Health-Related Behaviors in Adolescents Mediate the Association between Subjective Social Status and Body Mass Index
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Subjects
2.1.1. Outcome Variables
2.1.2. Exposure Variable (SSS)
2.2. Statistical Analyses
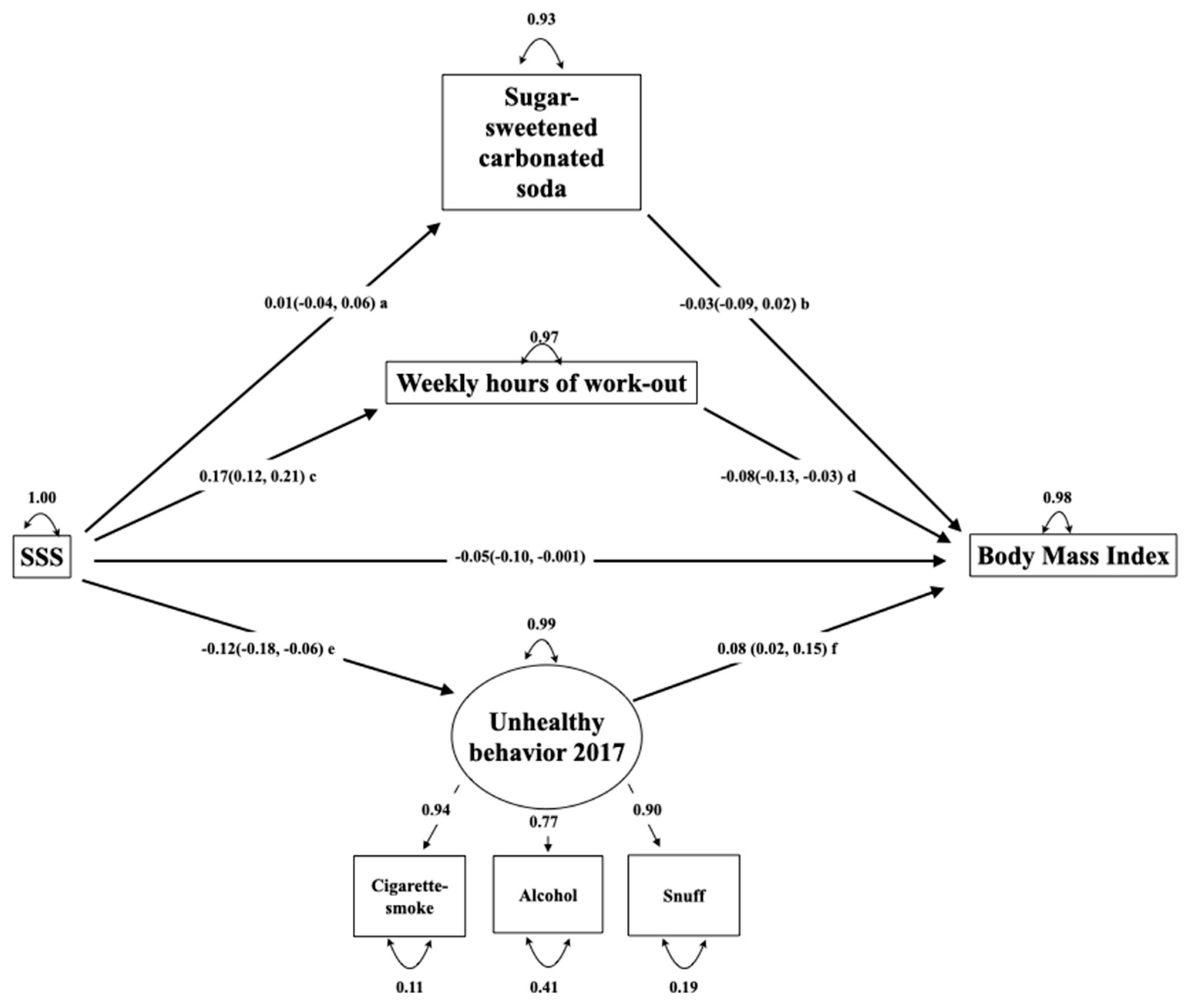
2.2.1. SEM Analyses
Latent Variables
Structural Model
Model Fit
3. Results
4. Discussion
4.1. Main Results
4.2. The Association between SSS and BMI in 2002 and 2017
4.3. Unhealthy Behaviors in Adolescents
4.4. Strengths
4.5. Limitations
4.6. Implications
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Variable Type | Categories | Use of Variable | |
|---|---|---|---|
| SSS = perceived family economy a | Ordinal | Poor, average, good, very good | Exposure |
| BMI b | Continuous | - | Outcome |
| Consumption of cakes and candy | Ordinal | Seldom/never, 1–3 times monthly, 1–3 times weekly, 4–6 times weekly, once-twice daily, ≥3 times daily | Not used in the model |
| Consumption of sugar-sweetened carbonated sodas | Ordinal | Seldom/never, 1–6 glasses weekly, 1 glass daily, 2–3 glasses daily and ≥4 glasses daily | Mediator |
| Consumption of lemonade | Ordinal | Seldom/never, 1–6 glasses weekly, 1 glass daily, 2–3 glasses daily and ≥4 glasses daily | Not used in the model |
| Consumption of energy drinks | Ordinal | Seldom/never, 1–3 times monthly, Once weekly, glass daily, 2–3 times weekly, 4–5 times weekly | Not used in the model |
| Weekly hours of leisure-time workout | Ordinal | 0, 1–2, 3–4, 5–7, 8–10 and ≥11 | Mediator |
| Member of sports team | Nominal | Yes/no | Not used in the model |
| Average daily screen time on school days | Ordinal | Less than 1 h, 1–2 h, 3–5 h, >5 h | Not used in the model |
| Cigarette smoking | Ordinal | Never, have quit, occasionally, daily | In latent variable |
| Snuff-use | Ordinal | Never, have quit, occasionally, daily | In latent variable |
| Ever tried alcohol | Nominal | No/yes | In latent variable |
| Frequency of daily toothbrushing | Ordinal | Once daily, Once daily, every second day, <every second day | Not used in the model |
| BMI a | SSS b | Soda c | Smoking d | Snuff e | Alcohol f | Exercise g | Lemonade h | Energydrink i | Not member of Sports Team j | Screen Time k | Toothbrush l | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI a | 1 | |||||||||||
| SSS b | −0.08 * | 1 | ||||||||||
| Soda c | −0.02 | −0.02 | 1 | |||||||||
| Smoking d | 0.06 * | −0.08 * | 0.12 * | 1 | ||||||||
