Assessment of the Risk of Oral Cancer Incidence in A High-Risk Population and Establishment of A Predictive Model for Oral Cancer Incidence Using A Population-Based Cohort in Taiwan
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Data Sources
2.3. Definition of Variables
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO Cancer Prevention. Available online: https://www.who.int/cancer/prevention/diagnosis-screening/oral-cancer/en/ (accessed on 20 January 2020).
- WHO Global Oral Health Programme. Available online: https://www.who.int/oral_health/objectives/en/ (accessed on 20 January 2020).
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Today; International Agency for Research on Cancer: Lyon, France, 2018. [Google Scholar]
- Oral Health Country Area Profile Project. Available online: https://capp.mau.se/oral-diseases/ (accessed on 20 January 2020).
- Chaturvedi, A.K.; Anderson, W.F.; Lortet-Tieulent, J.; Curado, M.P.; Ferlay, J.; Franceschi, S.; Rosenberg, P.S.; Bray, F.; Gillison, M.L. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J. Clin. Oncol. 2013, 31, 4550–4559. [Google Scholar] [CrossRef] [PubMed]
- Cancer Registry Annual Report, 2016 (Taiwan). Available online: https://www.hpa.gov.tw/Pages/ashx/File.ashx?FilePath=~/File/Attach/10232/File_11658.pdf (accessed on 20 January 2020).
- Baber, H.; Maqsood, S.; Soomro, M.; Ansari, Z.; Memon, M. Areca Nut Chewing—An Insight. J. Fundam. Appl. Sci. 2017, 9, 1771–1778. [Google Scholar] [CrossRef]
- Gupta, V.; Peterson, C.B.; Dice, L.T.; Uchiki, T.; Racca, J.; Guo, J.T.; Xu, Y.; Hettich, R.; Zhao, X.; Rothstein, R.; et al. Sml1p is a dimer in solution: Characterization of denaturation and renaturation of recombinant Sml1p. Biochemistry 2004, 43, 8568–8578. [Google Scholar] [CrossRef] [PubMed]
- Vanunu, O.; Magger, O.; Ruppin, E.; Shlomi, T.; Sharan, R. Associating genes and protein complexes with disease via network propagation. PLoS Comput. Biol. 2010, 6, e1000641. [Google Scholar] [CrossRef]
- Khawaja, M.R.; Mazahir, S.; Majeed, A.; Malik, F.; Merchant, K.A.; Maqsood, M.; Malik, R.; Ghaffar, S.; Fatmi, Z. Chewing of betel, areca and tobacco: Perceptions and knowledge regarding their role in head and neck cancers in an urban squatter settlement in Pakistan. Asian Pac. J. Cancer Prev. APJCP 2006, 7, 95–100. [Google Scholar]
- Auluck, A.; Hislop, G.; Bajdik, C. Gender-and ethnicity-specific survival trends of oral cavity and oropharyngeal cancers in British Columbia. Cancer Causes Control 2012, 23, 1899–1909. [Google Scholar] [CrossRef]
- Taj, F.; Tanwir, M.; Aly, Z.; Khowajah, A.A.; Tariq, A.; Syed, F.K.; Waqar, F.; Shahzada, K. Factors associated with non-adherence among psychiatric patients at a tertiary care hospital, Karachi, Pakistan: A questionnaire based cross-sectional study. J. Pak. Med Assoc. 2008, 58, 432–436. [Google Scholar]
- Guo, S.-E.; Huang, T.-J.; Huang, J.-C.; Lin, M.-S.; Hong, R.-M.; Chang, C.-H.; Chen, M.-Y. Alcohol, betel-nut and cigarette consumption are negatively associated with health promoting behaviors in Taiwan: A cross-sectional study. BMC Public Health 2013, 13, 257. [Google Scholar] [CrossRef]
- De Menezes, R.F.; Bergmann, A.; Thuler, L.C.S. Alcohol consumption and risk of cancer: A systematic literature review. Asian Pac. J. Cancer Prev. 2013, 14, 4965–4972. [Google Scholar] [CrossRef]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans; World Health Organization; International Agency for Research on Cancer. Tobacco Smoke and Involuntary Smoking; IARC: Lyon, France, 2004; Volume 83. [Google Scholar]
- Siegel, R.; Naishadham, D.; Jemal, A. Cancer statistics, 2013. CA Cancer J. Clin. 2013, 63, 11–30. [Google Scholar] [CrossRef]
- Clapp, R.W.; Jacobs, M.M.; Loechler, E.L. Environmental and occupational causes of cancer: New evidence 2005–2007. Rev. Environ. Health 2008, 23, 1–38. [Google Scholar] [CrossRef] [PubMed]
- Znaor, A.; Brennan, P.; Gajalakshmi, V.; Mathew, A.; Shanta, V.; Varghese, C.; Boffetta, P. Independent and combined effects of tobacco smoking, chewing and alcohol drinking on the risk of oral, pharyngeal and esophageal cancers in Indian men. Int. J. Cancer 2003, 105, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; AlMazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Mariola, W.; Sebastian, R.; Mateusz, S.; Jacek, K.; Leszek, Z.; Ewa, K.; Jacek, Z.; Andrzej, R.; Wojciech, M.; Krzysztof, B. Lymphocyte-to-monocyte ratio (LMR) is prognostic factor for selection of neoadjuvant treatment in locally advanced rectal cancer patients: Sub-set analysis of Polish-2 study. Ann. Oncol. 2017, 28, 124–125. [Google Scholar]
