Solid Oxygen-Purifying (SOP) Filters: A Self-Disinfecting Filters to Inactivate Aerosolized Viruses
Abstract
1. Introduction
2. Materials and Methods
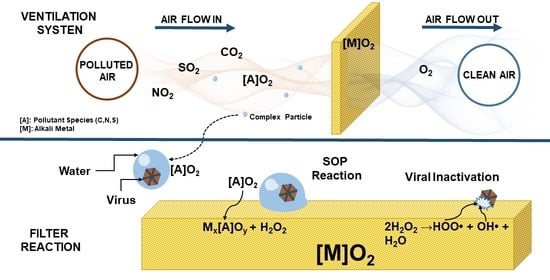
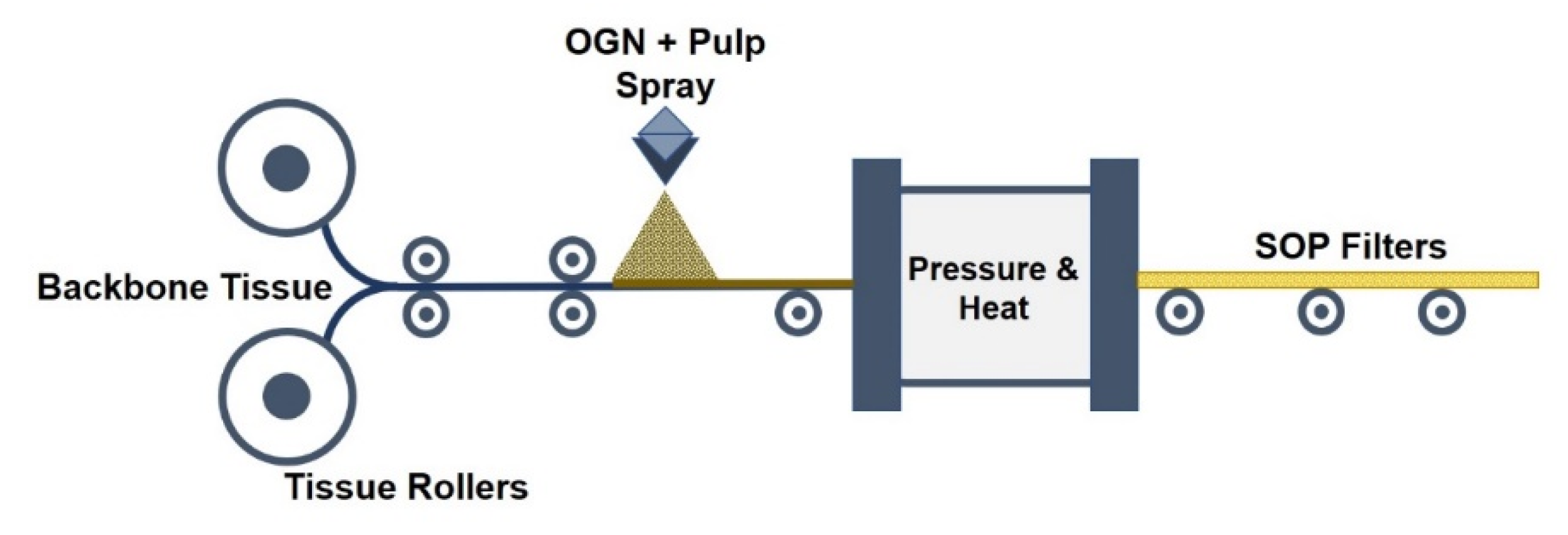
2.1. Manufacturing Solid Oxygen-Purifying (SOP) Filters
2.2. Virus and Host Preparation
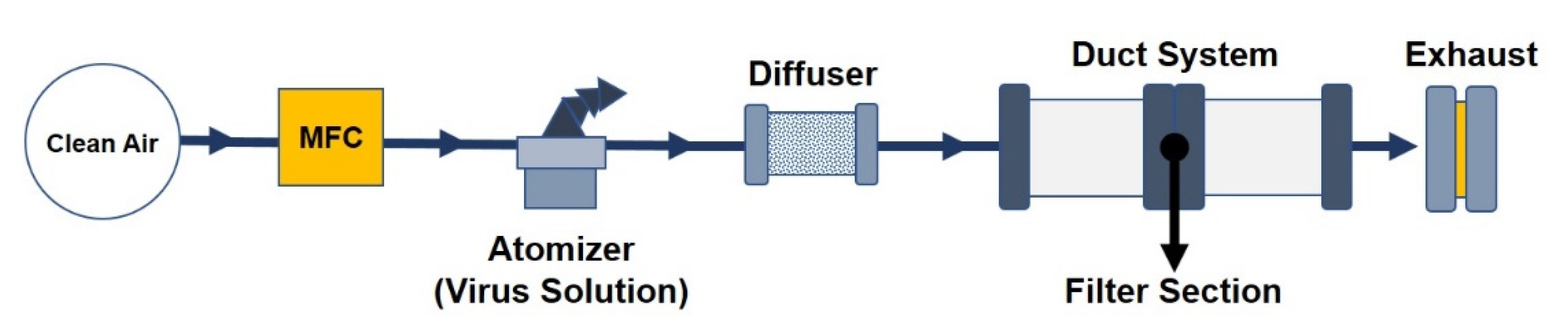
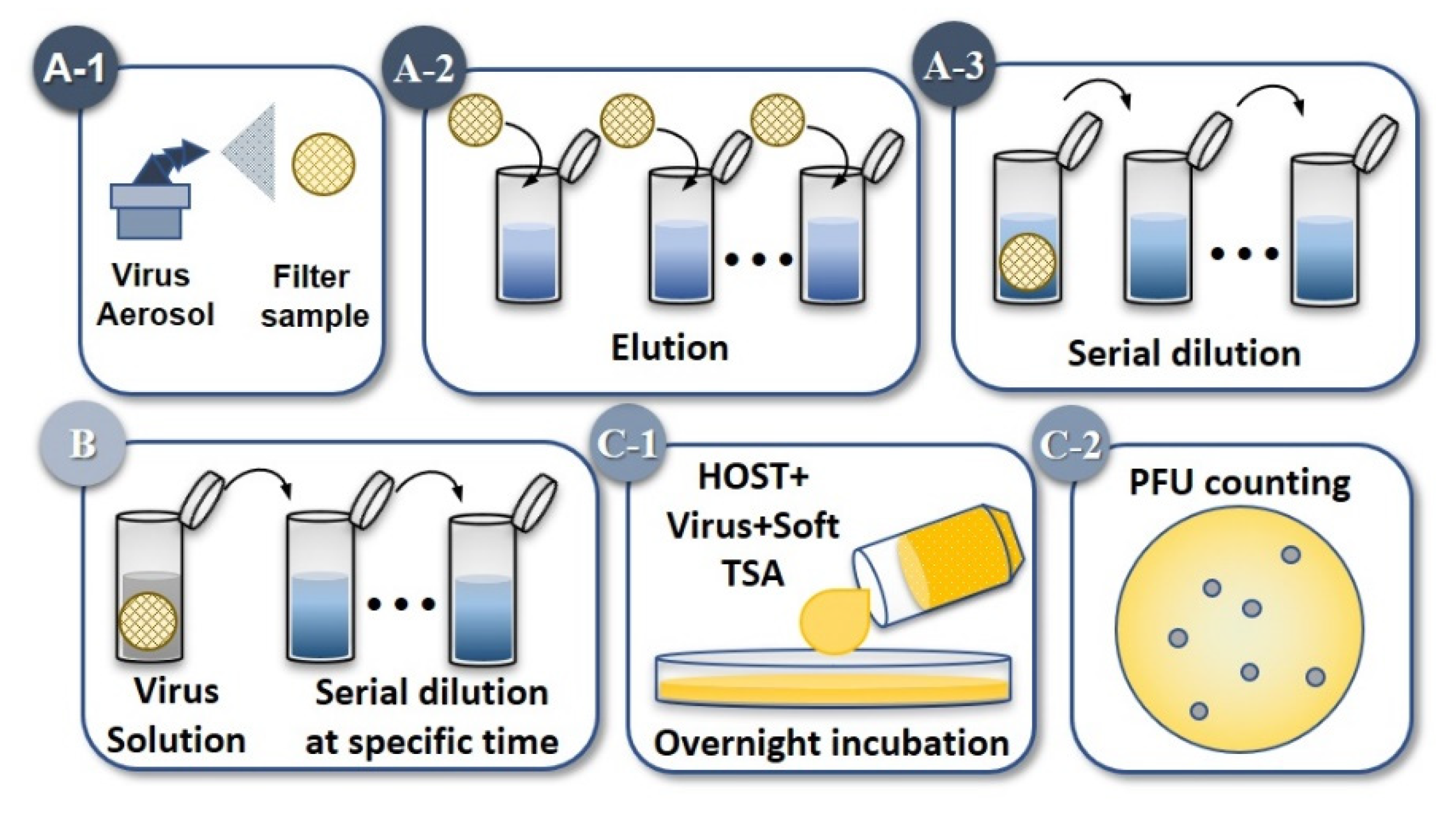
2.3. Experiment 1: Aerosolized MS2 Bacteriophage
2.4. Experiment 2: High Viral Load Exposure and Variable Exposure Time
2.5. Calculations
3. Results
3.1. MS2 Bacteriophage Inactivation Efficiency on Filters Configurations
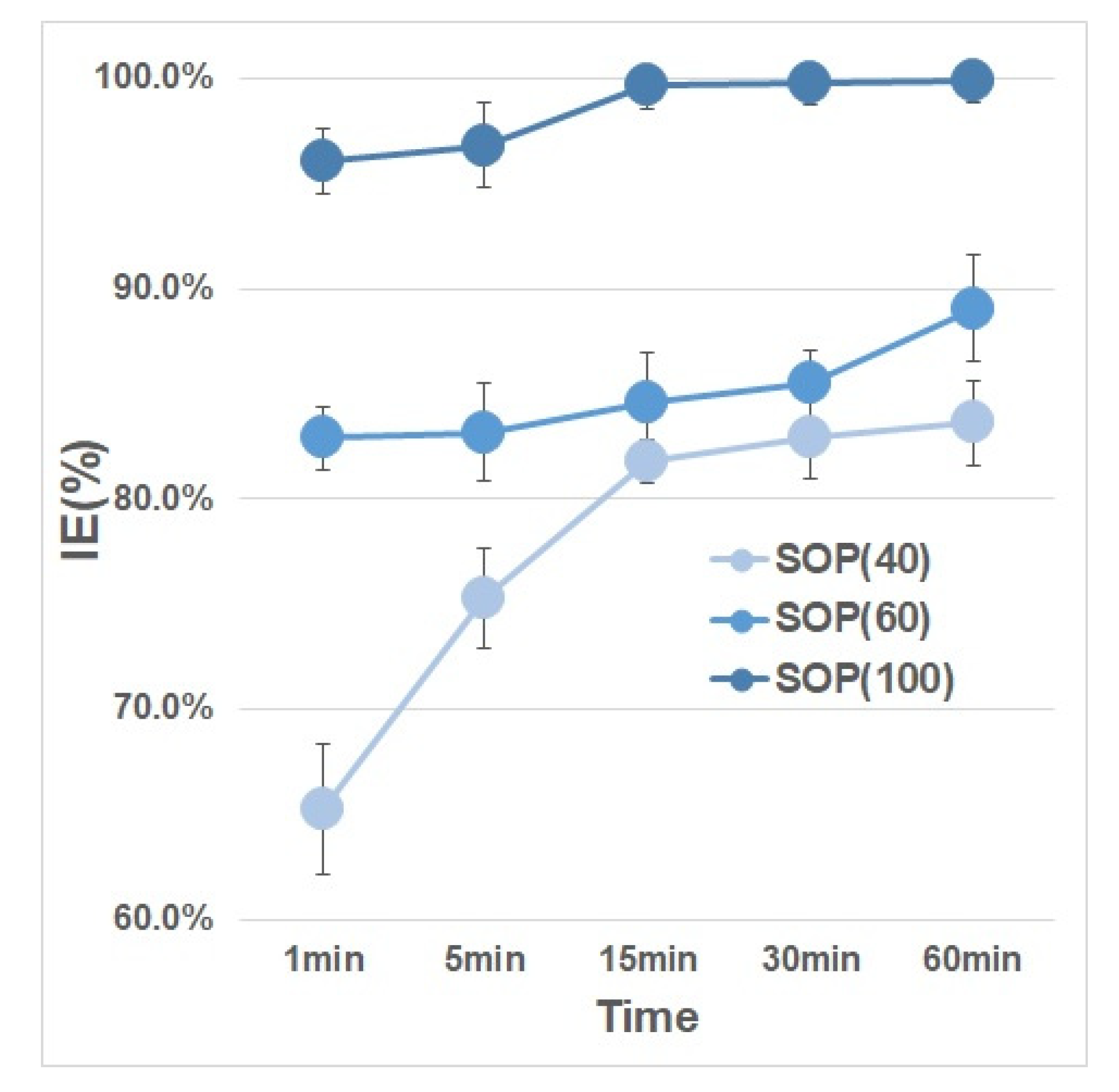
3.2. Effects of Exposure Time (High Viral Load)
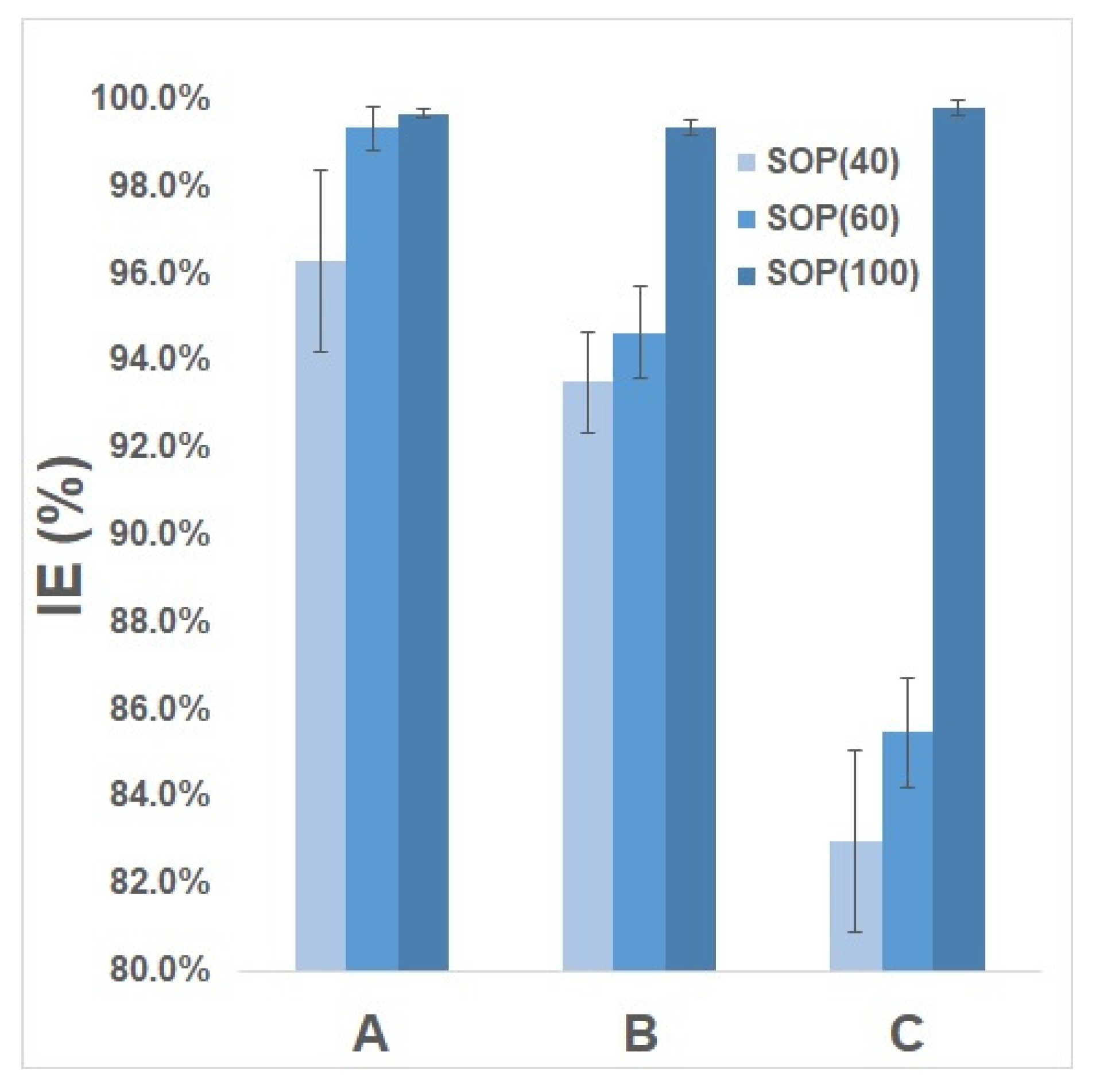
3.3. Comparison of Different Controls
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Riley, W.J.; Mckone, T.E.; Lai, A.C.K.; Nazaroff, W.W. Indoor particulate matter of outdoor origin: Importance of size-dependent removal mechanisms. Environ. Sci. Technol. 2002, 36, 200–207. [Google Scholar] [CrossRef]
- Qian, J.; Hospodsky, D.; Yamamoto, N.; Nazaroff, W.W.; Peccia, J. Size-resolved emission rates of airborne bacteria and fungi in an occupied classroom. Indoor Air 2012, 22, 339–351. [Google Scholar] [CrossRef]
- Pan, M.; Lednicky, J.A.; Wu, C.Y. Collection, particle sizing and detection of airborne viruses. J. Appl. Microbiol. 2019, 127, 1596–1611. [Google Scholar] [CrossRef]
- Tang, J.W. The effect of environmental parameters on the survival of airborne infectious agents. J. R. Soc. Interface. 2009, 6, S737. [Google Scholar] [CrossRef] [PubMed]
- Hinds, W.C. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles, 2nd ed.; Wiley: New York, NY, USA, 1998. [Google Scholar]
