Eating Out and Consumers’ Health: Evidence on Obesity and Balanced Nutrition Intakes
Abstract
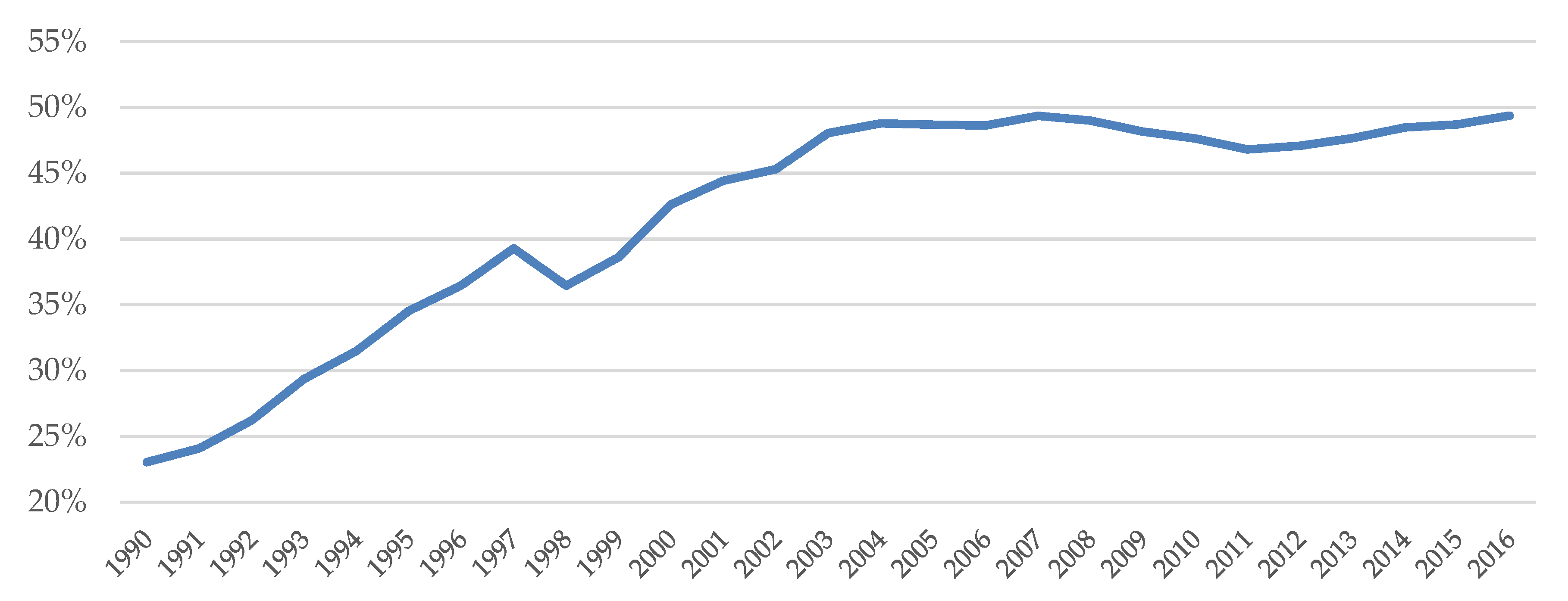
1. Introduction
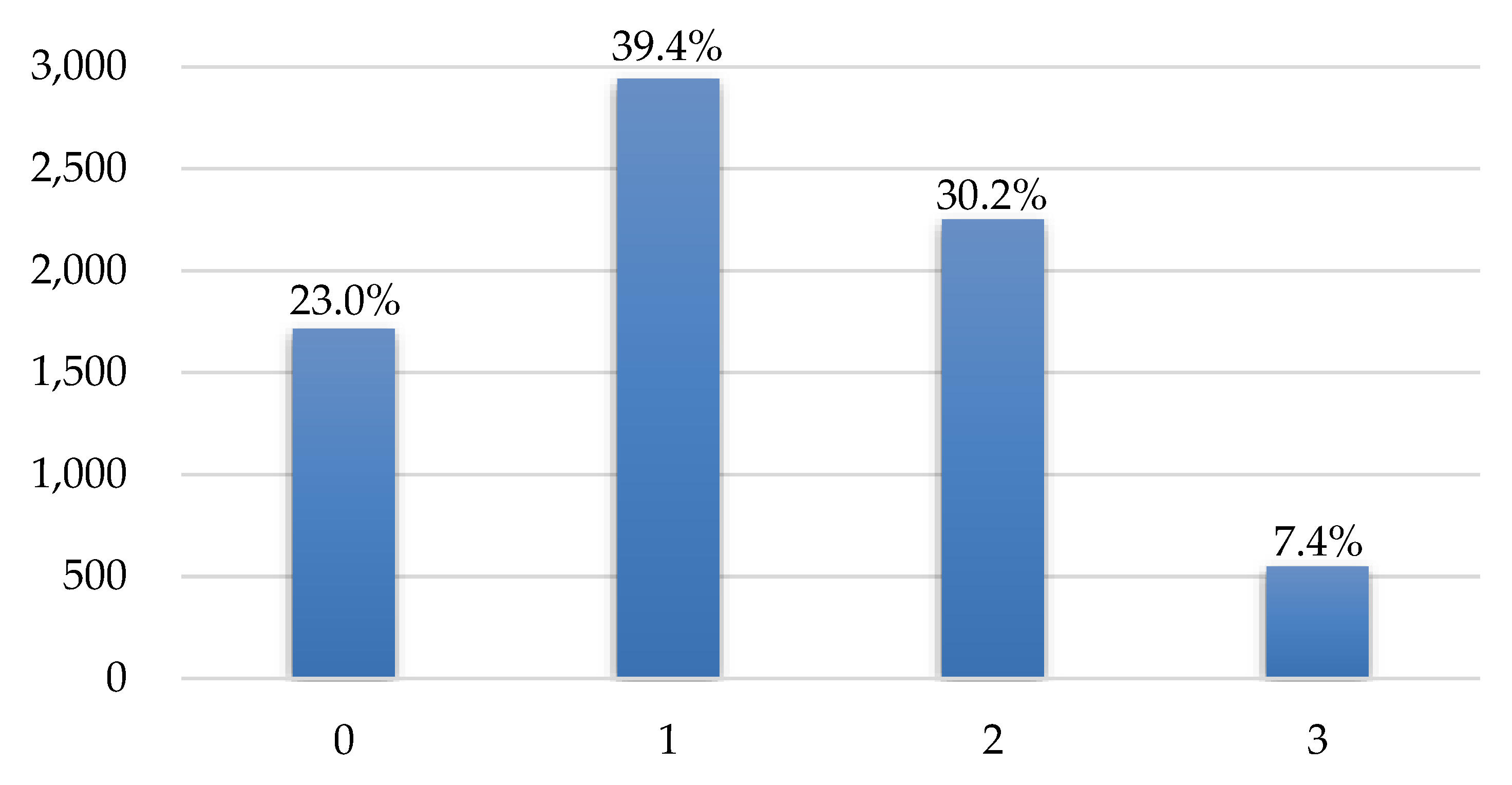
2. Data
3. Methodology
4. Results
4.1. Estimation Results for Treatment Model
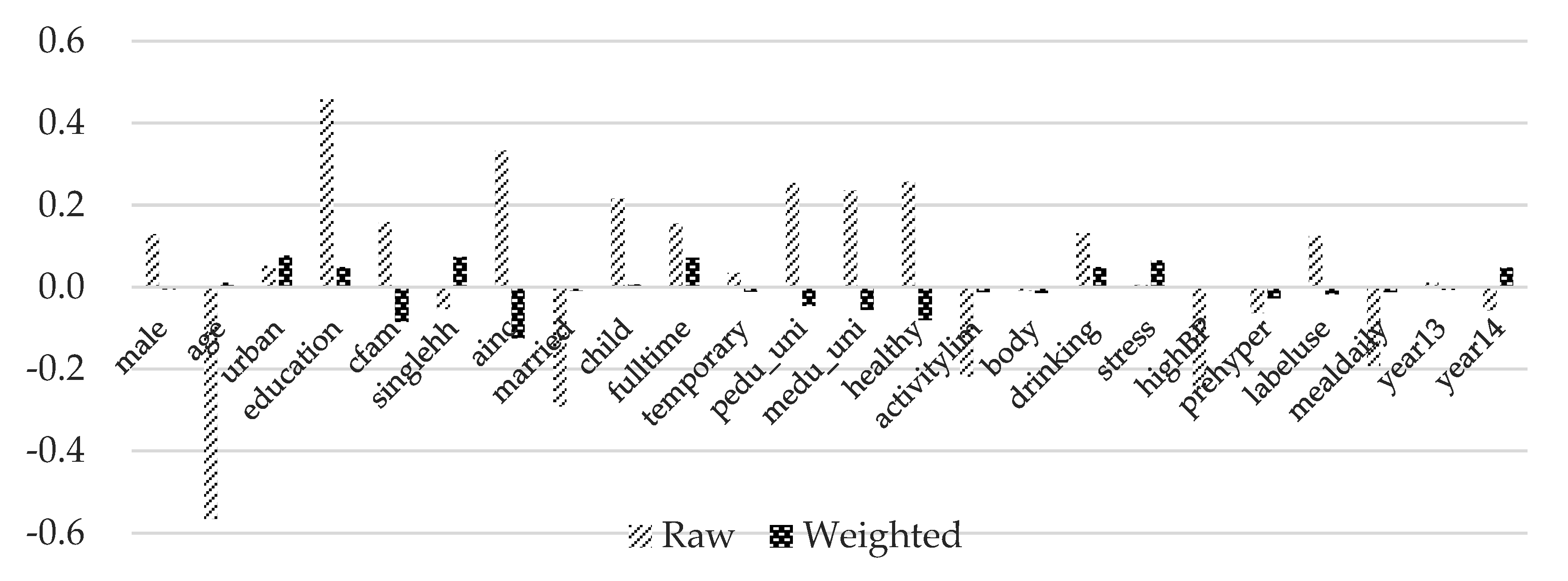
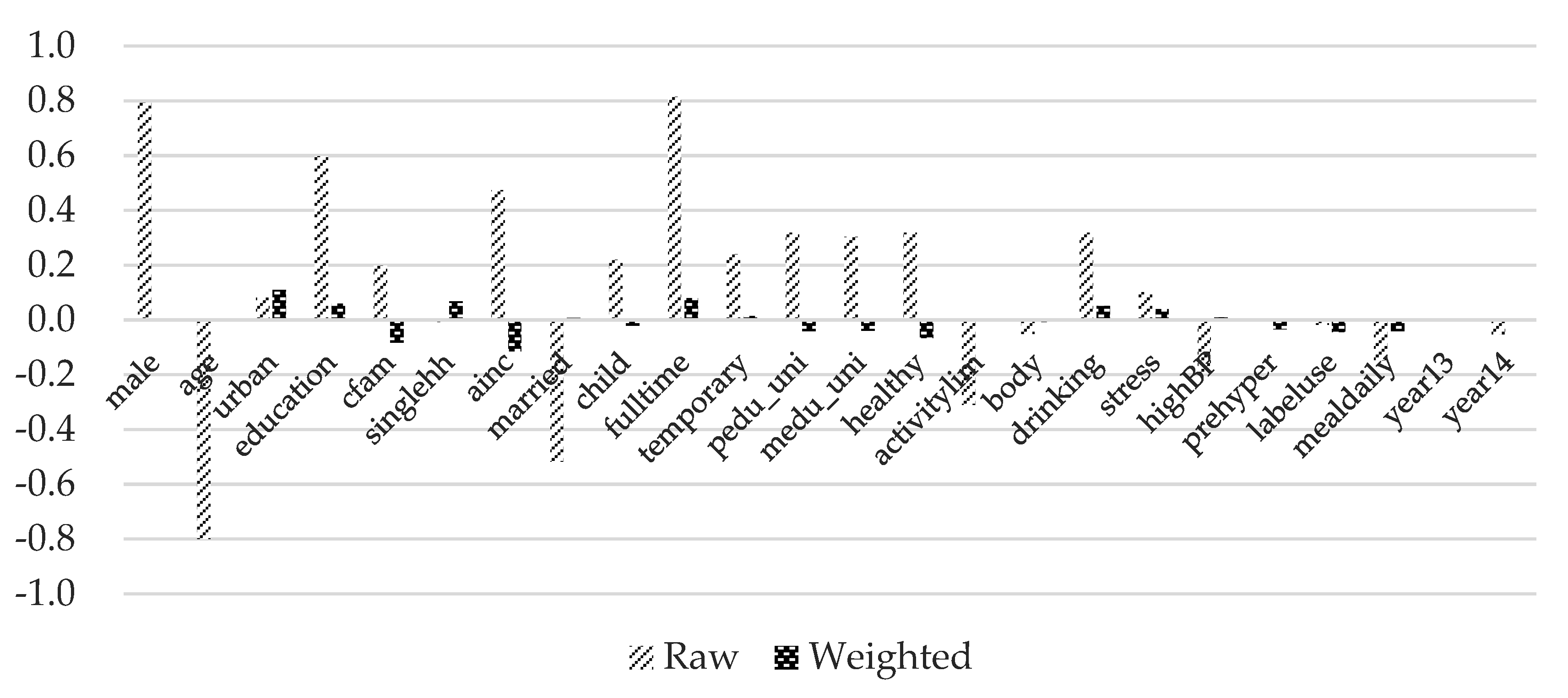
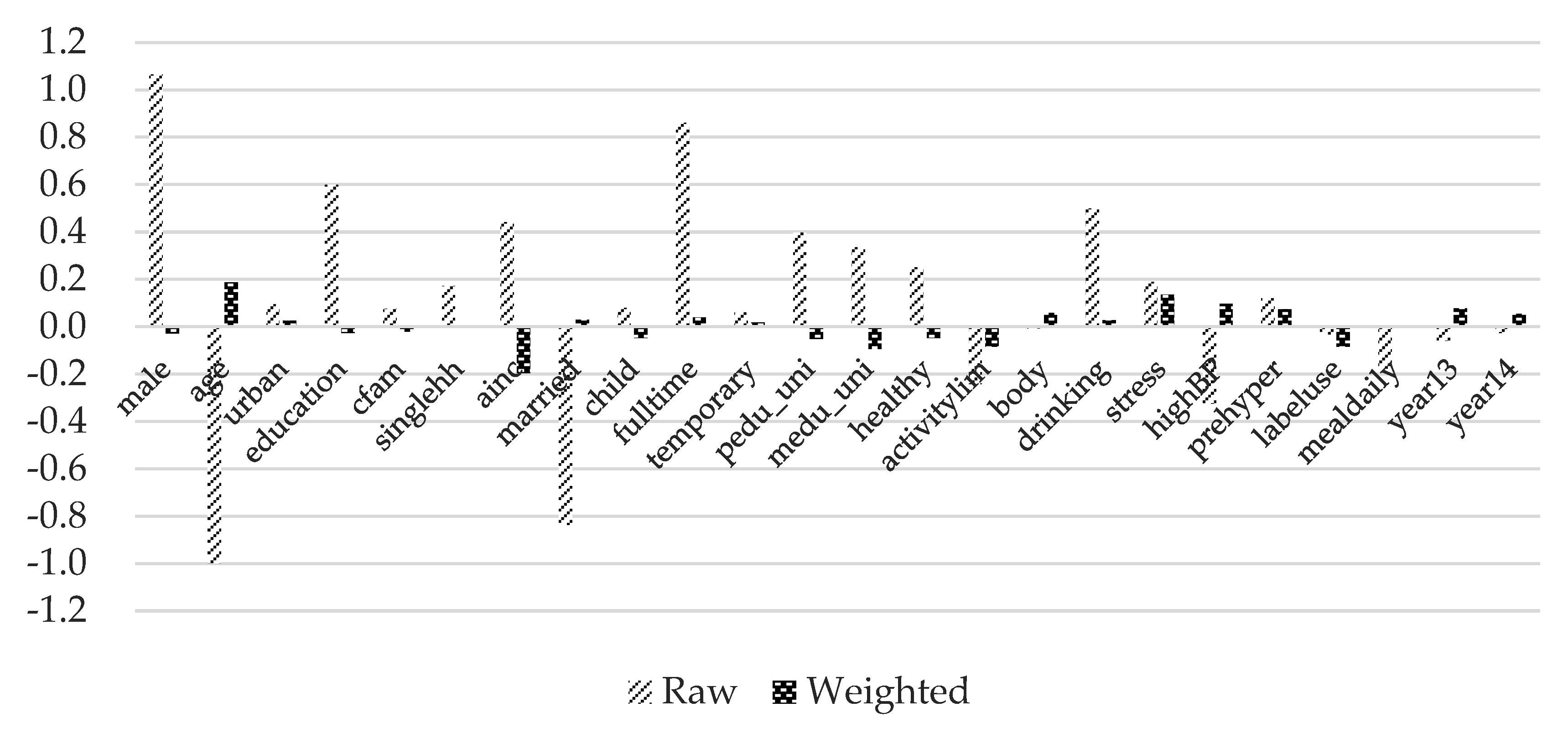
4.2. Covariate Balance Summary
4.3. The Average Treatment Fffects of FAFH
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Prochaska, F.J.; Schrimper, R.A. Opportunity cost of time and other socioeconomic effects on away-from-home food consumption. Am. J. Agric. Econ. 1973, 55, 595–603. [Google Scholar] [CrossRef]
- Nayga, R.M., Jr.; Capps, O., Jr. Analysis of food away from home and food at home consumption: A systems approach. J. Food Distrib. Res. 1992, 23, 1–10. [Google Scholar]
- Stewart, H.; Yen, S.T. Changing household characteristics and the away-from-home food market: A censored equation system approach. Food Policy 2004, 29, 643–658. [Google Scholar] [CrossRef]
- Drewnowski, A.; Darmon, N. Food choices and diet costs: An economic analysis. J. Nutr. 2005, 135, 900–904. [Google Scholar] [CrossRef] [PubMed]
- Stewart, H. Food Away from Home. In The Oxford Handbook of the Economics of Food Consumption and Policy; Oxford University Press: New York, NY, USA, 2011. [Google Scholar]
- Braha, K.; Cupák, A.; Pokrivčák, J.; Qineti ARizov, M. Economic analysis of the link between diet quality and health: Evidence from Kosovo. Econ. Hum. Biol. 2017, 27, 261–274. [Google Scholar] [CrossRef] [PubMed]
- Guthrie, J.F.; Lin, B.H.; Frazao, E. Role of food prepared away from home in the American diet, 1977–1978 versus 1994–1996: Changes and consequences. J. Nutr. Educ. Behav. 2002, 34, 140–150. [Google Scholar] [CrossRef]
- Mancino, L.; Todd, J.; Lin, B.H. Separating what we eat from where: Measuring the effect of food away from home on diet quality. Food Policy 2009, 34, 557–562. [Google Scholar] [CrossRef]
- Lin, B.H.; Guthrie, J. Nutritional Quality of Food Prepared at Home and Away From Home, 1977–2088; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2012. [Google Scholar]
- Dumagan, J.; Hackett, J. Trends in Eating Away from Home, 1982–1989; Statistical Bulletin No. 926; Economic Research Service, U.S. Department of Agriculture: Washington, DC, USA, 1995. [Google Scholar]
- Todd, J.E.; Mancino, L.; Lin, B.H. The Impact of Food Away from Home on Adult Diet Quality; EER-90; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2010. [Google Scholar]
- Larson, N.; Neumark-Sztainer, D.; Laska, M.N.; Story, M. Young adults and eating away from home: Associations with dietary intake patterns and weight status differ by choice of restaurant. J. Am. Diet. Assoc. 2011, 111, 1696–1703. [Google Scholar] [CrossRef]
