Acceptability and Feasibility of a Nurse-Led, Community Health Worker Partnered Latent Tuberculosis Medication Adherence Model for Homeless Adults
Abstract
1. Introduction
2. Latent Tuberculosis Infection (LTBI) Diagnosis, Risk Factors and Treatment Regimens
3. Impact of 3HP LTBI Medication on TB Prevention among Homeless Adults and Other Vulnerable Populations
4. Purpose
5. Methods
5.1. Design
5.2. Sample and Site
5.3. Brief Description of 3HP LTBI Nurse and CHW Intervention Program
6. Procedures
7. Data Analysis
8. Results
Sociodemographic Characteristics
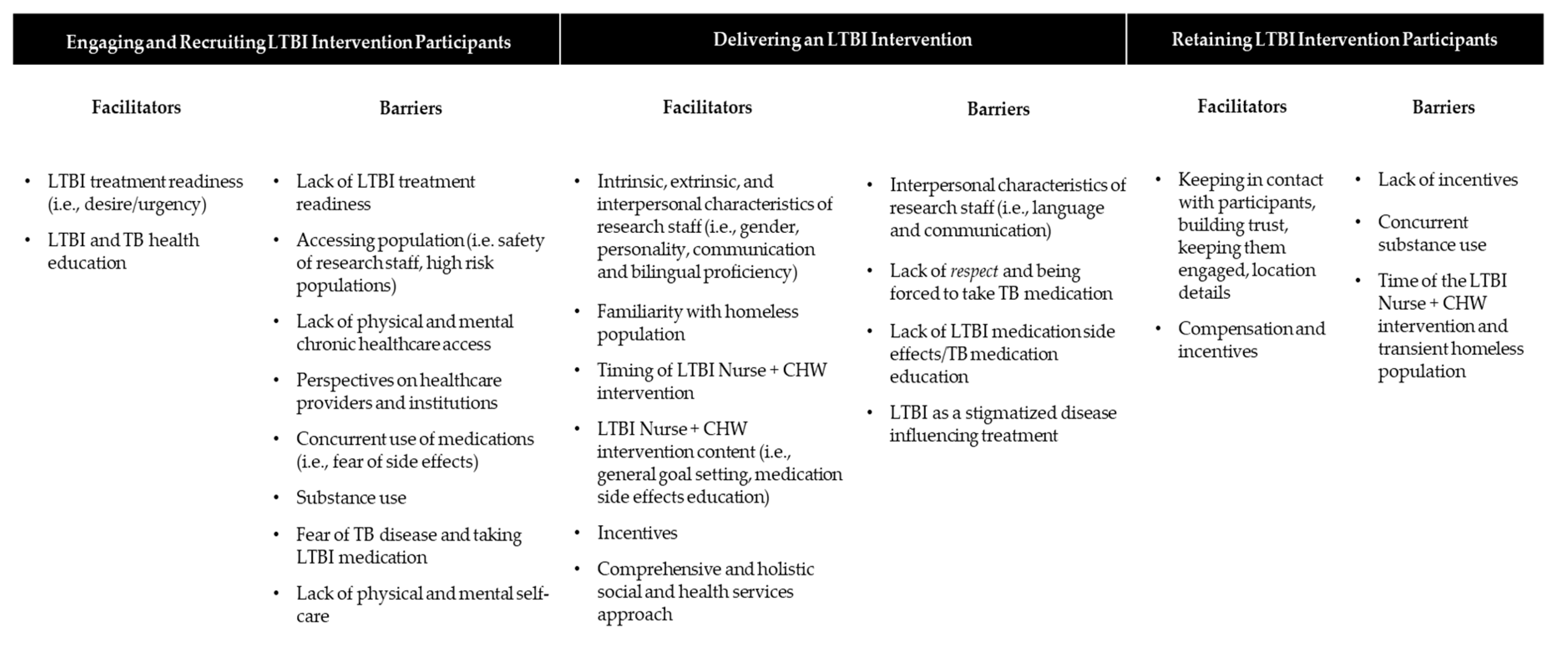
- Theme 1: Engaging and recruiting LTBI intervention participants
...If they want to stay out of harm’s way, it’s best to get and finish [LTBI treatment] where you can help yourself and help others around you. Because once you’re exposed, there’s nothing else to do… See, and myself, I did what I had to do...Participant 4, Focus Group 2
When they give me [LTBI medication], I was like all scared and all panicked. Oh, my God, hopefully I don’t got TB because the only thing you think about is …you got to leave this place. You can’t be in this shelter.Participant 9, Focus Group 3
...There’s a commercial about stopping smoking. But, the lady is smoking cigarettes and then you see her later on with a hole in her throat… And, that’s the way you have to come at people the same way you just--, you got to let them know, this could be you. Already have them in a casket. That still works.Participant 5, Focus Group 2
…down the line, you can actually die from [TB] which I already knew … Because like I say, I’ve been showing up [PPD] positive since I was a little kid. I never thought about, you know, when they always say, okay, you’re negative after a chest x-ray. I think that was just something I was going to have to do every time I take a TB test.Participant 5, Focus Group 2
I mean it’s a great thing you guys doing this but, most of the people don’t want to really get help around here.Participant 9, Focus Group 3
...There [are] a lot of people that are afraid to go to the doctor because they’re afraid that they’re going to have to pay something.Participant 10, Focus Group 3
…People think, you know, I don’t like doctors. I ain’t going to lie. I don’t like going to the hospital or nothing. So, people have that in their head. Oh, the doctor? No, no. Because I’ve been told, I got to go to the doctor. I’m the same way but since I’m not on, you know, crazy people on drugs.Participant 1, Focus Group 2
That’s what stops me from doing it if you talk about medicine because I be thinking about the side effects of it, you know. You know, but let them know that there’s nothing going to hurt you.Participant 5, Focus Group 2
For whatever reason, they just, I don’t want to say they don’t care. I’m thinking a lot lost how to care.Participant 8, Focus Group 3
- Theme 2: Delivering an LTBI intervention
I think that if ... I have like depression, I suffer from depression or anxiety, you know, the thought process is I need help, I need help… It doesn’t matter who’s going to help me.Participant 5, Focus Group 2
…I’ve talked to some battered women and worked in a facility where they [were] housed and yeah, trust, yeah, it’s harder. But...if it’s coming from a place of letting them know, look, we’re here to help you.Participant 1, Focus Group 2
So, they can have like a thing in common so people can really get cured. They can get the thing that they’re there for, you know, take the treatment.Participant 9, Focus Group 3
