Firefighter Overexertion: A Continuing Problem Found in an Analysis of Non-Fatal Injury Among Career Firefighters
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Setting
2.2. Classification of Injuries
2.3. Analysis
3. Results
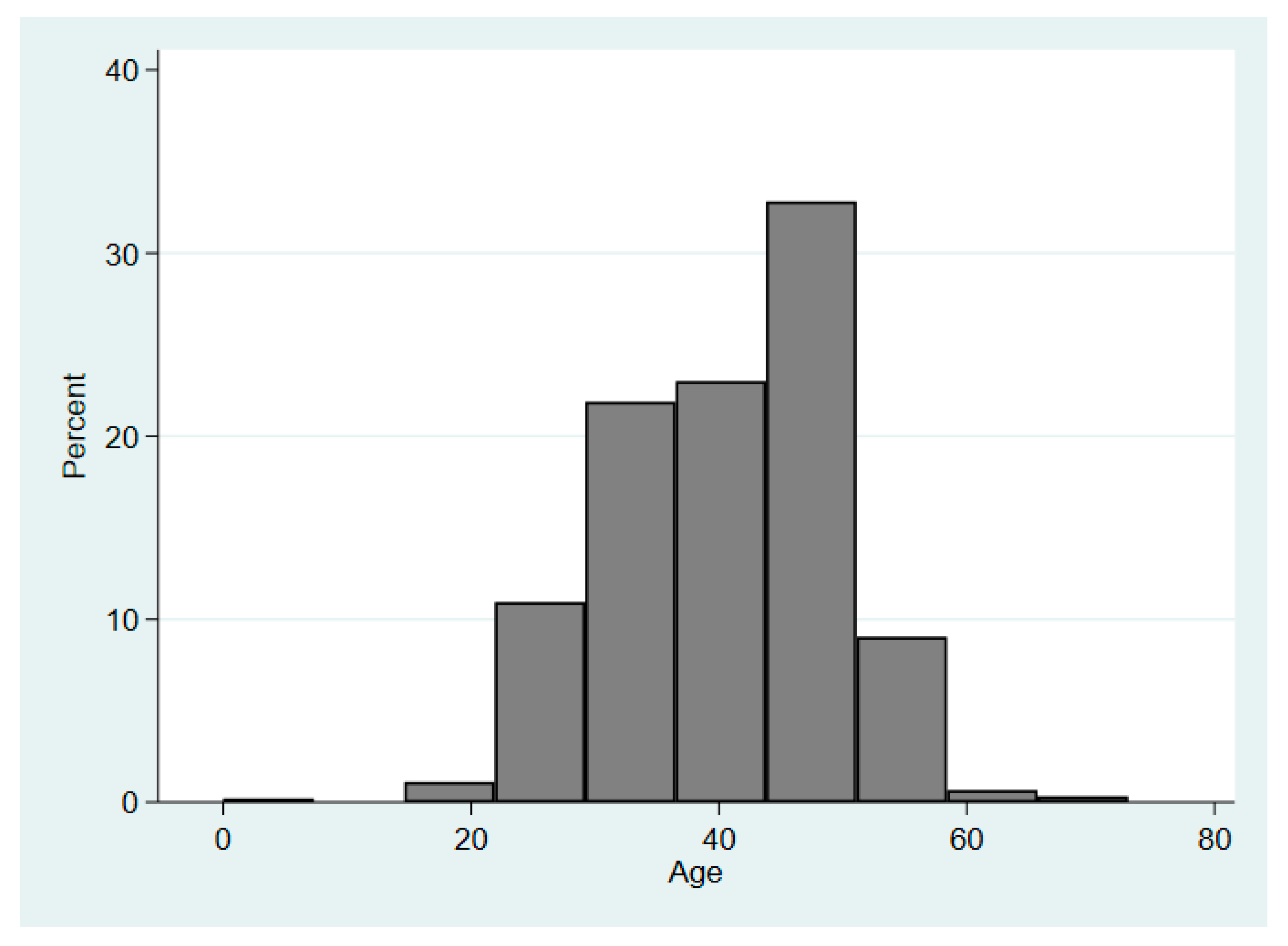
3.1. Demographics
3.2. Frequency, Causal Factors/Exposures of Injuries
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- U.S. Fire Department Profile. 2018. Available online: https://www.nfpa.org/-/media/Files/News-and-Research/Fire-statistics-and-reports/Emergency-responders/osfdprofile.pdf (accessed on 9 December 2019).
