The Adoption of Preventive Behaviors during the COVID-19 Pandemic in China and Israel
Abstract
1. Introduction
2. Literature Review
2.1. Confidence
2.2. Complacency
2.3. Constraints
3. Methodology
3.1. Data Collection
3.2. The Study’s Variables
3.2.1. Confidence in Social Institutions
3.2.2. Complacency
3.2.3. Constraints
3.2.4. Avoidant Behavior
3.3. Data Analysis
4. Results
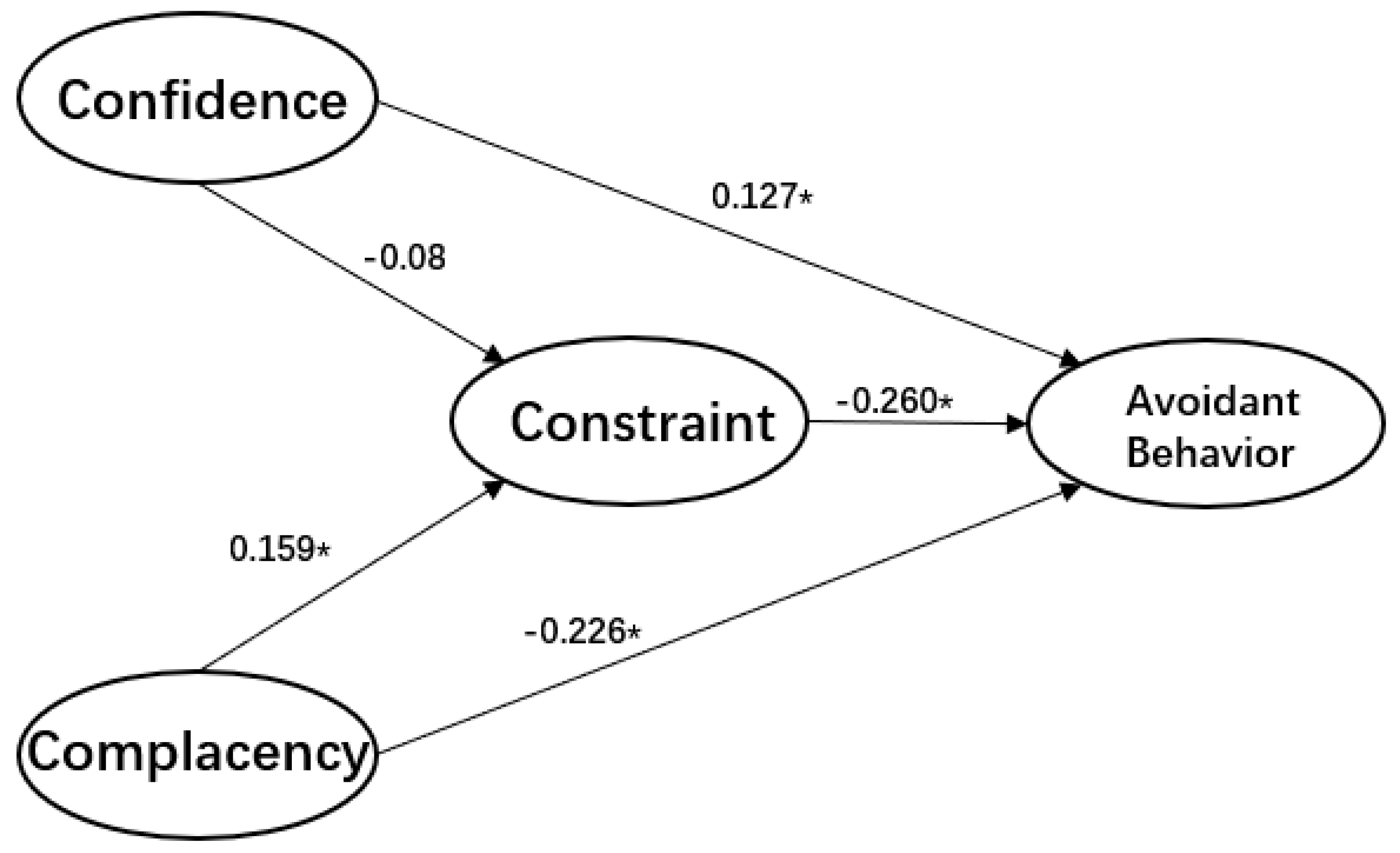
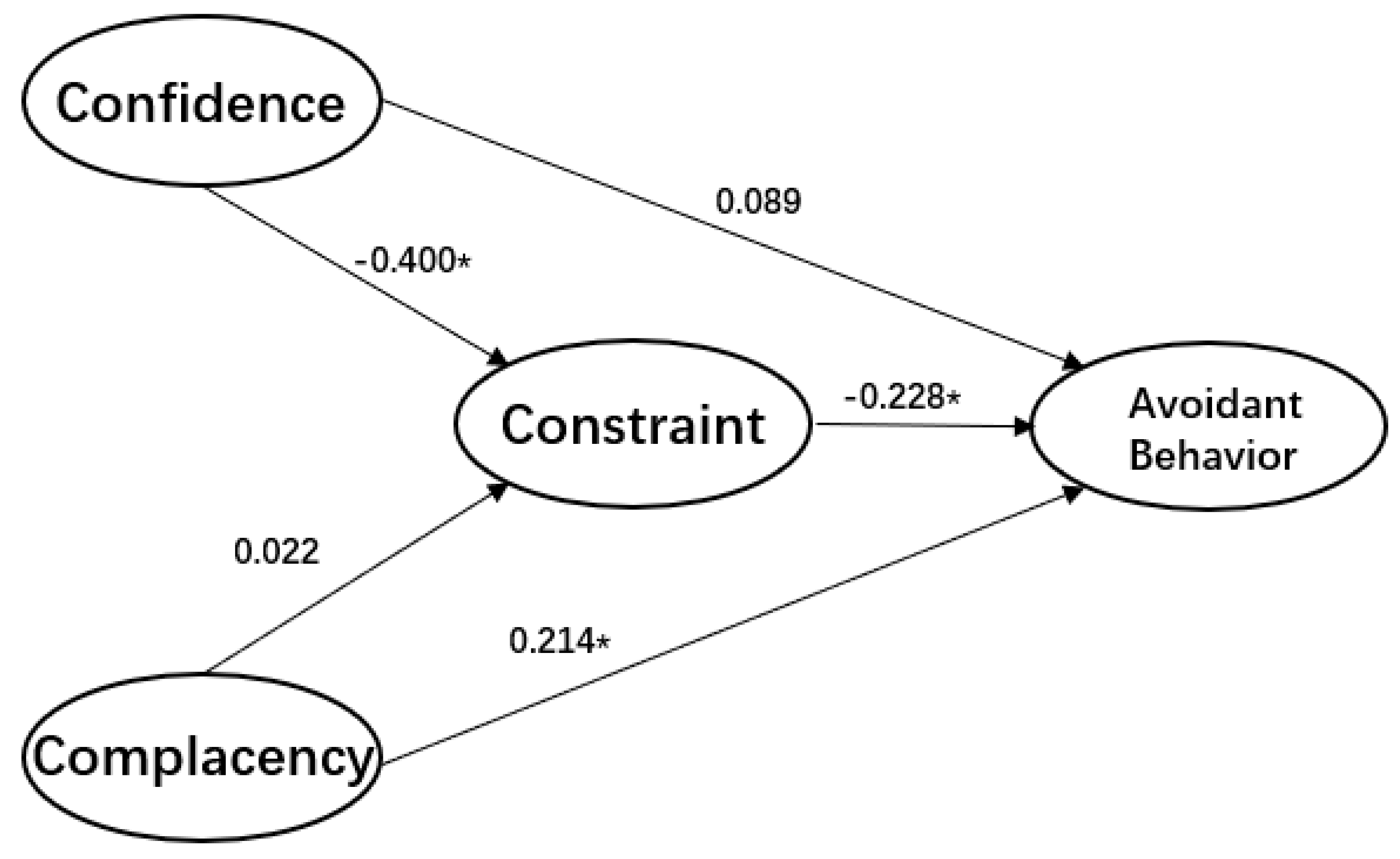
Multivariate Analysis
5. Discussion
6. Limitations
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Timeline-COVID-19. Available online: https://www.who.int/news-room/detail/29-06-2020-covidtimeline (accessed on 27 April 2020).
- Funk, S.; Salathé, M.; Jansen, V.A. Modelling the influence of human behaviour on the spread of infectious diseases: A review. J. R. Soc. Interface 2010, 7, 1247–1256. [Google Scholar] [CrossRef]
- Smith, R.D. Responding to global infectious disease outbreaks: lessons from SARS on the role of risk perception, communication and management. Soc. Sci. Med. 2006, 63, 3113–3123. [Google Scholar] [CrossRef]
- Smith, R.D.; Keogh-Brown, M.R.; Barnett, T.; Tait, J. The economy-wide impact of pandemic influenza on the UK: a computable general equilibrium modelling experiment. BMJ 2009, 339, b4571. [Google Scholar] [CrossRef]
- Green, L.W.; Kreuter, M.; Deeds, S.G.; Partridge, K.B. Health education planning: A diagnostic approach. In Health Education Planning: A Diagnostic Approach; Mayfield publishing: Mountain View, CA, USA, 1980; p. 306. [Google Scholar]
- Slater, M.; Flora, J. Is Health Behavior Consumer Behavior? Health Behavior Determinants, Audience Segmentation, and Designing Media Health Campaigns. In Attention, Attitude, and Affect in Response to Advertising; Psychology Press: London, UK, 2019; pp. 273–285. [Google Scholar]
- World Health Organization. Novel coronavirus–China. Available online: http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/ (accessed on 19 January 2020).