...That’s the risk you take when you’re trying to help people. So, like I say, you just got to get out there, you know and make an effort … and then have people like myself and whoever, not shy, they ain’t scared to talk about it. You get us out there and we relate to them.Participant 1, Focus Group 2
That’s the best way and like people like ourselves, me...have us go with you, you know. I used to use drugs or used to... Put us on the screen or TV. Not saying that that’s where I want to be but I’m not ashamed of nothing about myself.Participant 5, Focus Group 2
You don’t want to do it Fridays because Friday it’s like end of the week. Most people, in my opinion, like, you know what I’m saying, like Fridays see like oh, the weekends coming or by like the middle of the week, you know, Wednesdays.Participant 9, Focus Group 3
A goal, a homework assignment or something that I can look forward to. If I’m going to get better, if I want to get better... this is what I can do to help. Something to look for, give me a goal. Give me something.... What is TB? What is tuberculosis? Give me something I can study up on and learn about. I can’t just talk about it...Participant 1, Focus Group 2
I think the side–that was my first question. Because, you know, side effects, I see people take–they advertise medicine on TV like you guys are. And they come up with this long list of side effects. It sounds like I’m better off not taking it. So, that’s the key, you got to let them know and I take it. I take your medicine. Right now, I’m still on and I’m doing it for another month and a half. But that’s–I take a whole handful of pills at one time...Participant 2, Focus Group 2
...I’m already taking medication already for other illnesses, you know what I’m saying, what side effects is this going to–it could coincide with me. If I’m still drinking and using or I’m taking, or if I’m on it, I have HIV. I’m HIV positive. And I’m taking this other medication and I’m doing drugs, too, come on. That’s a battle in itself. That’s a battle.Participant 4, Focus Group 2
… He go to the clinic and they tell you to take this, take that but they don’t really explain it to you, what would be the benefits and all that.Participant 9, Focus Group 3
She didn’t want to comply. So they took her to put her in the hospital where she could take her medicine… See, a lot of people are not aware of that.Participant 5, Focus Group 2
Can we work on housing? Can we work on that? Can we work on the depression?”Participant 1, Focus Group 2
Yeah, very, very important and in Skid Row too much people problems mental.Participant 12, Focus Group 3
That’s a big barrier. Like people don’t really speak English and that’s a big cultural issue. If you don’t speak Spanish to them, they’re not really going to trust you.Participant 9, Focus Group 3
…Once you cross a certain barrier line, once you hear a person telling you you’re forced to take it, forced to do something, forced to take the medication, you cross that invisible line.Participant 2, Focus Group 2
That’s what happened with my fiancé I was with. She didn’t know and she didn’t want to take nothing. So, they had to incarcerate her to get her to take it. And she start taking it. After while they let her out but she had to comply. She didn’t want to comply. So, they took her put her in the hospital where she could take her medicine. And she didn’t like. She didn’t comply. See, a lot of people are not aware of that.Participant 5, Focus Group 2
When you’re in that element or you’re in that lifestyle, a lot of people, you tell a person they have a disease, a disease, they’re not going to respond to, really, they’re not going to–they’re going to, I mean, they’re going to treat it but it’s going to be a hush-hush thing. It’s going to be a, I’m not going to tell my friends. I don’t want nobody really to know.Participant 3, Focus Group 2