- Smith, T.D.; Dyal, M.A.; DeJoy, D.M. Workplace stress and firefighter health and safety. In Increasing Occupational Health and Safety in Workplaces; Burke, R.J., Richardsen, A.M., Eds.; Edward Elgar Publishing: Cheltenham, UK, 2019; pp. 274–292. [Google Scholar]
- Hanna, E.G.; Kjellstrom, T.; Bennett, C.; Dear, K. Climate change and rising heat: Population health implications for working people in Australia. Asia Pac. J. Public Health 2011, 23 (Suppl. 2), 14S–26S. [Google Scholar] [CrossRef]
- Withen, P. Climate change and wildland firefighter health and safety. New Solut. 2015, 24, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Clarke, C.; Zak, M.J. Fatalities to law enforcement officers and firefighters, 1992–1997. Environments 1999, 15, 3–7. [Google Scholar]
- Fabio, A.; Ta, M.; Strotmeyer, S.; Li, W.; Schmidt, E. Incident-level risk factors for firefighter injuries at structural fires. J. Occup. Environ. Med. 2002, 44, 1059–1063. [Google Scholar] [CrossRef] [PubMed]
- Szubert, Z.; Sobala, W. Work-related injuries among firefighters: Sites and circumstances of their occurrence. Int. J. Occup. Environ. Health 2002, 15, 49–55. [Google Scholar]
- United States Firefighter Injuries. 2018. Available online: https://www.nfpa.org/-/media/Files/News-and-Research/Fire-statistics-and-reports/Emergency-responders/osffinjuries.pdf (accessed on 11 September 2020).
- Overexertion and Bodily Reaction. Available online: https://injuryfacts.nsc.org/work/safety-topics/overexertion-and-bodily-reaction/ (accessed on 28 October 2020).
- Facts about Hospital Worker Safety. Available online: https://www.osha.gov/dsg/hospitals/documents/1.2_Factbook_508.pdf (accessed on 9 December 2019).
- Musculoskeletal Sprains and Strains. Available online: https://bestpractice.bmj.com/topics/en-us/578 (accessed on 30 November 2019).
- Liberty Mutual Workplace Safety Index 2018. Available online: https://business.libertymutualgroup.com/business-insurance/Documents/Services/Workplace%20Safety%20Index.pdf (accessed on 4 December 2019).