- Binkley, J.K. The effect of demographic, economic, and nutrition factors on the frequency of food away from home. J. Consum. Aff. 2006, 40, 372–391. [Google Scholar] [CrossRef]
- Prescott, S.L.; Logan, A.C. Each meal matters in the exposome: Biological and community considerations in fast-food-socioeconomic associations. Econ. Hum. Biol. 2017, 27, 328–335. [Google Scholar] [CrossRef]
- Zagorsky, J.L.; Smith, P.K. The association between socioeconomic status and adult fast-food consumption in the US. Econ. Hum. Biol. 2017, 27, 12–25. [Google Scholar] [CrossRef] [PubMed]
- Bezerra, I.N.; Junior, E.V.; Pereira, R.A.; Sichieri, R. Away-from-home eating: Nutritional status and dietary intake among Brazilian adults. Public Health Nutr. 2015, 18, 1011–1017. [Google Scholar] [CrossRef] [PubMed]
- Naska, A.; Katsoulis, M.; Orfanos, P.; Lachat, C.; Gedrich, K.; Rodrigues, S.S.; Freisling, H.; Kolsteren, P.; Engeset, D.; Lopes, C.; et al. Eating out is different from eating at home among individuals who occasionally eat out. A cross-sectional study among middle-aged adults from eleven European countries. Br. J. Nutr. 2015, 113, 1951–1964. [Google Scholar] [CrossRef] [PubMed]
- Du, W.W.; Zhang, B.; Wang, H.J.; Wang, Z.H.; Su, C.; Zhang, J.G.; Zhang, J.; Jia, X.F.; Jiang, H.R. Gender difference in the association between food away-from-home consumption and body weight outcomes among Chinese adults. Public Health Nutr. 2016, 19, 2984–2990. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Lee, E.K.; Han, E. Food away from home and body mass outcomes: Taking heterogeneity into account enhances quality of results. Nutrition 2014, 30, 1015–1021. [Google Scholar] [CrossRef]
- Park, M.S.; Ahn, B.I.; Han, D.B. Impacts of Food Away From Home on Calorie Intakes. Korean J. Agric. Econ. 2014, 55, 73–98. [Google Scholar]
- Kim, S.Y. An Impact of Changes in Korean Adults Dietary Life on Obesity: Focusing on Expansion in Eating Away from Home. Korean J. Agric. Manag. Policy 2015, 42, 862–887. [Google Scholar]
- Bhutani, S.; Schoeller, D.A.; Walsh, M.C.; McWilliams, C. Frequency of eating out at both fast-food and sit-down restaurants was associated with high body max index in non-large metropolitan communities in Midwest. Am. J. Health Promot. 2018, 32, 75–83. [Google Scholar] [CrossRef]
- Pareatakul, S.; Ferdinad, D.P.; Champagne, C.M.; Ryan, D.H.; Bray, G.A. Fast-food consumption among US adults and children: Dietary and nutrient intake profile. J. Am. Diet. Assoc. 2003, 103, 1332–1338. [Google Scholar] [CrossRef]
- Marín-Guerrero, A.C.; Gutierrez-Fisac, J.L.; Guallar-Castillon, P. Eating behaviours and obesity in the adult population of Spain. Br. J. Nutr. 2008, 100, 1142–1148. [Google Scholar] [CrossRef]
