What Has Been the Impact of Covid-19 on Safety Culture? A Case Study from a Large Metropolitan Healthcare Trust
Abstract
1. Introduction
Aim
2. Methods
2.1. Study Design
2.2. Setting
2.3. Data Collection
2.4. Questionnaire Items
2.4.1. Demographic Questions
2.4.2. Safety Attitudes Questionnaire (SAQ)
2.5. Statistical Analysis
2.6. Incident Reporting
3. Results
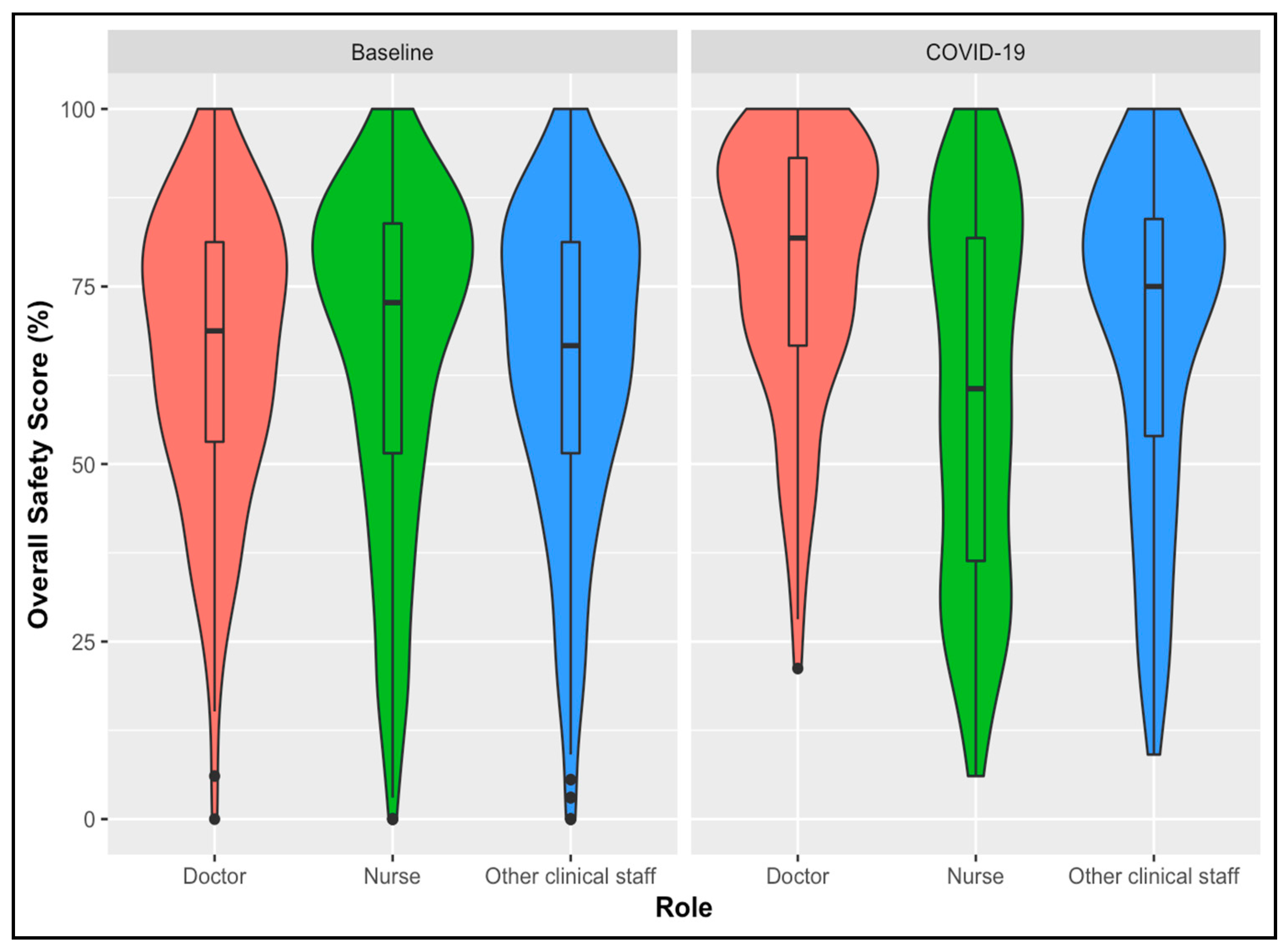
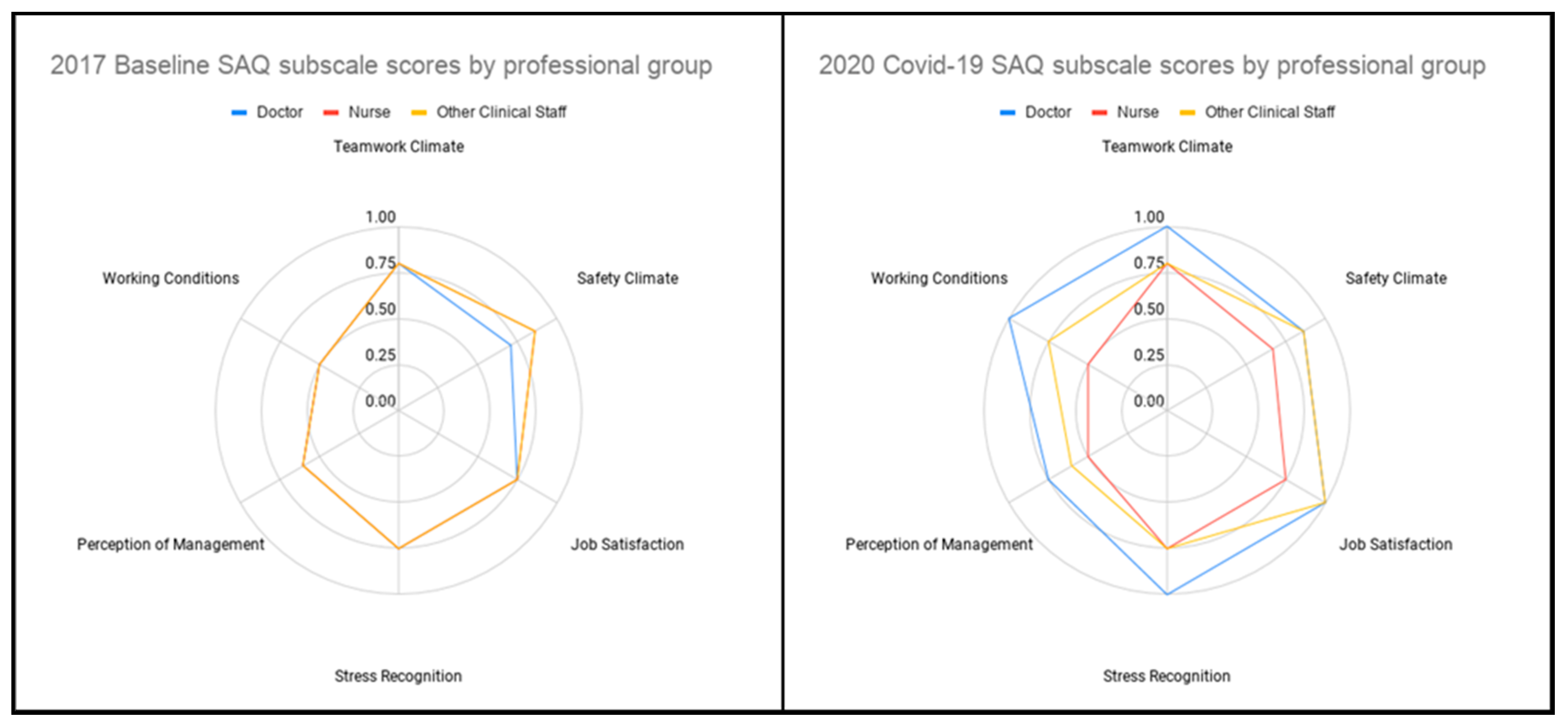
3.1. Comparison
3.2. Regression Analysis
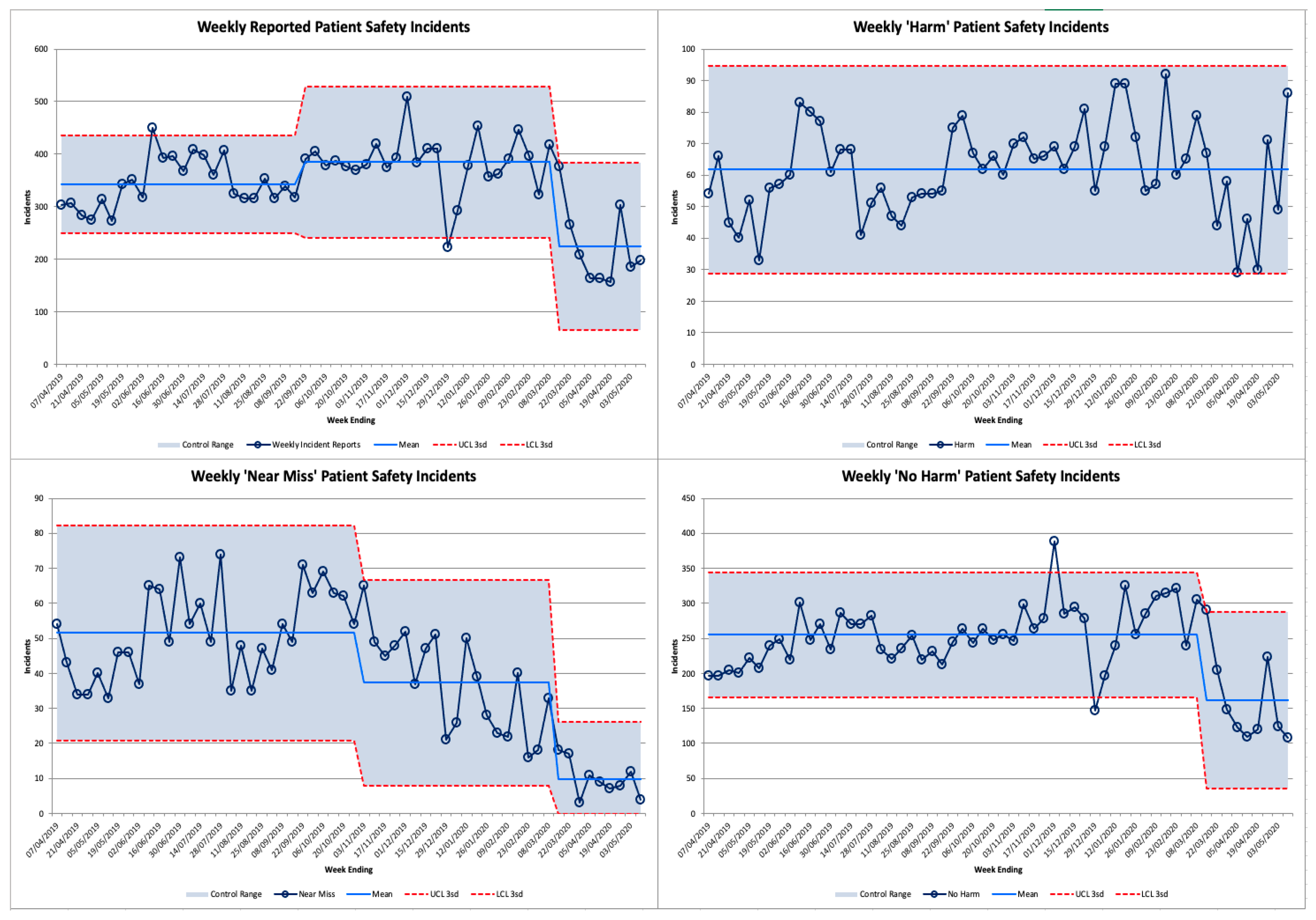
3.3. Error Reporting
4. Discussion
4.1. Incident Reporting
4.2. Recommendations for Future Pandemics
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jha, A.K.; Prasopa-Plaizier, N.; Larizgoitia, I.; Bates, D.W.; on behalf of the Research Priority Setting Working Group of the WHO World Alliance for Patient Safety. Patient safety research: An overview of the global evidence. Qual. Saf. Health Care 2010, 19, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Flin, R.; Winter, J.; Sarac, C.; Raduma, M. Human Factors in Patient Safety: Review of Topics and Tools. World Health 2009, 2, 11–12. [Google Scholar]
- Hofmann, D.A.; Mark, B. An Investigation of the Relationship between Safety Climate and Medication Errors as Well as other Nurse and Patient Outcomes. Pers. Psychol. 2006, 59, 847–869. [Google Scholar] [CrossRef]
