Preparedness and Response to the COVID-19 Emergency: Experience from the Teaching Hospital of Pisa, Italy
Abstract
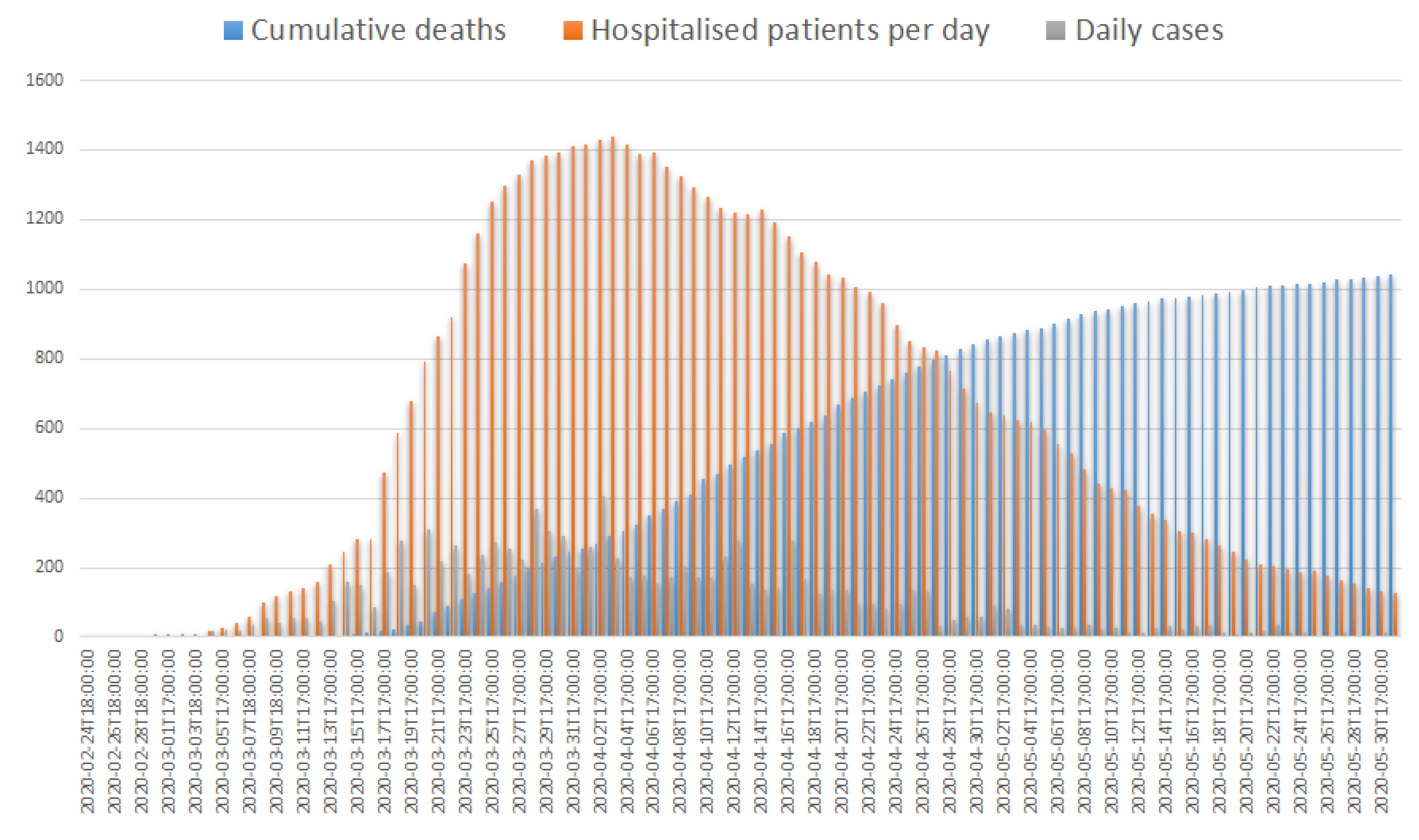
1. Introduction and Epidemiology
2. Regional Management of Pandemic
3. The North-West Area Setting and the Azienda Ospedaliero-Universitaria Pisana Renovation Plan
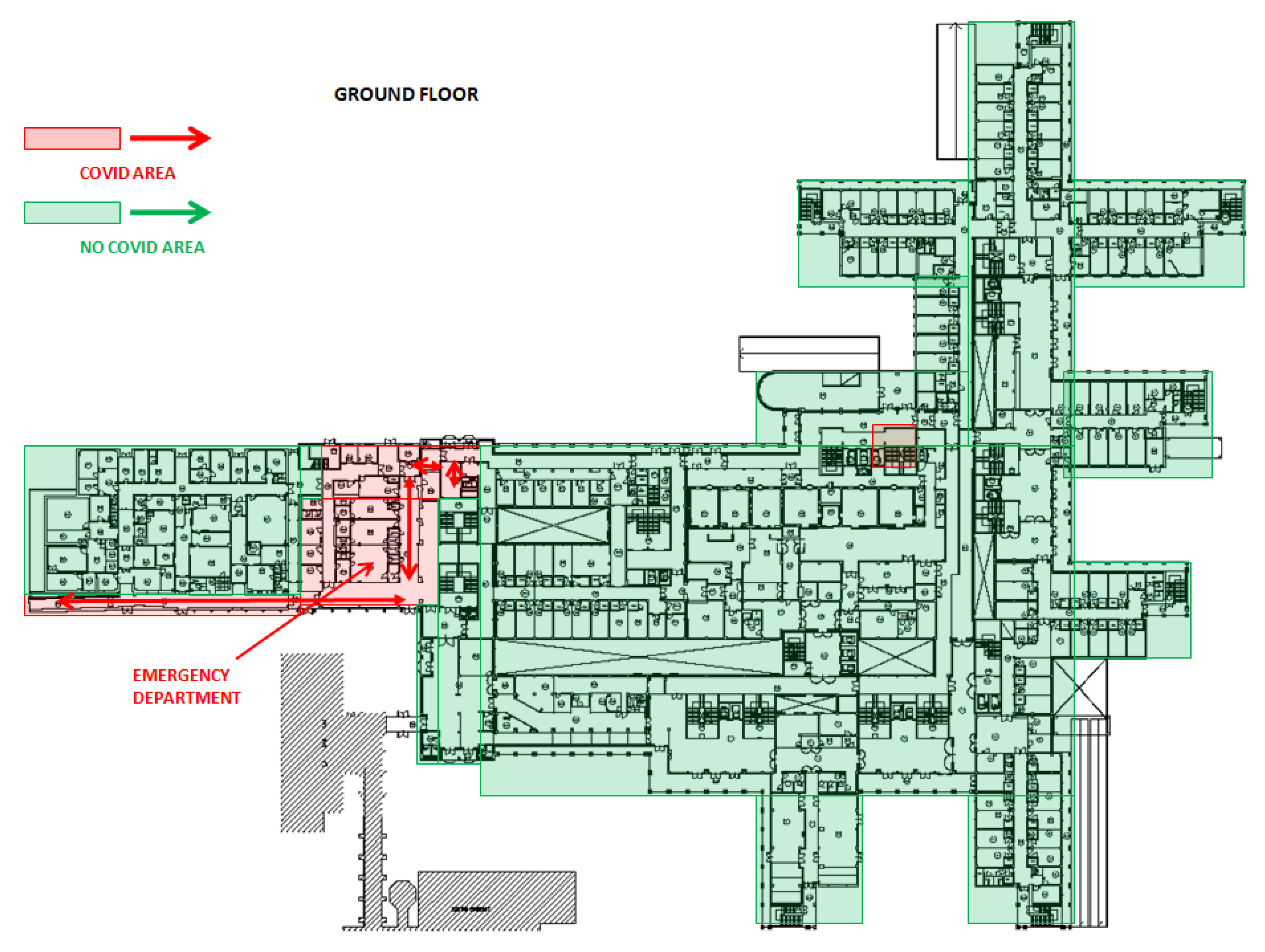