- Middlekauff, G.W. Cognitive-Behavior Modification: An Integrative Approach. Am. J. Psychiatry 1978, 135, 878-a. [Google Scholar] [CrossRef]
- Kraus, B.; Kitayama, S. Interdependent self-construal predicts emotion suppression in Asian Americans: An electro-cortical investigation. Biol. Psychol. 2019, 146, 107733. [Google Scholar] [CrossRef]
- Triandis, H.C. Individualism and Collectivism; Routledge: New York, NY, USA, 2018. [Google Scholar]
- Kitayama, S.; Park, J.; Miyamoto, Y.; Date, H.; Boylan, J.M.; Markus, H.R.; Karasawa, M.; Kawakami, N.; Coe, C.L.; Love, G.D.; et al. Behavioral Adjustment Moderates the Link Between Neuroticism and Biological Health Risk: A U.S.-Japan Comparison Study. Pers. Soc. Psychol. Bull. 2018, 44, 809–822. [Google Scholar] [CrossRef]
- Gelfand, M.J.; Raver, J.L.; Nishii, L.; Leslie, L.M.; Lun, J.; Lim, B.C.; Duan, L.; Almaliach, A.; Ang, S.; Arnadottir, J.; et al. Differences Between Tight and Loose Cultures: A 33-Nation Study. Science 2011, 332, 1100–1104. [Google Scholar] [CrossRef] [PubMed]
- Gelfand, M.J.; Harrington, J.R.; Jackson, J.C. The strength of social norms across human groups. Perspect. Psychol. Sci. 2017, 12, 800–809. [Google Scholar] [CrossRef] [PubMed]
- MacDonald NE, SAGE Working Group on VaccineHesitancy. Vaccinehesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Kelvin, D.J.; Rubino, S. Fear of the novel coronavirus. J. Infect. Dev. Ctries. 2020, 14, 1–2. [Google Scholar] [CrossRef] [PubMed]
- The Importance of Confidence, Complacency, and Convenience for Influenza Vaccination among Key Risk Groups in Large Urban Areas of Peru. Available online: https://doi.org/10.1080/21645515.2020.1777821 (accessed on 7 September 2020).
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Gilson, L. Trust and the development of health care as a social institution. Soc. Sci. Med. 2003, 56, 1453–1468. [Google Scholar] [CrossRef]
- Ward, P.R. Improving access to, use of, and outcomes from public health programs: the importance of building and maintaining trust with patients/clients. Front. Public Health 2017, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Mishler, W.; Rose, R. What are the origins of political trust? Testing institutional and cultural theories in post-communist societies. Comp. Political Stud. 2001, 34, 30–62. [Google Scholar] [CrossRef]
- Brewer, N.T.; Cuite, C.L.; Herrington, J.E.; Weinstein, N.D. Risk compensation and vaccination: Can getting vaccinated cause people to engage in risky behaviors? Ann. Behav. Med. 2007, 34, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Cairns, G.; De Andrade, M.; Macdonald, L. Reputation, Relationships, Risk Communication, and the Role of Trust in the Prevention and Control of Communicable Disease: A Review. J. Health Commun. 2013, 18, 1550–1565. [Google Scholar] [CrossRef]
- Fadda, M.; Galimberti, E.; Romanò, L.; Faccini, M.; Senatore, S.; Zanetti, A.; Schulz, P.J. Validation of a scale to measure parental psychological empowerment in the vaccination decision. J. Public Health Res. 2017, 6, 100–107. [Google Scholar] [CrossRef]
- Giddens, A. The Consequences of Modernity; John Wiley Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Bachmann, R. Conclusion: Trust–conceptual aspects of a complex phenomenon. Trust. Organ. 1998, 298–322. [Google Scholar]
- Rubin, G.J.; Amlôt, R.; Page, L.; Wessely, S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: Cross sectional telephone survey. BMJ 2009, 339, b2651. [Google Scholar] [CrossRef]
- Van Der Weerd, W.; Timmermans, D.R.M.; Beaujean, D.J.M.A.; Oudhoff, J.P.; Van Steenbergen, J. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in the Netherlands. BMC Public Health 2011, 11, 575. [Google Scholar] [CrossRef]
- Blair, R.A.; Morse, B.; Tsai, L.L. Public health and public trust: Survey evidence from the Ebola Virus Disease epidemic in Liberia. Soc. Sci. Med. 2017, 172, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Fischhoff, B.; Wong-Parodi, G.; Garfin, D.R.; Holman, E.A.; Silver, R.C. Public Understanding of Ebola Risks: Mastering an Unfamiliar Threat. Risk Anal. 2017, 38, 71–83. [Google Scholar] [CrossRef] [PubMed]
- Moxham-Hall, V.; Strang, L. Public Opinion and Trust in Government during a Public Health Crisis. Available online: https://www.kcl.ac.uk/news/public-opinion-and-trust-in-government-during-a-public-health-crisis (accessed on 22 April 2020).
