Mediating Factors in Nursing Competency: A Structural Model Analysis for Nurses’ Communication, Self-Leadership, Self-Efficacy, and Nursing Performance
Abstract
1. Introduction
1.1. Significance of the Study
1.2. The Purpose of the Study
- Establish a causal model among the nurses’ communication ability, self-leadership, self-efficacy, and nursing performance;
- Investigate the relationship between practitioner nurses’ communication ability, self-leadership, self-efficacy, and nursing performance;
- Examine the mediating effects of self-leadership and self-efficacy on the relationship between communication ability and nursing performance.
2. Materials and Methods
2.1. Study Participants
2.2. Research Instruments
2.2.1. Composition of Research Tools
2.2.2. Validity and Reliability of Research Tools
2.2.3. Communication Ability
2.2.4. Self-Leadership
2.2.5. Self-Efficacy
2.2.6. Nursing Performance
2.3. Data Collection and Processing Method
3. Results
3.1. Descriptive Statistics and Correlations
3.2. Measurement Model Analysis
3.2.1. Fit of Measurement Model
3.2.2. Validity of the Measurement Model
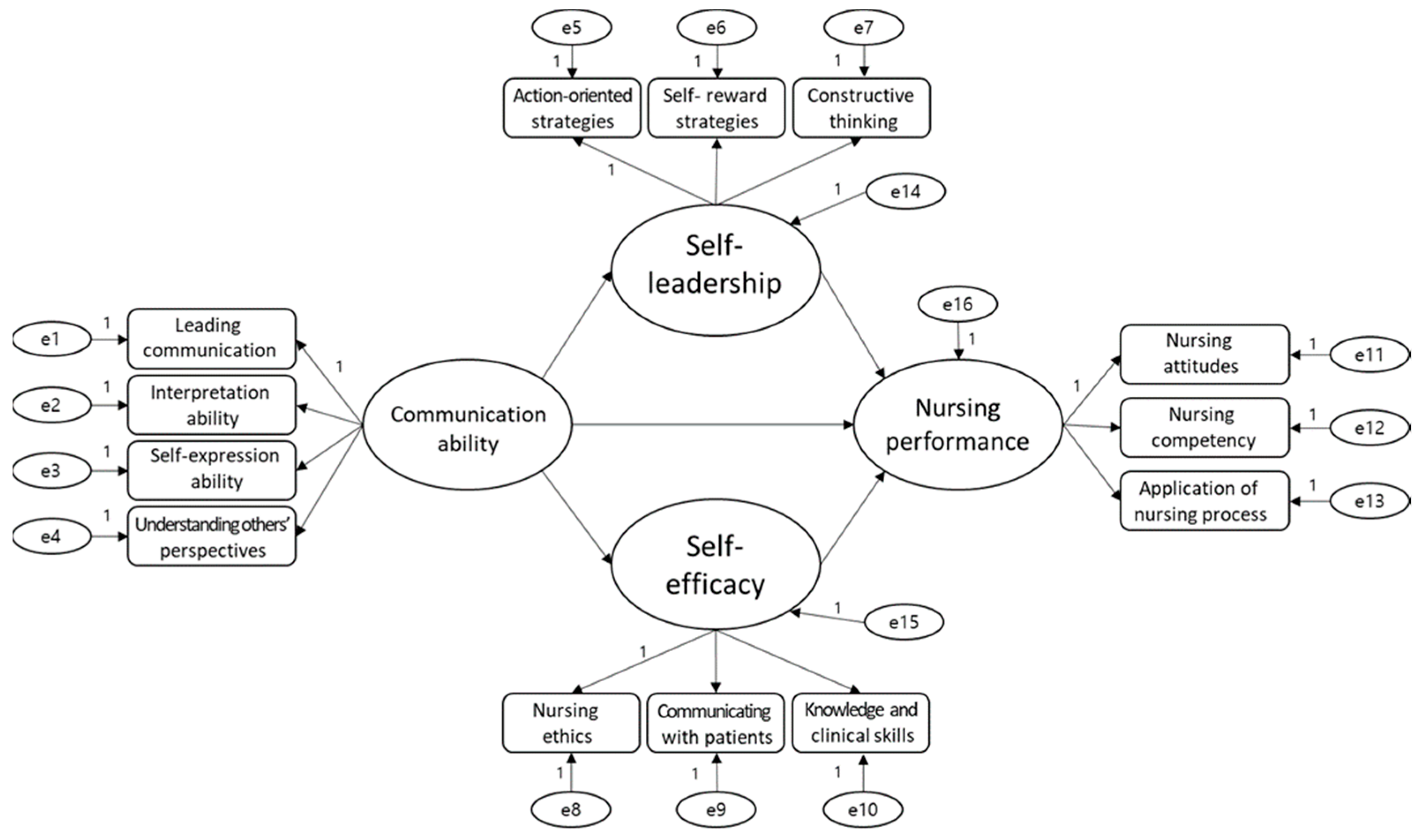
3.3. Structural Model Verification
3.3.1. Verification of Model Fit
3.3.2. Verification of Direct Effect
3.4. Verification of the Mediation Effect
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Korea Institute for Healthcare Accreditation. Healthcare Accreditation Program in Korea. Available online: http://www.koiha.kr/member/kr/index.co (accessed on 18 October 2018).