| Snuff e | 0.05 | −0.06 * | 0.11 * | 0.64 * | 1 | |||||||
| Alcohol f | 0.05 | −0.10 * | 0.13 * | 0.29 * | 0.30 * | 1 | ||||||
| Excercise g | −0.06 * | 0.15 * | −0.04 | −0.08 * | −0.06 * | −0.07 * | 1 | |||||
| Lemonade h | −0.04 | −0.04 | 0.30 * | 0.10 * | 0.10 * | 0.02 | −0.02 | 1 | ||||
| Energy drink i | 0.07 * | −0.05 | 0.27 * | 0.19 * | 0.23 * | 0.31 * | −0.03 | 0.18 * | 1 | |||
| Not member of sports team j | 0.09 * | −0.11 * | −0.04 | 0.12 * | 0.11 * | 0.09 * | −0.52 * | −0.08 * | 0.05 | 1 | ||
| Screen time k | 0.06 * | −0.07 * | 0.10 * | 0.13 * | 0.11 * | 0.14 * | 0.19 * | 0.02 | 0.16 * | 0.14 * | 1 | |
| Toothbrush l | 0.07 * | −0.11 * | 0.15 * | 0.16 * | 0.13 * | 0.06 * | −0.17 * | 0.11 * | 0.17 * | 0.11 * | 0.13 * | 1 |
| Candy and cakes m | −0.02 | −0.02 | 0.26 * | 0.01 | 0.01 | 0.05 | −0.10 * | 0.11 * | 0.08 * | −0.05 | 0.15 * | 0.06 * |
| Included in Study n = 1534 | Not included in Study n = 141 c | |
|---|---|---|
| Gender (boys) | 818 (47.8) | 76 (54) |
| BMI a; mean (SD b) | 21.4 (3.1) n = 1534 | 20.9 (3.2) n = 95 |
| SSS c | ||
| Poor | 62 (4.0) | 5(4.0) |
| Average | 469 (30.6) | 41(33.0) |
| Good | 832 (54.2) | 65 (52.4) |
| Very good | 171 (11.2) | 13(10.5) |
| Weekly hours of leisure-time workout | ||
| 0 | 150 (9.4) | 18 (13.6) |
| 1–2 | 362 (22.7) | 35 (26.5) |
| 3–4 | 417 (26.1) | 27 (20.5) |
| 5–7 | 362 (22.7) | 27 (20.5) |
| 8–10 | 190 (11.9) | 18 (13.6) |
| ≥11 | 115 (7.2) | 7 (5.3) |
| Sugar-sweetened carbonated sodas | ||
| Seldom/never | 169 (10.6.) | 23 (19.7) |
| 1–6 glasses weekly | 837 (52.4) | 73 (62.4) |
| 1 glass daily | 234 (14.7) | 9 (7.7) |
| 2–3 glasses daily | 235(14.7) | 10 (8.9) |
| ≥4 glasses daily | 121 (7.6) | 2 (1.7) |
| Cigarette smoking habits | ||
| Never | 993 (62.2) | 97 (83.6) |
| Have quit | 151 (9.5) | 9 (7.8) |
| Occasionally | 236 (14.8) | 8 (6.9) |
| Daily | 216 (13.5) | 2 (1.7) |
References
- Pulgaron, E.R. Childhood obesity: A review of increased risk for physical and psychological comorbidities. Clin. Ther. 2013, 35, A18–A32. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.S.; Mulder, C.; Twisk, J.W.; van Mechelen, W.; Chinapaw, M.J. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes. Rev. 2008, 9, 474–488. [Google Scholar] [CrossRef] [PubMed]
- HUNT Research Center. Self-Perceived Health, Body Mass and Risk Behavior among Adolescents in Nord-Trøndelag County 2017–19; Health Statistics Report No. 1, the Young-HUNT4 Survey; Hunt Research Centre: Levanger, Norway, March 2020; Available online: https://www.ntnu.no/documents/10304/4902807/Delrapport1_Ung_HUNT4+_Mars2020.pdf/e7f7a922-906f-aa1c-9aed-4fa2d7bf14b9?t=1584711026088 (accessed on 23 March 2020).