- Stepanov, I.; Carmella, S.G.; Briggs, A.; Hertsgaard, L.; Lindgren, B.; Hatsukami, D.; Hecht, S.S. Presence of the carcinogen N′-nitrosonornicotine in the urine of some users of oral nicotine replacement therapy products. Cancer Res. 2009, 69, 8236–8240. [Google Scholar] [CrossRef] [PubMed]
- Warnakulasuriya, S. Causes of oral cancer—an appraisal of controversies. Br. Dent. J. 2009, 207, 471–475. [Google Scholar] [CrossRef]
- Mehrtash, H.; Duncan, K.; Parascandola, M.; David, A.; Gritz, E.R.; Gupta, P.C.; Mehrotra, R.; Nordin, A.S.A.; Pearlman, P.C.; Warnakulasuriya, S. Defining a global research and policy agenda for betel quid and areca nut. Lancet Oncol. 2017, 18, e767–e775. [Google Scholar] [CrossRef]
- Anaya-Saavedra, G.; Ramírez-Amador, V.; Irigoyen-Camacho, M.E.; García-Cuellar, C.M.; Guido-Jiménez, M.; Méndez-Martínez, R.; García-Carrancá, A. High association of human papillomavirus infection with oral cancer: A case-control study. Arch. Med. Res. 2008, 39, 189–197. [Google Scholar] [CrossRef]
- Johnson, N.W.; Warnakulasuriya, S.; Gupta, P.; Dimba, E.; Chindia, M.; Otoh, E.; Sankaranarayanan, R.; Califano, J.; Kowalski, L. Global oral health inequalities in incidence and outcomes for oral cancer: Causes and solutions. Adv. Dent. Res. 2011, 23, 237–246. [Google Scholar] [CrossRef]
- Mehanna, H.; Beech, T.; Nicholson, T.; El-Hariry, I.; McConkey, C.; Paleri, V.; Roberts, S. Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer—systematic review and meta-analysis of trends by time and region. Head Neck 2013, 35, 747–755. [Google Scholar] [CrossRef]
- Meurman, J.H. Infectious and dietary risk factors of oral cancer. Oral Oncol. 2010, 46, 411–413. [Google Scholar] [CrossRef] [PubMed]
- Pintos, J.; Black, M.J.; Sadeghi, N.; Ghadirian, P.; Zeitouni, A.G.; Viscidi, R.P.; Herrero, R.; Coutlée, F.; Franco, E.L. Human papillomavirus infection and oral cancer: A case-control study in Montreal, Canada. Oral Oncol. 2008, 44, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Westra, W.H. The changing face of head and neck cancer in the 21st century: The impact of HPV on the epidemiology and pathology of oral cancer. Head Neck Pathol. 2009, 3, 78. [Google Scholar] [CrossRef] [PubMed]
- Gupta, B.; Kumar, N.; Johnson, N.W. Relationship of lifetime exposure to tobacco, alcohol and second hand tobacco smoke with upper aero-digestive tract cancers in India: A case-control study with a life-course perspective. Asian Pac. J. Cancer Prev. APJCP 2017, 18, 347–356. [Google Scholar]
- Ko, Y.-C.; Huang, Y.-L.; Lee, C.-H.; Chen, M.-J.; Lin, L.-M.; Tsai, C.-C. Betel quid chewing, cigarette smoking and alcohol consumption related to oral cancer in Taiwan. J. Oral Pathol. Med. 1995, 24, 450–453. [Google Scholar] [CrossRef]
- Warnakulasuriya, S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009, 45, 309–316. [Google Scholar] [CrossRef]
- Auluck, A.; Walker, B.B.; Hislop, G.; Lear, S.A.; Schuurman, N.; Rosin, M. Socio-economic deprivation: A significant determinant affecting stage of oral cancer diagnosis and survival. BMC Cancer 2016, 16, 569. [Google Scholar] [CrossRef]
- Brandt, M.J.; IJzerman, H.; Dijksterhuis, A.; Farach, F.J.; Geller, J.; Giner-Sorolla, R.; Grange, J.A.; Perugini, M.; Spies, J.R.; Van’t Veer, A. The replication recipe: What makes for a convincing replication? J. Exp. Soc. Psychol. 2014, 50, 217–224. [Google Scholar] [CrossRef]
- Wong, Y.-K.; Tsai, W.-C.; Lin, J.-C.; Poon, C.-K.; Chao, S.-Y.; Hsiao, Y.-L.; Chan, M.-Y.; Cheng, C.-S.; Wang, C.-C.; Wang, C.-P.; et al. Socio-demographic factors in the prognosis of oral cancer patients. Oral Oncol. 2006, 42, 893–906. [Google Scholar] [CrossRef]
- Hwang, E.; Johnson-Obaseki, S.; McDonald, J.T.; Connell, C.; Corsten, M. Incidence of head and neck cancer and socioeconomic status in Canada from 1992 to 2007. Oral Oncol. 2013, 49, 1072–1079. [Google Scholar] [CrossRef]
- Jemal, A.; Bray, F.; Center, M.M.; Ferlay, J.; Ward, E.; Forman, D. Global cancer statistics. CA Cancer J. Clin. 2011, 61, 69–90. [Google Scholar] [CrossRef] [PubMed]
- Cancer Screening Records. Available online: https://www.mohw.gov.tw/dl-15849-9c79d30d-f44e-4404-b582-124d841279c7.html (accessed on 20 January 2020).