- Song, H.J.; Lee, S.M. The effects of hospital nurses’ self-esteem and communication skill on self-leadership and the quality of nursing service. J. Korean Acad. Nurs. Adm. 2016, 22, 220–229. [Google Scholar] [CrossRef][Green Version]
- Blay, N.; Duffield, C.M.; Gallagher, R.; Roche, M. A systematic review of time studies to assess the impact of patient transfers on nurse workload. Int. J. Nurs. Stud. 2014, 20, 662–673. [Google Scholar] [CrossRef] [PubMed]
- Kang, K.H.; Han, Y.H.; Kang, S.J. Relationship between organizational communication satisfaction and organizational commitment among hospital nurses. J. Korean Acad. Nurs. Adm. 2012, 18, 13–22. [Google Scholar] [CrossRef]
- Choi, I.Y.; Park, N.H.; Jeong, J.H. Effects of clinical nurses’ self-leadership and nursing organizational culture on nursing performance. Int. J. Contents 2019, 19, 502–516. [Google Scholar] [CrossRef]
- Son, H.M.; Sung, K.M. The mediating effects of self-efficacy in the relationship between communicative competence within the medical team and turnover intention in hospital nurses. J. Korea Acad. Ind. Coop. Soc. 2017, 18, 300–309. [Google Scholar] [CrossRef]
- Kim, H.S.; Suh, E.E. The effects of an interactive nursing skills mobile application on nursing students’ knowledge, self-efficacy, and skills performance: A randomized controlled trial. Asian Nurs. Res. 2018, 12, 17–25. [Google Scholar] [CrossRef]
- Ko, Y.K.; Lee, T.W.; Lim, J.Y. Development of a performance measurement scale for hospital nurses. Taehan Kanho Hakhoe Chi 2007, 37, 286–294. [Google Scholar] [CrossRef]
- Im, S.I.; Park, J.; Kim, H.S. The effects of nurse’s communication and self-leadership on nursing performance. Korean J. Occup. Health Nurs. 2012, 21, 274–282. [Google Scholar] [CrossRef]
- Judge, T.A.; Bono, J.E. Relationship of core self-evaluations traits—Self-esteem, generalized self-efficacy, locus of control, and emotional stability—With job satisfaction and job performance; a meta-analysis. J. Appl. Psychol. 2001, 86, 80–92. [Google Scholar] [CrossRef]
- Hwang, Y.S.; Kim, E.J.; Kim, K.I.; Yoon, M.K. An analysis on the relationship between self-development needs, emotional labor, self-resilience and recognition of profession of teachers. J. Korea Open Assoc. Early Child. Educ. 2016, 21, 205–221. [Google Scholar]
- Hur, G.H. Construction and validation of a global interpersonal communication competence scale. Korean J. Journal. Commun. 2003, 47, 380–426. [Google Scholar]
- Lee, H.S.; Kim, J.K. Relationship among communication competence, communication types, and organizational commitment in hospital nurses. J. Korean Acad. Nurs. Adm. 2010, 16, 488–496. [Google Scholar] [CrossRef]
- Curtis, K.T.; Tzannes, A.; Rudge, T. How to talk to doctors—A guide for effective communication. Int. Nurs. Rev. 2011, 58, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Expósito, J.; Leal Costa, C.; Díaz Agea, J.L.; Carrillo Izquierdo, M.D.; Jiménez Rodríguez, D. Ensuring relational competency in critical care: Importance of nursing students’ communication skills. Intensive Crit. Care Nurs. 2018, 44, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Pangh, B.; Jouybari, L.; Vakili, M.A.; Sanagoo, A.; Torik, A. The effect of reflection on nurse–patient communication skills in emergency medical centers. J. Caring Sci. 2019, 8, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Parnian, N.; Behjat, M.; Samin, N.; Ali, R.Y. Nurses Communication Skills Training and Its Effect on Patients’ Satisfaction in Teaching Hospitals of Shiraz University of Medical Sciences. Maz. Univ. Med Sci. 2018, 6, 22–29. [Google Scholar]
- Colley, S.L. Voices of quiet students: Introverted nursing students’ perceptions of educational experiences and leadership preparation. Int. J. Nurs. Educ. Scolarsh. Berlin. 2018, 1. [Google Scholar] [CrossRef]
