Herlyn-Werner-Wunderlich Syndrome: Comparison of Two Cases
Abstract
1. Introduction
2. Case Reports
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Aveiro, A.C.; Miranda, V.; Cabral, A.J.; Nunes, S.; Paulo, F.; Freitas, C. Herlyn-Werner-Wunderlich syndrome: A rare cause of pelvic pain in adolescent girls. BMJ Case Rep. 2011, 2011, bcr0420114147. [Google Scholar] [CrossRef]
- Robbins, J.B.; Broadwell, C.; Chow, L.C.; Parry, J.P.; Sadowski, E.A. Müllerian duct anomalies: Embryological development, classification, and MRI assessment. J. Magn. Reson. Imaging 2015, 41, 1–12. [Google Scholar] [CrossRef]
- Nishu, D.S.; Uddin, M.M.; Akter, K.; Akter, S.; Sarmin, M.; Begum, S. Herlyn-Werner-Wunderlich syndrome presenting with dysmenorrhea: A case report. J. Med. Case Rep. 2019, 13, 323. [Google Scholar] [CrossRef]
- Burgis, J. Obstructive Müllerian anomalies’: Case report, diagnosis, and management. Am. J. Obstet. Gynecol. 2001, 185, 338–344. [Google Scholar] [CrossRef]
- Fascilla, F.D.; Olivieri, C.; Cannone, R.; De Palma, D.; Manosperta, F.; Costantino, A.S.; Carugno, J.; Vicino, M.; Cicinelli, E.; Bettocchi, S. In-office Hysteroscopic Treatment of Herlyn-Werner-Wunderlich Syndrome: A Case Series. J. Minim. Invasive Gynecol. 2020. [Google Scholar] [CrossRef]
- Tuna, T.; Estevão-Costa, J.; Ramalho, C.; Fragoso, A.C. Herlyn-Werner-Wunderlich Syndrome: Report of a Prenatally Recognised Case and Review of the Literature. Urology 2019, 125, 205–209. [Google Scholar] [CrossRef]
- Fachin, C.G.; Rocha, J.L.A.S.; Maltoni, A.A.; das Chagas Lima, R.L.; Zendim, V.A.; Agulham, M.A.; Tsouristakis, A.; dos Santos Dias, A.I.B. Herlyn-Werner-Wunderlich syndrome: Diagnosis and treatment of an atypical case and review of literature. Int. J. Surg. Case Rep. 2019, 63, 129–134. [Google Scholar] [CrossRef]
- Fedder, J. Case Report: Uterus Didelphys Associated with Duplex Kidneys and Ureters. Acta Obstet. Gynecol. Scand. 1990, 69, 665–666. [Google Scholar] [CrossRef]
- Bajaj, S.; Misra, R.; Thukral, B.; Gupta, R. OHVIRA: Uterus didelphys, blind hemivagina and ipsilateral renal agenesis: Advantage MRI. J. Hum. Reprod. Sci. 2012, 5, 67. [Google Scholar] [CrossRef]
- Piccinini, P.S.; Doski, J. Herlyn-Werner-Wunderlich syndrome: A case report [Síndrome de Herlyn-Werner-Wunderlich: Relato de caso]. Rev. Bras. Ginecol. Obstet. 2015, 37, 192–196. [Google Scholar] [CrossRef]
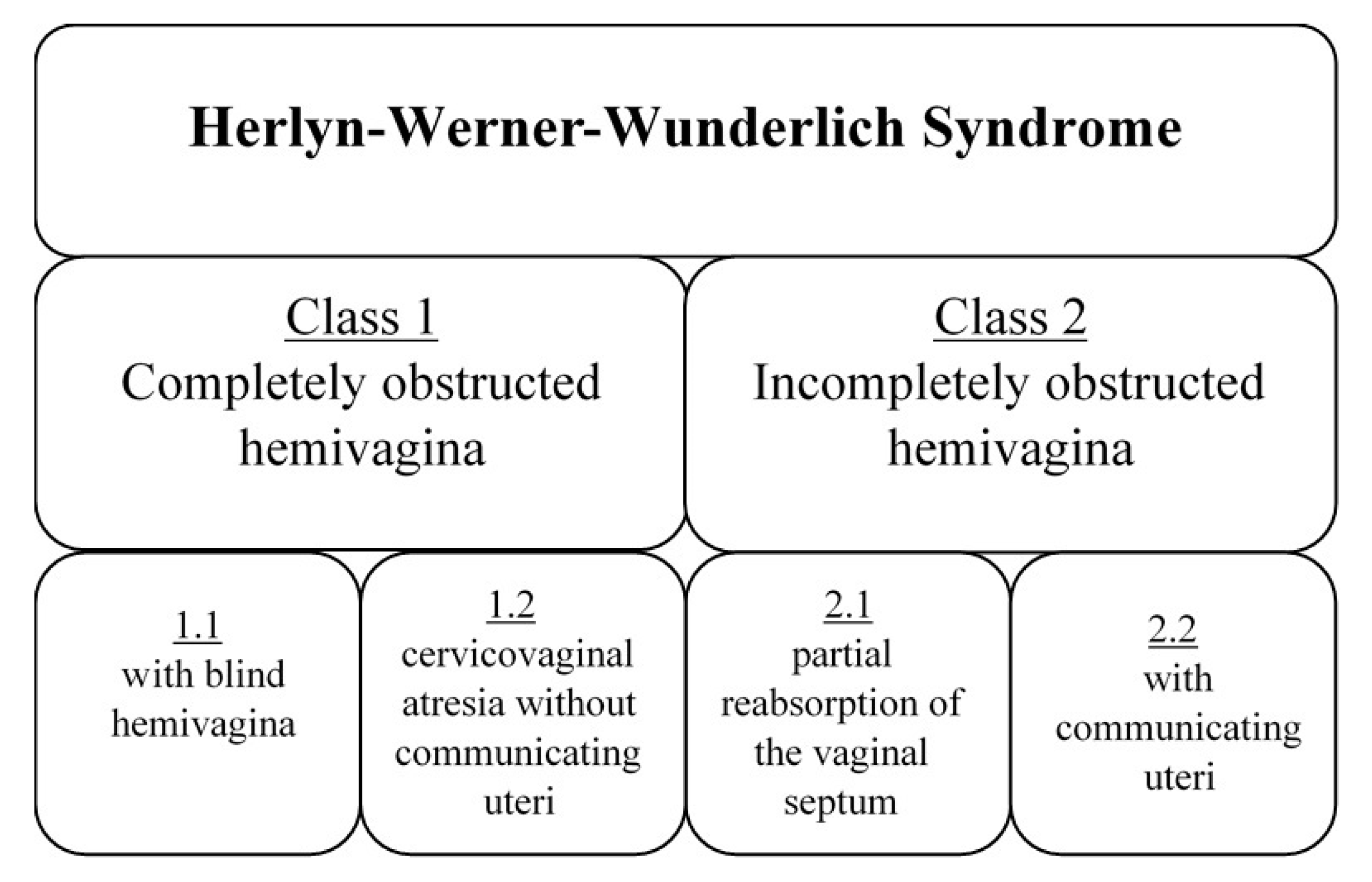
- Zhu, L.; Chen, N.; Tong, J.L.; Wang, W.; Zhang, L.; Lang, J.H. New classification of herlyn-werner-wunderlich syndrome. Chin. Med. J. 2015, 128, 222. [Google Scholar] [CrossRef] [PubMed]
- Jindal, G.; Kachhawa, S.; Meena, G.L.; Dhakar, G. Uterus didelphys with unilateral obstructed hemivagina with hematometrocolpos and hematosalpinx with ipsilateral renal agenesis. J. Hum. Reprod. Sci. 2009, 2, 87. [Google Scholar] [CrossRef]