- Marr, L.C.; Tang, J.W.; van Mullekom, J.; Lakdawala, S.S. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J. R. Soc. Interface. 2019, 16. [Google Scholar] [CrossRef] [PubMed]
- Barker, J.; Vipond, I.B.; Bloomfield, S.F. Effects of cleaning and disinfection in reducing the spread of norovirus contamination via environmental surfaces. J. Hosp. Infect. 2004, 58, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Winther, B.; Hayden, F.G.; Hendley, J.O. Picornavirus infections in children diagnosed by RT-PCR during longitudinal surveillance with weekly sampling: Association with symptomatic illness and effect of season. J. Med. Virol. 2006, 78, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Fornek, M.; Schwab, K.J.; Chapin, A.R.; Gibson, K.; Shwab, E.; Spencer, C.; Henning, K. A norovirus outbreak at a long-term-care facility: The role of environmental surface contamination. Infect. Control. Hosp. Epidemiol. 2005, 26, 802–810. [Google Scholar] [CrossRef] [PubMed]
- Kiseleva, L.F. Survival of enteric viruses in water and food stuffs and on various surfaces. Hyg. Sanit. 1968, 33, 439–440. [Google Scholar]
- Abad, F.X.; Villena, C.; Guix, S.; Caballero, S.; Pinto, R.M.; Bosch, A. Potential role of fomites in the vehicular transmission of human astroviruses. Appl. Environ. Microbiol. 2001, 67, 3904–3907. [Google Scholar] [CrossRef]
- Sattar, S.A.; Ijaz, M.K.; Lloyd-Evans, N.; Springthorpe, V.S.; Nair, R.C. Institutional outbreaks, of rotavirus diarrhea: Potential role of fomites and environmental surfaces as vehicles for virus transmission. J. Hyg. Camb. 1986, 96, 277–289. [Google Scholar] [CrossRef] [PubMed]