- Weihrauch-Blüher, S.; Kromeyer-Hauschild, K.; Graf, C.; Widhalm, K.; Korsten-Reck, U.; Jödicke, B.; Markert, J.; Müller, M.J.; Moss, A.; Wabitsch, M. Current guidelines for obesity prevention in childhood and adolescence. Obes. Facts 2018, 11, 263–276. [Google Scholar] [CrossRef]
- Euteneuer, F. Subjective social status and health. Curr. Opin. Psychiatry 2014, 27, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Pampel, F.C.; Krueger, P.M.; Denney, J.T. Socioeconomic disparities in health behaviors. Annu. Rev. Sociol. 2010, 36, 349–370. [Google Scholar] [CrossRef]
- West, P. Health inequalities in the early years: Is there equalisation in youth? Soc. Sci. Med. 1997, 44, 833–858. [Google Scholar] [CrossRef]
- Broyles, S.; Denstel, K.; Church, T.; Chaput, J.; Fogelholm, M.; Hu, G.; Kuriyan, R.; Kurpad, A.; Lambert, E.; Maher, C. The epidemiological transition and the global childhood obesity epidemic. Int. J. Obes. Suppl. 2015, 5, S3–S8. [Google Scholar] [CrossRef]
- Bann, D.; Johnson, W.; Li, L.; Kuh, D.; Hardy, R. Socioeconomic inequalities in childhood and adolescent body-mass index, weight, and height from 1953 to 2015: An analysis of four longitudinal, observational, British birth cohort studies. Lancet Public Health 2018, 3, e194–e203. [Google Scholar] [CrossRef]
- Swinburn, B.; Sacks, G.; Vandevijvere, S.; Kumanyika, S.; Lobstein, T.; Neal, B.; Barquera, S.; Friel, S.; Hawkes, C.; Kelly, B. INFORMAS (International Network for Food and Obesity/non-communicable diseases Research, Monitoring and Action Support): Overview and key principles. Obes. Rev. 2013, 14, 1–12. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Mason, C. The physical activity transition. J. Phys. Act. Health 2009, 6, 269–280. [Google Scholar] [CrossRef]
- Viner, R.M.; Ozer, E.M.; Denny, S.; Marmot, M.; Resnick, M.; Fatusi, A.; Currie, C. Adolescence and the social determinants of health. Lancet 2012, 379, 1641–1652. [Google Scholar] [CrossRef]
- Shulman, E.P.; Smith, A.R.; Silva, K.; Icenogle, G.; Duell, N.; Chein, J.; Steinberg, L. The dual systems model: Review, reappraisal, and reaffirmation. Dev. Cogn. Neurosci. 2016, 17, 103–117. [Google Scholar] [CrossRef] [PubMed]