- Cancer Registration Records. Available online: https://www.mohw.gov.tw/dl-16047-58258053-4580-493d-a697-39606fe852b3.html (accessed on 20 January 2020).
- Akhtar, S. Areca nut chewing and esophageal squamous-cell carcinoma risk in Asians: A meta-analysis of case-control studies. Cancer Causes Control 2013, 24, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, S.; Sheikh, A.A.; Qureshi, H.U. Chewing areca nut, betel quid, oral snuff, cigarette smoking and the risk of oesophageal squamous-cell carcinoma in South Asians: A multicentre case–control study. Eur. J. Cancer 2012, 48, 655–661. [Google Scholar] [CrossRef] [PubMed]
- Auluck, A.; Hislop, G.; Poh, C.; Zhang, L.; Rosin, M.P. Areca nut and betel quid chewing among South Asian immigrants to Western countries and its implications for oral cancer screening. Rural Remote Health 2009, 9, 1118. [Google Scholar] [CrossRef] [PubMed]
- Bell, N.J.; Schuurman, N.; Morad, H.S. A small-area population analysis of socioeconomic status and incidence of severe burn/fire-related injury in British Columbia, Canada. Burns 2009, 35, 1133–1141. [Google Scholar] [CrossRef] [PubMed]
- Blot, W.J.; McLaughlin, J.K.; Winn, D.M.; Austin, D.F.; Greenberg, R.S.; Preston-Martin, S.; Bernstein, L.; Schoenberg, J.B.; Stemhagen, A.; Fraumeni, J.F. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1998, 48, 3282–3287. [Google Scholar]
- Booth, C.M.; Li, G.; Zhang-Salomons, J.; Mackillop, W.J. The impact of socioeconomic status on stage of cancer at diagnosis and survival: A population-based study in Ontario, Canada. Cancer 2010, 116, 4160–4167. [Google Scholar] [CrossRef]
- Bunnell, A.; Pettit, N.; Reddout, N.; Sharma, K.; O’Malley, S.; Chino, M.; Kingsley, K. Analysis of primary risk factors for oral cancer from select US states with increasing rates. Tob. Induc. Dis. 2010, 8, 5. [Google Scholar] [CrossRef]
- Chu, K.P.; Shema, S.; Wu, S.; Gomez, S.L.; Chang, E.T.; Le, Q.T. Head and neck cancer-specific survival based on socioeconomic status in Asians and Pacific Islanders. Cancer 2011, 117, 1935–1945. [Google Scholar] [CrossRef]
- Davies, L.; Welch, H.G. Epidemiology of head and neck cancer in the United States. Otolaryngol. Head Neck Surg. 2006, 135, 451–457.e3. [Google Scholar] [CrossRef]
- Johnson, S.; Corsten, M.J.; McDonald, J.T.; Chun, J. Socio-economic factors and stage at presentation of head and neck cancer patients in Ottawa, Canada: A logistic regression analysis. Oral Oncol. 2010, 46, 366–368. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.; McDonald, J.T.; Corsten, M.; Rourke, R. Socio-economic status and head and neck cancer incidence in Canada: A case-control study. Oral Oncol. 2010, 46, 200–203. [Google Scholar] [CrossRef] [PubMed]
- Kister Mateusz, P.; Borowska, K.; Kister Karolina, A.; Wojtowicz, A.; Jodlowska-Jedrych, B. Risks associated with betel quid chewing. Curr. Issues Pharm. Med. Sci. 2017, 30, 24–26. [Google Scholar] [CrossRef]
- McDonald, J.T.; Johnson-Obaseki, S.; Hwang, E.; Connell, C.; Corsten, M. The relationship between survival and socio-economic status for head and neck cancer in Canada. J. Otolaryngol. Head Neck Surg. 2014, 43, 2. [Google Scholar] [CrossRef] [PubMed]
- Muwonge, R.; Ramadas, K.; Sankila, R.; Thara, S.; Thomas, G.; Vinoda, J.; Sankaranarayanan, R. Role of tobacco smoking, chewing and alcohol drinking in the risk of oral cancer in Trivandrum, India: A nested case-control design using incident cancer cases. Oral Oncol. 2008, 44, 446–454. [Google Scholar] [CrossRef]
- Pervez, S.; Abro, B. Oral Cancer and Chewing Habits. In Development of Oral Cancer: Risk Factors and Prevention Strategies; Al Moustafa, A.-E., Ed.; Springer: Cham, Switzerland, 2017; pp. 115–132. [Google Scholar] [CrossRef]
- Petti, S. Lifestyle risk factors for oral cancer. Oral Oncol. 2009, 45, 340–350. [Google Scholar] [CrossRef]
- Sharpe, K.H.; McMahon, A.D.; Raab, G.M.; Brewster, D.H.; Conway, D.I. Association between socioeconomic factors and cancer risk: A population cohort study in Scotland (1991–2006). PLoS ONE 2014, 9, e89513. [Google Scholar] [CrossRef]
- Warnakulasuriya, S. Living with oral cancer: Epidemiology with particular reference to prevalence and life-style changes that influence survival. Oral Oncol. 2010, 46, 407–410. [Google Scholar] [CrossRef]
- Household Registration Records. Available online: https://www.mohw.gov.tw/dl-17770-e13b366b-822c-4324-ba96-a9d76c053c36.html (accessed on 20 January 2020).