- Boone, S.A.; Gerba, C.P. Significance of foraites in the spread of respiratory and enteric viral disease. Appl. Environ. Microbiol. 2007, 73, 1687–1696. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.C.; Li, C.S. Inactivation of virus-containing aerosols by ultraviolet germicidal irradiation. Aerosol. Sci. Tech. 2007, 39, 1136–1142. [Google Scholar] [CrossRef]
- Wigginton, K.R.; Menin, L.; Montoya, J.P.; Kohn, T. Oxidation of virus proteins during UV254 and singlet oxygen mediated inactivation. Environ. Sci. Technol. 2010, 44, 5437–5443. [Google Scholar] [CrossRef]
- Wigginton, K.R.; Pecson, B.M.; Sigstam, T.; Bosshard, F.; Kohn, T. Virus inactivation mechanisms: Impact of disinfectants on virus function and structural integrity. Environ. Sci Technol. 2012, 46, 12069–12078. [Google Scholar] [CrossRef]
- Versoza, M.; Jung, W.S.; Barabad, M.L.; Ko, S.; Kim, M.; Park, D. Reduction of Escherichia Coli using metal plates with the influence of applied low current and physical barrier of filter layers. Int. J. Environ. Res. Public Health 2019, 16, 3887. [Google Scholar] [CrossRef]
- van Doremalen, N.; Bushmaker, T.; Morris, D. Aerosol and surface of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Farnsworth, J.E.; Goyal, S.M.; Kim, S.W.; Kuehn, T.H.; Raynor, P.C.; Ramakrishnan, M.; Anantharaman, S.; Tang, W. Development of a method for bacteria and virus recovery from heating, ventilation, and air conditioning (HVAC) filters. J. Environ. Monit. 2006, 8, 1006–1013. [Google Scholar] [CrossRef]
- Pitkin, A.; Otake, S.; Dee, S. Biosecurity Protocols for the Prevention of Spread of Porcine Reproductive and Respiratory Syndrome Virus. Available online: https://www.swineweb.com/biosecurity-protocols-for-the-prevention-of-spread-of-porcine-reproductive-and-respiratory-syndrome-virus/ (accessed on 2 May 2018).
