Healthcare and Health Problems from the Perspective of Indigenous Population of the Peruvian Amazon: A Qualitative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
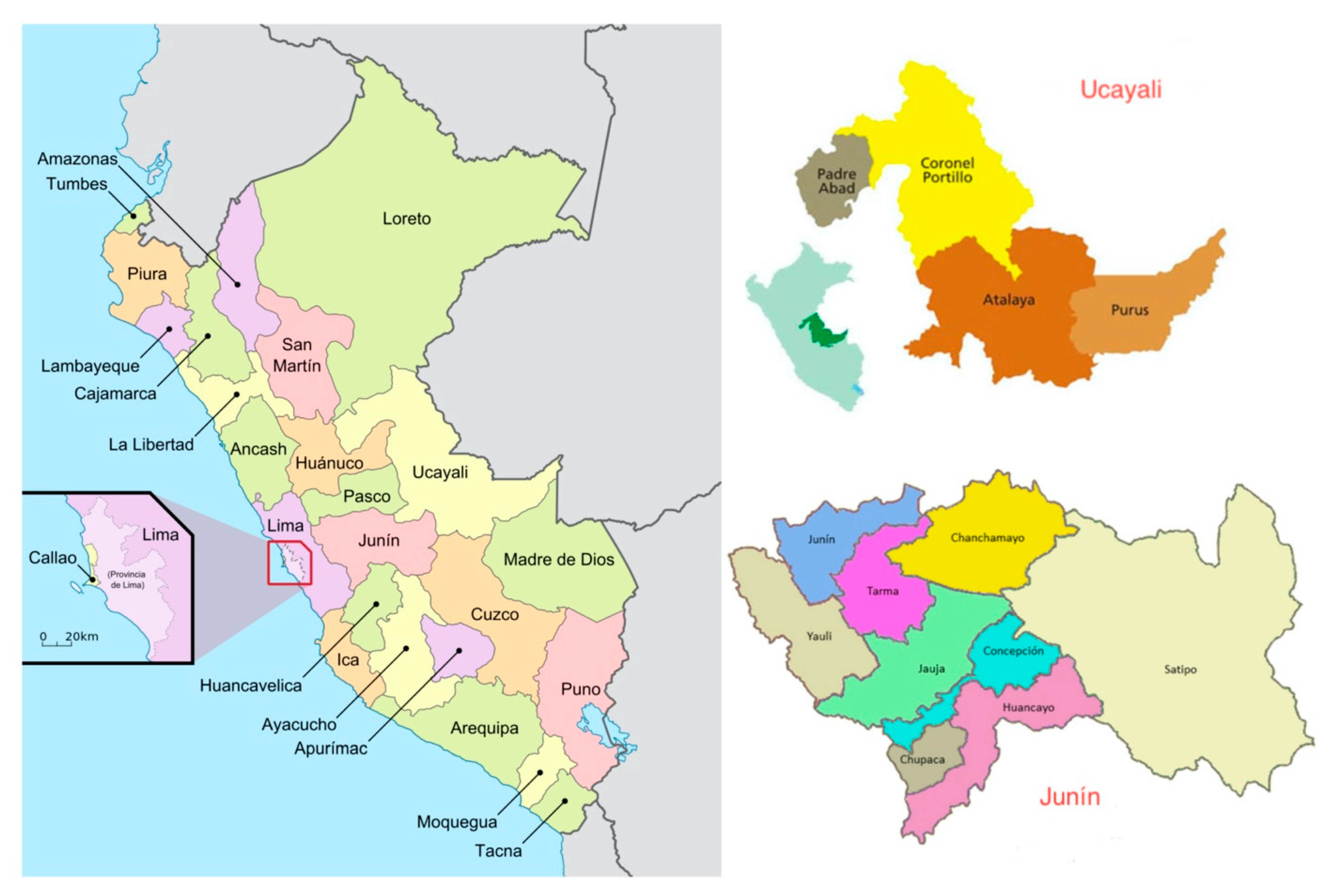
2.2. Population and Setting
2.3. Procedure
2.4. Instrument
2.5. Data Analysis
2.6. Trustworthy
2.7. Ethical Considerations
3. Results
3.1. Health Problems
3.2. Health Practices
3.2.1. Traditional Medicine
Self-Care at Home
Traditional Specialized Care
3.2.2. Official Health System
Use of the Official Health System
Strategies to Enhance Healthcare
Weaknesses/Barriers to Healthcare
4. Discussion
Study Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Instituto Nacional de Estadística e Informática. III Censo de Comunidades Nativas 2017. Resultados definitivos. Tomo II; INEI: Lima, Peru, 2018.