- Smith, K.J.; McNaughton, S.A.; Gall, S.L. Takeaway food consumption and its associations with diet quality and abdominal obesity: A cross-sectional study of young adults. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 29. [Google Scholar] [CrossRef] [PubMed]
- Ayala, G.X.; Rogers, M.; Arredondo, E.M. Away-from-home food intake and risk for obesity: Examining the influence of context. Obesity 2008, 16, 1002–1008. [Google Scholar] [CrossRef] [PubMed]
- Orfanos, P.; Naska, A.; Trichopoulos, D. Eating out of home and its correlates in 10 European countries. The European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr. 2007, 10, 1515–1525. [Google Scholar] [CrossRef] [PubMed]
- Cornelisse-Vermaat, J.R.; van den Brink, H.M. Ethnic differences in lifestyle and overweight in the Netherlands. Obesity 2007, 15, 483–493. [Google Scholar] [CrossRef]
- Boutelle, K.N.; Fulkerson, J.A.; Neumark-Sztainer, D. Fast food for family meals: Relationships with parent and adolescent food intake, home food availability and weight status. Public Health Nutr. 2007, 10, 16–23. [Google Scholar] [CrossRef]
- Fulkerson, J.A.; Farbakhsh, K.; Lytle, L. Away-from-home family dinner sources and associations with weight status, body composition, and related biomarkers of chronic disease among adolescents and their parents. J. Am. Diet. Assoc. 2011, 111, 1892–1897. [Google Scholar] [CrossRef]
- Seguin, R.A.; Aggrawal, A.; Vermeylen, F.; Drewnowski, A. Comsumption Frequency of Foods Away from Home Linked with Higher Body Mass Index and Lower Fruit and Vegetable Intake among Adults: A Cross-Sectional Stydym. J. Environ. Public Health 2016, 2016, 3074241. [Google Scholar] [CrossRef]
- McClain, A.C.; Ayala, G.X.; Stores-Alvarez, D.; Siega-Riz, A.M.; Kaplan, R.C.; Gellman, M.D.; Gallo, L.C.; Van Horn, L.; Daviglus, M.L.; Perera, M.J.; et al. Frequency of Intake and Type of Away-from-Home Foods Consumed Are Associated with Diet Quality in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). J. Nutr. 2018, 148, 453–463. [Google Scholar] [CrossRef]
- Seo, J.; Ma, H.; Kim, S.; Kim, J.; Shin, M.; Yang, Y.J. Effects of the difference between actual body condition and body image perception on nutrient intake, weight control and mental health in Korean adults: Based on the 5th Korea National Health and Nutrition Examination Survey. J. Nutr. Health 2016, 49, 153–164. [Google Scholar] [CrossRef]
- Kim, S.Y.; Nayga, R.M., Jr.; Capps, O., Jr. The effect of food label use on nutrient intakes: An endogenous switching regression analysis. J. Agric. Resour. Econ. 2000, 25, 215–231. [Google Scholar]
- Rubin, D.B. Estimating causal effects of treatments in randomized and nonrandomized studies. J. Educ. Psychol. 1974, 66, 688. [Google Scholar] [CrossRef]
- Heckman, J.J.; Ichimura, H.; Todd, P.E. Matching as an econometric evaluation estimator: Evidence from evaluating a job training programme. Rev. Econ. Stud. 1997, 64, 605–654. [Google Scholar] [CrossRef]