- Walton, S.M.; Conrad, K.M.; Furner, S.E.; Samo, D.G. Cause, type, and workers’ compensation costs of injury to fire fighters. Am. J. Ind. Med. 2003, 43, 454–458. [Google Scholar] [CrossRef] [PubMed]
- Poplin, G.S.; Harris, R.B.; Pollack, K.M.; Peate, W.F.; Burgess, J.L. Beyond the fireground: Injuries in the fire service. Inj. Prev. 2012, 18, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Marsh, S.M.; Gwilliam, M.; Konda, S.; Tiesman, H.M.; Fahy, R. Nonfatal Injuries to Firefighters Treated in US Emergency Departments, 2003–2014. Am. J. Prev. Med. 2018, 55, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Perkins, K.B. Volunteer fire departments: Community integration, autonomy and survival. Hum. Organ. 1987, 46, 342–348. [Google Scholar] [CrossRef]
- Jahnke, S.; Poston, W.; Haddock, C.; Jitnarin, N. Obesity and incident injury among career firefighters in the central United States. Obesity 2013, 21, 1505–1508. [Google Scholar] [CrossRef]
- Jahnke, S.A.; Hyder, M.L.; Haddock, C.K.; Jitnarin, N.; Day, R.S.; Poston, W.S.C. High-intensity fitness training among a national sample of male career firefighters. Saf. Health Work 2015, 6, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Jahnke, S.A.; Poston, W.S.C.; Haddock, C.K.; Jitnarin, N. Injury among a population based sample of career firefighters in the central USA. Inj. Prev. 2013, 19, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi-Bazargani, H. Injury epidemiology and publishing injury research. J. Inj. Violence. Res. 2011, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine and National Research Council Committee on Trauma Research. Epidemiology of Injuries: The Need for More Adequate Data. In Injury in America: A Continuing Public Health Problem; National Academics Press: Washington, DC, USA, 1985; pp. 25–36. [Google Scholar]
- Occupational Injury and Illness Classification System (OIICS) Code Trees v2.01. Available online: https://wwwn.cdc.gov/Wisards/oiics/About.aspx (accessed on 30 November 2019).
- Heiden, B.; Weigel, M.; Angerer, P.; Müller, A. Association of age and physical job demands with musculoskeletal disorders in nurses. Appl. Ergon. 2013, 44, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Holmström, E.; Engholm, G. Musculoskeletal disorders in relation to age and occupation in Swedish construction workers. Am. J. Ind. Med. 2003, 44, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Linaker, C.H.; Walker-Bone, K.; Palmer, K.; Cooper, C. Frequency and impact of regional musculoskeletal disorders. Best Pract Res. Clin. Rheumatol. 1999, 13, 197–215. [Google Scholar] [CrossRef]
- Nahrgang, J.D.; Morgeson, F.P.; Hofmann, D.A. Safety at work: A meta-analytic investigation of the link between job demands, job resources, burnout, engagement, and safety outcomes. J. Appl. Psychol. 2011, 96, 71. [Google Scholar] [CrossRef]
- Smith, T.D.; Dyal, M.-A. A conceptual safety-oriented job demands and resources model for the fire service. Int. J. Workplace Health Manag. 2016, 9, 443–460. [Google Scholar] [CrossRef]
- Smith, T.D.; DeJoy, D.M. Safety climate, safety behaviors and line-of-duty injuries in the fire service. Int. J. Emerg. Serv. 2014, 3, 49–64. [Google Scholar] [CrossRef]
- Andel, S.A.; Pindek, S.; Spector, P.E. Being called to safety: Occupational callings and safety climate in the emergency medical services. J. Occup. Environ. Med. 2016, 58, 1245–1249. [Google Scholar] [CrossRef]
- Poston, W.S.; Haddock, C.K.; Jahnke, S.A.; Jitnarin, N.; Tuley, B.C.; Kales, S.N. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J. Occup. Environ. Med. 2011, 53, 266–273. [Google Scholar] [PubMed]
- Poston, W.S.; Haddock, C.K.; Jahnke, S.A.; Jitnarin, N.; Day, R.S. An examination of the benefits of health promotion programs for the national fire service. BMC Public Health 2013, 13, 805. [Google Scholar]
- Standard on Comprehensive Occupational Medical Program for Fire Departments. Available online: https://www.nfpa.org/codes-and-standards/all-codes-and-standards/list-of-codes-and-standards/detail?code=1582 (accessed on 10 December 2019).