- Vargas-García, S.; Berúmen-Burciaga, L.V.; Arias-Pacheco, I.; Mejia-Mejia, Y.; Realivázquez-Pérez, L.; Portillo-Sánchez, R. Social determinants of community care: Perceptions of the nurse and indigenous Raramuris. CULCyT Cult. Científica Tecnológica 2016, 57, 310–318. [Google Scholar]
- Anderson, I.; Robson, B.; Connolly, M.; Al-Yaman, F.; Bjertness, E.; King, A.; Tynan, M.; Madden, R.; Bang, A.; Coimbra, C.E.A.J.; et al. Indigenous and tribal peoples’ health (The Lancet-Lowitja Institute Global Collaboration): A population study. Lancet 2016, 388, 131–157. [Google Scholar] [CrossRef]
- Díaz, A.; Arana, A.; Vargas-Machuca, R.; Antiporta, D. Health and nutrition of indigenous and nonindigenous children in the Peruvian Amazon. Rev. Panam. Salud Pública 2015, 38, 49–56. [Google Scholar] [PubMed]
- Terán-Hernández, M.; Díaz-Barriga, F.; Cubillas-Tejeda, A.C. Health diagnosis and risk perception: Key elements of a proposed intervention for indigenous communities in Mexico. Rev. Panam. Salud Publica 2016, 39, 106–114. [Google Scholar] [PubMed]
- Bradford, L.E.A.; Okpalauwaekwe, U.; Waldner, C.L.; Bharadwaj, L.A. Drinking water quality in Indigenous communities in Canada and health outcomes: A scoping review. Int. J. Circumpolar Health 2016, 75, 32336. [Google Scholar] [CrossRef] [PubMed]
- Lafontaine, A. Indigenous health disparities: A challenge and an opportunity. Can. J. Surg. 2018, 61, 300–301. [Google Scholar] [CrossRef]
- Schuch, H.S.; Haag, D.G.; Kapellas, K.; Arantes, R.; Peres, M.A.; Thomson, W.M.; Jamieson, L.M. The magnitude of Indigenous and non-Indigenous oral health inequalities in Brazil, New Zealand and Australia. Community Dent. Oral Epidemiol. 2017, 45, 434–441. [Google Scholar] [CrossRef]
- Jauregui, X.; Clavo, Z.M.; Jovel, E.M.; Pardo-de-Santayana, M. “Plantas con madre”: Plants that teach and guide in the shamanic initiation process in the East-Central Peruvian Amazon. J. Ethnopharmacol. 2011, 134, 739–752. [Google Scholar] [CrossRef]
- Fokunang, C.N.; Ndikum, V.; Tabi, O.Y.; Jiofack, R.B.; Ngameni, B.; Guedje, N.M.; Tembe-Fokunang, E.A.; Tomkins, P.; Barkwan, S.; Kechia, F.; et al. Traditional medicine: Past, present and future research and development prospects and integration in the National Health System of Cameroon. Afr. J. Tradit. Complement. Altern. Med. 2011, 8, 284–295. [Google Scholar] [CrossRef]
- Brierley, C.K.; Suarez, N.; Arora, G.; Graham, D. Healthcare access and health beliefs of the indigenous peoples in remote Amazonian Peru. Am. J. Trop. Med. Hyg. 2014, 90, 180–183. [Google Scholar] [CrossRef]
- Cetrángolo, O.; Bertranou, F.; Casanova, L.; Casali, P. EL Sistema de Salud del Perú: Situación Actual y Estrategias Para Orientar la Extensión de la Cobertura Contributiva, 1st ed.; OIT/Oficina de la OIT para los Países Andinos: Lima, Peru, 2013; ISBN 978-92-2-327525-9. [Google Scholar]
- Llanos, R.Q.; Ramirez, R.R.; Palacios, M.T.; Flores, C.F.; Borda-Olivas, A.; Castillo, R.A.; Guanira, J.; Condor, R.S.; Villasante, M.C.; Hurtado-Roca, Y. Health Survey in a Peruvian health system (ENSSA): Design, methodology and general results. Rev. Saude Publica 2019, 53, 33. [Google Scholar] [CrossRef] [PubMed]
- Giovanella, L.; de Almeida, P.F.; Vega Romero, R.; Oliveira, S.; Tejerina Silva, H. Panorama de la Atención Primaria de Salud en Suramérica: Concepciones, componentes y desafíos. Saúde Debate 2015, 39, 300–322. [Google Scholar] [CrossRef]
- Langdon, E.J.; Garnelo, L. Articulation between health services and “indigenous medicine”: Anthropological reflections on policies and reality in Brazil. Salud Colect. 2017, 13, 457–470. [Google Scholar] [CrossRef] [PubMed]
- Gianella, C.; Ugarte-Gil, C.; Caro, G.; Aylas, R.; Castro, C.; Lema, C. TB in Vulnerable Populations: The Case of an Indigenous Community in the Peruvian Amazon. Health Hum. Rights 2016, 18, 55–68. [Google Scholar]
- Roper, J.M.; Shapira, J. Ethnography in Nursing Research; SAGE Publications Inc.: Thousand Oaks, CA, USA; London, UK; New Delhi, India, 2000; ISBN 0-7619-0873-o. [Google Scholar]