- Schultz, T.P. School subsidies for the poor: Evaluating the Mexican Progresa poverty program. J. Dev. Econ. 2004, 74, 199–250. [Google Scholar] [CrossRef]
- Imai, K.; Van Dyk, D.A. Causal inference with general treatment regimes: Generalizing the propensity score. J. Am. Stat. Assoc. 2004, 99, 854–866. [Google Scholar] [CrossRef]
- Gibson-Davis, C.M.; Foster, E.M. A cautionary tale: Using propensity scores to estimate the effect of food stamps on food insecurity. Soc. Serv. Rev. 2006, 80, 93–126. [Google Scholar] [CrossRef]
- Foster, E.M. Propensity score matching: An illustrative analysis of dose response. Med. Care 2003, 41, 1183–1192. [Google Scholar] [CrossRef]
- Imbens, G.W. The role of the propensity score in estimating dose-response functions. Biometrika 2000, 87, 706–710. [Google Scholar] [CrossRef]
- Lechner, M. Identification and estimation of causal effects of multiple treatments under the conditional independence assumption. In Econometric Evaluation of Labour Market Policies; Springer: Mannheim, Germany, 2001; pp. 43–58. [Google Scholar]
- Frölich, M. Programme evaluation with multiple treatments. J. Econ. Surv. 2004, 18, 181–224. [Google Scholar] [CrossRef]
- Blundell, R.; Dearden, L.; Sianesi, B. Evaluating the effect of education on earnings: Models, methods and results from the National Child Development Survey. J. R. Stat. Soc. Ser. A (Stat. Soc.) 2005, 168, 473–512. [Google Scholar] [CrossRef]
- Tan, Z. Bounded, efficient and doubly robust estimation with inverse weighting. Biometrika 2010, 97, 661–682. [Google Scholar] [CrossRef]
- Cattaneo, M.D. Efficient semiparametric estimation of multi-valued treatment effects under ignorability. J. Econom. 2010, 155, 138–154. [Google Scholar] [CrossRef]
- Wooldridge, J.M. Econometric Analysis of Cross Section and Panel Data; MIT Press: London, UK, 2010. [Google Scholar]
- Rosenbaum, P.R.; Rubin, D.B. The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70, 41–55. [Google Scholar] [CrossRef]
- Uysal, S.D. Doubly robust estimation of causal effects with multivalued treatments: An application to the returns to schooling. J. Appl. Econom. 2015, 5, 763–786. [Google Scholar] [CrossRef]
- Imbens, G.W.; Rubin, D.B. Causal Inference in Statistics, Social, and Biomedical Sciences; Cambridge University Press: New York, NY, USA, 2015. [Google Scholar]
| Variable | Description |
|---|---|
| FAFH | More than or equal to twice a day = 3, 5–7 times per week = 2, 1–4 times per week = 1, Less than or equal to 3 times per month = 0 |
| Variable | Description | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| Energy deviation | (Daily energy intake—EER)/EER | −0.02 | 0.35 | −0.83 | 2.85 |