- Baik, J.H. Dopamine signaling in reward-related behaviors. Front. Neural Circuits 2013, 7, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Galván, A. Adolescent development of the reward system. Front. Hum. Neurosci. 2010, 4, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Krach, S.; Paulus, F.M.; Bodden, M.; Kircher, T. The rewarding nature of social interactions. Front. Behav. Neurosci. 2010, 4, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Adler, N.E.; Epel, E.S.; Castellazzo, G.; Ickovics, J.R. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, White women. Health Psychol. 2000, 19, 586. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, M.; Kent, B.V.; Henderson, W.M.; Setar, A.C. Subjective social status, life course SES, and BMI in young adulthood. Health Psychol. 2017, 36, 682. [Google Scholar] [CrossRef] [PubMed]
- Azzopardi, P.S.; Hearps, S.J.C.; Francis, K.L.; Kennedy, E.C.; Mokdad, A.H.; Kassebaum, N.J.; Lim, S.; Irvine, C.M.S.; Vos, T.; Brown, A.D.; et al. Progress in adolescent health and wellbeing: Tracking 12 headline indicators for 195 countries and territories, 1990–2016. Lancet 2019, 393, 1101–1118. [Google Scholar] [CrossRef]
- Norwegian Institute of Public Health; Soegaard, A.J.; Eide, T. Youth Studies 2000–2009. Available online: https://www.fhi.no/en/more/health-studies/landsomfattende-helseundersokelser-lhu/helseundersokelser/youth-studies-2000-2009/ (accessed on 12 February 2020).
- Greenland, S.; Senn, S.J.; Rothman, K.J.; Carlin, J.B.; Poole, C.; Goodman, S.N.; Altman, D.G. Statistical tests, p values, confidence intervals, and power: A guide to misinterpretations. Eur. J. Epidemiol. 2016, 31, 337–350. [Google Scholar] [CrossRef]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef]
- Schreiber, J.B.; Nora, A.; Stage, F.K.; Barlow, E.A.; King, J. Reporting structural equation modeling and confirmatory factor analysis results: A review. J. Educ. Res. 2006, 99, 323–338. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Publications: New York, NY, USA, 2015; pp. 257–278. [Google Scholar]
- Rosseel, Y.; Oberski, D.; Byrnes, J.; Vanbrabant, L.; Savalei, V.; Merkle, E.; Chow, M. Package ‘lavaan’ 0.6–2. Available online: https://cran.r-project.org/web/packages/lavaan/lavaan.pdf (accessed on 18 December 2019).
- Epskamp, S.; Stuber, S.; Nak, J.; Veenman, M.; Jorgensen, T.D. Package ‘semPlot’ 1.1.2. Available online: https://github.com/SachaEpskamp/semPlot (accessed on 18 December 2019).
- Jorgensen, T.D.; Pornprasertmanit, S.; Schoemann, A.M.; Rosseel, Y. Package ‘semTools’ v 0.5–2.0. Available online: https://github.com/simsem/semTools/wiki (accessed on 19 December 2019).