- Muecke, M.A. On the Evaluation of Ethnographies; Morse, J.M., Ed.; Sage Publications, Inc.: Thousand Oaks, CA, USA; London, UK; New Delhi, India, 1994; Volume 187, ISBN 0-8039-5042-X. [Google Scholar]
- Espino Delgado, L.M. Mapa Político del Perú: 25 Regiones. Available online: http://auladegeografialm.blogspot.com/2017/05/mapa.html?m=1 (accessed on 17 September 2020).
- Instituto Nacional de Estadística e Informática Región Ucayali. Available online: http://www4.congreso.gob.pe/dgp/didp/boletines/amazonia/UCAYALI/UCAYALI.html (accessed on 17 September 2020).
- FamilySearch Junín, Perú -Genealogía. Available online: https://www.familysearch.org/wiki/es/Junín,_Perú_-_Genealogía (accessed on 17 September 2020).
- Gamlin, J.; Osrin, D. Preventable infant deaths, lone births and lack of registration in Mexican indigenous communities: Health care services and the afterlife of colonialism. Ethn. Health 2018. [Google Scholar] [CrossRef]
- Higginbottom, G.M.A. Sampling issues in qualitative research. Nurse Res. 2004, 12, 7–19. [Google Scholar] [CrossRef]
- Cruz, E.V.; Higginbottom, G. The use of focused ethnography in nursing research. Nurse Res. 2013, 20, 36–43. [Google Scholar] [CrossRef]
- Boulkedid, R.; Abdoul, H.; Loustau, M.; Sibony, O.; Alberti, C. Using and reporting the Delphi method for selecting healthcare quality indicators: A systematic review. PLoS ONE 2011, 6, e20476. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V.; Hayfield, N.; Terry, G. Thematic Analysis BT Handbook of Research Methods in Health Social Sciences; Liamputtong, P., Ed.; Springer: Singapore, 2019; pp. 843–860. ISBN 978-981-10-5251-4. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Rodrigues de Souza Silva, P.; Ignotti, E.; de Oliveira, B.F.A.; Junger, W.L.; Morais, F.; Artaxo, P.; Hacon, S. High risk of respiratory diseases in children in the fire period in Western Amazon. Rev. Saude Publica 2016, 50, 29. [Google Scholar] [CrossRef]
- Cabezas-Sánchez, C.; Trujillo-Villarroel, O.; Zavaleta-Cortijo, C.; Culqui-Lévano, D.; Suarez-Jara, M.; Cueva-Maza, N.; Monzon, S. Prevalence of hepatitis B infection in children under 5 years old on indigenous communities of the Peruvian Amazonia after immunization interventions. Rev. Peru. Med. Exp. Salud Publica 2014, 31, 204–210. [Google Scholar] [PubMed]
- McNally, T.W.; de Wildt, G.; Meza, G.; Wiskin, C.M.D. Improving outcomes for multi-drug-resistant tuberculosis in the Peruvian Amazon—A qualitative study exploring the experiences and perceptions of patients and healthcare professionals. BMC Health Serv. Res. 2019, 19, 594. [Google Scholar] [CrossRef]
- Morocho, A.; Espinoza, I. Acute diarrhea for intestinal parasitosis in children 5 to 10 years old of shuar ethnic in an amazonian indigenous community of Ecuador. Arch. Venez. Farmacol. Ter. 2017, 36, 192–196. [Google Scholar]
- Torres-Slimming, P.A.; Wright, C.; Carcamo, C.P.; Garcia, P.J.; Research Team, I.; Harper, S.L. Achieving the Sustainable Development Goals: A Mixed Methods Study of Health-Related Water, Sanitation, and Hygiene (WASH) for Indigenous Shawi in the Peruvian Amazon. Int. J. Environ. Res. Public Health 2019, 16, 2429. [Google Scholar] [CrossRef]
- Monteban, M.; Yucra Velasquez, V.; Yucra Velasquez, B. Comparing Indigenous and public health infant feeding recommendations in Peru: Opportunities for optimizing intercultural health policies. J. Ethnobiol. Ethnomed. 2018, 14, 69. [Google Scholar] [CrossRef] [PubMed]
- Haque, M.I.; Chowdhury, A.B.M.A.; Shahjahan, M.; Harun, M.G.D. Traditional healing practices in rural Bangladesh: A qualitative investigation. BMC Complement. Altern. Med. 2018, 18, 62. [Google Scholar] [CrossRef]
- Sanz-Biset, J.; Campos-de-la-Cruz, J.; Epiquien-Rivera, M.A.; Canigueral, S. A first survey on the medicinal plants of the Chazuta valley (Peruvian Amazon). J. Ethnopharmacol. 2009, 122, 333–362. [Google Scholar] [CrossRef]
- Luziatelli, G.; Sorensen, M.; Theilade, I.; Molgaard, P. Ashaninka medicinal plants: A case study from the native community of Bajo Quimiriki, Junin, Peru. J. Ethnobiol. Ethnomed. 2010, 6, 21. [Google Scholar] [CrossRef]