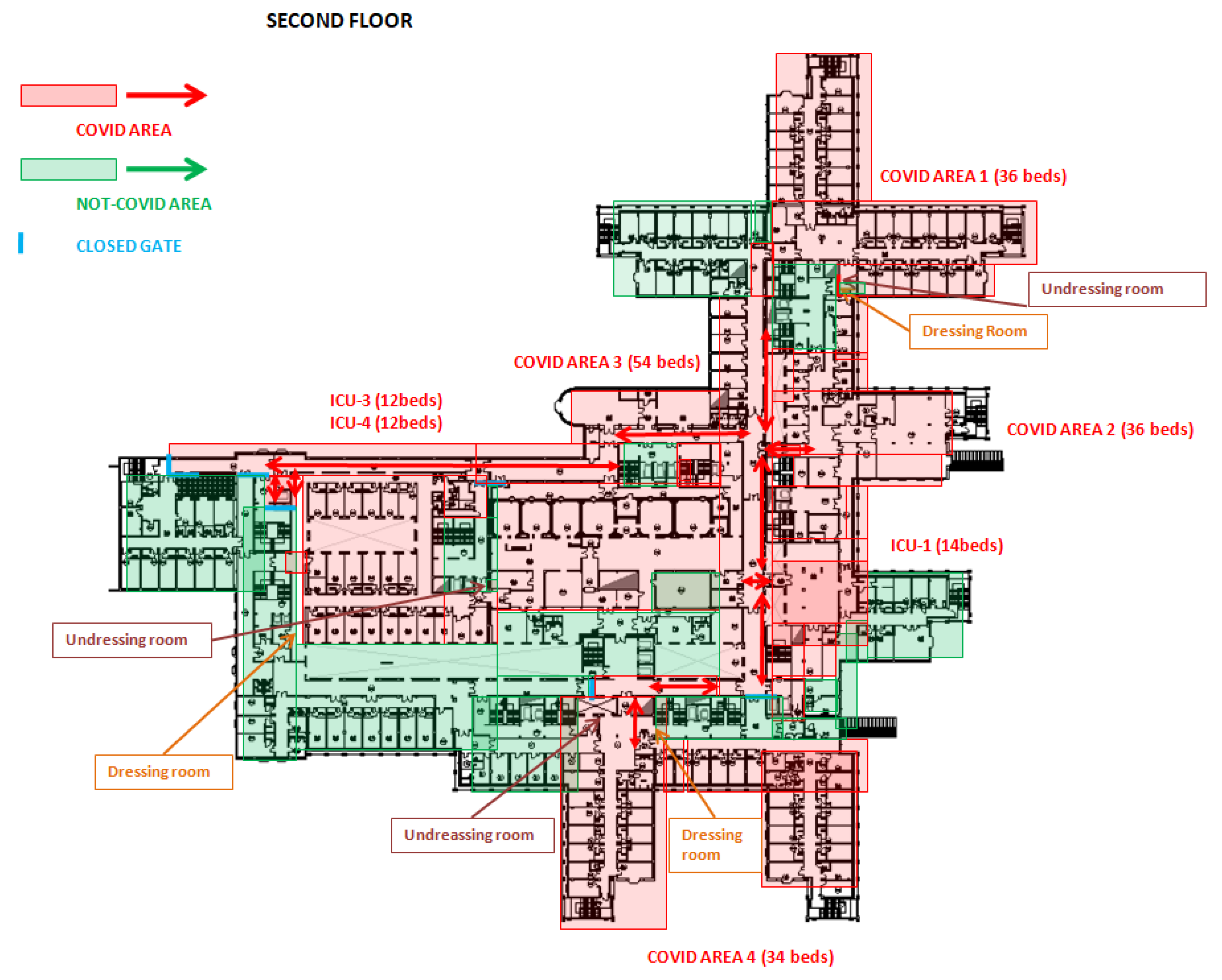
3.1. Reorganization of Hospital Services
3.2. Management of Suspected or Confirmed COVID-19 Patients
3.3. Management of Corpses
3.4. Guidelines for Cleaning and Disinfection
- 70% ethyl alcohol;
- 0.5% hydrogen peroxide;
- sodium hypochlorite (0.1–0.5% free chlorine);
- other disinfectants proved for virucidal activity according to European Standard (EN) 14,476 for medical devices [21].
3.5. Implementation of Cleaning and Disinfection Procedures
3.6. Personal Protective Equipment (PPE)
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Novel Coronavirus (COVID-19) Situation. Available online: https://COVID19.who.int/ (accessed on 15 June 2020).