- Naveh, E.; Katz-Navon, T.; Stern, Z. Treatment Errors in Healthcare: A Safety Climate Approach. Manag. Sci. 2005, 51, 948–960. [Google Scholar] [CrossRef]
- Zohar, D.; Livne, Y.; Tenne-Gazit, O.; Admi, H.; Donchin, Y. Healthcare climate: A framework for measuring and improving patient safety. Crit. Care Med. 2007, 35, 1312–1317. [Google Scholar] [CrossRef]
- Murphy, T. CCHSA Client/Patient Safety Culture Assessment Project: Lessons learned. Health Q. 2006, 9, 52. [Google Scholar] [CrossRef]
- The Evidence Centre. Evidence Scan: Measuring Safety Culture; The Health Foundation: London, UK, 2011. [Google Scholar]
- DiCuccio, M.H. The Relationship Between Patient Safety Culture and Patient Outcomes: A Systematic Review. J. Patient Saf. 2015, 11, 135–142. [Google Scholar] [CrossRef]
- Institute of Medicine Committee on Quality of Health Care in A. To Err Is Human: Building a Safer Health System; Kohn, L.T., Corrigan, J.M., Donaldson, M.S., Eds.; National Academies Press: Washington, DC, USA, 2000. [Google Scholar]
- Perez-Guzman, P.N.; Daunt, A.; Mukherjee, S.; Crook, P.; Forlano, R.; Kont, M.D.; Løchen, A.; Vollmer, M.; Middleton, P.; Judge, R.; et al. Clinical characteristics and predictors of outcomes of hospitalized patients with COVID-19 in a multi-ethnic London NHS Trust: A retrospective cohort study. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Sexton, J.B.; Helmreich, R.L.; Neilands, T.B.; Rowan, K.; Vella, K.; Boyden, J.; Roberts, P.R.; Thomas, E.J. The Safety Attitudes Questionnaire: Psychometric properties, benchmarking data, and emerging research. BMC Health Serv. Res. 2006, 6, 44. [Google Scholar] [CrossRef]
- Ningrum, E.; Evans, S.M.; Soh, S.-E. Validation of the Indonesian version of the Safety Attitudes Questionnaire: A Rasch analysis. PLoS ONE 2019, 14, e0215128. [Google Scholar] [CrossRef]
- Kaya, S.; Barsbay, S.; Karabulut, E. The Turkish version of the safety attitudes questionnaire: Psychometric properties and baseline data. BMJ Qual. Saf. 2010, 19, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.; Chang, Q.; Zhang, X.; Wu, Q.; Wu, N.; He, J.; Zhao, Y. Evaluation of safety attitudes of hospitals and the effects of demographic factors on safety attitudes: A psychometric validation of the safety attitudes and safety climate questionnaire. BMC Health Serv. Res. 2019, 19, 836. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, G.; Gambashidze, N.; Ilyas, S.A.; Pascu, D. Validation of the safety attitudes questionnaire (short form 2006) in Italian in hospitals in the northeast of Italy. BMC Health Serv. Res. 2015, 15, 284. [Google Scholar] [CrossRef] [PubMed]