- Meltzer, M.I.; Cox, N.J.; Fukuda, K. The economic impact of pandemic influenza in the United States: Priorities for intervention. Emerg. Infect. Dis. 1999, 5, 659. [Google Scholar] [CrossRef] [PubMed]
- Sibley, C.G.; Greaves, L.M.; Satherley, N.; Wilson, M.S.; Overall, N.C.; Lee, C.H.; Milojev, P.; Bulbulia, J.; Osborne, D.; Milfont, T.L.; et al. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am. Psychol. 2020, 75, 618–630. [Google Scholar] [CrossRef] [PubMed]
- Dussaillant, F.; Guzmán, E. Trust via disasters: the case of Chile’s 2010 earthquake. Disasters 2014, 38, 808–832. [Google Scholar] [CrossRef] [PubMed]
- Van Prooijen, J.W.; Van Dijk, E. When consequence size predicts belief in conspiracy theories: The moderating role of perspective taking. J. Exp. Soc. Psychol. 2014, 55, 63–73. [Google Scholar] [CrossRef]
- Ibuka, Y.; Chapman, G.B.; Meyers, L.A.; Li, M.; Galvani, A.P. The dynamics of risk perceptions and precautionary behavior in response to 2009 (H1N1) pandemic influenza. BMC Infect. Dis. 2010, 10, 296. [Google Scholar] [CrossRef]
- Drottz-Sjöberg, B.-M. Perception of Risk. Studies of Risk Attitudes, Perceptions and Definitions; Stockholm School of Economics: Stockholm, Sweden, 1991. [Google Scholar]
- Van der Pligt, J. Risk perception and self-protective behavior. Eur. Psychol. 1996, 1, 34–43. [Google Scholar] [CrossRef]
- Loewenstein, G.F.; Weber, E.U.; Hsee, C.K.; Welch, N. Risk as feelings. Psychol. Bull. 2001, 127, 267. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Judgment under uncertainty: heuristics and biases. Science 1974, 185, 1124–1131. [Google Scholar] [CrossRef]
- Folkes, V.S. The availability heuristic and perceived risk. J. Consum. Res. 1988, 15, 13–23. [Google Scholar] [CrossRef]
- Sjöberg, L. The methodology of risk perception research. Qual. Quant. 2000, 34, 407–418. [Google Scholar] [CrossRef]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Fuchs, R. Self-efficacy and health behaviours. Predict. Health Behav Res PractSoc Cogn Models 1996, 163–196. [Google Scholar] [CrossRef]
- Becker, M.H. The health belief model and personal health behavior. Health Educ. Monogr 1974, 2, 324–508. [Google Scholar]
- Prentice-Dunn, S.; Rogers, R.W. Protection motivation theory and preventive health: Beyond the health belief model. Health Educ. Res 1986, 1, 153–161. [Google Scholar] [CrossRef]
- Leung, G.M.; Ho, L.M.; Chan, S.K.; Ho, S.Y.; Bacon-Shone, J.; Choy, R.Y.; Fielding, R. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin. Infect. Dis. 2005, 40, 1713–1720. [Google Scholar] [CrossRef]
- Pike, J.; Shogren, J.F.; Aadland, D.; Viscusi, W.K.; Finnoff, D.; Skiba, A.; Daszak, P. Catastrophic Risk: Waking Up to the Reality of a Pandemic? Ecohealth 2020, 17, 217–221. [Google Scholar] [CrossRef]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PloS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef]
- Askelson, N.M.; Campo, S.; Lowe, J.B.; Smith, S.; Dennis, L.K.; Andsager, J. Using the theory of planned behavior to predict mothers’ intentions to vaccinate their daughters against HPV. J. Sch. Nurs. 2010, 26, 194–202. [Google Scholar] [CrossRef]
- Luszczynska, A.; Scholz, U.; Schwarzer, R. The general self-efficacy scale: multicultural validation studies. J. Psychol. 2005, 139, 439–457. [Google Scholar] [CrossRef] [PubMed]
- Sundaram, Neisha, Teck Chuan Voo, and Clarence C. Tam. Adolescent HPV vaccination: empowerment, equity and ethics. Hum. Vaccines Immunother. 2020, 16, 1835–1840. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the health belief model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Foundations of Thought and Action; Englewood Cliffs: Bergen County, NJ, USA, 1986; pp. 23–28. [Google Scholar]