- Deyo, R.A.; Cherkin, D.C.; Ciol, M.A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 1992, 45, 613–619. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare, Taiwan. List of Catastrophic Illnesses. Available online: https://www.mohw.gov.tw/dl-16096-1b42448d-3306-4270-acaa-722752d564cb.html (accessed on 20 January 2020).
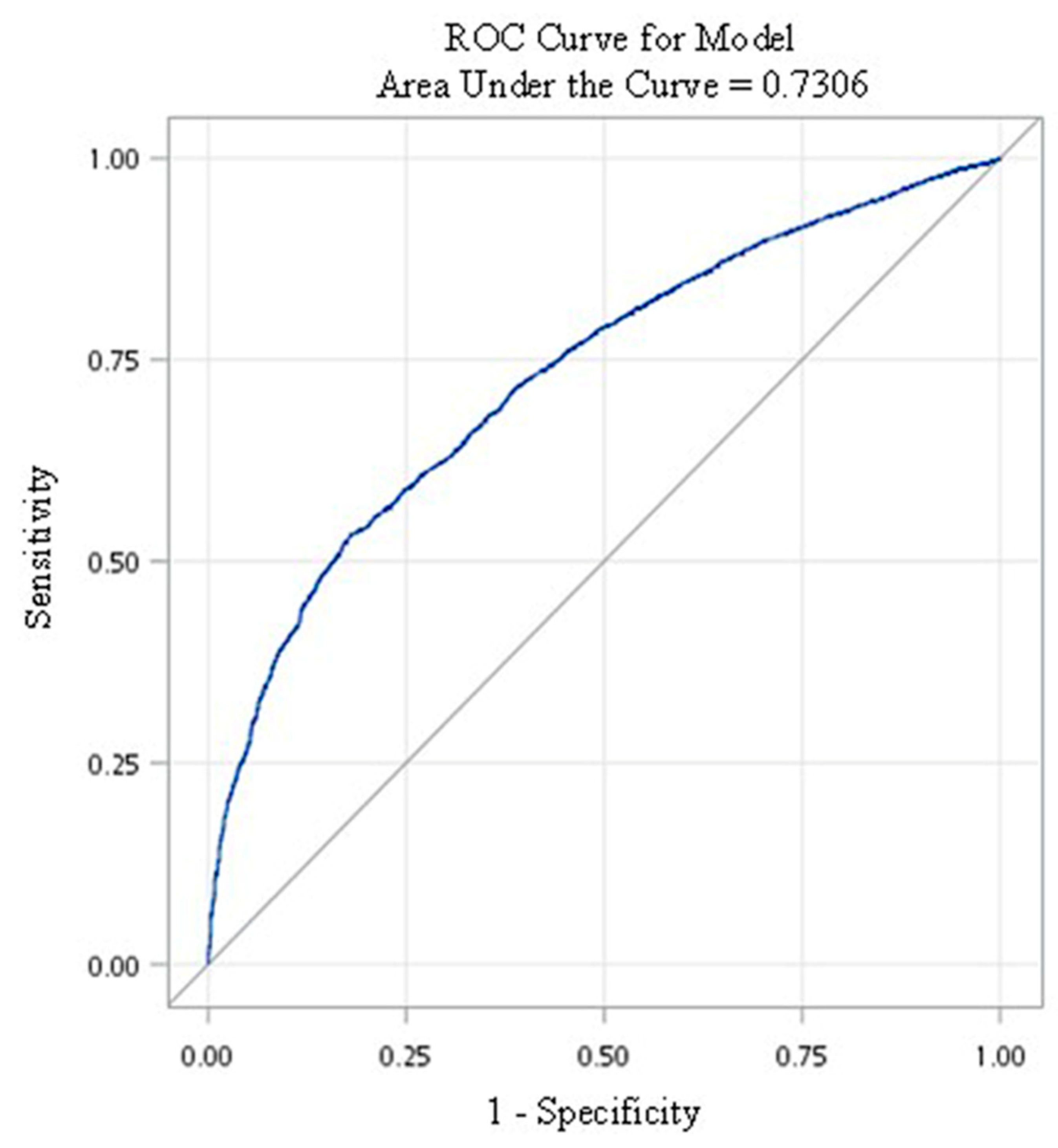
- Kuchibhotla, S.; Vankayalapati, H.; Yalamanchili, B.; Anne, K.R. ROC analysis of class dependent and class independent linear discriminant classifiers using frequency domain features. In Proceedings of the 2014 International Conference on Advances in Computing, Communications and Informatics (ICACCI), New Delhi, India, 24–27 September 2014; pp. 1916–1920. [Google Scholar]
- National Cancer Prevention and Control Program (Third Phase) (Taiwan). Available online: https://www.hpa.gov.tw/Pages/ashx/File.ashx?FilePath=%7E/File/Attach/1094/File_464.pdf (accessed on 20 January 2020).
