8) | 40 (2.2) | 24 (4.3) | 88 (11.4) |
| Mild | 701 (9.1) | 225 (8.9) | 286 (9.7) | 190 (8.6) | 453 (11.5) | 63 (7.9) | 164 (9) | 65 (11.8) | 161 (20.9) |
| None | 6855 (88.8) | 2246 (88.6) | 2613 (88.1) | 1996 (89.8) | 3329 (84.3) | 722 (90.4) | 1622 (88.8) | 464 (83.9) | 521 (67.7) |
| Living Location n (%) | |||||||||
| Rural | 1030 (13.3) | 373 (14.7) | 426 (14.4) | 231 (10.4) | 621 (15.7) | 79 (9.9) | 302 (16.5) | 109 (19.7) | 131 (17.0) |
| Urban | 3390 (43.9) | 1080 (42.6) | 1296 (43.7) | 1014 (45.6) | 1695 (42.9) | 336 (42.1) | 786 (43) | 233 (42.1) | 340 (44.2) |
| Metropolitan | 3300 (42.7) | 1081 (42.7) | 1242 (41.9) | 977 (44.0) | 1632 (41.3) | 384 (48.1) | 738 (40.4) | 211 (38.2) | 299 (38.8) |
| Visited ED n (%) | |||||||||
| Rural | 226 (2.9) | 85 (3.3) | 98 (3.3) | 43 (1.9) | 155 (3.9) | 16 (2.0) | 68 (3.7) | 33 (6.0) | 38 (4.9) |
| Urban | 3462 (44.9) | 1117 (44.1) | 1341 (45.2) | 1004 (45.2) | 1800 (45.6) | 315 (39.4) | 856 (46.9) | 260 (47.0) | 369 (47.9) |
| Metropolitan | 4032 (52.2) | 1332 (52.6) | 1525 (51.5) | 1175 (52.9) | 1993 (50.5) | 468 (58.6) | 902 (49.4) | 260 (47.0) | 363 (47.1) |
| Incidence Year of Initial Stroke Event n (%) | |||||||||
| 2004–2006 | 1856 (24.0) | 601 (23.7) | 727 (24.5) | 528 (23.8) | |||||
| 2007–2010 | 3023 (39.2) | 995 (39.3) | 1192 (40.2) | 836 (37.6) | 1890 (47.9) | 376 (47.1) | 828 (45.3) | 261 (47.2) | 425 (55.2) |
| 2011–2014 | 2841 (36.8) | 938 (37.0) | 1045 (35.3) | 858 (38.6) | 2058 (52.1) | 423 (52.9) | 998 (54.7) | 292 (52.8) | 345 (44.8) |
| CCI n (%) | |||||||||
| 0–2 | 1375 (17.8) | 328 (12.9) | 539 (18.2) | 508 (22.9) | 698 (17.7) | 154 (19.3) | 399 (21.9) | 85 (15.4) | 60 (7.8) |
| 3–5 | 2921 (37.8) | 839 (33.1) | 1176 (39.7) | 906 (40.8) | 1427 (36.1) | 308 (38.5) | 694 (38.0) | 199 (36.0) | 226 (29.4) |
| ≥6 | 3424 (44.4) | 1367 (54.0) | 1249 (42.1) | 808 (36.3) | 1823 (46.2) | 337 (42.2) | 733 (40.1) | 269 (48.6) | 484 (62.9) |
| Type of the Stroke n (%) | |||||||||
| Hemorrhagic | 2132 (27.6) | 629 (24.8) | 818 (27.6) | 685 (30.8) | 1194 (30.2) | 238 (29.8) | 613 (33.6) | 160 (28.9) | 183 (23.8) |
| Ischemic | 5331 (69.1) | 1827 (72.1) | 2048 (69.1) | 1456 (65.5) | 2621 (66.4) | 541 (67.7) | 1145 (62.7) | 369 (66.7) | 566 (73.5) |
| Mixed | 257 (3.3) | 78 (3.1) | 98 (3.3) | 81 (3.7) | 133 (3.4) | 20 (2.5) | 68 (3.7) | 24 (4.3) | 21 (2.7) |
| Visited Hospital Level n (%) | |||||||||
| Primary | 430 (5.6) | 150 (5.9) | 161 (5.4) | 119 (5.3) | 253 (6.4) | 38 (4.8) | 108 (5.9) | 37 (6.7) | 70 (9.1) |
| Secondary | 4035 (52.3) | 1288 (50.8) | 1530 (51.6) | 1217 (54.8) | 2240 (56.7) | 382 (47.8) | 1033 (56.6) | 345 (62.4) | 480 (62.3) |
| Tertiary | 3255 (42.1) | 1096 (43.3) | 1273 (43.0) | 886 (39.9) | 1455 (36.9) | 379 (47.4) | 685 (37.5) | 171 (30.9) | 220 (28.6) |
| Clinical Outcome n (%) | |||||||||
| Survived | 5225 (67.7) | 1605 (63.3) | 2021 (68.2) | 1599 (72.0) | 2611 (66.1) | 599 (75.0) | 1286 (70.4) | 324 (58.6) | 402 (52.2) |