- Rojas Rojas, T.; Bourdy, G.; Ruiz, E.; Cerapio, J.-P.; Pineau, P.; Gardon, J.; Doimi, F.; Deparis, X.; Deharo, E.; Bertani, S. Herbal Medicine Practices of Patients With Liver Cancer in Peru: A Comprehensive Study Toward Integrative Cancer Management. Integr. Cancer Ther. 2018, 17, 52–64. [Google Scholar] [CrossRef]
- Yashadhana, A.; Fields, T.; Blitner, G.; Stanley, R.; Zwi, A.B. Trust, culture and communication: Determinants of eye health and care among Indigenous people with diabetes in Australia. BMJ Glob. Health 2020, 5, e001999. [Google Scholar] [CrossRef]
- Lina, A.; González, V. Análisis comparativo de modelos de atención en salud para población indígena en la región Andina TT—Comparative analysis of health care models for indigenous population of the Andean region. Rev. Fac. Nac. Salud Pública 2015, 33, 7–14. [Google Scholar]
- Huicho, L.; Canseco, F.D.; Lema, C.; Miranda, J.J.; Lescano, A.G. Incentives to attract and retain the health workforce in rural areas of Peru: A qualitative study. Cad. Saude Publica 2012, 28, 729–739. [Google Scholar] [CrossRef] [PubMed]
- Palma-Pinedo, H.; Reyes-Vega, M. Barriers For The Quality of Information in Health Facilities of Amazon Region. Rev. Peru. Med. Exp. Salud Publica 2018, 35, 25–31. [Google Scholar] [CrossRef]
- Pelcastre-Villafuerte, B.E.; Meneses-Navarro, S.; Ruelas-Gonzalez, M.G.; Reyes-Morales, H.; Amaya-Castellanos, A.; Taboada, A. Aging in rural, indigenous communities: An intercultural and participatory healthcare approach in Mexico. Ethn. Health 2017, 22, 610–630. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.H.; Subhan, F.B.; Williams, K.; Chan, C.B. Barriers and Mitigating Strategies to Healthcare Access in Indigenous Communities of Canada: A Narrative Review. Healthcare 2020, 8, 112. [Google Scholar] [CrossRef] [PubMed]
| Code | Indigenous *** | Sex | Place of Residence | Social/Labor Profile |
|---|---|---|---|---|
| I-1 | Yes | Woman | Nopoki (Atalaya) | University professor |
| I-2 | Yes | Woman | Shonori | Community leader |
| I-3 | Yes | Woman | Shonori | Healer |
| I-4 | Yes | Woman | Shonori | JASS member * |
| I-5 | Yes | Woman | Quimiriki | Traditional midwife |
| I-6 | Yes | Man | Llaiya | Agricultural Technician |
| I-7 | No | Woman | Llaiya | Doctor |
| I-8 | No | Woman | Llaiya | Pediatrician |
| I-9 | Yes | Woman | Satipo (Junín) | Coordinator of a residence for students |
| I-10 | No | Woman | Huantashiri | Doctor |
| I-11 | Yes | Woman | Huantashiri | CHA ** |
| I-12 | Yes | Woman | San Pedro de Lagarto | Secretary |
| I-13 | No | Man | San Pedro de Lagarto | Priest |
| I-14 | Yes | Man | San Pedro de Lagarto | Project technician |
| I-15 | Yes | Man | San Juan de Cheny | Cocoa producer |
| I-16 | Yes | Man | Maranquiari | Community leader |
| I-17 | Yes | Woman | Maranquiari | CHA ** |
| I-18 | Yes | Woman | Bajo Capiri | Agricultural Technician |
| I-19 | Yes | Man | Bajo Capiri | Community leader |
| I-20 | Yes | Woman | Shintoriato | JASS member * |
| Theme | Category | Subcategory | Description |
|---|---|---|---|
| Health Problems | Health Problems | Diseases diagnosed Signs/symptoms | The health problems reflect alterations of a bio–psychosocial–spiritual nature identified by the indigenous population and health professionals. In addition to signs and symptoms, perceptions of the causes of health problems or certain factors that contribute to perpetuating poor health conditions are also incorporated. |
| Attributed Related Factors | - | ||
| Health Practices | Traditional care | Self-care at home Traditional specialized care | The use of traditional medicine includes all those popular health practices, preventive, curative or palliative derived from beliefs, customs and ancestral knowledge, not associated with the usual practices of care of Westernized health systems. It also includes care providers, either at home or outside, such as specialized health agents (e.g., healer, midwife or huesero *). Health professionals have a perception about the health problems of the indigenous population and their methods of approaching these issues. The official health system uses strategic mechanisms to care for indigenous people and faces weaknesses that make care difficult. |