- Nordén-Hägg, A.; Sexton, J.B.; Sporrong, S.K.; Ring, L.; Kettis-Lindblad, A. Assessing Safety Culture in Pharmacies: The psychometric validation of the Safety Attitudes Questionnaire (SAQ) in a national sample of community pharmacies in Sweden. BMC Clin. Pharmacol. 2010, 10, 8. [Google Scholar] [CrossRef]
- Alzahrani, N.; Jones, R.; Abdel-Latif, M.E. Attitudes of doctors and nurses toward patient safety within emergency departments of two Saudi Arabian hospitals. BMC Health Serv. Res. 2018, 18, 736. [Google Scholar] [CrossRef]
- Pronovost, P.; Sexton, B. Assessing safety culture: Guidelines and recommendations. Qual. Saf. Health Care 2005, 14, 231–233. [Google Scholar] [CrossRef]
- Vincent, C.; Burnett, S.; Carthey, J. The Measurement and Monitoring of Safety; Centre for Patient Safety and Service Quality Imperial College London: London, UK, 2013. [Google Scholar]
- Benneyan, J.C.; Lloyd, R.C.; Plsek, P. Statistical process control as a tool for research and healthcare improvement. Qual. Saf. Health Care 2003, 12, 458–464. [Google Scholar] [CrossRef]
- Kagan, I.; Barnoy, S. Organizational Safety Culture and Medical Error Reporting by Israeli Nurses. J. Nurs. Sch. 2013, 45. [Google Scholar] [CrossRef]