| Died | 2495 (32.3) | 929 (36.7) | 943 (31.8) | 623 (28.0) | 1337 (33.9) | 200 (25.0) | 540 (29.6) | 229 (41.4) | 368 (47.8) |
| Groups | Patients (n) | Death (n) | Mortality Rate (%) | aHR (95% CI) |
|---|---|---|---|---|
| High income | 2534 | 929 | 36.7 | Reference |
| Middle income | 2964 | 943 | 31.8 | 1.06 (0.97–1.17) |
| Low income | 2222 | 623 | 28.0 | 1.15 (1.04–1.28) |
| Groups | Self-Employed Insured/Medical Aid Patients | |
|---|---|---|
| n (Mortality Rate%) | aOR (95% CI) | |
| Total death | 1337 (33.9%) | |
| High income | 200 (25.0%) | Reference |
| Middle income | 540 (29.6%) | 1.38 (1.12–1.70) |
| Low income | 229 (41.4%) | 1.88 (1.45–2.44) |
| Medical Aid beneficiaries | 368 (47.8%) | 2.06 (1.62–2.62) |
| Within 3 months of initial stroke | 578 (14.6%) | |
| High income | 89 (11.1%) | Reference |
| Middle income | 255 (14%) | 1.37 (1.04–1.81) |
| Low income | 95 (17.2%) | 1.70 (1.20–2.39) |
| Medical Aid beneficiaries | 139 (18.1%) | 1.74 (1.26–2.41) |
| 3–12 months after initial stroke | 217 (5.5%) | |
| High income | 32 (4.0%) | Reference |
| Middle income | 79 (4.3%) | 1.27 (0.83–1.97) |
| Low income | 42 (7.6%) | 2.15 (1.31–3.55) |
| Medical Aid beneficiaries | 64 (8.3%) | 2.27 (1.43–3.62) |
| 13–36 months after initial stroke | 293 (7.4%) | |
| High income | 38 (4.8%) | Reference |
| Middle income | 110 (6.0%) | 1.52 (1.03–2.26) |
| Low income | 55 (9.9%) | 2.31 (1.47–3.64) |
| Medical Aid beneficiaries | 90 (11.7%) | 2.53 (1.66–3.85) |
| Over 36 months past initial stroke | 249 (6.3%) | |
| High income | 41 (5.1%) | Reference |
| Middle income | 96 (5.3%) | 1.27 (0.85–1.90) |
| Low income | 37 (6.7%) | 1.55 (0.95–2.55) |
| Medical Aid beneficiaries | 75 (9.7%) | 2.04 (1.33–3.15) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, S.; Cho, S.-i.; Kong, S.Y. Long-Term Effect of Income Level on Mortality after Stroke: A Nationwide Cohort Study in South Korea. Int. J. Environ. Res. Public Health 2020, 17, 8348. https://doi.org/10.3390/ijerph17228348
Jeong S, Cho S-i, Kong SY. Long-Term Effect of Income Level on Mortality after Stroke: A Nationwide Cohort Study in South Korea. International Journal of Environmental Research and Public Health. 2020; 17(22):8348. https://doi.org/10.3390/ijerph17228348
Chicago/Turabian StyleJeong, Seungmin, Sung-il Cho, and So Yeon Kong. 2020. "Long-Term Effect of Income Level on Mortality after Stroke: A Nationwide Cohort Study in South Korea" International Journal of Environmental Research and Public Health 17, no. 22: 8348. https://doi.org/10.3390/ijerph17228348
APA StyleJeong, S., Cho, S.-i., & Kong, S. Y. (2020). Long-Term Effect of Income Level on Mortality after Stroke: A Nationwide Cohort Study in South Korea. International Journal of Environmental Research and Public Health, 17(22), 8348. https://doi.org/10.3390/ijerph17228348