- Miaskiewiez-Peska, E.; Lebkowska, M. Comparison of aerosol and bioaerosol collection on air filters. Aerobiologia 2012, 28, 185–193. [Google Scholar] [CrossRef]
- Prussin, A.J., II; Vikram, A.; Bibby, K.J.; Marr, L.C. Seasonal dynamics of the airborne bacterial community and selected viruses in a children’s daycare center. PLoS ONE 2016, 11, e0151104. [Google Scholar] [CrossRef]
- Afshinnekoo, E.; Meydan, C.; Chowdhury, S.; Jaroudi, D.; Boyer, C.; Bernstein, N.; Maritz, J.M.; Reeves, D.; Gandara, J.; Chhangawala, S.; et al. Geospatial resolution of human and bacterial diversity with city-scale metagenomics. Cells 2015, 1, 1–15. [Google Scholar]
- Mason, C.E.; Chernomoretz, A.; Stolovitzky, G.; Labaj, P.P.; Graf, A.B.; Darling, A.; Burke, C.; Noushmehr, H.; Moraes, M.O.; Dias-Neto, E.; et al. The metagenomics and metadesign of the subway and urban biomes (MetaSUB) international consortium inaugural meeting report. Microbiome 2016, 4. [Google Scholar] [CrossRef]
- Li, Y.; Leung, G.M.; Tang, J.W.; Yang, X.; Chao, C.Y.H.; Lin, J.Z.; Lu, J.W.; Nielsen, P.V.; Niu, J.; Qian, H.; et al. Role of ventilation in airborne transmission of infectious agents in the built environment: A multidisciplinary systematic review. Indoor. Air. 2007, 17, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Shui, E.Y.C.; Leung, N.H.L.; Cowling, B.J. Controversy around airborne versus droplet transmission of respiratory viruses: Implication for infection prevention. Curr. Opin. Infect. Dis. 2019, 32, 372–379. [Google Scholar] [CrossRef]
- Lu, J.; Gu, J.; Li, K.; Xu, C.; Su, W.; Lai, Z.; Zhou, D.; Yu, C.; Xu, B.; Yang, Z. Covid-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerging Infect. Dis. 2020, 26, 2789–2791. [Google Scholar] [CrossRef]