- Ministry of Health and Welfare, Taiwan. Follow-up Rate for Cases of Positive Results from Oral Cancer Screening, 2018. Available online: https://www.mohw.gov.tw/dl-55653-662d45e6-0fd2-4bdf-8ac3-80968e3f9c4c.html (accessed on 20 January 2020).
- Auluck, A.; Walker, B.B.; Hislop, G.; Lear, S.A.; Schuurman, N.; Rosin, M. Population-based incidence trends of oropharyngeal and oral cavity cancers by sex among the poorest and underprivileged populations. BMC Cancer 2014, 14, 314. [Google Scholar] [CrossRef]
- Adrien, J.; Bertolus, C.; Gambotti, L.; Mallet, A.; Baujat, B. Why are head and neck squamous cell carcinoma diagnosed so late? Influence of health care disparities and socio-economic factors. Oral Oncol. 2014, 50, 94–97. [Google Scholar] [CrossRef]
- Agarwal, A.K.; Sethi, A.; Sareen, D.; Dhingra, S. Treatment delay in oral and oropharyngeal cancer in our population: The role of socio-economic factors and health-seeking behaviour. Indian J. Otolaryngol. Head Neck Surg. 2011, 63, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Gupta, B.; Kumar, N.; Johnson, N.W. A risk factor-based model for upper aerodigestive tract cancers in India: Predicting and validating the receiver operating characteristic curve. J. Oral Pathol. Med. 2017, 46, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Oral Cancer Screening Program (Taiwan). Available online: https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=1100&pid=6461 (accessed on 20 January 2020).
- Petersen, P.E. Strengthening the prevention of oral cancer: The WHO perspective. Community Dent. Oral Epidemiol. 2005, 33, 397–399. [Google Scholar] [PubMed]
- Feu, D.; Miguel, J.A.M.; Celeste, R.K.; Oliveira, B.H. Effect of orthodontic treatment on oral health–related quality of life. Angle Orthod. 2013, 83, 892–898. [Google Scholar] [CrossRef] [PubMed]
| Variable | All Screened Persons | Positive Cases | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | Mean | IDR a | p-Value b | N | n | Mean | IDR a | p-Value b | |
| Total | 1,719,191 | 6275 | 3.80 | 96 | - | 117,697 | 2777 | 3.78 | 624 | - |
| Sex | ||||||||||
| Female | 347,477 | 267 | 3.77 | 20 | - | 8163 | 91 | 3.78 | 295 | - |
| Male | 1,371,714 | 6008 | 3.81 | 115 | <0.001 | 109,534 | 2686 | 3.78 | 649 | <0.001 |
| Age, years | ||||||||||
| <45 | 613,275 | 1306 | 3.85 | 55 | - | 42,531 | 652 | 3.84 | 400 | - |
| 45–54 | 445,594 | 2085 | 3.84 | 122 | <0.001 | 35,937 | 956 | 3.80 | 700 | <0.001 |
| 55–64 | 328,320 | 1757 | 3.81 | 140 | <0.001 | 24,712 | 793 | 3.75 | 855 | <0.001 |
| ≥65 | 332,002 | 1127 | 3.66 | 93 | <0.001 | 14,517 | 376 | 3.62 | 716 | <0.001 |
| Educational level | ||||||||||
| Elementary and below | 399,726 | 1915 | 3.72 | 129 | - | 24,082 | 768 | 3.68 | 866 | - |
| Junior high school | 448,680 | 1987 | 3.82 | 116 | <0.001 | 35,535 | 930 | 3.78 | 692 | <0.001 |
| Senior high school | 561,113 | 1971 | 3.83 | 92 | <0.001 | 43,869 | 912 | 3.81 | 545 | <0.001 |
| Tertiary | 293,723 | 401 | 3.83 | 36 | <0.001 | 13,600 | 166 | 3.85 | 317 | <0.001 |
| Unknown | 15,949 | 1 | 3.93 | 2 | <0.001 | 611 | 1 | 3.93 | 42 | 0.002 |
| Marital status | ||||||||||
| Married | 1,224,584 | 4614 | 3.82 | 99 | - | 83,139 | 2030 | 3.80 | 642 | - |
| Divorced | 176,592 | 869 | 3.78 | 130 | <0.001 | 15,254 | 393 | 3.74 | 688 | 0.222 |