- Gurses, A.P.; Tschudy, M.M.; McGrath-Morrow, S.; Husain, A.; Solomon, B.S.; A Gerohristodoulos, K.; Kim, J.M. Overcoming COVID-19: What can human factors and ergonomics offer? J. Patient Saf. Risk Manag. 2020, 25, 49–54. [Google Scholar] [CrossRef]
- Staines, A.; Amalberti, R.; Berwick, D.M.; Braithwaite, J.; Lachman, P.; A Vincent, C. COVID-19: Patient safety and quality improvement skills to deploy during the surge. Int. J. Qual. Health Care 2020. [Google Scholar] [CrossRef]
- Cook, J.V.F.; Dickinson, H.; Eccles, M.P. Response rates in postal surveys of healthcare professionals between 1996 and 2005: An observational study. BMC Health Serv. Res. 2009, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- McMahon, S.R.; Iwamoto, M.; Massoudi, M.S.; Yusuf, H.R.; Stevenson, J.M.; David, F.; Chu, S.Y.; Pickering, L.K. Comparison of e-mail, fax, and postal surveys of pediatricians. Pediatrics 2003, 111, e299–e303. [Google Scholar] [CrossRef] [PubMed]
- NHS Digital. Narrowing of NHS Gender Divide but Men still the Majority in Senior Roles Leeds: NHS Digital. 2018. Available online: https://digital.nhs.uk/news-and-events/latest-news/narrowing-of-nhs-gender-divide-but-men-still-the-majority-in-senior-roles (accessed on 11 June 2020).