- Liu, Y.; Ning, Z.; Chen, Y.; Guo, M.; Liu, Y.; Gali, N.K.; Sun, L.; Duan, Y.; Cai, J.; Westerdahl, D.; et al. Aerodynamics of SARS-COV-2 in two Wuhan hospitals. Nature 2020, 528, 557–560. [Google Scholar] [CrossRef]
- Correia, G.; Rodrigues, L.; Gameiro da Silva, M.; Goncalves, T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-COV-2 transmission. Med. Hypotheses. 2020, 141. [Google Scholar] [CrossRef]
- Ong, S.W.X.; Tan, Y.K.; Chia, P.Y.; Lee, T.H.; Ng, O.T.; Wong, M.S.Y.; Marimuthu, K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 1 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020, 323, 1610–1612. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Chughtai, A.A. A rapid systemic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, health workers and sick patients. Intl. J. Nurs. Stud. 2020, 108. [Google Scholar] [CrossRef]
- Yoo, J.-H. Review of disinfection and sterilization—Back to the basics. Infect. Chemother. 2018, 50, 101–109. [Google Scholar] [CrossRef]
- Falagas, M.E.; Thomaidis, P.C.; Kotsanis, I.K.; Sgouros, K.; Samonis, G.; Karageorgopoulos, D.E. Airborne hydrogen peroxide for disinfection of the hospital environment and infection control: A systematic review. J. Hosp. Infect. 2011, 78, 171–177. [Google Scholar] [CrossRef]
- Wallace, C.A. New developments in disinfection and sterilization. Am. J. Infect. Control 2016, 44, e23–e27. [Google Scholar] [CrossRef] [PubMed]
- Havelaar, A.H.; van Olphen, M.; Drost, Y.C. F-specific RNA bacteriophages are adequate model organisms for enteric viruses in fresh water. Appl. Environ. Microbiol. 1993, 59, 2956–2962. [Google Scholar] [CrossRef] [PubMed]
