Effect of Early Mobilization on Physical Function in Patients after Cardiac Surgery: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
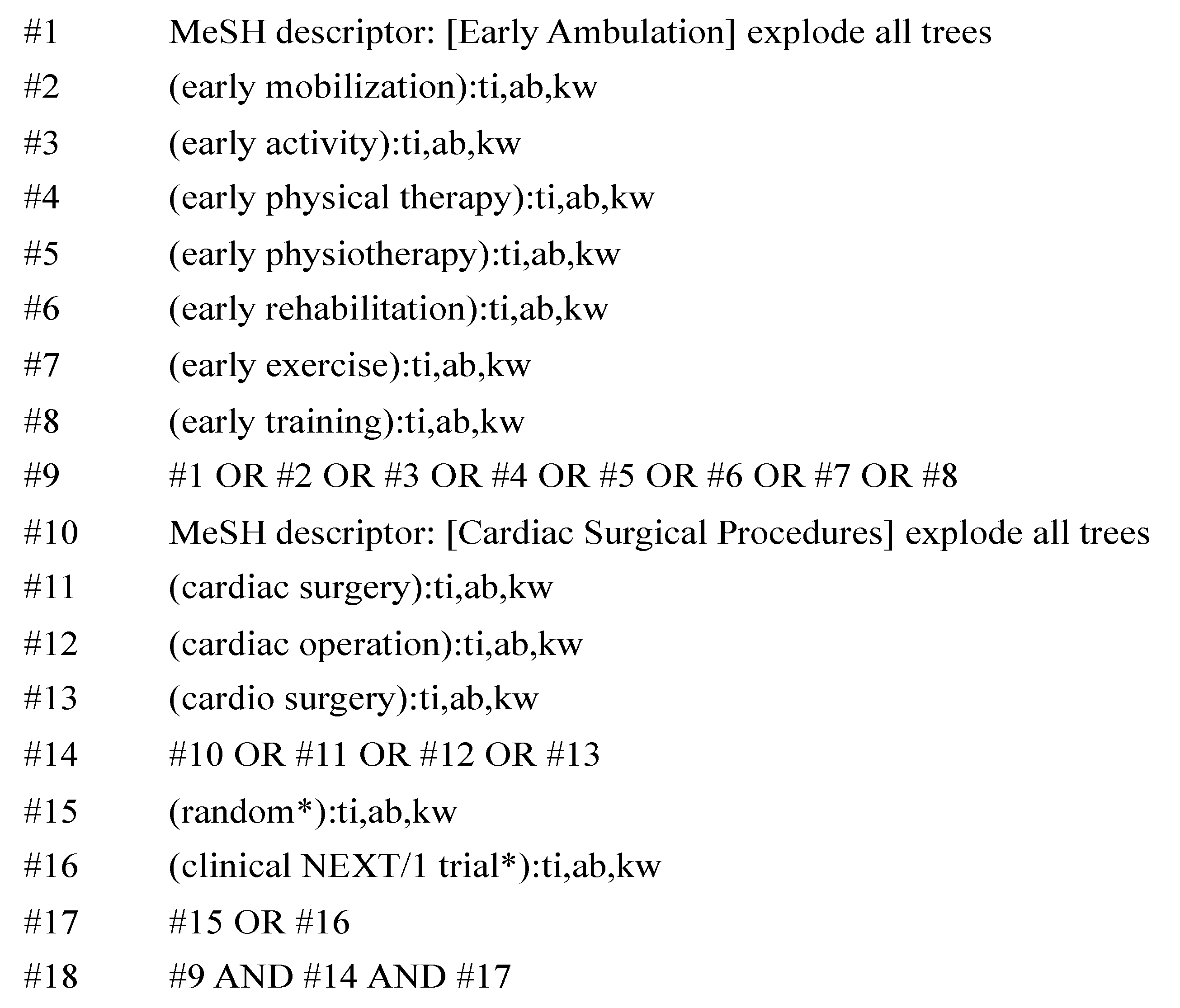
2.2. Search Strategy
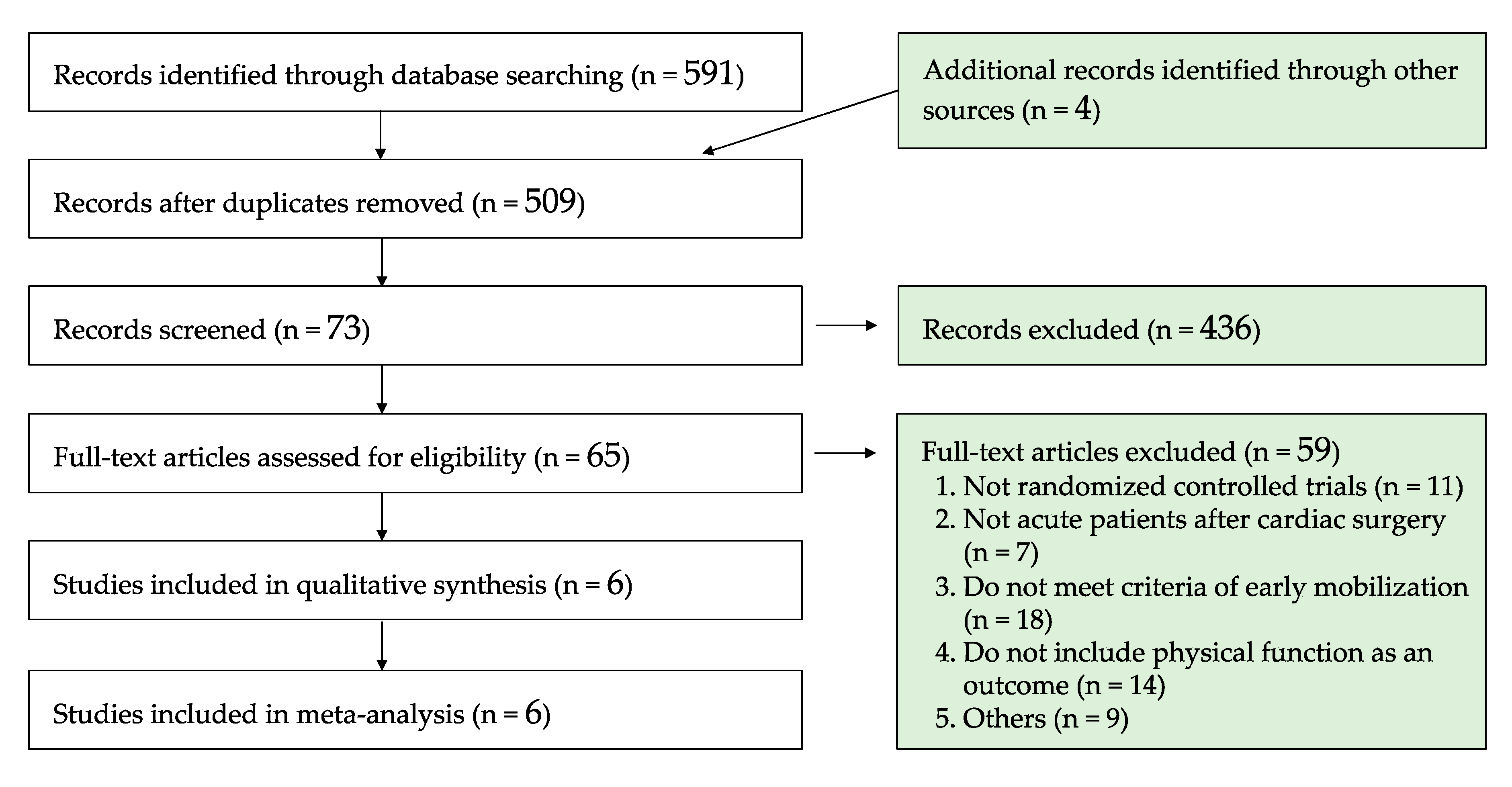
2.3. Study Selection
2.4. Data Extraction
2.5. Quality Assessment
2.6. Statistical Analysis
3. Results
3.1. Overview of Included Studies
3.2. Trend of Interventions
3.3. Risk of Bias
3.4. Meta-Analysis
4. Discussion
4.1. Comparison with Previous Studies
4.2. Possible Explanation and Implications
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef]
- Leitz, K.H.; Ziemer, G. The History of Cardiac Surgery. In Cardiac Surgery; Springer: Berlin/Heidelberg, Germany, 2017; pp. 3–31. [Google Scholar]
- Ball, L.; Costantino, F.; Pelosi, P. Postoperative complications of patients undergoing cardiac surgery. Curr. Opin. Crit. Care 2016, 22, 386–392. [Google Scholar] [CrossRef]
- Jenkins, C.D.; Jono, R.T.; Stanton, B.A. Predicting Completeness of Symptom Relief after Major Heart Surgery. Behav. Med. 1996, 22, 45–57. [Google Scholar] [CrossRef]
- Dock, W. The evil sequelae of complete bed rest. J. Am. Med. Assoc. 1944, 125, 1083–1085. [Google Scholar] [CrossRef]
- English, K.L.; Paddon-Jones, D. Protecting muscle mass and function in older adults during bed rest. Curr. Opin. Clin. Nutr. 2010, 13, 34–39. [Google Scholar] [CrossRef]
- Cameron, S.; Ball, I.; Cepinskas, G.; Choong, K.; Doherty, T.J.; Ellis, C.G.; Martin, C.M.; Mele, T.S.; Sharpe, M.; Shoemaker, J.K.; et al. Early mobilization in the critical care unit: A review of adult and pediatric literature. J. Crit. Care 2015, 30, 664–672. [Google Scholar] [CrossRef]
- Hodgson, C.L.; Berney, S.; Harrold, M.; Saxena, M.; Bellomo, R. Clinical review: Early patient mobilization in the ICU. Crit. Care 2013, 17, 207. [Google Scholar] [CrossRef]
- Zang, K.; Chen, B.; Wang, M.; Chen, D.; Hui, L.; Guo, S.; Ji, T.; Shang, F. The effect of early mobilization in critically ill patients: A meta-analysis. Nurs. Crit. Care 2019. [Google Scholar] [CrossRef]
- Schweickert, W.D.; Pohlman, M.C.; Pohlman, A.S.; Nigos, C.; Pawlik, A.J.; Esbrook, C.L.; Spears, L.; Miller, M.; Franczyk, M.; Deprizio, D.; et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet 2009, 373, 1874–1882. [Google Scholar] [CrossRef]