- Rosenstock, I.M. Historical origins of the health belief model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Velicer, W.F.; DiClemente, C.C.; Prochaska, J.O.; Brandenburg, N. Decisional balance measure for assessing and predicting smoking status. J. Personal. Soc. Psychol. 1985, 48, 1279. [Google Scholar] [CrossRef]
- Rogers, R.W. A protection motivation theory of fear appeals and attitude change1. J. Psychol. 1975, 91, 93–114. [Google Scholar] [CrossRef]
- Yzer, M. Theory of reasoned action and theory of planned behavior. Int. Encycl. Media Eff. 2017, 50, 1–7. [Google Scholar]
- Farooq, A.; Jeske, D.; Isoaho, J. Predicting Students’ Security Behavior Using Information-Motivation-Behavioral Skills Model. In Integrity and Internal Control in Information Systems; Dhillon, G., Karlsson, F., Hedstrom, K., Zuquete, A., Eds.; Springer Science and Business Media LLC: Berlin, Germany, 2019; pp. 238–252. [Google Scholar]
- Rappapon, J. Studies in empowerment: Introduction to the issue. Prev. in Hum. Serv. 1984, 3, 1–7. [Google Scholar] [CrossRef]
- Perkins, D.D.; Zimmerman, M.A. Empowerment theory, research, and application. Am. J. Community Psychol. 1995, 23, 569–579. [Google Scholar] [CrossRef]
- Alsulaiman, S.A.; Rentner, T.L. The Health Belief Model and Preventive Measures: A Study of the Ministry of Health Campaign on Coronavirus in Saudi Arabia. J. Int. Crisis Risk Commun. Res. 2018, 1, 3. [Google Scholar] [CrossRef]
- Farooq, A.; Laato, S.; Islam, A.N. Impact of online information on self-isolation intention during the COVID-19 pandemic: Cross-sectional study. J. Med. Internet Res. 2020, 22, e19128. [Google Scholar] [CrossRef] [PubMed]
- Cahyanto, I.; Wiblishauser, M.; Pennington-Gray, L.; Schroeder, A. The dynamics of travel avoidance: The case of Ebola in the US. Tour. Manag. Perspect. 2016, 20, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Bults, M.; Beaujean, D.J.M.A.; De Zwart, O.; Kok, G.; Van Empelen, P.; Van Steenbergen, J.; Richardus, J.H.; Voeten, H.A. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: results of three consecutive online surveys. BMC Public Health 2011, 11, 2. [Google Scholar] [CrossRef]
- Zydney, J.M.; Hai-Jew, S.; Renninger, K.A.; List, A.; Hardy, I.; Koerber, S.; Lattal, K.A.; Farrell, J.M.; Fretwell, H.; Reiss, N.; et al. Social Cognitive Theory. Encycl. Sci. Learn. 2012, 2, 3095. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191. [Google Scholar] [CrossRef]
- Durham, D.P.; Casman, E.A.; Albert, S.M. Deriving behavior model parameters from survey data: Self-protective behavior adoption during the 2009–2010 influenza a (H1N1) pandemic. Risk Anal. Int. J. 2012, 32, 2020–2031. [Google Scholar] [CrossRef]
- Liao, Q.; Cowling, B.; Lam, W.T.; Ng, M.W.; Fielding, R. Situational awareness and health protective responses to pandemic influenza A (H1N1) in Hong Kong: A cross-sectional study. PLoS ONE 2010, 5, e13350. [Google Scholar] [CrossRef]
- Johnson, R.A.; Wichern, D.W. Applied Multivariate Correspondence Analysis; Prentice Hall International, Inc.: Hoboken, NJ, USA, 2007. [Google Scholar]
- Cowling, B.J.; Ng, D.M.W.; Ip, D.; Liao, Q.; Lam, W.W.T.; Wu, J.T.; Lau, J.T.F.; Griffiths, S.; Fielding, R. Community Psychological and Behavioral Responses through the First Wave of the 2009 Influenza A(H1N1) Pandemic in Hong Kong. J. Infect. Dis. 2010, 202, 867–876. [Google Scholar] [CrossRef]