- Troiano, R.N. Magnetic Resonance Imaging of Mullerian Duct Anomalies of the Uterus. Top. Magn. Reson. Imaging 2003, 14, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Acién, P.; Acién, M.; Sánchez-Ferrer, M. Complex malformations of the female genital tract. New types and revision of classification. Hum. Reprod. 2004, 19, 2377–2384. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, M.; Esmailzadeh, A. An unusual appearance of the post-pubertal herlyn-werner-wunderlich syndrome with acute abdominal pain: A case report. Int. J. Reprod. Biomed. 2019, 17, 851. [Google Scholar] [CrossRef]
- Grimbizis, G.F.; Gordts, S.; Di Spiezio Sardo, A.; Brucker, S.; De Angelis, C.; Gergolet, M.; Li, T.C.; Tanos, V.; Brölmann, H.; Gianaroli, L.; et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum. Reprod. 2013. [Google Scholar] [CrossRef]
- Grimbizis, G.F.; Di Spiezio Sardo, A.; Saravelos, S.H.; Gordts, S.; Exacoustos, C.; Van Schoubroeck, D.; Bermejo, C.; Amso, N.N.; Nargund, G.; Timmerman, D.; et al. The Thessaloniki ESHRE/ESGE consensus on diagnosis of female genital anomalies. Hum. Reprod. 2016, 31, 2–7. [Google Scholar] [CrossRef]
- Zurawin, R.K.; Dietrich, J.E.; Heard, M.J.; Edwards, C.L. Didelphic uterus and obstructed hemivagina with renal agenesis: Case report and review of the literature. J. Pediatric Adolesc. Gynecol. 2004, 17, 137–141. [Google Scholar] [CrossRef]
- Shavell, V.I.; Montgomery, S.E.; Johnson, S.C.; Diamond, M.P.; Berman, J.M. Complete septate uterus, obstructed hemivagina, and ipsilateral renal anomaly: Pregnancy course complicated by a rare urogenital anomaly. Arch. Gynecol. Obstet. 2009, 280, 449–452. [Google Scholar] [CrossRef]
- Gupta, N.; Gandhi, D.; Gupta, S.; Goyal, P.; Li, S.; Kumar, Y. A Variant of Herlyn-Werner-Wunderlich Syndrome Presenting with Acute Abdomen: A Case Report and Review of Literature. Glob. Pediatric Health 2018, 5. [Google Scholar] [CrossRef]
- Smith, N.A.; Laufer, M.R. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: Management and follow-up. Fertil. Steril. 2007, 87, 918–922. [Google Scholar] [CrossRef] [PubMed]
- Mandava, A.; Prabhakar, R.R.; Smitha, S. OHVIRA Syndrome (obstructed hemivagina and ipsilateral renal anomaly) with Uterus Didelphys, an Unusual Presentation. J. Pediatric Adolesc. Gynecol. 2012, 25, e23–e25. [Google Scholar] [CrossRef] [PubMed]
- Jarząbek, G.; Friebe, Z.; Szafińska, A. Psychological problems affecting patients with congenital malformations of genital organs. Seksuol. Pol. 2004, 2, 5–10. [Google Scholar]

| Patient | Age of Diagnosis | Age of Menarche | Symptoms | Examination | Obstructed Hemivagina/Renal Agenesis | Surgical Interventions |
|---|---|---|---|---|---|---|
| 17-year-old | 17 years | 13 years | Acute lower abdominal pain, dysmenorrhea | Vaginal mass, pyohematocolpos, pyohematometra | L/L | Laparoscopy, vaginal septotomy, resection of vaginal septum, extension of hemivaginal entry (twice) |