| Official health system | Use of the official health system Strategies for attention Weaknesses/barriers to healthcare |
| Health Problems | Statements (n) | Attributed Causes/Related Factors |
|---|---|---|
| Respiratory problems | 16 | I-2; indigenous, woman, community leader “We get the flu from people who come from other places, but we don’t take care of ourselves either”. I-4; indigenous, woman, JASS member “When it rains we get wet and because of the distance we have to walk to the post, our body heats up and we get the flu. I was until last week almost 15 days wrong”. I-7; non-indigenous, woman, doctor “We also cannot improve the situation of respiratory infections if we do not have the influenza vaccine for adults”. I-17; indigenous, woman, community health agent “We all needed housing here, when the wind blows strong our entire roof flies and the rain wets our bed”. I-8; non-indigenous, woman, pediatrician “There is quite a lot of overcrowding, they all live together with their little animals inside, they cook with coal and their room is next door. There is no smoke elimination, so that in the long term will affect them with respiratory infections”. |
| Gastrointestinal infections | 15 | I-18; indigenous, woman, agricultural technician “Sometimes we work in the farm with the machete and when we rest we grab our coconut (refered to using the same machete) and of course, this is how gastritis appears”. I-11; indigenous, woman, community health agent “We are improving on not consuming cold water [referred to water without boiling] because it contains several parasites, so sometimes children get sick from the belly”. |
| Malnutrition and childhood anemia | 11 | I-20; indigenous, woman, JASS member “Fish farming is not constant; neither is the daily protein consumption or that of other necessary nutrients habitual”. |
| Musculoskeletal problems | 8 | I-7; non-indigenous, woman, doctor “Due to continuous work in the farms, older patients have muscle contractures and arthralgic problems. I tell them they have to rest but they tell me they can’t because they eat that” (they feed from that). |
| Other health problems | Oral: 4 Ophthalmological: 4 Teenage pregnancies: 7 Injuries, accidents: 5 | I-6; indigenous, man, agricultural technician “Everyone here has teeth problems. The dentist says there are some special toothbrushes for babies, but they cost expensive and we can’t afford it”. I-10; non-indigenous, woman, doctor “I detect quite a lot of cataract problems, because the sun is very strong here and it affects a lot, so I am warning them and they are spreading the word. But when they come I find them wrong because nobody tells you anything, they think it’s normal with age”. I-19; indigenous, woman, JASS member “The last time I went to the doctor was because I cut myself with a knife working on the farm. They had to sew my hand”. |
| Participant (Code) | Verbatim |
|---|---|
| I-11; community health agent | The achiote is very good for the eyes. Recently we had an epidemic of conjunctivitis. You break the seed and put it in a glass of water for 5 min. A drop appears and you must put it in the eye to relieve. With one or two drops is enough”. |
| I-4; JASS member | “With a catawa seed you have enough. The inner part is eaten, about half. You should do it on an empty stomach and, you should drink plenty of lemon water, since you can die from dehydration. It starts to sound and turn the belly and you go to the bathroom with diarrhea expelling the parasites”. |