| Covariates | Baseline Survey | Covid-19 Survey | Chi-Square p-Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Role | |||
| Other clinical staff | 325 (31) | 127 (30) | <0.001 |
| Doctor | 157 (15) | 105 (25) | |
| Nurse | 557 (54) | 183 (44) | |
| Division | |||
| Medicine | 536 (34) | 188 (45) | <0.001 |
| Surgery | 445 (28) | 112 (27) | |
| Other | 599 (38) | 115 (28) | |
| Age, years; mean (SD) | 36.8 [10.5] | ||
| 18–29 | Not available | 142 (34) | |
| 30–39 | Not available | 131 (32) | |
| 40–49 | Not available | 96 (23) | |
| 50+ | Not available | 46 (11) | |
| Gender | |||
| Male | Not available | 100 (26) | |
| Female | Not available | 288 (73) | |
| Not stated | Not available | 5 (1) | |
| Ethnicity | |||
| White | Not available | 212 (51) | |
| Black, Asian and Minority Ethnic (BAME) | Not available | 182 (44) | |
| Not stated | Not available | 21 (5) | |
| Redeployed | |||
| No | N/A | 250 (60) | |
| Yes | N/A | 165 (40) | |
| Redeployed to | |||
| Not redeployed | N/A | 249 (60) | |
| Covid-19 ward medicine | N/A | 50 (12) | |
| Intensive treatment unit (ITU) | N/A | 70 (17) | |
| Other | N/A | 46 (11) | |
| Symptoms of Covid-19 | |||
| Asymptomatic | N/A | 367 (88) | |
| Symptomatic | N/A | 48 (12) | |
| Covid-19 Testing | |||
| Not tested | N/A | 258 (62) | |
| Tested | N/A | 157 (38) | |
| Training for redeployment * | |||
| None/Very Poor/Poor | N/A | 54 (32) | |
| Neutral/Good/Very Good | N/A | 113 (68) | |
| Support during redeployment ** | |||
| None/Very Poor/Poor | N/A | 40 (25) | |
| Neutral/Good/Very Good | N/A | 120 (75) | |
| Total | 1039 (100) | 415 (100) |
| Covariate (Baseline) | Median | Univariate Analysis (All Respondents) | Multivariate Analysis (All Respondents) | Univariate Analysis (Redeployed Subgroup) § | Multivariate Analysis (Redeployed Subgroup) § | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SAQ Score | Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI | |||||
| Age (18–29) | 0.76 | - | - | - | - | - | - | - | - | - | - | - | - |
| 30–39 | 0.70 | −0.06 | −0.14 | 0.02 | −0.03 | −0.14 | 0.08 | −0.03 | −0.28 | 0.22 | −0.01 | −0.16 | 0.14 |
| 40–49 | 0.64 | −0.13 ** | −0.23 | −0.03 | −0.06 | −0.13 | 0.01 | −0.21 * | −0.41 | −0.01 | −0.06 | −0.23 | 0.11 |
| 50+ | 0.73 | −0.03 | −0.11 | 0.05 | −0.04 | −0.14 | 0.06 | 0.00 | −0.14 | 0.14 | −0.01 | −0.16 | 0.14 |
| Gender (Male) | 0.76 | - | - | - | - | - | - | - | - | - | - | - | - |
| Female | 0.73 | −0.03 | −0.11 | 0.05 | 0.00 | −0.08 | 0.08 | 0.11 | −0.04 | 0.26 | 0.01 | −0.13 | 0.11 |
| Not stated | 0.42 | −0.34 *** | −0.42 | −0.26 | −0.13* | −0.26 | 0.00 | - | - | - | - | - | - |
| Ethnicity (White) | 0.77 | - | - | - | - | - | - | - | - | - | - | - | - |
| BAME | 0.61 | −0.16*** | −0.23 | −0.09 | −0.08 | −0.18 | 0.02 | −0.18 ** | −0.29 | −0.07 | −0.08 | −0.21 | 0.05 |
| Not stated | 0.74 | −0.03 | −0.13 | 0.07 | −0.11 * | −0.22 | 0.00 | - | - | - | - | - | - |
| Role (Doctor) | 0.82 | - | - | - | - | - | - | - | - | - | - | - | - |
| Nurse | 0.61 | −0.21 *** | −0.32 | −0.10 | −0.15 *** | −0.24 | −0.06 | −0.15 ** | −0.27 | −0.03 | −0.12 * | −0.23 | −0.01 |
| Other clinical staff | 0.73 | −0.09 ** | −0.16 | −0.02 | −0.05 | −0.13 | 0.03 | 0.00 | −0.07 | 0.07 | −0.04 | −0.16 | 0.08 |