I think that’s going to be a very hard issue for like the young adults. Like, people over, like a little bit over 20 because some of them are teenage runaways and they stay down here. And they don’t want their picture being posted anywhere because that’s going to be a major issue for them.Participant 4, Focus Group 2
- Theme 3: Retaining LTBI intervention participants
… It’s not just a hi, bye, thing, you know what I’m saying. And make sure they continue getting to know, keep random coming down here, check in on them. Get their phone number.Participant 1, Focus Group 2
Like me, it doesn’t really matter. But, like take the medication, I don’t know if I’m right or wrong. It’s a cultural thing, too. Like, you know what I’m saying? Like, trust, when I went out there, there was this nurse.Participant 9, Focus Group 3
Keep them engaged. You know I’m saying? And a lot of people, and then people, your information, and people’s information, they’re really tired of giving–they don’t want to give up that information, you know. And they think that, and then you have to really, like I said, just baby steps before you.Participant 4, Focus Group 2
You giving me a whole handful of pills, yours might be less but I was like, you know, since I’m new, just getting here, I ain’t got no money. I was like oh, you get a card? Oh, really? Give it here. I’ll take the chance. That makes a big difference if it’s any kind of, like I said, what I’ve done and I still take it every Tuesday.Participant 2, Focus Group 2
You quit giving, they’re going to stop coming.Participant 8, Focus Group 3
...If they drinking or doing whatever they want to do, they ain’t trying to–they ain’t worrying about doing whatever. Like, taking medication. You got to hit them a day or a time that they’re willing to do that because you see them drinking or whatever they’re doing, even though they got–they got an appointment with you guys or they give you their word, they’re not going to honor that because they’re doing.Participant 9, Focus Group 3
People here, they going get their money in part or for like a week, one or two weeks and then come back. They stay in the area but you won’t see them because a lot of people go to hotels and do things like that.Participant 9, Focus Group 3
Yeah, you got to show urgency. You need to–it’s hard to keep them in one place.Participant 8, Focus Group 3
9. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kahwati, L.C.; Feltner, C.; Halpern, M.; Woodell, C.L.; Boland, E.; Amick, H.R.; Weber, R.P.; Jonas, D.E. Primary Care Screening and Treatment for Latent Tuberculosis Infection in Adults: Evidence Report and Systematic Review for the US Preventive Services Task ForceEvidence Report: Primary Care Approaches to Latent TB in AdultsEvidence Report: Primary Care Approaches to Latent TB in Adults. JAMA 2016, 316, 970–983. [Google Scholar] [PubMed]
- Goetsch, U.; Bellinger, O.K.; Buettel, K.-L.; Gottschalk, R. Tuberculosis among drug users and homeless persons: Impact of voluntary X-ray investigation on active case finding. Infection 2012, 40, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Bamrah, S.; Woodruff, R.S.Y.; Powell, K.; Ghosh, S.; Kammerer, J.S.; Haddad, M.B. Tuberculosis among the homeless, United States, 1994–2010. The international journal of tuberculosis and lung disease. Off. J. Int. Union Against Tuberc. Lung Dis. 2013, 17, 1414–1419. [Google Scholar] [CrossRef] [PubMed]
- Rosales, M.; Guevara, R.E. Tuberculosis in Los Angeles County: Surveillance Report 2016; Los Angeles County Department of Public Health: Los Angeles, CA, USA, 2016; p. 59.