- Pehkonen, I.; Takala, E.-P.; Ketola, R.; Viikari-Juntura, E.; Leino-Arjas, P.; Hopsu, L.; Virtanen, T.; Haukka, E.; Holtari-Leino, M.; Nykyri, E. Evaluation of a participatory ergonomic intervention process in kitchen work. Appl. Ergon. 2009, 40, 115–123. [Google Scholar] [PubMed]
- Rivilis, I.; Cole, D.C.; Frazer, M.B.; Kerr, M.S.; Wells, R.P.; Ibrahim, S. Evaluation of a participatory ergonomic intervention aimed at improving musculoskeletal health. Am. J. Ind. Med. 2006, 49, 801–810. [Google Scholar]
- Rivilis, I.; Van Eerd, D.; Cullen, K.; Cole, D.C.; Irvin, E.; Tyson, J.; Mahood, Q. Effectiveness of participatory ergonomic interventions on health outcomes: A systematic review. Appl. Ergon. 2008, 39, 342–358. [Google Scholar]
- Silverstein, B.; Clark, R. Interventions to reduce work-related musculoskeletal disorders. J. Electromyogr. Kines. 2004, 14, 135–152. [Google Scholar]
- Alexandre, N.M.C.; de Moraes, M.A.A.; Corrêa Filho, H.R.; Jorge, S.A. Evaluation of a program to reduce back pain in nursing personnel. Rev. Saude. Publica. 2001, 35, 356–361. [Google Scholar]
- Conrad, K.M.; Lavender, S.A.; Reichelt, P.A.; Meyer, F.T. Initiating an ergonomic analysis: A process for jobs with highly variable tasks. AAOHN J. 2000, 48, 423–429. [Google Scholar] [PubMed]
- Conrad, K.M.; Reichelt, P.A.; Lavender, S.A.; Gacki-Smith, J.; Hattle, S. Designing ergonomic interventions for EMS workers: Concept generation of patient-handling devices. Appl. Ergon. 2008, 39, 792–802. [Google Scholar]
- Phillips, M.; Payne, W.; Lord, C.; Netto, K.; Nichols, D.; Aisbett, B. Identification of physically demanding tasks performed during bushfire suppression by Australian rural firefighters. Appl. Ergon. 2012, 43, 435–441. [Google Scholar]
- Poplin, G.S.; Pollack, K.M.; Griffin, S.; Day-Nash, V.; Peate, W.F.; Nied, E.; Gulotta, J.; Burgess, J.L. Establishing a proactive safety and health risk management system in the fire service. BMC Public Health 2015, 15, 407. [Google Scholar] [CrossRef]
- Frost, D.M.; Beach, T.A.; Callaghan, J.P.; McGill, S.M. Exercise-based performance enhancement and injury prevention for firefighters: Contrasting the fitness-and movement-related adaptations to two training methodologies. J. Strength Cond. Res. 2015, 29, 2441–2459. [Google Scholar] [CrossRef] [PubMed]
- Frost, D.M.; Beach, T.A.; McGill, S.M.; Callaghan, J.P. The predictive value of general movement tasks in assessing occupational task performance. Work 2015, 52, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Nevala-Puranen, N.; Pakarinen, K.; Louhevaara, V. Ergonomic intervention on neck, shoulder and arm symptoms of newspaper employees in work with visual display units. Int. J. Ind. Ergon. 2003, 31, 1–10. [Google Scholar] [CrossRef]
- Hierarchy of Controls. Available online: https://www.cdc.gov/niosh/topics/hierarchy/default.htm (accessed on 10 December 2019).
- Hur, P.; Rosengren, K.S.; Horn, G.P.; Smith, D.L.; Hsiao-Wecksler, E.T. Effect of protective clothing and fatigue on functional balance of firefighters. J. Ergon. 2013, S2, 1–7. [Google Scholar] [CrossRef]
- Park, K.; Rosengren, K.S.; Horn, G.P.; Smith, D.L.; Hsiao-Wecksler, E.T. Assessing gait changes in firefighters due to fatigue and protective clothing. Saf. Sci. 2011, 49, 719–726. [Google Scholar] [CrossRef]
- National Fire Incident Reporting System. Available online: https://www.nfirs.fema.gov/ (accessed on 18 December 2019).