- Champion, V.L.; Skinner, C.S. The health belief model. Health behavior and health education: Theory Res. Pract. 2008, 4, 45–65. [Google Scholar]
- Champion, V.L.; Monahan, P.O.; Springston, J.K.; Russell, K.; Zollinger, T.W.; Saywell Jr, R.M.; Maraj, M. Measuring mammography and breast cancer beliefs in African American women. J. Health Psychol. 2008, 13, 827–837. [Google Scholar] [CrossRef]
- Janz, N.K.; Becker, M.H. The health belief model: A decade later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, R.F.; Leary, M.R. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol. Bull. 1995, 117, 497. [Google Scholar] [CrossRef] [PubMed]
| Demographic Variable | Both | Israel | China |
|---|---|---|---|
| Sample (%) | 1406 (100%) | 703 (50%) | 703 (50%) |
| Gender | |||
| Male | 694 (49.36%) | 336 (23.90%) | 358 (25.46%) |
| Female | 712 (50.64%) | 367 (26.10%) | 345 (24.54%) |
| Age | |||
| Under 17 years old | 36 (2.56%) | 0 | 36 (2.56%) |
| 18–30 years old | 550 (39.12%) | 194 (13.8%) | 356 (25.32%) |
| 31–50 years old | 518 (36.84%) | 262 (18.63%) | 256 (18.21%) |
| 51–70 years old | 253 (17.99%) | 199 (14.15%) | 54 (3.84%) |
| Older than 70 years old | 49 (3.49%) | 48 (3.41%) | 1 (0.07%) |
| Education | |||
| No schooling completed | 28 (1.99%) | 16 (1.14%) | 12 (0.85%) |
| Primary school | 21 (1.49%) | 5 (0.36%) | 16 (1.14%) |
| Secondary school | 100 (7.11%) | 35 (2.49%) | 65 (4.62%) |
| High school or equivalent | 367 (26.10%) | 202 (14.37%) | 165 (11.74%) |
| Trade/technical/vocational training | 277 (19.70%) | 133 (9.46%) | 144 (10.24%) |
| BA | 459 (32.65%) | 209 (14.86%) | 250 (17.78%) |
| graduate | 154 (10.95%) | 103 (7.33%) | 51 (3.63%) |
| Marital status | |||
| Single | 549 (39.05%) | 221 (15.72%) | 328 (23.33%) |
| Living together | 37 (2.63%) | 13 (0.92%) | 24 (1.71%) |
| Married | 746 (53.06%) | 412 (29.3%) | 334 (23.76%) |
| Widowed | 10 (0.71%) | 6 (0.43%) | 4 (0.28%) |
| Divorced | 58 (4.13%) | 46 (3.27%) | 12 (0.85%) |
| Separated | 6 (0.43%) | 5 (0.36%) | 1 (0.07%) |
| Income | |||
| a lot below-average | 367 (26.10%) | 169 (12.02%) | 198 (14.08%) |
| a little below average income | 398 (28.31%) | 146 (10.38%) | 252 (17.92%) |
| average income | 311 (22.12%) | 135 (9.6%) | 176 (12.52%) |
| a little more than average | 178 (12.66%) | 122 (8.68%) | 56 (3.98%) |
| significantly higher than average | 69 (4.91%) | 48 (3.41%) | 21 (1.49%) |
| missing data | 83 (5.90%) | 83 (5.9%) | 0 |
| Latent Variable | Indicator | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Complacency | 1 | Susceptibility 1 | 3.09 | 1.088 | 1.184 | 0.534 | 0.396 | 0.435 | −0.113 | −0.044 | −0.022 | −0.056 | 0.034 | 0.034 | 0.050 |
| Cronbach’s α = 0.771 | 2 | Susceptibility 2 | 2.92 | 1.141 | 0.430 ** | 1.302 | 0.520 | 0.764 | 0.068 | 0.110 | 0.036 | −0.064 | −0.003 | 0.034 | 0.051 |
| 3 | Seriousness 1 | 3.48 | 1.071 | 0.340 ** | 0.425 ** | 1.147 | 0.767 | −0.017 | −0.001 | −0.008 | −0.012 | 0.023 | 0.035 | 0.027 | |
| 4 | Seriousness 2 | 2.88 | 1.163 | 0.343 ** | 0.576 ** | 0.616 ** | 1.354 | 0.145 | 0.209 | 0.069 | −0.013 | −0.052 | 0.010 | 0.031 | |
| constraint | 5 | Outcome expectation 1 | 1.92 | 0.946 | −0.110 ** | 0.063 | −0.017 | 0.132 ** | 0.895 | 0.512 | 0.325 | −0.025 | −0.036 | −0.016 | −0.052 |
| Cronbach’s α = 0.543 | 6 | Outcome expectation 2 | 1.97 | 0.926 | −0.044 | 0.104 ** | −0.001 | 0.194 ** | 0.585 ** | 0.857 | 0.341 | 0.017 | −0.046 | −0.007 | −0.027 |