| Widowed | 89,821 | 251 | 3.59 | 78 | <0.001 | 3799 | 90 | 3.56 | 666 | 0.736 |
| Unmarried | 211,957 | 540 | 3.79 | 67 | <0.001 | 14,869 | 263 | 3.76 | 471 | <0.001 |
| Unknown | 16,237 | 1 | 3.93 | 2 | <0.001 | 636 | 1 | 3.92 | 40 | 0.006 |
| Indigenous peoples | ||||||||||
| No | 1,677,465 | 6126 | 3.80 | 96 | - | 114,451 | 2707 | 3.78 | 625 | - |
| Yes | 41,726 | 149 | 3.77 | 95 | 0.865 | 3246 | 70 | 3.69 | 585 | 0.582 |
| Degree of urbanization | ||||||||||
| 1 | 318,859 | 965 | 3.79 | 80 | - | 20,691 | 443 | 3.78 | 566 | - |
| 2 | 424,799 | 1412 | 3.79 | 88 | 0.024 | 28,949 | 652 | 3.78 | 595 | 0.418 |
| 3 | 359,434 | 1303 | 3.81 | 95 | <0.001 | 24,656 | 580 | 3.79 | 621 | 0.147 |
| 4 | 312,636 | 1223 | 3.82 | 102 | <0.001 | 21,004 | 511 | 3.79 | 641 | 0.056 |
| 5 | 61,900 | 293 | 3.80 | 124 | <0.001 | 4174 | 110 | 3.73 | 706 | 0.039 |
| 6 | 129,846 | 573 | 3.82 | 116 | <0.001 | 9090 | 236 | 3.73 | 696 | 0.011 |
| 7 | 111,717 | 506 | 3.79 | 119 | <0.001 | 9133 | 245 | 3.79 | 708 | 0.005 |
| Monthly salary | ||||||||||
| Low income c | 25,565 | 158 | 3.69 | 167 | - | 2160 | 68 | 3.66 | 860 | - |
| <17,280 | 325,769 | 1177 | 3.80 | 95 | <0.001 | 23,243 | 552 | 3.77 | 630 | 0.015 |
| 17,281–22,800 | 638,031 | 2688 | 3.77 | 112 | <0.001 | 45,604 | 1172 | 3.74 | 688 | 0.073 |
| 22,801–28,800 | 135,455 | 565 | 3.82 | 109 | <0.001 | 9616 | 247 | 3.79 | 678 | 0.082 |
| 28,801–36,300 | 168,481 | 608 | 3.83 | 94 | <0.001 | 11,630 | 271 | 3.81 | 612 | 0.012 |
| 36,300–45,800 | 206,153 | 663 | 3.85 | 84 | <0.001 | 14,264 | 303 | 3.85 | 551 | 0.001 |
| ≥45,801 | 219,737 | 416 | 3.85 | 49 | <0.001 | 11,180 | 164 | 3.87 | 379 | <0.001 |
| Health-related behaviors | ||||||||||
| Smoking | 618,732 | 1007 | 3.78 | 43 | - | 23,560 | 316 | 3.76 | 356 | - |
| Betel nut chewing | 119,804 | 354 | 3.75 | 79 | <0.001 | 5204 | 162 | 3.76 | 827 | <0.001 |
| Both | 980,655 | 4914 | 3.82 | 131 | <0.001 | 88,933 | 2299 | 3.79 | 683 | <0.001 |
| Diabetes | ||||||||||
| No | 1,533,980 | 5271 | 3.81 | 90 | - | 101,563 | 2334 | 3.79 | 607 | - |
| Yes | 185,211 | 1004 | 3.72 | 146 | <0.001 | 16,134 | 443 | 3.73 | 735 | <0.001 |
| Other cancers d | ||||||||||
| No | 1,672,783 | 5967 | 3.82 | 93 | - | 114,472 | 2700 | 3.80 | 621 | - |
| Yes | 46,408 | 308 | 3.35 | 198 | <0.001 | 3225 | 77 | 3.20 | 746 | 0.114 |
| CCI | ||||||||||
| 0 | 1,370,338 | 4634 | 3.83 | 88 | - | 90,473 | 2099 | 3.81 | 609 | - |
| 1 | 233,794 | 1012 | 3.76 | 115 | <0.001 | 18,010 | 425 | 3.75 | 629 | 0.551 |
| ≥2 | 115,059 | 629 | 3.53 | 155 | <0.001 | 9214 | 253 | 3.56 | 770 | <0.001 |
| Other catastrophic illnesses e | ||||||||||
| No | 1,657,132 | 5997 | 3.81 | 95 | - | 112,708 | 2660 | 3.79 | 623 | - |
| Yes | 62,059 | 278 | 3.64 | 123 | <0.001 | 4989 | 117 | 3.60 | 651 | 0.645 |
| Variable | No cancer | Cancer | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-Value a | |
| Total | 1,719,191 | 100.00 | 1,712,916 | 99.64 | 6275 | 0.36 | - |
| Sex | <0.001 | ||||||
| Female | 347,477 | 20.21 | 347,210 | 99.92 | 267 | 0.08 | |
| Male | 1,371,714 | 79.79 | 1,365,706 | 99.56 | 6008 | 0.44 | |
| Age, years | <0.001 | ||||||
| <45 | 613,275 | 35.67 | 611,969 | 99.79 | 1306 | 0.21 | |
| 45–54 | 445,594 | 25.92 | 443,509 | 99.53 | 2085 | 0.47 | |
| 55–64 | 328,320 | 19.10 | 326,563 | 99.46 | 1757 | 0.54 | |