- Centers for Disease Control and Prevention. TB in the Homeless Population. 2018. Available online: https://www.cdc.gov/tb/topic/populations/homelessness/default.htm (accessed on 21 June 2019).
- Nava-Aguilera, E.; Andersson, N.; Harris, E.; Mitchell, S.; Hamel, C.; Shea, B.; López-Vidal, Y.; Villegas-Arrizón, A.; Morales-Pérez, A. Risk factors associated with recent transmission of tuberculosis: Systematic review and meta-analysis. Int. J. Tuberc. Lung Dis. 2009, 13, 17–26. [Google Scholar]
- Barnes, P.F.; Yang, Z.; Preston-Martin, S.; Pogoda, J.M.; Jones, B.E.; Otaya, M.; Eisenach, K.D.; Knowles, L.; Harvey, S.; Cave, M.D.; et al. Patterns of tuberculosis transmission in Central Los Angeles. JAMA 1997, 278, 1159–1163. [Google Scholar] [CrossRef]
- United States Preventive Services Task Force. Screening for Latent Tuberculosis Infection in Adults: US Preventive Services Task Force Recommendation Statement. USPSTF Recommendation: Screening for Latent Tuberculosis in Adults. USPSTF Recommendation: Screening for Latent Tuberculosis in Adults. JAMA 2016, 316, 962–969. [Google Scholar] [CrossRef]
- United States Interagency Council on Homelessness. Fact Sheet on Preventing and Addressing Tuberculosis among People Experiencing Homelessness. 2014. Available online: https://www.usich.gov/tools-for-action/preventing-and-addressing-tuberculosis (accessed on 21 June 2019).
- Morbidity and Mortality Weekly Report. Tuberculosis outbreak associated with a homeless shelter—Kane County, Illinois, 2007–2011. MMWR Morb. Mortal. Wkly. Rep. 2012, 61, 186. [Google Scholar]
- Morbidity and Mortality Weekly Report. Targeted tuberculin testing and treatment of latent tuberculosis infection. American Thoracic Society. MMWR Recomm. Rep. 2000, 49, 1–51. [Google Scholar]
- Centers for Disease Control and Prevention. Latent Tuberculosis Infection: A Guide for Primary Health Care Providers. 2014. Available online: https://www.cdc.gov/tb/publications/ltbi/diagnosis.htm#tbInfection (accessed on 21 June 2019).
- Jasmer, R.M.; Nahid, P.; Hopewell, P.C. Latent tuberculosis infection. N. Engl. J. Med. 2002, 347, 1860–1866. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. TB Elimination—The Difference Between Latent TB Infection and TB Disease. 2011. Available online: https://www.cdc.gov/tb/publications/factsheets/general/LTBIandActiveTB.pdf (accessed on 21 June 2019).
- Centers for Disease Control and Prevention. Recommendations for Use of an Isoniazid-Rifapentine Regimen with Direct Observation to Treat Latent Mycobacterium Tuberculosis Infection. MMWR Morb. Mortal. Wkly. Rep. 2011, 60, 1650–1653. [Google Scholar]
- Hirsch-Moverman, Y.; Daftary, A.; Franks, J.; Colson, P.W. Adherence to treatment for latent tuberculosis infection: Systematic review of studies in the US and Canada. Int. J. Tuberc. Lung Dis. 2008, 12, 1235–1254. [Google Scholar] [PubMed]
- Centers for Disease Control and Prevention. Treatment Regimens for Latent TB Infection (LTBI). 2016. Available online: https://www.cdc.gov/tb/topic/treatment/ltbi.htm (accessed on 22 June 2019).