- Odone, A.; Delmonte, D.; Scognamiglio, T.; Signorelli, C. COVID-19 Deaths in Lombardy, Italy: Data in Context. Lancet Public Health 2020, 5, e315. [Google Scholar] [CrossRef]
- Ministero della Salute. COVID-19, Situation Report Updated at 30 March 2020 18.00. Available online: http://www.salute.gov.it/imgs/C_17_notizie_4362_0_file.pdf (accessed on 9 May 2020).
- Ministero della Salute. Decreto del Presidente del Consiglio dei Ministri 09 Marzo 2020. Available online: http://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=73629 (accessed on 9 May 2020).
- Ministero della Salute. Decreto del Presidente del Consiglio dei Ministri 22 Marzo 2020. Available online: http://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=73729 (accessed on 9 May 2020).
- Toscana Notizie. Coronavirus, I Due Casi Sospetti Ancora in Attesa di Conferma Dall’iss. Available online: https://www.toscana-notizie.it/web/toscana-notizie/-/coronavirus-tutti-i-numeri-e-gli-indirizzi-mail-utili (accessed on 9 May 2020).
- Agenzia di Sanità (ARS) Toscana. Ricostruzione di Scenari Dell’epidemia COVID-19 in Toscana. Available online: https://www.ars.toscana.it/2-articoli/4294-report-ars-toscana-nuovo-coronavirus.html (accessed on 12 August 2020).
- Regione Toscana. Ordinanza del Presidente Della Giunta Regionale N° 7 del 04 Marzo 2020. Available online: https://www.regione.toscana.it/-/ordinanze-della-regione-toscana (accessed on 9 May 2020).
- Agenzia di Sanità (ARS) Toscana. COVID-19 Ricostruzione di Scenari Dell’epidemia in Toscana—Rapporto 24 Luglio 2020. Available online: https://www.ars.toscana.it/images/qualita_cure/coronavirus/rapporti_Covid-19/report_covid19_24_luglio.pdf (accessed on 11 August 2020).
- Regione Toscana. Ordinanza del Presidente della Giunta Regionale N° 20 del 29 Marzo 2020. Available online: https://www.regione.toscana.it/-/ordinanze-della-regione-toscana (accessed on 9 May 2020).
- Regione Toscana. Ordinanza del Presidente della Giunta Regionale N° 18 del 25 Marzo 2020. Available online: https://www.regione.toscana.it/-/ordinanze-della-regione-toscana (accessed on 9 May 2020).
- Regione Toscana Ordinanza del Presidente della Giunta Regionale N° 28 del 07 Aprile 2020. Florence 2020. Available online: https://www.regione.toscana.it/-/ordinanze-della-regione-toscana (accessed on 9 May 2020).
- Baggiani, A.; Briani, S.; Luchini, G.; Giraldi, M.; Martino, M.C.; Porretta, A.; Totaro, M.; Privitera, G. Management of healthcare areas for the prevention of COVID-19 emergency in an Italian teaching hospital (Pisa, Tuscany): A hospital renovation plan. In Infection Control & Hospital Epidemiology; Cambridge University Press: Cambridge, UK, 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Infezione Respiratoria da COVID-19—Documento su Autopsia e Riscontro Diagnostic—COMLAS e SIAPEC-IAP. Available online: https://www.siapec.it/public/uploads/archiviodocumenti/PRD%20COVID-19-9%20rev001%20010420.pdf (accessed on 22 March 2020).
- Circolare del Ministero della Salute, 25/02/2020 protocollo 0005889-25/02/2020. Available online: http://www.salute.gov.it/portale/nuovocoronavirus/archivioNormativaNuovoCoronavirus.jsp?lingua=italiano&testo=&tipologia=CIRCOLARE&giorno=25&mese=02&anno=2020&btnCerca=cerca (accessed on 25 February 2020).
- Istituto Superiore di Sanità. Rapporto ISS COVID-19-n. 1/2020 “Indicazioni ad Interim per L’effettuazione Dell’isolamento e della Assistenza Sanitaria Domiciliare Nell’attuale Contesto COVID-19. Available online: https://www.iss.it/en/rapporti-covid-19 (accessed on 9 May 2020).