| ≥65 | 332,002 | 19.31 | 330,875 | 99.66 | 1127 | 0.34 | |
| Educational level | <0.001 | ||||||
| Elementary and below | 399,726 | 23.25 | 397,811 | 99.52 | 1915 | 0.48 | |
| Junior high school | 448,680 | 26.10 | 446,693 | 99.56 | 1987 | 0.44 | |
| Senior high school | 561,113 | 32.64 | 559,142 | 99.65 | 1971 | 0.35 | |
| Tertiary | 293,723 | 17.08 | 293,322 | 99.86 | 401 | 0.14 | |
| Unknown | 15,949 | 0.93 | 15,948 | 99.99 | 1 | 0.01 | |
| Marital status | <0.001 | ||||||
| Married | 1,224,584 | 71.23 | 1,219,970 | 99.62 | 4614 | 0.38 | |
| Divorce | 176,592 | 10.27 | 175,723 | 99.51 | 869 | 0.49 | |
| Widowed | 89,821 | 5.22 | 89,570 | 99.72 | 251 | 0.28 | |
| Unmarried | 211,957 | 12.33 | 211,417 | 99.75 | 540 | 0.25 | |
| Unknown | 16,237 | 0.94 | 16,236 | 99.99 | 1 | 0.01 | |
| Indigenous peoples | 0.763 | ||||||
| No | 1,677,465 | 97.57 | 1,671,339 | 99.63 | 6126 | 0.37 | |
| Yes | 41,726 | 2.43 | 41,577 | 99.64 | 149 | 0.36 | |
| Degree of urbanization | <0.001 | ||||||
| 1 | 318,859 | 18.55 | 317,894 | 99.70 | 965 | 0.30 | |
| 2 | 424,799 | 24.71 | 423,387 | 99.67 | 1412 | 0.33 | |
| 3 | 359,434 | 20.91 | 358,131 | 99.64 | 1303 | 0.36 | |
| 4 | 312,636 | 18.19 | 311,413 | 99.61 | 1223 | 0.39 | |
| 5 | 61,900 | 3.60 | 61,607 | 99.53 | 293 | 0.47 | |
| 6 | 129,846 | 7.55 | 129,273 | 99.56 | 573 | 0.44 | |
| 7 | 111,717 | 6.50 | 111,211 | 99.55 | 506 | 0.45 | |
| Diabetes | <0.001 | ||||||
| No | 1,533,980 | 89.23 | 1,528,709 | 99.66 | 5271 | 0.34 | |
| Yes | 185,211 | 10.77 | 184,207 | 99.46 | 1004 | 0.54 | |
| Other cancers | <0.001 | ||||||
| No | 1,672,783 | 97.30 | 1,666,816 | 99.64 | 5967 | 0.36 | |
| Yes | 46,408 | 2.70 | 46,100 | 99.34 | 308 | 0.66 | |
| CCI | <0.001 | ||||||
| 0 | 1,370,338 | 79.71 | 1,365,704 | 99.66 | 4634 | 0.34 | |
| 1 | 233,794 | 13.60 | 232,782 | 99.57 | 1012 | 0.43 | |
| ≥2 | 115,059 | 6.69 | 114,430 | 99.45 | 629 | 0.55 | |
| Other catastrophic illnesses | <0.001 | ||||||
| No | 1,657,132 | 96.39 | 1,651,135 | 99.64 | 5997 | 0.36 | |
| Yes | 62,059 | 3.61 | 61,781 | 99.55 | 278 | 0.45 | |
| Health-related behaviors | <0.001 | ||||||
| Smoking | 618,732 | 35.99 | 617,725 | 99.84 | 1007 | 0.16 | |
| Betel nut chewing | 119,804 | 6.97 | 119,450 | 99.70 | 354 | 0.30 | |
| Both | 980,655 | 57.04 | 975,741 | 99.50 | 4914 | 0.50 | |
| Monthly salary | <0.001 | ||||||
| Low income | 25,565 | 1.49 | 25,407 | 99.38 | 158 | 0.62 | |
| <17,280 | 325,769 | 18.95 | 324,592 | 99.64 | 1177 | 0.36 | |
| 17,281–22,800 | 638,031 | 37.11 | 635,343 | 99.58 | 2688 | 0.42 | |
| 22,801–28,800 | 135,455 | 7.88 | 134,890 | 99.58 | 565 | 0.42 | |
| 28,801–36,300 | 168,481 | 9.80 | 167,873 | 99.64 | 608 | 0.36 | |
| 36,300–45,800 | 206,153 | 11.99 | 205,490 | 99.68 | 663 | 0.32 | |
| ≥45,801 | 219,737 | 12.78 | 219,321 | 99.81 | 416 | 0.19 | |
| Sex | Adjusted HR | 95% CI | p-Value a | |
|---|---|---|---|---|
| Female (ref) | - | - | - | - |
| Male | 5.72 | 5.04 | 6.49 | <0.001 |
| Age, years | ||||
| <45 (ref) | - | - | - | - |
| 45–54 | 1.88 | 1.75 | 2.02 | <0.001 |
| 55–64 | 1.93 | 1.77 | 2.09 | <0.001 |
| ≥65 | 1.05 | 0.95 | 1.16 | 0.375 |
| Educational level | ||||
| Elementary and below (ref) | - | - | - | - |
| Junior high school | 0.89 | 0.83 | 0.96 | 0.003 |