| 7 | Efficacy expectation 1 | 2.16 | 0.879 | −0.023 | 0.036 | −0.008 | 0.068 | 0.391 ** | 0.419** | 0.773 | −0.034 | −0.086 | −0.072 | −0.088 | |
| 8 | Efficacy expectation 2 | 2.16 | 0.885 | −0.059 | −0.064 | −0.013 | −0.012 | −0.030 | 0.021 | −0.044 | 0.783 | −0.016 | −0.016 | −0.021 | |
| confidence | 9 | Confidence in government | 2.67 | 0.813 | 0.038 | −0.003 | 0.026 | −0.055 | −0.047 | −0.062 | −0.121 ** | −0.022 | 0.661 | 0.430 | 0.362 |
| Cronbach’s α = 0.851 | 10 | Confidence in hospitals | 2.55 | 0.802 | 0.039 | 0.037 | 0.041 | 0.011 | −0.021 | −0.009 | −0.103 ** | −0.022 | 0.660 ** | 0.644 | 0.472 |
| 11 | Confidence in medical workers | 2.77 | 0.791 | 0.058 | 0.056 | 0.031 | 0.034 | −0.070 | −0.036 | −0.126 ** | −0.030 | 0.563 ** | 0.744 ** | 0.626 |
| Latent Variable | Indicator | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Complacency | 1 | Susceptibility 1 | 3.72 | 1.167 | 1.363 | 0.615 | 0.590 | 0.212 | −0.057 | −0.003 | −0.079 | −0.059 | 0.003 | 0.029 | 0.017 |
| Cronbach’s α = 0.682 | 2 | Susceptibility 2 | 3.43 | 1.104 | 0.477 ** | 1.220 | 0.534 | 0.410 | −0.017 | 0.025 | −0.093 | −0.025 | 0.014 | 0.013 | 0.002 |
| 3 | Seriousness 1 | 2.60 | 1.275 | 0.397 ** | 0.379 ** | 1.625 | 0.508 | 0.118 | 0.109 | −0.051 | 0.034 | −0.008 | −0.020 | −0.031 | |
| 4 | Seriousness 2 | 2.16 | 1.125 | 0.161 ** | 0.330 ** | 0.354 ** | 1.265 | 0.178 | 0.351 | 0.011 | 0.119 | −0.020 | −0.034 | −0.020 | |
| Constraint | 5 | Outcome expectation 1 | 1.62 | 0.822 | −0.059 | −0.019 | 0.113 ** | 0.192 ** | 0.675 | 0.282 | 0.211 | 0.259 | −0.078 | −0.116 | −0.068 |
| Cronbach’s α = 0.707 | 6 | Outcome expectation 2 | 1.72 | 0.830 | −0.003 | 0.027 | 0.103 ** | 0.376 ** | 0.413 ** | 0.689 | 0.233 | 0.292 | −0.088 | −0.098 | −0.079 |
| 7 | Efficacy expectation 1 | 1.88 | 0.912 | −0.074 * | −0.093 * | −0.044 | 0.011 | 0.281 ** | 0.308 ** | 0.832 | 0.397 | −0.093 | −0.130 | −0.110 | |
| 8 | Efficacy expectation 2 | 1.84 | 0.877 | −0.058 | −0.026 | 0.031 | 0.120 ** | 0.360 ** | 0.401 ** | 0.496 ** | 0.769 | −0.081 | −0.116 | −0.087 | |
| Confidence | 9 | Confidence in government | 3.71 | 0.483 | 0.005 | 0.026 | −0.013 | −0.036 | −0.197 ** | −0.219 ** | −0.210 ** | −0.192 ** | 0.234 | 0.190 | 0.171 |
| Cronbach’s α = 0.885 | 10 | Confidence in hospitals | 3.62 | 0.562 | 0.045 | 0.021 | −0.029 | −0.053 | −0.251 ** | −0.209 ** | −0.253 ** | −0.236 ** | 0.701 ** | 0.315 | 0.218 |
| 11 | Confidence in medical workers | 3.69 | 0.505 | 0.028 | 0.004 | −0.049 | −0.035 | −0.164 ** | −0.189 ** | −0.239 ** | −0.196 ** | 0.699 ** | 0.767 ** | 0.255 |
| Latent Variable | Indicator | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Complacency | 1 | Susceptibility 1 | 3.40 | 1.170 | 1.370 | 0.653 | 0.356 | 0.211 | −0.131 | −0.063 | −0.094 | −0.109 | 0.181 | 0.199 | 0.177 |
| Cronbach’s α = 0.675 | 2 | Susceptibility 2 | 3.18 | 1.151 | 0.485 ** | 1.324 | 0.415 | 0.496 | −0.012 | 0.036 | −0.064 | −0.086 | 0.138 | 0.159 | 0.143 |
| 3 | Seriousness 1 | 3.04 | 1.256 | 0.242 ** | 0.287 ** | 1.577 | 0.794 | 0.116 | 0.109 | 0.032 | 0.083 | −0.222 | −0.227 | −0.204 | |
| 4 | Seriousness 2 | 2.52 | 1.199 | 0.150 ** | 0.359 ** | 0.528 ** | 1.437 | 0.214 | 0.325 | 0.090 | 0.111 | −0.223 | −0.203 | −0.159 | |
| Constraint | 5 | Outcome expectation 1 | 1.77 | 0.898 | −0.125 ** | −0.012 | 0.103 ** | 0.199 ** | 0.806 | 0.415 | 0.289 | 0.141 | −0.135 | −0.145 | −0.129 |
| Cronbach’s α = 0.65 | 6 | Outcome expectation 2 | 1.85 | 0.888 | −0.060 * | 0.035 | 0.098 ** | 0.305 ** | 0.521 ** | 0.788 | 0.304 | 0.175 | −0.133 | −0.120 | −0.111 |