- Istituto Superiore di Sanità. Rapporto ISS COVID-19 n. 4/2020 Rev.-Indicazioni ad Interim per la Prevenzione e il Controllo Dell’infezione da SARS-CoV-2 in Strutture Residenziali Sociosanitarie. Available online: https://www.iss.it/en/rapporti-covid-19 (accessed on 9 May 2020).
- Kampf, G.; Todt, D.; Pfaender, S.; Steinmannb, E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020, 104, 246–251. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7132493/ (accessed on 6 February 2020). [CrossRef] [PubMed]
- Ryu, B.H.; Cho, Y.; Cho, O.H.; Hong, S.I.; Kim, S.; Lee, S. Environmental contamination of SARS-CoV-2 during the COVID-19 outbreak in South Korea. Am. J. Infect. Control 2020, 48, 875–879. Available online: https://www.sciencedirect.com/science/article/pii/S0196655320303448 (accessed on 1 August 2020). [CrossRef] [PubMed]
- van Doremalen, N.; Bushmaker, T. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 17, NEJMc2004973. Available online: https://www.nejm.org/doi/full/10.1056/NEJMc2004973 (accessed on 17 March 2020). [CrossRef] [PubMed]
- European Standard EN 14476+A1. Chemical Disinfectants and Antiseptics—Quantitative Suspension Test for the Evaluation of Virucidal Activity in the Medical Area—Test Method and Requirements (Phase 2/Step 1) Pilsen 2019. Available online: http://store.uni.com/catalogo/uni-en-14476-2015 (accessed on 9 May 2020).
- Istituto Superiore di Sanità. Rapporto ISS COVID-19 n. 3/2020 Rev. 2-Indicazioni ad Interim per la Gestione dei Rifiuti Urbani in Relazione Alla Trasmissione Dell’infezione da Virus SARS-COV-2. Available online: https://www.iss.it/en/rapporti-covid-19 (accessed on 15 June 2020).
- World Health Organization. Rational Use of Personal Protective Equipment for Coronavirus Disease (Covid-19) and Considerations during Severe Shortages. Available online: https://apps.who.int/iris/handle/10665/331215?show=full (accessed on 9 May 2020).
- Istituto Superiore di Sanità. Rapporto ISS COVID-19 n. 2/2020 Rev. 2-Indicazioni ad Interim per un Utilizzo Razionale Delle Protezioni per Infezione da SARS-COV-2 Nelle Attività Sanitarie e Sociosanitarie (Assistenza a Soggetti Affetti da COVID-19) Nell’attuale Scenario Emergenziale SARS-COV-2. Available online: https://www.iss.it/en/rapporti-covid-19 (accessed on 15 June 2020).
- BS EN 149:2001 Respiratory Protective Devices. Filtering Half Masks to Protect against Particles. Requirements, Testing, Marking. Available online: https://infostore.saiglobal.com/en-us/Standards/BS-EN-149-2001-279247_SAIG_BSI_BSI_645067/ (accessed on 12 August 2020).
- Ministero della Salute Circolare N. 5443 del 22/02/2020. Polmonite da Nuovo Coronavirus COVID-19—Ulteriori Informazioni e Precauzioni ed Indicazioni Operative su Utilizzo DPI. Available online: http://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2020&codLeg=73195&parte=1%20&serie=null (accessed on 19 August 2020).