- Shields, P.A.; Farrah, S.R. Characterization of virus adsorption by using DEAE-sepharose and octyl-sepharoser. Appl. Environ. Microbiol. 2002, 68, 3965–3968. [Google Scholar] [CrossRef] [PubMed]
- Drier, J.; Stormer, M.; Kleesiek, K. Use of bacteriophage MS2 as an internal control in virus reverse transcription-PCR assays. J. Clin. Microbiol. 2005, 43, 4551–4557. [Google Scholar] [CrossRef] [PubMed]
- Mittal, H.; Parks, S.R.; Pottage, T.; Walker, J.T.; Bennett, A.M. Survival of microorganisms on HEPA filters. Appl. Biosaf. 2011, 16, 163–166. [Google Scholar] [CrossRef]
- Versoza, M.; Jung, W.; Barabad, M.L.; Lee, Y.; Choi, K.; Park, D. Inactivation of filter bound aerosolized MS2 bacteriophages using non-conductive ultrasound transducer. J. Virol. Methods. 2018, 255, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.; Roh, J.; Park, W.M. Comparison of the relative performance efficiencies of melt-blown and glass fiber filter media for managing fine particles. Aerosol. Sci. Technol. 2018, 52, 451–458. [Google Scholar] [CrossRef]
- Dembinski, J.L.; Hungnes, O.; Hauge, A.G.; Kristoffersen, A.C.; Haneberg, B.; Mjaaland, S. Hydrogen peroxide inactivation of influenza virus preserves antigenic structure and immunogenicity. J. Virol. Methods. 2014, 207, 232–237. [Google Scholar] [CrossRef]
- Hole, K.; Ahmadpour, F.; Krishnan, J.; Stansfield, C.; Copps, J.; Nfon, C. Efficacy of accelerated hydrogen peroxide disinfectant on foot-and-mouth disease virus, swine vesicular disease virus and Senecarvirus A. J. Appl. Microbiol. 2016, 122, 634–639. [Google Scholar] [CrossRef]
- Holtkamp, D.J.; Myers, J.; Thomas, P.R.; Karriker, L.A.; Ramirez, A.; Zhang, J.; Wang, C. Efficiency of an accelerated hydrogen peroxide disinfectant to inactivate porcine epidemic diarrhea virus in swine feces on metal surfaces. Can. J. Vet. Res. 2017, 81, 100–107. [Google Scholar] [PubMed]