- Sterling, T.R.; Villarino, M.E.; Borisov, A.S.; Shang, N.; Gordin, F.; Bliven-Sizemore, E.; Hackman, J.; Hamilton, C.D.; Menzies, D.; Kerrigan, A.; et al. Three months of rifapentine and isoniazid for latent tuberculosis infection. N. Engl. J. Med. 2011, 365, 2155–2166. [Google Scholar] [CrossRef] [PubMed]
- Sterling, T.R.; Moro, R.N.; Borisov, A.S.; Phillips, E.; Shepherd, G.; Adkinson, N.F.; Weis, S.; Ho, C.; Villarino, M.E.; Grosset, J.; et al. Flu-like and Other Systemic Drug Reactions among Persons Receiving Weekly Rifapentine Plus Isoniazid or Daily Isoniazid for Treatment of Latent Tuberculosis Infection in the PREVENT Tuberculosis Study. Clin. Infect. Dis. 2015, 61, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Yamin, A.; Bornstein, E.; Hensel, R.; Mohamed, O.; Kempker, R.R. Predictors of Latent Tuberculosis Infection Treatment after Introduction of a New Regimen: A Retrospective Cohort Study at an Inner City Clinic. Open Forum Infect. Dis. 2016, 3, ofw082. [Google Scholar] [CrossRef]
- Nwana, N.; Marks, S.M.; Lan, E.; Chang, A.H.; Holcombe, M.; Morris, S.B. Treatment of latent Mycobacterium tuberculosis infection with 12 once weekly directly-observed doses of isoniazid and rifapentine among persons experiencing homelessness. PLoS ONE 2019, 14, e0213524. [Google Scholar] [CrossRef]
- Nyamathi, A.; Nahid, P.; Berg, J.; Burrage, J.; Christiani, A.; Aqtash, S.; Leake, B. Efficacy of nurse case-managed intervention for latent tuberculosis among homeless subsamples. Nurs. Res. 2008, 57, 33–39. [Google Scholar] [CrossRef][Green Version]
- Nyamathi, A.; Stein, J.A.; Schumann, A.; Tyler, D. Latent variable assessment of outcomes in a nurse-managed intervention to increase latent tuberculosis treatment completion in homeless adults. Health Psychol 2007, 26, 68–76. [Google Scholar] [CrossRef]
- Nyamathi, A.M.; Christiani, A.; Nahid, P.; Gregerson, P.; Leake, B. A randomized controlled trial of two treatment programs for homeless adults with latent tuberculosis infection. Int. J. Tuberc. Lung Dis. 2006, 10, 775–782. [Google Scholar]
- Shenton, A.K. Strategies for ensuring trustworthiness in qualitative research projects. Educ. Inf. 2004, 22, 63–75. [Google Scholar] [CrossRef]
- Babor, T.F.; McRee, B.; Kassebaum, P.A.; Grimaldi, P.L.; Ahmed, K.; Bray, J. Screening, Brief Intervention, and Referral to Treatment (SBIRT) toward a public health approach to the management of substance abuse. Subst. Abus. 2007, 28, 7–30. [Google Scholar] [CrossRef]
- Munro, S.A.; Lewin, S.A.; Smith, H.J.; Engel, M.E.; Fretheim, A.; Volmink, J. Patient adherence to tuberculosis treatment: A systematic review of qualitative research. PLoS Med. 2007, 4, e238. [Google Scholar] [CrossRef] [PubMed]
- Nyamathi, A.M.; Shin, S.S.; Smeltzer, J.; Salem, B.E.; Yadav, K.; Ekstrand, M.L.; Faucette, M. Achieving Drug and Alcohol Abstinence Among Recently Incarcerated Homeless Women: A Randomized Controlled Trial Comparing Dialectical Behavioral Therapy-Case Management With a Health Promotion Program. Nurs. Res. 2007, 66, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Nyamathi, A.; Liu, Y.; Marfisee, M.; Shoptaw, S.; Gregerson, P.; Saab, S.; Gelberg, L. Effects of a nurse-managed program on hepatitis A and B vaccine completion among homeless adults. Nurs. Res. 2009, 58, 13–22. [Google Scholar] [CrossRef] [PubMed]
| Mean | SD, Range | |
| Age | 51.18 | 8.60, 35–60 |
| Number of Children | 2.43 | 2.23, 1–7 |