| Percentage deviation of energy | Absolute value of ((Daily energy intake—EER)/EER) | 0.27 | 0.22 | 0.0001 | 2.85 |
| Percentage deviation of protein | Absolute value of ((Daily protein intake—RI)/RI) | 0.41 | 0.43 | 2.07 × 10−5 | 6.28 |
| Percentage deviation of fat | Absolute value of ((Daily fat intake-AMDR)/AMDR) | 0.41 | 0.32 | 3.60 × 10−6 | 5.82 |
| Percengate deviation of carbohydarate | Absolute value of ((Daily carbohydrate intake—AMDR)/AMDR) | 0.30 | 0.26 | 1.42 × 10−5 | 2.23 |
| Percentage deviation of 3 essential nutrients | Average of percentage deviation of protein, fat and carbohydrate | 0.37 | 0.28 | 0.02 | 4.63 |
| Percentage deviation of sodium | Absolute value of ((Daily sodium intake—AI)/AI) | 1.26 | 1.10 | 0.0001 | 13.00 |
| Percentage of calcium | Absolute value of ((Daily calcium intake—RI)/RI) | 0.42 | 0.22 | 4.26 × 10−5 | 2.16 |
| Percentage deviation of Potassium | Absolute value of ((Daily potassium intake—AI)/AI) | 0.34 | 0.23 | 4.25 × 10−5 | 2.58 |
| BMI | Body mass index | 23.68 | 3.53 | 14.59 | 48.96 |
| Obesity | If BMI is greater than or equal to 25 kg/m2 = 1, otherwise = 0 | 0.31 | 0.46 | 0 | 1 |
| Variable | Description | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| male | Male = 1, Female = 0 | 0.38 | 0.49 | 0 | 1 |
| age | Age | 43.76 | 12.75 | 19 | 64 |
| urban | Urban = 1, Rural = 0 | 0.47 | 0.50 | 0 | 1 |
| education | At least university = 1, otherwise = 0 | 0.40 | 0.49 | 0 | 1 |
| cfam | The number of family member(s) | 3.24 | 1.17 | 1 | 6 |
| singlehh | If single household = 1, otherwise = 0 | 0.06 | 0.24 | 0 | 1 |
| ainc | Average monthly household income (unit: 10,000 won) If less than or equal to 17 = 17, 18-1499 = continuous value, If greater than or equal to 1500 = 1500 | 415.78 | 284.71 | 17 | 1500 |
| married | If married = 1, otherwise = 0 | 0.80 | 0.40 | 0 | 1 |
| child | If have child under 19 = 1, otherwise = 0 | 0.42 | 0.49 | 0 | 1 |
| fulltime | If have full-time job = 1, otherwise = 0 | 0.19 | 0.39 | 0 | 1 |
| temporary | If have temporary job = 1, otherwise = 0 | 0.24 | 0.43 | 0 | 1 |
| unemployed | If unemployed = 1, otherwise = 0 | 0.57 | 0.49 | 0 | 1 |
| pedu_uni | Father’s education level If higher than high school graduation = 1, otherwise = 0 | 0.14 | 0.35 | 0 | 1 |
| medu_uni | Mother’s education level If higher than high school graduation = 1, otherwise = 0 | 0.06 | 0.24 | 0 | 1 |
| healthy | Subjective health status If more than or equal to “good” = 1, otherwise = 0 | 0.33 | 0.47 | 0 | 1 |
| activitylim | If have activity limitation = 1, otherwise = 0 | 0.06 | 0.23 | 0 | 1 |
| body | Subjective body perception If fat = 1, otherwise = 0 | 0.46 | 0.50 | 0 | 1 |
| drinking | Frequency of drinking If drink twice or more per week = 1, otherwise = 0 | 0.21 | 0.41 | 0 | 1 |
| stress | Stress awareness If get stress a lot = 1, otherwise = 0 | 0.26 | 0.44 | 0 | 1 |