| 7 | Efficacy expectation 1 | 2.02 | 0.907 | −0.089 ** | −0.061 * | 0.028 | 0.083 ** | 0.354 ** | 0.378 ** | 0.822 | 0.204 | −0.163 | −0.176 | −0.163 | |
| 8 | Efficacy expectation 2 | 2.00 | 0.896 | −0.104 ** | −0.083 ** | 0.073 ** | 0.104 ** | 0.176 ** | 0.220 ** | 0.252 ** | 0.802 | −0.134 | −0.153 | −0.129 | |
| Confidence | 9 | Confidence in government | 3.19 | 0.848 | 0.182 ** | 0.141 ** | −0.208 ** | −0.220 ** | −0.177 ** | −0.176 ** | −0.211 ** | −0.176 ** | 0.720 | 0.589 | 0.506 |
| Cronbach’s α = 0.918 | 10 | Confidence in hospitals | 3.09 | 0.874 | 0.194 ** | 0.158 ** | −0.207 ** | −0.194 ** | −0.185 ** | −0.154 ** | −0.222 ** | −0.195 ** | 0.794 ** | 0.765 | 0.590 |
| 11 | Confidence in medical workers | 3.23 | 0.807 | 0.187 ** | 0.154 ** | −0.201 ** | −0.165 ** | −0.177 ** | −0.155 ** | −0.223 ** | −0.178 ** | 0.739 ** | 0.836 ** | 0.651 |
| No | Avoidant Behavior | Israel | China | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| 1 | Avoid arriving in places where it is known that the virus is locally transmitted | 4.43 | 1.04 | 4.65 | 0.80 |
| 2 | Do not share your towel with others | 3.84 | 1.35 | 4.63 | 0.79 |
| 3 | Maintain at least 1 metre distance between yourself and anyone who is coughing or sneezing. | 4.08 | 1.03 | 4.21 | 0.96 |
| 4 | Avoid shaking hands | 4.49 | 0.87 | 4.41 | 0.81 |
| 5 | Avoid using common utensils in the same meal. | 4.24 | 1.10 | 4.33 | 1.01 |
| 6 | Do not visit your family members and friends who do not live with you. | 4.31 | 0.88 | 4.35 | 0.83 |
| 7 | Do not going into crowded or airtight places | 4.56 | 0.74 | 4.39 | 0.82 |
| 8 | Put on facial mask when you go outside | 2.57 | 1.50 | 4.69 | 0.73 |
| 9 | Do not use public transportation | 4.33 | 1.12 | 3.93 | 1.15 |
| Original Model | Multiple-Group Analysis | |||
|---|---|---|---|---|
| Model-Fix Goodness | Israel | China | Israel | China |
| model fit | ||||
| χ2 | 646.396 | 628.974 | 1256.452 | |
| df | 165 | 166 | 333 | |
| χ2/df | 3.92 | 3.79 | 3.773 | |
| RMSEA | 0.06 | 0.06 | 0.045 | |
| GFI | 0.91 | 0.91 | 0.912 | |
| SRMR | 0.06 | 0.06 | 0.0586 | |
| Standardized coefficient | ||||
| confidence->constraints | −0.08 | −0.400 * | −0.072 | −0.400 * |
| complacency->constraints | 0.159 * | 0.022 | 0.154 * | 0.022 |
| confidence->avoidant behavior | 0.127 * | 0.089 | 0.127 * | 0.089 |
| complacency->avoidant behavior | −0.226 * | 0.214 * | −0.227 * | 0.214 * |
| constraint->avoidant behavior | −0.260 * | −0.228 * | −0.274 * | −0.228 * |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, X.-J.; Mesch, G.S. The Adoption of Preventive Behaviors during the COVID-19 Pandemic in China and Israel. Int. J. Environ. Res. Public Health 2020, 17, 7170. https://doi.org/10.3390/ijerph17197170
Liu X-J, Mesch GS. The Adoption of Preventive Behaviors during the COVID-19 Pandemic in China and Israel. International Journal of Environmental Research and Public Health. 2020; 17(19):7170. https://doi.org/10.3390/ijerph17197170
Chicago/Turabian StyleLiu, Xue-Jing, and Gustavo S. Mesch. 2020. "The Adoption of Preventive Behaviors during the COVID-19 Pandemic in China and Israel" International Journal of Environmental Research and Public Health 17, no. 19: 7170. https://doi.org/10.3390/ijerph17197170
APA StyleLiu, X.-J., & Mesch, G. S. (2020). The Adoption of Preventive Behaviors during the COVID-19 Pandemic in China and Israel. International Journal of Environmental Research and Public Health, 17(19), 7170. https://doi.org/10.3390/ijerph17197170