- Choi, J.; Tasota, F.J.; Hoffman, L.A. Mobility Interventions to Improve Outcomes in Patients Undergoing Prolonged Mechanical Ventilation: A Review of the Literature. Biol. Res. Nurs. 2008, 10, 21–33. [Google Scholar] [CrossRef]
- Itagaki, A.; Saitoh, M.; Okamura, D.; Kawamura, T.; Otsuka, S.; Tahara, M.; Mori, Y.; Kamisaka, K.; Ochi, Y.; Yuguchi, S.; et al. Factors related to physical functioning decline after cardiac surgery in older patients: A multicenter retrospective study. J. Cardiol. 2019, 74, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Pavasini, R.; Serenelli, M.; Celis-Morales, C.A.; Gray, S.R.; Izawa, K.P.; Watanabe, S.; Colin-Ramirez, E.; Castillo-Martínez, L.; Izumiya, Y.; Hanatani, S.; et al. Grip strength predicts cardiac adverse events in patients with cardiac disorders: An individual patient pooled meta-analysis. Heart 2019, 105, 834. [Google Scholar] [CrossRef]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory Fitness as a Quantitative Predictor of All-Cause Mortality and Cardiovascular Events in Healthy Men and Women: A Meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef]
- Oliveira, G.U.; Carvalho, V.O.; Cacau, L.P.D.A.; Filho, A.A.D.A.; Neto, M.L.D.C.; da Silva, W.M.; Cerqueira, T.C.F.; Filho, V.J.D.S. Determinants of distance walked during the six-minute walk test in patients undergoing cardiac surgery at hospital discharge. J. Cardiothorac. Surg. 2014, 9, 95. [Google Scholar] [CrossRef] [PubMed]
- Passantino, A.; Lagioia, R.; Mastropasqua, F.; Scrutinio, D. Short-Term Change in Distance Walked in 6 Min Is an Indicator of Outcome in Patients With Chronic Heart Failure in Clinical Practice. J. Am. Coll. Cardiol. 2006, 48, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, F.; Abete, P.; Mazzella, F.; Furgi, G.; Nicolino, A.; Longobardi, G.; Testa, G.; Langellotto, A.; Infante, T.; Napoli, C.; et al. Six-minute walking test but not ejection fraction predicts mortality in elderly patients undergoing cardiac rehabilitation following coronary artery bypass grafting. Eur. J. Prev. Cardiol. 2011, 19, 1401–1409. [Google Scholar] [CrossRef]