| Department Characteristics | FD1 (Western U.S.) | FD2 (Eastern U.S.) |
|---|---|---|
| Number of Stations | 33 | 35 |
| Number of Personnel | ~750 sworn firefighters | ~1000 sworn firefighters |
| Number of Calls per year | ~95,000 | ~100,000 |
| Population Served | ~1.2 million | ~519,000 |
| Square Miles Protected | 181 | 132 |
| International Airport Protected? | Yes | Yes |
| Causal Factor/Exposure | Count | Percentage |
|---|---|---|
| Overexertion and bodily reaction | 494 | 54.1 |
| Exposure to harmful substances or environments | 150 | 16.4 |
| Contact with objects and equipment | 103 | 11.3 |
| Falls, slips, and trips | 79 | 8.7 |
| Violence and other injuries by persons or animals | 24 | 2.6 |
| Transportation incidents | 23 | 2.5 |
| Fires and explosions | 18 | 2.0 |
| Other | 22 | 2.4 |
| Injury Region | Count | Percentage |
|---|---|---|
| Multiple body parts | 331 | 36.3 |
| Upper extremities | 173 | 19.0 |
| Body systems (i.e., circulatory, nervous, immune) | 121 | 13.2 |
| Trunk | 120 | 13.1 |
| Lower extremities | 103 | 11.3 |
| Head | 24 | 2.6 |
| Neck, including throat | 12 | 1.3 |
| Other | 29 | 3.2 |
| Causal Factor/Exposure, n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Contact with Objects and Equipment | Exposure to Harmful Substances or Environments | Falls, Slips, and Trips | Fires and Explosions | Overexertion and Bodily Reaction | Transportation Incidents | Violence and Other Injuries by Persons or Animals | Other | Total | |
| Age Group | |||||||||
| 18–29 | 17/103 (16.5%) | 26/150 (17.3%) | 5/78 (6.4%) | 4/18 (22.2%) | 44/494 (8.9%) | 5/23 (21.7%) | 5/23 (21.7%) | 2/22 (9.1%) | 108/911 (11.9%) |
| 30–39 | 33/103 (32.1%) | 63/150 (42.0%) | 19/78 (24.4%) | 7/18 (38.9%) | 146/494 (29.6%) | 8/23 (34.9%) | 7/23 (30.5%) | 3/22 (13.6%) | 286/911 (31.4%) |
| 40–49 | 31/103 (30.1%) | 48/150 (32.0%) | 37/78 (47.4%) | 4/18 (22.2%) | 205/494 (41.5%) | 5/23 (21.7%) | 6/23 (26.1%) | 13/22 (59.1%) | 349/911 (38.3%) |
| 50–59 | 19/103 (18.4%) | 12/150 (8.0%) | 16/78 (20.5%) | 3/18(16.7%) | 82/494 (16.6%) | 5/23 (21.7%) | 4/23 (17.4%) | 3/22 (13.6%) | 144/911 (15.8%) |
| 60–64 | 1/103 (1.0%) | 0 | 0 | 0 | 3/494 (0.6%) | 0 | 0 | 0 | 4/911 (0.4%) |
| 65 and above | 2/103 (1.9%) | 1/150 (0.7%) | 1/78 (1.3%) | 0 | 14/494 (2.8%) | 0 | 1/23 (4.3%) | 1/22 (4.6%) | 20/911 (2.2%) |
| Rank/Occupation | |||||||||
| Firefighters | 68/103 (66.0%) | 119/150 (79.3%) | 52/79 (65.8%) | 15/18 (83.3%) | 349/493 (70.8%) | 12/23 (52.3%) | 11/23 (47.8%) | 10/22 (45.5%) | 636/911 (69.8%) |
| Company officers | 23/103 (22.3%) | 28/150 (18.7%) | 17/79 (21.5%) | 2/18 (11.1%) | 108/493 (21.9%) | 5/23 (21.7%) | 8/23 (34.8%) | 4/22 (18.2%) | 195/911 (21.4%) |