| 13-year-old | 13 years | 12 years | Polymenorrhoea, dysmenorrhea | Vaginal mass, hematocolpos | R/R | Laparoscopy, vaginal septotomy, resection of vaginal septum, extension of hemivaginal entry (twice) |
| Piccinini et al. [10] | 13 years | 11 years | Episodic perineal and rectal pain, abdominal fullness unrelated to eating | Abdominal mass, hydro/hemato-metrocolpos | L/L | Longitudinal vaginal septotomy, drainage of left tubo-ovarian abscess (on postoperative day 6) |
| Jindal et al. [12] | 14 years | 12 years | Recurrent pelvic pain (mainly at the time of menses), increasing lower abdominal swelling since menarche | Cystic mass arising from the pelvis, hematometro-colpos, hydrosalpinx | R/R | Vaginal septotomy, laparoscopy |
| Ghasemi et al. [15] | 13 years | 12 years | Acute abdominal pain, dysmenorrhea, fever, chills, nausea | Generalized abdominal tenderness, mild vaginal bleeding and right lateral vaginal wall bulging, cystic mass close to the right ovary, cystic mass in the right adnexa, hematocolpos, hematosalpinx, pyocolpos | R/R | Cutting the closed end of the hemilateral obstruction of the vagina, resection of vaginal septum, laparotomy (twice—during the second: appendectomy, right salpingectomy, entrolysis, abscess drainage) |
| Aveiro et al. [1] | 13 years | 13 years (5 months before) | Right lower quadrant and hypogastric pain, nausea, vomiting, dysmenorrhoea | Tenderness on right lower quadrant and hypogastric palpation, hematocolpos | R/R | Resection of the vaginal septum |
| Mandava et al. [22] | 14 years | 11 years | Acute retention of urine, fever, vomiting, lower abdominal pain | Pelvic mass palpable up to the level of the umbilicus, hematometro-colpos and hematosalpinx | L/L | Laparoscopy, resection of the vaginal septum, drainage of hematometro-colpos and hematosalpinx |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kozłowski, M.; Nowak, K.; Boboryko, D.; Kwiatkowski, S.; Cymbaluk-Płoska, A. Herlyn-Werner-Wunderlich Syndrome: Comparison of Two Cases. Int. J. Environ. Res. Public Health 2020, 17, 7173. https://doi.org/10.3390/ijerph17197173
Kozłowski M, Nowak K, Boboryko D, Kwiatkowski S, Cymbaluk-Płoska A. Herlyn-Werner-Wunderlich Syndrome: Comparison of Two Cases. International Journal of Environmental Research and Public Health. 2020; 17(19):7173. https://doi.org/10.3390/ijerph17197173
Chicago/Turabian StyleKozłowski, Mateusz, Katarzyna Nowak, Dominika Boboryko, Sebastian Kwiatkowski, and Aneta Cymbaluk-Płoska. 2020. "Herlyn-Werner-Wunderlich Syndrome: Comparison of Two Cases" International Journal of Environmental Research and Public Health 17, no. 19: 7173. https://doi.org/10.3390/ijerph17197173
APA StyleKozłowski, M., Nowak, K., Boboryko, D., Kwiatkowski, S., & Cymbaluk-Płoska, A. (2020). Herlyn-Werner-Wunderlich Syndrome: Comparison of Two Cases. International Journal of Environmental Research and Public Health, 17(19), 7173. https://doi.org/10.3390/ijerph17197173