- Santos, P.M.R.; Ricci, N.A.; Suster, É.A.B.; Paisani, D.M.; Chiavegato, L.D. Effects of early mobilisation in patients after cardiac surgery: A systematic review. Physiotherapy 2017, 103, 1–12. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Højskov, I.; Moons, P.; Egerod, I.; Olsen, P.; Thygesen, L.; Hansen, N.; Cour, S.; Bech, K.; Borregaard, B.; Gluud, C.; et al. Early physical and psycho-educational rehabilitation in patients with coronary artery bypass grafting: A randomized controlled trial. J. Rehabil. Med. 2019, 51, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Zanini, M.; Nery, R.M.; de Lima, J.B.; Buhler, R.P.; da Silveira, A.D.; Stein, R. Effects of Different Rehabilitation Protocols in Inpatient Cardiac Rehabilitation After Coronary Artery Bypass Graft Surgery: A Randomized Clinical Trial. J. Cardiopulm. Rehabil. Prev. 2019, 39, E19–E25. [Google Scholar] [CrossRef] [PubMed]
- Borges, D.L.; Silva, M.G.; Silva, L.N.; Fortes, J.V.; Costa, E.T.; Assunção, R.P.; Lima, C.M.; Nina, V.J.D.S.; Bernardo-Filho, M.; Caputo, D.S. Effects of Aerobic Exercise Applied Early After Coronary Artery Bypass Grafting on Pulmonary Function, Respiratory Muscle Strength, and Functional Capacity: A Randomized Controlled Trial. J. Phys. Act. Health 2016, 13, 946–951. [Google Scholar] [CrossRef] [PubMed]
- Højskov, I.E.; Moons, P.; Hansen, N.V.; Greve, H.; Olsen, D.B.; Cour, S.L.; Glud, C.; Winkel, P.; Lindschou, J.; Egerod, I.; et al. Early physical training and psycho-educational intervention for patients undergoing coronary artery bypass grafting. The SheppHeart randomized 2 × 2 factorial clinical pilot trial. Eur. J. Cardiovasc. Nurs. 2015, 15, 425–437. [Google Scholar]
- Stein, R.; Maia, C.P.; Silveira, A.D.; Chiappa, G.R.; Myers, J.; Ribeiro, J.P. Inspiratory Muscle Strength as a Determinant of Functional Capacity Early After Coronary Artery Bypass Graft Surgery. Arch. Phys. Med. Rehab. 2009, 90, 1685–1691. [Google Scholar] [CrossRef]
- Herdy, A.H.; Marcchi, P.L.B.; Vila, A.; Tavares, C.; Collaço, J.; Niebauer, J.; Ribeiro, J.P. Pre- and Postoperative Cardiopulmonary Rehabilitation in Hospitalized Patients Undergoing Coronary Artery Bypass Surgery. Am. J. Phys. Med. Rehab. 2008, 87, 714–719. [Google Scholar] [CrossRef]
- Parse, R.R. The human becoming school of thought: A perspective for nurses and other health professionals. Choice Rev. Online 1998, 35, 35–6265. [Google Scholar]
- Savci, S.; Sakinç, S.; Ince, D. Active cycle of breathing techniques and incentive spirometer in coronary artery bypass graft surgery. Fiz. Rehabil. 2006, 17, 61–69. [Google Scholar]