| I-18; agricultural technician | “Red pinion: one of them is used to heal wounds (the resin) and another is crushed when you have severe headache, the leaves are crushed well and put on as a poultice. And there are also people with beliefs when you have itchy feet, or you get something weird like a tumor and it does not heal with anything ... it also serves as sorcery, but it has to be colored, the white pinion with the green leaves does not work. Be careful because only the sheet is used; The healthy leaf but the seed is poison”. |
| I-12; secretary | I have faith in this plant, it is the piripiri. Sometimes for body aches, internal fever, for the flu, or “mal aire” [evil eye], squeeze the leaves and heat the water, and bathe with it. You have to meet the doses and finish all that pot bathing, 2 or 3 times a day. My children have grown up with this and it is very effective”. |
| I-3; healer | If a snake bites you, you should put on the tear that comes out of the catawa’s bark, also called camana [Asháninka term]. Where you have the scar, you should wash it with that, three times a day, and although it takes about 15 days, in the end it heals. In addition to the tear you can use this remedy also as a bath. |
| I-20; JASS member | I am taking a medicinal herb from the bush to avoid pregnancy. It is a rope that is crushed and boiled and you have to take it after menstruating for three months. And you shouldn’t be close to your husband for it to take effect. If you want another baby, you have to take another herb to end that effect. These herbs are not taken at a young age because it hurts, they are taken from 18–20 years onwards. |
| I-5; traditional midwife | To avoid problems during pregnancy, you cannot eat beef, because the baby will grow too much. To avoid excessive pain in childbirth, we recommend avoiding the consumption of jungle animals. When the woman begins with labor pains, we know how to control it with herbs, and when the baby is born, we give the woman another herb so that the placenta comes out quickly. Everything has a process and must be given at the right time. |
| I-1; university professor | When the child is scared because he has fallen or a dog has attacked him, at night he gets up, his emotional stability is not right. For that the cow horn is used; scratches and dust is thrown into a candle. Smoke is the treatment of the child, who gets on top to receive that smoke or steam. The child is passed two to four times through that candle. You do not need a specialist for this treatment, the mother can do it alone. It doesn’t have much risk, you just have to control the candle well. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Badanta, B.; Lucchetti, G.; Barrientos-Trigo, S.; Fernández-García, E.; Tarriño-Concejero, L.; Vega-Escaño, J.; de Diego-Cordero, R. Healthcare and Health Problems from the Perspective of Indigenous Population of the Peruvian Amazon: A Qualitative Study. Int. J. Environ. Res. Public Health 2020, 17, 7728. https://doi.org/10.3390/ijerph17217728
Badanta B, Lucchetti G, Barrientos-Trigo S, Fernández-García E, Tarriño-Concejero L, Vega-Escaño J, de Diego-Cordero R. Healthcare and Health Problems from the Perspective of Indigenous Population of the Peruvian Amazon: A Qualitative Study. International Journal of Environmental Research and Public Health. 2020; 17(21):7728. https://doi.org/10.3390/ijerph17217728
Chicago/Turabian StyleBadanta, Bárbara, Giancarlo Lucchetti, Sergio Barrientos-Trigo, Elena Fernández-García, Lorena Tarriño-Concejero, Juan Vega-Escaño, and Rocío de Diego-Cordero. 2020. "Healthcare and Health Problems from the Perspective of Indigenous Population of the Peruvian Amazon: A Qualitative Study" International Journal of Environmental Research and Public Health 17, no. 21: 7728. https://doi.org/10.3390/ijerph17217728
APA StyleBadanta, B., Lucchetti, G., Barrientos-Trigo, S., Fernández-García, E., Tarriño-Concejero, L., Vega-Escaño, J., & de Diego-Cordero, R. (2020). Healthcare and Health Problems from the Perspective of Indigenous Population of the Peruvian Amazon: A Qualitative Study. International Journal of Environmental Research and Public Health, 17(21), 7728. https://doi.org/10.3390/ijerph17217728