| Chiefs | 4/103 (3.9%) | 1/150 (0.7%) | 2/79 (2.5%) | 0 | 20/493 (4.1%) | 3/23 (13.0%) | 0 | 1/22 (4.5%) | 31/911 (3.4%) |
| Other | 8/103 (7.8%) | 2/150 (1.3%) | 8/79 (10.2%) | 1/18 (5.6%) | 16/493 (3.2%) | 3/23 (13.0%) | 4/23 (17.4%) | 7/22 (31.8%) | 49/911(5.4%) |
| Injury Region | |||||||||
| Head | 9/103 (8.8%) | 4/150 (2.7%) | 0 | 5/18 (27.7%) | 3/494 (0.6%) | 1/23 (4.8%) | 0 | 2/22 (9.1%) | 24/913 (2.6%) |
| Neck | 2/103 (1.9%) | 0 | 0 | 1/18 (5.6%) | 4/494 (0.8%) | 5/23 (23.8%) | 0 | 0 | 12/913 (1.3%) |
| Trunk | 6/103 (5.8%) | 0 | 4/79 (5.1%) | 1/18 (5.6%) | 105/494 (21.3%) | 2/23 (9.5%) | 1/24 (4.2%) | 1/22 (4.5%) | 120/913 (13.2%) |
| Upper extremities | 23/103 (22.3%) | 2/150 (1.3%) | 3/79 (3.8%) | 0 | 142/494 (28.7%) | 1/23 (4.8%) | 2/24 (8.3%) | 0 | 173/913 (18.9%) |
| Lower extremities | 10/103 (9.7%) | 1/150 (0.7%) | 15/79 (18.9%) | 0 | 71/494 (14.4%) | 5/23(14.3%) | 1/24 (4.2%) | 0 | 103/913 (11.3%) |
| Body systems | 3/103 (2.9%) | 82/150 (54.7%) | 0 | 2/18 (11.1%) | 13/494 (2.6%) | 1/23 (4.8%) | 17/24 (70.8%) | 3/22 (13.6%) | 121/913 (13.2%) |
| Multiple parts | 50/103 (48.6%) | 44/150 (29.3%) | 56/79 (70.9%) | 9/18 (50.0%) | 147/494 (29.8%) | 6/23 (28.5%) | 3/24 (12.5%) | 16/22 (72.8%) | 331/913 (36.3%) |
| Other | 0 | 17/150 (11.3%) | 1/79 (1.3%) | 0 | 9/494 (1.8%) | 2/23 (9.5%) | 0 | 0 | 29/913 (3.2%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
B. Le, A.; McNulty, L.A.; Dyal, M.-A.; DeJoy, D.M.; Smith, T.D. Firefighter Overexertion: A Continuing Problem Found in an Analysis of Non-Fatal Injury Among Career Firefighters. Int. J. Environ. Res. Public Health 2020, 17, 7906. https://doi.org/10.3390/ijerph17217906
B. Le A, McNulty LA, Dyal M-A, DeJoy DM, Smith TD. Firefighter Overexertion: A Continuing Problem Found in an Analysis of Non-Fatal Injury Among Career Firefighters. International Journal of Environmental Research and Public Health. 2020; 17(21):7906. https://doi.org/10.3390/ijerph17217906
Chicago/Turabian StyleB. Le, Aurora, Lily A. McNulty, Mari-Amanda Dyal, David M. DeJoy, and Todd D. Smith. 2020. "Firefighter Overexertion: A Continuing Problem Found in an Analysis of Non-Fatal Injury Among Career Firefighters" International Journal of Environmental Research and Public Health 17, no. 21: 7906. https://doi.org/10.3390/ijerph17217906
APA StyleB. Le, A., McNulty, L. A., Dyal, M.-A., DeJoy, D. M., & Smith, T. D. (2020). Firefighter Overexertion: A Continuing Problem Found in an Analysis of Non-Fatal Injury Among Career Firefighters. International Journal of Environmental Research and Public Health, 17(21), 7906. https://doi.org/10.3390/ijerph17217906