| highBP | If high blood pressure = 1, otherwise = 0 | 0.20 | 0.40 | 0 | 1 |
| hypertension | If hypertension = 1, otherwise = 0 | 0.24 | 0.43 | 0 | 1 |
| labeluse | If use nutrition label = 1, otherwise = 0 | 0.31 | 0.46 | 0 | 1 |
| mealdaily | The number of meals per day | 2.53 | 0.56 | 0 | 6 |
| strength | The number of days of weight training exercises per week | 0.78 | 1.50 | 0 | 5 |
| stretch | The number of days of flexibility exercise per week | 1.91 | 1.96 | 0 | 5 |
| dietetictherapy | If practice dietetic therapy =1, otherwise = 0 | 0.24 | 0.43 | 0 | 1 |
| year13 | If year 2013 = 1, otherwise = 0 | 0.36 | 0.48 | 0 | 1 |
| year14 | If year 2014 = 1, otherwise = 0 | 0.32 | 0.47 | 0 | 1 |
| year15 | If year 2015 = 1, otherwise = 0 | 0.32 | 0.47 | 0 | 1 |
| Variables | 1–4 Times per Week | 5–7 Times per Week | At Least Twice per Day |
|---|---|---|---|
| male | 0.3577 *** | 1.4795 *** | 1.8656 *** |
| (0.0831) | (0.0898) | (0.1287) | |
| age | −0.0369 *** | −0.0475 *** | −0.0502 *** |
| (0.0045) | (0.0052) | (0.0074) | |
| urban | 0.0858 | 0.1755 ** | 0.1985 * |
| (0.0648) | (0.0749) | (0.1085) | |
| education | 0.4987 *** | 0.4076 *** | 0.3938 *** |
| (0.0793) | (0.0883) | (0.1223) | |
| cfam | −0.1409 *** | −0.1302 *** | −0.1680 ** |
| (0.0390) | (0.0447) | (0.0664) | |
| singlehh | 0.0343 | 0.2573 | 0.6158 ** |
| (0.1580) | (0.1820) | (0.2430) | |
| ainc | 0.0011 *** | 0.0015 *** | 0.0015 *** |
| (0.0001) | (0.0002) | (0.0002) | |
| married | 0.0975 | −0.2368 | −0.8527 *** |
| (0.1480) | (0.1614) | (0.2122) | |
| child | 0.1284 | 0.2015 * | 0.1964 |
| (0.0928) | (0.1058) | (0.1541) | |
| fulltime | 0.1713 | 2.0289 *** | 1.9568 *** |
| (0.1294) | (0.1263) | (0.1584) | |
| temporary | 0.1316 | 1.2096 *** | 0.6755 *** |
| (0.0801) | (0.0886) | (0.1383) | |
| pedu_uni | 0.1975 | 0.1861 | 0.3476 ** |
| (0.1253) | (0.1376) | (0.1760) | |
| medu_uni | 0.4360 * | 0.4863 ** | 0.1983 |
| (0.2264) | (0.2381) | (0.2831) | |
| healthy | 0.2863 *** | 0.3059 *** | 0.1307 |
| (0.0738) | (0.0836) | (0.1198) | |
| activitylim | −0.3813 *** | −0.580 *** | −0.3086 |
| (0.1228) | (0.1650) | (0.2439) | |
| body | 0.1159 * | 0.1314 * | 0.2704 ** |
| (0.0660) | (0.0767) | (0.1119) | |
| drinking | 0.3389 *** | 0.4428 *** | 0.8488 *** |
| (0.0929) | (0.1004) | (0.1307) | |
| stress | −0.0360 | 0.1710 * | 0.2911 ** |
| (0.0777) | (0.0878) | (0.1227) | |
| highBP | −0.1816 ** | −0.0864 | −0.5131 *** |
| (0.0904) | (0.1068) | (0.1696) | |
| prehyper | −0.1251 | −0.1689 * | −0.0857 |
| (0.0827) | (0.0959) | (0.1334) | |
| labeluse | −0.0816 | −0.1669 * | −0.1383 |
| (0.0735) | (0.0858) | (0.1253) | |
| mealdaily | −0.1478 ** | 0.0008 | 0.1130 |
| (0.0615) | (0.0711) | (0.1026) | |
| year13 | −0.0476 | −0.0862 | −0.2004 |
| (0.0796) | (0.0919) | (0.1333) | |