| Division (Medicine) | 0.68 | - | - | - | - | - | - | - | - | - | - | - | - |
| Surgery | 0.62 | −0.08 | −0.17 | 0.01 | - | - | - | −0.15 | −0.31 | 0.01 | - | - | - |
| Other | 0.69 | −0.02 | −0.09 | 0.05 | - | - | - | 0.03 | −0.11 | 0.17 | - | - | - |
| Redeployed (No) | 0.75 | - | - | - | - | - | - | - | - | - | - | - | - |
| Yes | 0.70 | −0.04 | −0.11 | 0.03 | −0.07 | −0.14 | 0.00 | - | - | - | - | - | - |
| Redeployed to (Not redeployed) | 0.74 | - | - | - | - | - | - | - | - | - | - | - | - |
| Covid-19 ward medicine | 0.67 | −0.07 | −0.23 | 0.09 | - | - | - | - | - | - | - | - | - |
| ITU | 0.73 | −0.01 | −0.07 | 0.05 | - | - | - | 0.09 | −0.03 | 0.21 | - | - | - |
| Other | 0.65 | −0.11 | −0.25 | 0.03 | - | - | - | −0.01 | −0.20 | 0.18 | - | - | - |
| Had symptoms (Asymptomatic) | 0.73 | - | - | - | - | - | - | - | - | - | - | - | - |
| Symptomatic | 0.66 | −0.09 | −0.27 | 0.09 | - | - | - | −0.26 ** | −0.46 | −0.06 | −0.10 | −0.22 | 0.02 |
| Tested (No) | 0.73 | - | - | - | - | - | - | - | - | - | - | - | - |
| Yes | 0.67 | −0.06 | −0.15 | 0.03 | - | - | - | −0.09 | −0.27 | 0.09 | - | - | - |
| Training (None/Very Poor/Poor) n = 167 | 0.52 | - | - | - | - | - | - | - | - | - | - | - | - |
| Neutral/Good/Very Good | 0.76 | - | - | - | - | - | - | 0.21 *** | 0.07 | 0.35 | 0.07 | −0.04 | 0.18 |
| Support (None/Very Poor/Poor) n = 160 | 0.40 | - | - | - | - | - | - | - | - | - | - | - | - |
| Neutral/Good/Very Good | 0.74 | - | - | - | - | - | - | 0.34 *** | 0.22 | 0.46 | 0.29 *** | 0.14 | 0.44 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Denning, M.; Goh, E.T.; Scott, A.; Martin, G.; Markar, S.; Flott, K.; Mason, S.; Przybylowicz, J.; Almonte, M.; Clarke, J.; et al. What Has Been the Impact of Covid-19 on Safety Culture? A Case Study from a Large Metropolitan Healthcare Trust. Int. J. Environ. Res. Public Health 2020, 17, 7034. https://doi.org/10.3390/ijerph17197034
Denning M, Goh ET, Scott A, Martin G, Markar S, Flott K, Mason S, Przybylowicz J, Almonte M, Clarke J, et al. What Has Been the Impact of Covid-19 on Safety Culture? A Case Study from a Large Metropolitan Healthcare Trust. International Journal of Environmental Research and Public Health. 2020; 17(19):7034. https://doi.org/10.3390/ijerph17197034
Chicago/Turabian StyleDenning, Max, Ee Teng Goh, Alasdair Scott, Guy Martin, Sheraz Markar, Kelsey Flott, Sam Mason, Jan Przybylowicz, Melanie Almonte, Jonathan Clarke, and et al. 2020. "What Has Been the Impact of Covid-19 on Safety Culture? A Case Study from a Large Metropolitan Healthcare Trust" International Journal of Environmental Research and Public Health 17, no. 19: 7034. https://doi.org/10.3390/ijerph17197034
APA StyleDenning, M., Goh, E. T., Scott, A., Martin, G., Markar, S., Flott, K., Mason, S., Przybylowicz, J., Almonte, M., Clarke, J., Winter Beatty, J., Chidambaram, S., Yalamanchili, S., Tan, B. Y.-Q., Kanneganti, A., Sounderajah, V., Wells, M., Purkayastha, S., & Kinross, J. (2020). What Has Been the Impact of Covid-19 on Safety Culture? A Case Study from a Large Metropolitan Healthcare Trust. International Journal of Environmental Research and Public Health, 17(19), 7034. https://doi.org/10.3390/ijerph17197034