- Hodgson, C.L.; Stiller, K.; Needham, D.M.; Tipping, C.J.; Harrold, M.; Baldwin, C.E.; Bradley, S.; Berney, S.; Caruana, L.R.; Elliott, D.; et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit. Care 2014, 18, 658. [Google Scholar] [CrossRef]
- Gremeaux, V.; Troisgros, O.; Benaïm, S.; Hannequin, A.; Laurent, Y.; Casillas, J.-M.; Benaïm, C. Determining the Minimal Clinically Important Difference for the Six-Minute Walk Test and the 200-Meter Fast-Walk Test During Cardiac Rehabilitation Program in Coronary Artery Disease Patients After Acute Coronary Syndrome. Arch. Phys. Med. Rehab. 2011, 92, 611–619. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Crouch, R. Minimal clinically important difference for change in 6-min walk test distance of adults with pathology: A systematic review. J. Eval. Clin. Pract. 2016, 23, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, E.K.D.; Silva, V.Z.M.D.; Turquetto, A.L.R. Relationship on walk test and pulmonary function tests with the length of hospitalization in cardiac surgery patients. Braz. J. Cardiovasc. Surg. 2009, 24, 478–484. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Needham, D.M. Mobilizing Patients in the Intensive Care Unit. JAMA 2008, 300, 1685. [Google Scholar] [CrossRef] [PubMed]
- Winkelman, C. Inactivity and Inflammation in the Critically Ill Patient. Crit. Care Clin. 2007, 23, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Hung, J.; Goldwater, D.; Convertino, V.A.; McKillop, J.H.; Goris, M.L.; DeBusk, R.F. Mechanisms for decreased exercise capacity after bed rest in normal middle-aged men. Am. J. Cardiol. 1983, 51, 344–348. [Google Scholar] [CrossRef]
- Natelson, B.; Deroshia, C.; Levin, B. Physiological Effects of Bed Rest. Lancet 1982, 319, 51. [Google Scholar] [CrossRef]
- Lie, I.; Bunch, E.H.; Smeby, N.A.; Arnesen, H.; Hamilton, G. Patients’ experiences with symptoms and needs in the early rehabilitation phase after coronary artery bypass grafting. Eur. J. Cardiovasc. Nurs. 2010, 11, 14–24. [Google Scholar] [CrossRef]
- Hulzebos, E.H.J.; Helders, P.J.M.; Favié, N.J.; Bie, R.A.D.; de la Riviere, A.B.; Meeteren, N.L.U.V. Preoperative Intensive Inspiratory Muscle Training to Prevent Postoperative Pulmonary Complications in High-Risk Patients Undergoing CABG Surgery. JAMA 2006, 296, 1851. [Google Scholar] [CrossRef]