- Lineback, C.B.; Nkemngong, C.A.; Wu, S.T.; Li, X.; Teska, P.J.; Oliver, H.F. Hydrogen peroxide and sodium hypochlorite disinfectants are more effective against Staphylococcus aureus and Pseudomonas aeruginosa biofilms than quaternary ammonium compounds. Antimicrob. Resist. Infect. Control. 2018, 7, 154. [Google Scholar] [CrossRef]
- Zhou, S.S.; Lukula, S.; Chiossone, C.; Nims, R.W.; Suchmann, D.B.; Ijaz, M.K. Assessment of a respiratory face mask for capturing air pollutants and pathogens including human influenza and rhinoviruses. J. Thorac. Dis. 2018, 10, 2059–2069. [Google Scholar] [CrossRef] [PubMed]
- van der Sande, M.; Teunis, P.; Sabel, R. Professional and home-made mask reduce exposure to respiratory infections among the general population. PLoS ONE 2008, 3, e2618. [Google Scholar] [CrossRef]
- He, X.; Lau, E.H.; Wu, P.; Deng, X.; Wang, J.; Hao, X.; Lau, Y.C.; Wong, J.Y.; Guan, Y.; Tan, X.; et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 2020. [Google Scholar] [CrossRef]
- Hassan, M.A.; Yeom, B.Y.; Wilkie, A.; Pourdeyhimi, B.; Khan, S.A. Fabrication of nanofiber meltblown membranes and their filtration properties. J. Membr. Sci. 2013, 427, 336–344. [Google Scholar] [CrossRef]
- Hyun-tai, S. Elstech Launches Solid Oxygen Mask Pads. Available online: http://n537.ndsoftnews.com/news/articleView.html?idxno=8015 (accessed on 7 September 2020).
- Xia, T.; Yang, M.; Marabella, I.; Lee, E.M.; Olson, B.; Zarling, D.; Torremorell, M.; Clack, H.L. Inactivation of airborne porcine reproductive and respiratory syndrome virus (PRRSv) by packed bed dielectric barrier discharge non-thermal plasma. J. Hazard. Mater. 2020, 393, 122266. [Google Scholar] [CrossRef]