| N | % | |
| Gender | ||
| Male | 10 | 90.9% |
| Female | 1 | 9.1% |
| Race | ||
| Black/African American | 5 | 45.5% |
| White | 5 | 45.5% |
| Other | 1 | 9.1% |
| Ethnicity | ||
| Not Hispanic or Latino | 7 | 63.6% |
| Hispanic or Latino | 4 | 36.4% |
| Country of Birth | ||
| United States | 6 | 54.5% |
| Mexico | 3 | 27.3% |
| Other | 2 | 18.2% |
| Children | ||
| Yes | 7 | 63.6% |
| No | 4 | 36.4% |
| N | % | |
| Religion | ||
| Catholic | 4 | 36.4% |
| Other | 4 | 36.4% |
| Protestant | 3 | 27.3% |
| Educational Status | ||
| <12 years | 4 | 36.4% |
| >12 years | 3 | 27.3% |
| College/Post High School | 3 | 27.3% |
| Graduate School | 1 | 9.1% |
| Homeless Status, Ever | ||
| Yes | 11 | 100% |
| No | 0 | 0% |
| A Great Deal | Somewhat | Not At All | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Did the session bring up the challenges homeless adults face when attempting to complete a medication treatment program? | 10 | 90.9% | 1 | 9.1% | 0 | 0% |
| Did the session identify the challenges experienced by someone with a substance use problem? | 7 | 63.6% | 3 | 27.3% | 1 | 9.1% |
| Did the session identify the challenges experienced by someone who is experiencing a mental health issue? | 5 | 45.5% | 5 | 45.5% | 1 | 9.1% |
| Did the session bring up useful information on strategies that can help you if you needed more stable housing? | 8 | 72.7% | 3 | 27.3% | 0 | 0% |
| Do you feel this program would be relevant for men as well as women? | 11 | 100% | 0 | 0% | 0 | 0% |
| Do you feel the session was conducted in a useful and understandable way? | 11 | 100% | 0 | 0% | 0 | 0% |
| Do you feel the discussion helped to improve the program? | 11 | 100% | 0 | 0% | 0 | 0% |
| Overall, would you recommend this program to other persons with latent TB who need to complete a medication treatment program. | 11 | 100% | 0 | 0% | 0 | 0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salem, B.E.; Klansek, E.; Morisky, D.E.; Shin, S.S.; Yadav, K.; Chang, A.H.; Nyamathi, A.M. Acceptability and Feasibility of a Nurse-Led, Community Health Worker Partnered Latent Tuberculosis Medication Adherence Model for Homeless Adults. Int. J. Environ. Res. Public Health 2020, 17, 8342. https://doi.org/10.3390/ijerph17228342
Salem BE, Klansek E, Morisky DE, Shin SS, Yadav K, Chang AH, Nyamathi AM. Acceptability and Feasibility of a Nurse-Led, Community Health Worker Partnered Latent Tuberculosis Medication Adherence Model for Homeless Adults. International Journal of Environmental Research and Public Health. 2020; 17(22):8342. https://doi.org/10.3390/ijerph17228342
Chicago/Turabian StyleSalem, Benissa E., Erin Klansek, Donald E. Morisky, Sanghyuk S. Shin, Kartik Yadav, Alicia H. Chang, and Adeline M. Nyamathi. 2020. "Acceptability and Feasibility of a Nurse-Led, Community Health Worker Partnered Latent Tuberculosis Medication Adherence Model for Homeless Adults" International Journal of Environmental Research and Public Health 17, no. 22: 8342. https://doi.org/10.3390/ijerph17228342
APA StyleSalem, B. E., Klansek, E., Morisky, D. E., Shin, S. S., Yadav, K., Chang, A. H., & Nyamathi, A. M. (2020). Acceptability and Feasibility of a Nurse-Led, Community Health Worker Partnered Latent Tuberculosis Medication Adherence Model for Homeless Adults. International Journal of Environmental Research and Public Health, 17(22), 8342. https://doi.org/10.3390/ijerph17228342