- Fitchet, A.; Doherty, P.J.; Bundy, C.; Bell, W.; Fitzpatrick, A.P.; Garratt, C.J. Comprehensive cardiac rehabilitation programme for implantable cardioverter-defibrillator patients: A randomised controlled trial. Heart 2003, 89, 155–160. [Google Scholar] [CrossRef]


| Study/Country | Sample Size | Mean Age, Years | % Female | Surgery/Diagnosis | Intervention | Start Day/Frequency | Duration |
|---|---|---|---|---|---|---|---|
| Herdy, 2008 Brazil [22] | 56 | 59.5 | 17/56 (30%) | CABG/CAD |
| POD 1/NR | Started from at least preoperative day 5 and continued to discharge. |
| Hojskov, 2016 Denmark [23] | 60 | 64.8 | 13/60 (22%) | CABG/CAD |
| POD 1/twice daily | Started at admission and continued to 4 weeks after CABG |
| Zanini, 2019 Brazil [24] | 40 | 58.5 | 11/40 (28%) | CABG/CAD |
| POD 2/twice daily | Started preoperatively and continued to discharge |
| Stein, 2009 Brazil [25] | 20 | 63.5 | 9/20 (45%) | CABG/CAD |
| POD 1/NR | Started preoperatively and continued to discharge |
| Hojskov, 2019 Denmark [26] | 326 | 65.1 | 42/326 (13%) | CABG/Ischemic heart disease |
| POD 1/NR | Started at admission and continued to 4 weeks after CABG |
| Borges, 2016 Brazil [27] | 34 | 62.7 | 12/34 (35%) | CABG/CAD |
| POD 1/twice daily | Started preoperatively and continued to discharge |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanejima, Y.; Shimogai, T.; Kitamura, M.; Ishihara, K.; Izawa, K.P. Effect of Early Mobilization on Physical Function in Patients after Cardiac Surgery: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 7091. https://doi.org/10.3390/ijerph17197091
Kanejima Y, Shimogai T, Kitamura M, Ishihara K, Izawa KP. Effect of Early Mobilization on Physical Function in Patients after Cardiac Surgery: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(19):7091. https://doi.org/10.3390/ijerph17197091
Chicago/Turabian StyleKanejima, Yuji, Takayuki Shimogai, Masahiro Kitamura, Kodai Ishihara, and Kazuhiro P. Izawa. 2020. "Effect of Early Mobilization on Physical Function in Patients after Cardiac Surgery: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 19: 7091. https://doi.org/10.3390/ijerph17197091
APA StyleKanejima, Y., Shimogai, T., Kitamura, M., Ishihara, K., & Izawa, K. P. (2020). Effect of Early Mobilization on Physical Function in Patients after Cardiac Surgery: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 17(19), 7091. https://doi.org/10.3390/ijerph17197091