- Chung, H.S.; Lee, D.E.; Kim, J.K.; Yeo, I.H.; Kim, C.; Park, J.; Seo, K.S.; Park, S.Y.; Kim, J.H.; Kim, G.; et al. Revised Triage and Surveillance Protocols for Temporary Emergency Department Closures in Tertiary Hospitals as a Response to COVID-19 Crisis in Daegu Metropolitan City. J. Korean Med. Sci. 2020, 35, e189. Available online: https://pubmed.ncbi.nlm.nih.gov/32419401/ (accessed on 18 May 2020). [CrossRef] [PubMed]

| Setting 1—Emergency Department (Pre-Triage Area—Emergency Room—Diagnostic Radiology) All Patients Have Surgical Mask | |||||||
| Location | Activity | Surgical Mask | FFP2/FFP3 Mask | Eye Protection | Gown | Gloves | Overshoes and Hair Cap |
| Pre-Triage Area | Pre-Triage | X | X | 1 pair | |||
| Not-COVID Area | Triage, Healthcare, Cleaning, Reception | X | X | 1 pair | |||
| COVID Area | Swabbing, Healthcare, Cleaning | X | X | X | 2 pair | X | |
| Setting 2—Medical Stays All Patients Have Surgical Mask | |||||||
| Location | Activity | Surgical Mask | FFP2/FFP3 Mask | Eye Protection | Gown | Gloves | Overshoes and Hair Cap |
| Not-COVID Area | Healthcare, Swabbing, Cleaning | X | X(swabbing) | X(swabbing) | X | 1 pair | X |
| COVID Area | Healthcare, Swabbing, Cleaning | X | X | X | 2 pair | X | |
| Setting 3—Operating Rooms All Patients Have Surgical Mask | |||||||
| Location | Activity | Surgical Mask | FFP2/FFP3 Mask | Eye Protection | Gown | Gloves | Overshoes and Hair Cap |
| Not-COVID Area | Patient Entrance, Intubation and Intervention, Cleaning | X | X | 1 pair | X | ||
| COVID Area | Patient Entrance, Intubation and Intervention, Cleaning | X | X | X | 2 pair | X | |
| Setting 4—Delivery Area All Patients Have Surgical Mask | |||||||
| Location | Activity | Surgical Mask | FFP2/FFP3 Mask | Eye Protection | Gown | Gloves | Overshoes and Hair Cap |
| Not-COVID Area | Patient Entrance, Delivery, Cleaning | X | X | 1 pair | X | ||
| COVID Area | Patient Entrance, Delivery, Cleaning | X | X | X | 2 pair | X | |
| Setting 5—Mortuary All Patients Have Surgical Mask | |||||||
| Location | Activity | Surgical Mask | FFP2/FFP3 Mask | Eye Protection | Gown | Gloves | Overshoes and Hair Cap |
| Death in Not-COVID Area | Assistance, Transport, Cleaning | X | X | 1 pair | |||
| Death in COVID Area | Assistance, Transport, Cleaning | X | X | 2 pair | X | ||
| Necropsy Area for COVID Dead Body | Necropsy | X | X | x | 2 pair | X | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baggiani, A.; Briani, S.; Luchini, G.; Giraldi, M.; Milli, C.; Cristaudo, A.; Trillini, L.; Rossi, L.; Gaffi, S.; Ceccanti, G.; et al. Preparedness and Response to the COVID-19 Emergency: Experience from the Teaching Hospital of Pisa, Italy. Int. J. Environ. Res. Public Health 2020, 17, 7376. https://doi.org/10.3390/ijerph17207376
Baggiani A, Briani S, Luchini G, Giraldi M, Milli C, Cristaudo A, Trillini L, Rossi L, Gaffi S, Ceccanti G, et al. Preparedness and Response to the COVID-19 Emergency: Experience from the Teaching Hospital of Pisa, Italy. International Journal of Environmental Research and Public Health. 2020; 17(20):7376. https://doi.org/10.3390/ijerph17207376
Chicago/Turabian StyleBaggiani, Angelo, Silvia Briani, Grazia Luchini, Mauro Giraldi, Carlo Milli, Alfonso Cristaudo, Lucia Trillini, Lorenzo Rossi, Stefano Gaffi, Giovanni Ceccanti, and et al. 2020. "Preparedness and Response to the COVID-19 Emergency: Experience from the Teaching Hospital of Pisa, Italy" International Journal of Environmental Research and Public Health 17, no. 20: 7376. https://doi.org/10.3390/ijerph17207376
APA StyleBaggiani, A., Briani, S., Luchini, G., Giraldi, M., Milli, C., Cristaudo, A., Trillini, L., Rossi, L., Gaffi, S., Ceccanti, G., Martino, M. C., Marchetti, F., Pardi, M., Escati, F., Scateni, M., Frangioni, S., Ciucci, A., Arzilli, G., Sironi, D., ... Privitera, G. P. (2020). Preparedness and Response to the COVID-19 Emergency: Experience from the Teaching Hospital of Pisa, Italy. International Journal of Environmental Research and Public Health, 17(20), 7376. https://doi.org/10.3390/ijerph17207376