| Senior high school | 0.76 | 0.71 | 0.82 | <0.001 |
| Tertiary | 0.37 | 0.33 | 0.42 | <0.001 |
| Unknown | 0.73 | 0.00 | 2597.95 | 0.939 |
| Marital status | ||||
| Married (ref) | - | - | - | - |
| Divorced | 1.35 | 1.25 | 1.45 | <0.001 |
| Widowed | 1.07 | 0.93 | 1.22 | 0.341 |
| Unmarried | 0.86 | 0.79 | 0.95 | 0.003 |
| Unknown | 0.03 | 0.00 | 90.44 | 0.379 |
| Indigenous peoples | ||||
| No (ref) | - | - | - | - |
| Yes | 1.02 | 0.86 | 1.21 | 0.821 |
| Degree of urbanization | ||||
| 1 (ref) | - | - | - | - |
| 2 | 1.04 | 0.96 | 1.13 | 0.335 |
| 3 | 0.97 | 0.89 | 1.05 | 0.454 |
| 4 | 0.92 | 0.85 | 1.01 | 0.068 |
| 5 | 0.96 | 0.84 | 1.10 | 0.552 |
| 6 | 0.97 | 0.87 | 1.08 | 0.620 |
| 7 | 1.00 | 0.89 | 1.11 | 0.956 |
| Monthly salary | ||||
| Low income (ref) | - | - | - | - |
| <17,280 | 0.75 | 0.63 | 0.89 | 0.001 |
| 17,281–22,800 | 0.74 | 0.63 | 0.87 | <0.001 |
| 22,801–28,800 | 0.74 | 0.62 | 0.89 | 0.001 |
| 28,801–36,300 | 0.65 | 0.55 | 0.78 | <0.001 |
| 36,300–45,800 | 0.55 | 0.46 | 0.66 | <0.001 |
| ≥45,801 | 0.44 | 0.37 | 0.54 | <0.001 |
| Health-related behaviors | ||||
| Smoking (ref) | - | - | - | - |
| Betel nut chewing | 2.12 | 1.87 | 2.39 | <0.001 |
| Both | 2.29 | 2.14 | 2.46 | <0.001 |
| Diabetes | ||||
| No (ref) | - | - | - | - |
| Yes | 1.20 | 1.12 | 1.29 | <0.001 |
| Other cancer | ||||
| No (ref) | - | - | - | - |
| Yes | 1.91 | 1.70 | 2.14 | <0.001 |
| CCI | ||||
| 0 (ref) | - | - | - | - |
| 1 | 1.08 | 1.01 | 1.16 | 0.025 |
| ≥2 | 1.27 | 1.16 | 1.39 | <0.001 |
| Other catastrophic illnesses | ||||
| No (ref) | - | - | - | - |
| Yes | 1.06 | 0.94 | 1.20 | 0.352 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, L.-C.; Kung, P.-T.; Lung, C.-H.; Tsai, M.-H.; Liu, S.-A.; Chiu, L.-T.; Huang, K.-H.; Tsai, W.-C. Assessment of the Risk of Oral Cancer Incidence in A High-Risk Population and Establishment of A Predictive Model for Oral Cancer Incidence Using A Population-Based Cohort in Taiwan. Int. J. Environ. Res. Public Health 2020, 17, 665. https://doi.org/10.3390/ijerph17020665
Hung L-C, Kung P-T, Lung C-H, Tsai M-H, Liu S-A, Chiu L-T, Huang K-H, Tsai W-C. Assessment of the Risk of Oral Cancer Incidence in A High-Risk Population and Establishment of A Predictive Model for Oral Cancer Incidence Using A Population-Based Cohort in Taiwan. International Journal of Environmental Research and Public Health. 2020; 17(2):665. https://doi.org/10.3390/ijerph17020665
Chicago/Turabian StyleHung, Li-Chen, Pei-Tseng Kung, Chi-Hsuan Lung, Ming-Hsui Tsai, Shih-An Liu, Li-Ting Chiu, Kuang-Hua Huang, and Wen-Chen Tsai. 2020. "Assessment of the Risk of Oral Cancer Incidence in A High-Risk Population and Establishment of A Predictive Model for Oral Cancer Incidence Using A Population-Based Cohort in Taiwan" International Journal of Environmental Research and Public Health 17, no. 2: 665. https://doi.org/10.3390/ijerph17020665
APA StyleHung, L.-C., Kung, P.-T., Lung, C.-H., Tsai, M.-H., Liu, S.-A., Chiu, L.-T., Huang, K.-H., & Tsai, W.-C. (2020). Assessment of the Risk of Oral Cancer Incidence in A High-Risk Population and Establishment of A Predictive Model for Oral Cancer Incidence Using A Population-Based Cohort in Taiwan. International Journal of Environmental Research and Public Health, 17(2), 665. https://doi.org/10.3390/ijerph17020665