- Eisenlöffel, L.; Reutterm, T.; Horn, M.; Schelegel, S.; Truyen, U.; Speck, S. Impact of UVC-sustained recirculating air filtration on airborne bacteria and dust in a pig facility. PLoS ONE 2019, 14, e225047. [Google Scholar] [CrossRef]

| Filter Type | Density (g/m2) | IE (%) | Diff (Log10PFU/mL) |
|---|---|---|---|
| SOP | 15 | 52.6 ± 1.15% | 0.53 |
| 40 | 93.5 ± 1.06% | 1.32 | |
| 60 | 94.7 ± 0.18% | 1.59 | |
| 100 | 99.4 ± 2.17% | 2.32 | |
| F1 – config. | 60 | 81.8 ± 1.26% | 0.57 |
| F2 – config. | 94.6 ± 2.08% | 1.36 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Versoza, M.; Heo, J.; Ko, S.; Kim, M.; Park, D. Solid Oxygen-Purifying (SOP) Filters: A Self-Disinfecting Filters to Inactivate Aerosolized Viruses. Int. J. Environ. Res. Public Health 2020, 17, 7858. https://doi.org/10.3390/ijerph17217858
Versoza M, Heo J, Ko S, Kim M, Park D. Solid Oxygen-Purifying (SOP) Filters: A Self-Disinfecting Filters to Inactivate Aerosolized Viruses. International Journal of Environmental Research and Public Health. 2020; 17(21):7858. https://doi.org/10.3390/ijerph17217858
Chicago/Turabian StyleVersoza, Michael, Jaeseok Heo, Sangwon Ko, Minjeong Kim, and Duckshin Park. 2020. "Solid Oxygen-Purifying (SOP) Filters: A Self-Disinfecting Filters to Inactivate Aerosolized Viruses" International Journal of Environmental Research and Public Health 17, no. 21: 7858. https://doi.org/10.3390/ijerph17217858
APA StyleVersoza, M., Heo, J., Ko, S., Kim, M., & Park, D. (2020). Solid Oxygen-Purifying (SOP) Filters: A Self-Disinfecting Filters to Inactivate Aerosolized Viruses. International Journal of Environmental Research and Public Health, 17(21), 7858. https://doi.org/10.3390/ijerph17217858