- Chen, E.; Paterson, L.Q. Neighborhood, family, and subjective socioeconomic status: How do they relate to adolescent health? Health Psychol. 2006, 25, 704. [Google Scholar] [CrossRef] [PubMed]
- Goodman, E.; Adler, N.E.; Daniels, S.R.; Morrison, J.A.; Slap, G.B.; Dolan, L.M. Impact of objective and subjective social status on obesity in a biracial cohort of adolescents. Obes. Res. 2003, 11, 1018–1026. [Google Scholar] [CrossRef] [PubMed]
- Sobal, J.; Stunkard, A.J. Socioeconomic status and obesity: A review of the literature. Psychol. Bull. 1989, 105, 260–275. [Google Scholar] [CrossRef]
- Shrewsbury, V.; Wardle, J. Socioeconomic atatus and adiposity in childhood: A systematic review of cross-sectional studies 1990–2005. Obesity 2008, 16, 275–284. [Google Scholar] [CrossRef]
- Barriuso, L.; Miqueleiz, E.; Albaladejo, R.; Villanueva, R.; Santos, J.M.; Regidor, E. Socioeconomic position and childhood-adolescent weight status in rich countries: A systematic review, 1990–2013. BMC Pediatrics 2015, 15, 129–143. [Google Scholar] [CrossRef]
- Omram, A.R. The epidemiologic transition: A theory of the epidemiology of population change. Bull. World Health Organ. 1971, 49, 509–538. [Google Scholar]
- Drewnowski, A.; Popkin, B.M. The nutrition transition: New trends in the global diet. Nutr. Rev. 1997, 55, 31–43. [Google Scholar] [CrossRef]
- Mekonnen, T.; Havdal, H.H.; Lien, N.; O’Halloran, S.A.; Arah, O.A.; Papadopoulou, E.; Gebremariam, M.K. Mediators of socioeconomic inequalities in dietary behaviours among youth: A systematic review. Obes. Rev. 2020, 21, e13016. [Google Scholar] [CrossRef]
- Evans, G.W.; Jones-Rounds, M.L.; Belojević, G.; Vermeylen, F. Family income and childhood obesity in eight European cities: The mediating roles of Neighborhood characteristics and physical activity. Soc. Sci. Med. 2012, 75, 477–481. [Google Scholar] [CrossRef]
- Tyrrell, J.; Wood, A.R.; Ames, R.M.; Yaghootkar, H.; Beaumont, R.N.; Jones, S.E.; Tuke, M.A.; Ruth, K.S.; Freathy, R.M.; Smith, G.D.; et al. Gene-obesogenic environment interactions in the UK Biobank study. Int. J. Epidemiol. 2017, 46, 559–575. [Google Scholar] [CrossRef] [PubMed]
- Claassen, M.A.; Klein, O.; Bratanova, B.; Claes, N.; Corneille, O. A systematic review of psychosocial explanations for the relationship between socioeconomic status and body mass index. Appetite 2019, 132, 208–221. [Google Scholar] [CrossRef] [PubMed]
- MacKenbach, J.D.; Lakerveld, J.; van Oostveen, Y.; Compernolle, S.; De Bourdeaudhuij, I.; Bárdos, H.; Rutter, H.; Glonti, K.; Oppert, J.M.; Charreire, H.; et al. The mediating role of social capital in the association between neighbourhood income inequality and body mass index. Eur. J. Public Health 2017, 27, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Fleary, S.A. Combined patterns of risk for problem and obesogenic behaviors in adolescents: A latent class analysis approach. J. Sch. Health 2017, 87, 182–193. [Google Scholar] [CrossRef] [PubMed]
- Van Ansem, W.J.; van Lenthe, F.J.; Schrijvers, C.T.; Rodenburg, G.; van de Mheen, D. Socio-economic inequalities in children’s snack consumption and sugar-sweetened beverage consumption: The contribution of home environmental factors. Br. J. Nutr. 2014, 112, 467–476. [Google Scholar] [CrossRef] [PubMed]
- Gebremariam, M.K.; Lien, N.; Nianogo, R.A.; Arah, O.A. Mediators of socioeconomic differences in adiposity among youth: A systematic review. Obes. Rev. 2017, 18, 880–898. [Google Scholar] [CrossRef] [PubMed]
- Helsedirektoratet. Utviklingen i Norsk Kosthold 2019. Available online: https://www.helsedirektoratet.no/rapporter/utviklingen-i-norsk-kosthold/Utviklingen%20i%20norsk%20kosthold%202019%20–%20Kortversjon.pdf/_/attachment/inline/aff8abec-7eb3-4b19-98a6-7358d500da48:f6bdf858604dc30399e7ae9a9d815c4658365243/Utviklingen%20i%20norsk%20kosthold%202019%20–%20Kortversjon.pdf (accessed on 20 August 2020).