| year14 | −0.1517 * | −0.1019 | −0.1093 |
| (0.0805) | (0.0928) | (0.1328) | |
| Constant | 2.2025 *** | 0.7760 ** | −0.4771 |
| (0.2666) | (0.3013) | (0.4259) | |
| Observations | 7456 | ||
| Covariates | Control (Having FAFH Less Than or Equal to 3 Times per Month) | Treated 1 (Having FAFH 1–4 Times per Week) | Treated 2 (Having FAFH 5–7 Times per Week) | Treated 3 (Having FAFH at Least Twice per Day) |
|---|---|---|---|---|
| male | 0.22 | 0.27 | 0.58 | 0.68 |
| age | 50.14 | 43.37 | 40.74 | 38.30 |
| urban | 0.45 | 0.47 | 0.49 | 0.50 |
| education | 0.21 | 0.42 | 0.49 | 0.49 |
| cfam | 3.09 | 3.28 | 3.33 | 3.18 |
| singlehh | 0.06 | 0.05 | 0.06 | 0.11 |
| ainc | 331.49 | 422.15 | 463.09 | 451.03 |
| married | 0.92 | 0.82 | 0.73 | 0.59 |
| child | 0.34 | 0.44 | 0.45 | 0.38 |
| fulltime | 0.06 | 0.10 | 0.36 | 0.38 |
| temporary | 0.20 | 0.21 | 0.30 | 0.22 |
| pedu_uni | 0.07 | 0.15 | 0.17 | 0.21 |
| medu_uni | 0.02 | 0.06 | 0.08 | 0.09 |
| healthy | 0.24 | 0.35 | 0.38 | 0.35 |
| activitylim | 0.11 | 0.05 | 0.03 | 0.05 |
| body | 0.47 | 0.47 | 0.45 | 0.47 |
| drinking | 0.14 | 0.18 | 0.26 | 0.34 |
| stress | 0.24 | 0.24 | 0.28 | 0.32 |
| highBP | 0.27 | 0.17 | 0.19 | 0.14 |
| prehyper | 0.24 | 0.22 | 0.24 | 0.30 |
| labeluse | 0.29 | 0.35 | 0.28 | 0.27 |
| mealdaily | 2.60 | 2.50 | 2.52 | 2.50 |
| year13 | 0.36 | 0.36 | 0.36 | 0.33 |
| year14 | 0.34 | 0.31 | 0.32 | 0.33 |
| POMs/ATEs | Precentage Deviation of Energy | Percentage Deviation of Three Essential Nutrients | Percentage Deviation of Protein | Percentage Deviation of Fat | Percentae Deviation of Carbohydarate |
|---|---|---|---|---|---|
| POMs | |||||
| 0 | 0.2515 *** | 0.3409 *** | 0.3368 *** | 0.3976 *** | 0.2885 *** |
| (0.0070) | (0.0068) | (0.0100) | (0.0085) | (0.0078) | |
| 1 | 0.2677 *** | 0.3774 *** | 0.4210 *** | 0.4026 *** | 0.3087 *** |
| (0.0045) | (0.0056) | (0.0087) | (0.0061) | (0.0052) | |
| 2 | 0.2632 *** | 0.3656 *** | 0.4100 *** | 0.3990 *** | 0.2877 *** |
| (0.0059) | (0.0073) | (0.0108) | (0.0083) | (0.0069) | |
| 3 | 0.2737 *** | 0.3695 *** | 0.4133 *** | 0.4122 *** | 0.2830 *** |
| (0.0137) | (0.0145) | (0.0210) | (0.0174) | (0.0160) | |
| ATEs | |||||
| 1 vs. 0 | 0.0162 * | 0.0365 *** | 0.0842 *** | 0.0051 | 0.0202 ** |
| (0.0083) | (0.0088) | (0.0132) | (0.0104) | (0.0094) | |
| 2 vs. 0 | 0.0117 | 0.0246 ** | 0.0732 *** | 0.0014 | −0.0008 |
| (0.0091) | (0.0099) | (0.0147) | (0.0119) | (0.0104) | |
| 3 vs. 0 | 0.0222 | 0.0286 * | 0.0765 *** | 0.0146 | −0.0054 |
| (0.0154) | (0.0160) | (0.0232) | (0.0193) | (0.0178) |
| POMs/ATEs | Percentage Deviation of Calcium | Percentage Deviation of Sodium | Percentage Deviation of Potassium |
|---|---|---|---|
| POMs | |||
| 0 | 0.4378 *** | 0.9990 *** | 0.3543 *** |
| (0.0086) | (0.0314) | (0.0076) | |
| 1 | 0.4064 *** | 1.2787 *** | 0.3259 *** |
| (0.0043) | (0.0214) | (0.0046) | |
| 2 | 0.4155 *** | 1.3166 *** | 0.3327 *** |
| (0.0058) | (0.0256) | (0.0061) | |
| 3 | 0.4101 *** | 1.3161 *** | 0.3278 *** |
| (0.0142) | (0.0616) | (0.0129) | |
| ATEs | |||
| 1 vs. 0 | −0.0314 *** | 0.2797 *** | −0.0284 *** |
| (0.0096) | (0.0378) | (0.0089) | |
| 2 vs. 0 | −0.0223 ** | 0.3176 *** | −0.0216 ** |
| (0.0103) | (0.0403) | (0.0098) | |
| 3 vs. 0 | −0.0277 * | 0.3172 *** | −0.0264 * |
| (0.0165) | (0.0690) | (0.0150) |
| POMs/ATEs | Energy Deviation | BMI | Obesity |
|---|---|---|---|
| POMs | |||
| 0 | −0.0941 *** | 23.7889 *** | 0.3228 *** |
| (0.0102) | (0.0863) | (0.0109) | |
| 1 | −0.0039 | 23.7350 *** | 0.3166 *** |
| (0.0069) | (0.0575) | (0.0080) | |
| 2 | −0.0173 ** | 23.4991 *** | 0.2917 *** |
| (0.0088) | (0.0736) | (0.0107) | |
| 3 | −0.0311 | 24.0698 *** | 0.3622 *** |
| (0.0206) | (0.1731) | (0.0243) | |
| ATEs | |||
| 1 vs. 0 | 0.0902 *** | −0.0539 | −0.0062 |
| (0.0122) | (0.0943) | (0.0125) | |
| 2 vs. 0 | 0.0768 *** | −0.2898 *** | −0.0311 ** |
| (0.0133) | (0.1052) | (0.0144) | |
| 3 vs. 0 | 0.0630 *** | 0.2809 | 0.0394 |
| (0.0230) | (0.1887) | (0.0261) |
| POMs/ATEs | Obesity Age < 40 | Obesity Age ≥ 40 | Obesity Age ≥ 50 |
|---|---|---|---|
| POMs | |||
| 0 | 0.2699 *** | 0.3481 *** | 0.3843 *** |
| (0.0213) | (0.0132) | (0.0146) | |
| 1 | 0.2631 *** | 0.3457 *** | 0.3723 *** |
| (0.0116) | (0.0108) | (0.0134) | |
| 2 | 0.2615 *** | 0.3193 *** | 0.3512 *** |
| (0.0140) | (0.0154) | (0.0213) | |
| 3 | 0.2621 *** | 0.4276 *** | 0.4362 *** |
| (0.0345) | (0.0315) | (0.0383) | |
| ATEs | |||
| 1 vs. 0 | −0.00676 | −0.0024 | −0.0120 |
| (0.0229) | (0.0159) | (0.0181) | |
| 2 vs. 0 | −0.00842 | −0.0288 | −0.0331 |
| (0.0241) | (0.0192) | (0.0245) | |
| 3 vs. 0 | −0.00776 | 0.0795 ** | 0.0519 |
| (0.0397) | (0.0336) | (0.0403) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.; Ahn, B.-i. Eating Out and Consumers’ Health: Evidence on Obesity and Balanced Nutrition Intakes. Int. J. Environ. Res. Public Health 2020, 17, 586. https://doi.org/10.3390/ijerph17020586
Kim D, Ahn B-i. Eating Out and Consumers’ Health: Evidence on Obesity and Balanced Nutrition Intakes. International Journal of Environmental Research and Public Health. 2020; 17(2):586. https://doi.org/10.3390/ijerph17020586
Chicago/Turabian StyleKim, Dahye, and Byeong-il Ahn. 2020. "Eating Out and Consumers’ Health: Evidence on Obesity and Balanced Nutrition Intakes" International Journal of Environmental Research and Public Health 17, no. 2: 586. https://doi.org/10.3390/ijerph17020586
APA StyleKim, D., & Ahn, B.-i. (2020). Eating Out and Consumers’ Health: Evidence on Obesity and Balanced Nutrition Intakes. International Journal of Environmental Research and Public Health, 17(2), 586. https://doi.org/10.3390/ijerph17020586