- Casetta, B.; Videla, A.J.; Bardach, A.; Morello, P.; Soto, N.; Lee, K.; Camacho, P.A.; Moquillaza, R.V.H.; Ciapponi, A. Association between cigarette smoking prevalence and income level: A systematic review and meta-analysis. Nicotine Tob. Res. 2017, 19, 1401–1407. [Google Scholar] [CrossRef]
- Hagquist, C.E. Health inequalities among adolescents—The impact of academic orientation and parents’ education. Eur. J. Public Health 2007, 17, 21–26. [Google Scholar] [CrossRef]
- Pedersen, W.; von Soest, T. Tobacco use among Norwegian adolescents: From cigarettes to snus. Addiction 2014, 109, 1154–1162. [Google Scholar] [CrossRef]
- WHO Regional Office for Europe. Key Findings from the Health Behaviour in School-Aged Children (HBSC) Study: International Report from the 2009/2010 Survey; WHO Regional Office for Europe: Copenhagen, Denmark, 2012; Available online: http://www.euro.who.int/en/countries/armenia/publications/social-determinants-of-health-and-well-being-among-young-people.-health-behaviour-in-school-aged-children-hbsc-study/key-findings-from-the-health-behaviour-in-school-aged-children-hbsc-study-international-report-from-the-20092010-survey (accessed on 31 October 2019).
- Noble, N.; Paul, C.; Turon, H.; Oldmeadow, C. Which modifiable health risk behaviours are related? A systematic review of the clustering of Smoking, Nutrition, Alcohol and Physical activity (‘SNAP’) health risk factors. Prev. Med. 2015, 81, 16–41. [Google Scholar] [CrossRef]
- Beauchamp, A.; Backholer, K.; Magliano, D.; Peeters, A. The effect of obesity prevention interventions according to socioeconomic position: A systematic review. Obes. Rev. 2014, 15, 541–554. [Google Scholar] [CrossRef] [PubMed]
- Nunkoo, R.; Ramkissoon, H. Structural equation modelling and regression analysis in tourism research. Curr. Issues Tour. 2012, 15, 777–802. [Google Scholar] [CrossRef]
- Beaujean, A.A. Latent Variable Modeling Using R: A Step-by-Step Guide; Routledge: New York, NY, USA, 2014; pp. 38–39. [Google Scholar]
- Leech, R.M.; McNaughton, S.A.; Timperio, A. The clustering of diet, physical activity and sedentary behavior in children and adolescents: A review. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Goodman, E.; Adler, N.E.; Kawachi, I.; Frazier, A.L.; Huang, B.; Colditz, G.A. Adolescents’ perceptions of social status: Development and evaluation of a new indicator. Pediatrics 2001, 108, e31. [Google Scholar] [CrossRef]
- VanderWeele, T.J. Invited commentary: Structural equation models and epidemiologic analysis. Am. J. Epidemiol. 2012, 176, 608–612. [Google Scholar] [CrossRef]
- Hall, D.M.B.; Cole, T.J. What use is the BMI? Arch. Dis. Child. 2006, 91, 283–286. [Google Scholar] [CrossRef]

| 2002 n = 1596 | 2017 n = 1534 | |
|---|---|---|
| Boys | 818 (51.3) | 734 (47.8) |
| Age; years, mean (SD a) | 15.9 (0.3) | 15.8 (0.3) |
| Weight; kg, mean (SD) | 62.4 (11.1) | 63.5 (11.4) |
| Height; cm, mean (SD) | 171.6 (8.5) | 171.9 (8.6) |
| BMIb; mean (SD) | 21.1 (3.0) | 21.4 (3.1) |
| SSSc | ||
| Poor | 57 (3.6) | 62 (4.0) |
| Average | 620 (38.9) | 469 (30.6) |
| Good | 842 (52.8) | 832 (54.2) |
| Very good | 77 (4.8) | 171 (10.7) |
| Sodasd | ||
| Seldom/never | 169 (10.6.) | 437 (28.5) |
| 1–6 glasses weekly | 837 (52.4) | 893 (58.2) |
| 1 glass daily | 234 (14.7) | 111 (7.2) |
| 2–3 glasses daily | 235(14.7) | 70 (4.6) |
| ≥4 glasses daily | 121 (7.6) | 23 (1.5) |
| Smokinge | ||
| Never | 993 (62.2) | 1336 (87.1) |
| Used to, but quit | 151 (9.5) | 92 (6.0) |
| Occasionally | 236 (14.8) | 97 (6.3) |
| Daily | 216 (13.5) | 9 (0.6) |
| Snufff | ||
| Never | 1337 (83.8) | 1310 (85.4) |
| Used to, but quit | 78 (4.9) | 89 (5.8) |
| Occasionally | 142 (8.9) | 75 (4.9) |
| Daily | 39 (2.4) | 60 (3.9) |
| Alcoholg | ||
| No | 209 (13.0) | 650 (42.4) |
| Yes | 1397 (87.0) | 884 (57.6) |
| Exerciseh | ||
| 0 | 150 (9.4) | 149 (9.7) |
| 1–2 | 362 (22.7) | 346 (22.6) |
| 3–4 | 417 (26.1) | 308 (20.1) |
| 5–7 | 362 (22.7) | 352 (22.9) |
| 8–10 | 190 (11.9) | 227 (14.8) |
| ≥11 | 115 (7.2) | 152 (9.9) |
| SSS a | 2002 | 2017 |
|---|---|---|
| Poor | 1.23 (0.42, 2.03) | 0.03 (−0.80, 0.85) |
| Average | 0 (Reference) | 0 (Reference) |
| Good | 0.04 (−0.27, 0.34) | −0.48 (−0.84, −0.13) |
| Very good | 0.17 (−0.53, 0.87) | −0.58 (−1.13, −0.04) |
| BMI a | SSS b | Soda c | Smoking d | Snuff e | Alcohol f | |
|---|---|---|---|---|---|---|
| BMI a | ||||||
| SSS b | −0.06 * | |||||
| Soda c | −0.03 | −0.02 | ||||
| Smoking d | 0.05 | −0.08 ** | 0.13 *** | |||
| Snuff e | 0.04 | −0.06 * | 0.13 *** | 0.68 *** | ||
| Alcohol f | 0.05 | −0.08 ** | 0.15 *** | 0.31 *** | 0.32 *** | |
| Exercise g | −0.05 | 0.15 *** | −0.06 * | −0.09 *** | −0.07 ** | −0.07 ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bjertnaes, A.A.; Schwinger, C.; Juliusson, P.B.; Strand, T.A.; Holten-Andersen, M.N.; Bakken, K.S. Health-Related Behaviors in Adolescents Mediate the Association between Subjective Social Status and Body Mass Index. Int. J. Environ. Res. Public Health 2020, 17, 7307. https://doi.org/10.3390/ijerph17197307
Bjertnaes AA, Schwinger C, Juliusson PB, Strand TA, Holten-Andersen MN, Bakken KS. Health-Related Behaviors in Adolescents Mediate the Association between Subjective Social Status and Body Mass Index. International Journal of Environmental Research and Public Health. 2020; 17(19):7307. https://doi.org/10.3390/ijerph17197307
Chicago/Turabian StyleBjertnaes, Asborg A., Catherine Schwinger, Petur B. Juliusson, Tor A. Strand, Mads N. Holten-Andersen, and Kjersti S. Bakken. 2020. "Health-Related Behaviors in Adolescents Mediate the Association between Subjective Social Status and Body Mass Index" International Journal of Environmental Research and Public Health 17, no. 19: 7307. https://doi.org/10.3390/ijerph17197307
APA StyleBjertnaes, A. A., Schwinger, C., Juliusson, P. B., Strand, T. A., Holten-Andersen, M. N., & Bakken, K. S. (2020). Health-Related Behaviors in Adolescents Mediate the Association between Subjective Social Status and Body Mass Index. International Journal of Environmental Research and Public Health, 17(19), 7307. https://doi.org/10.3390/ijerph17197307