- Park, N.H.; Lee, K.J.; Lee, S.J. Mediating effects of self-leadership in the relationship between public health nurses’ organizational culture and their job performance. J. Korean Acad. Commun. Health Nurs. 2017, 28, 23–33. [Google Scholar] [CrossRef]
- Shim, D.S.; Ha, S.W. A Study on the Relationship between Job Characteristics and Innovative Behavior: The Mediating Effect of Self-Efficacy. J. Bus. Econ. 2013, 29, 95–124. [Google Scholar]
- Cho, I.H.; Meera, P. Comparison of problem solving ability according to degree of communication ability of nursing students. AJMAHS Converg. Res. Soc. Humanit. Sociol. Sci. Technol. 2017, 7, 397–404. [Google Scholar] [CrossRef][Green Version]
- Neck, C.P.; Houghton, J.D. Two decades of self-leadership theory and research. J. Manag. Psychol. 2006, 21, 270–295. [Google Scholar] [CrossRef]
- Kim, B.K.; Jyung, C.Y. The casual relationship among career decision-making self-efficacy, self-leadership, problem solving ability, and career motivation. J. Agric. Educ. Hum. Resour. Dev. 2012, 44, 49–71. [Google Scholar]
- Lee, J.C.; Hong, A.J. The influence of university students’ self-leadership upon career preparation behavior and mediating effect of career decision self-efficacy and employability. J. Health Inform. Stat. 2013, 26, 69–92. [Google Scholar] [CrossRef]
- Park, K.W.; Chung, W.J.; Lee, W.K.; Shin, E.K.; Hong, E.H. Relationship between the Clinical Performance Examination and Associated Variables. Korean J. Med. Educ. 2009, 21, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Van de Ven, A.H.; Ferry, D.L. Measuring and Assessing Organizations; John Wiley & Sons: New York, NY, USA, 1980. [Google Scholar]
- Hu, L.Z.; Bentler, P.M. Cut off criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, M.G.; Hong, S.H. Writing with a Structural Equation Model; Communication Books: Seoul, Korea, 2009. [Google Scholar]
- Kim, G.S.A. 18.0 Analysis of AMOS 18.0. In Structural Equation Modeling Seoul; Hannarae: Seoul, Korea, 2013. [Google Scholar]
- Clements, A.; Curtis, K.; Horvat, L.; Shaban, R.Z. The effect of a nurse team leader on communication and leadership in major trauma resuscitations. Int. Emerg. Nurs. 2015, 23, 3–7. [Google Scholar] [CrossRef]
- Bullington, J.; Sparén, E.B.; Kneck, Å.; Omérov, P.; Söderlund, M.; Cronqvist, A. Communication skills in nursing: A phenomenological-based communication training approach. Nurse Educ. Pract. 2019, 39, 136–141. [Google Scholar] [CrossRef]
- Al-Hamdan, Z.; Banerjee, T.; Manojlovich, M. Communication with physicians as a mediator in the relationship between the nursing work environment and select nurse outcomes in jordan. J. Nurs. Scholarsh. 2018, 50, 714–721. [Google Scholar] [CrossRef]
- Hong, S.M.; Kim, M.H.; Suh, S.R. Health Beliefs, Self-Efficacy and Medical Care Utilization of Korean Nurses. Korean J. Occup. Health Nurs. 2010, 19, 170–179. [Google Scholar]
- Bang, M.; Sim, S. Relationship among Empathy Ability, Creativity Confluence Competency and Problem-Solving Ability in Nursing Students. Indian J. Public Health Res. Dev. 2018, 9, 939–944. [Google Scholar] [CrossRef]
- Long, T. Influence of International Service-Learning on Nursing Student Self-Efficacy Toward Cultural Competence. J. Nurs. Educ. 2014, 53, 474–478. [Google Scholar] [CrossRef] [PubMed]
- Roh, J.Y.; Hwang, C.G.; Song, Y.W. The Effect of Self Leadership of Polytechnic University Students on Educational Performance. Korean J. Converg. Sci. 2020, 9, 16–29. [Google Scholar] [CrossRef]
- Park, K.T. The influence of food service company team leaders’ coaching leadership on the self-efficacy and job performance of team members. Int. J. Tour. Res. 2019, 33, 187–200. [Google Scholar] [CrossRef]
- Cho, J.S. The Impacts of Self-Leadership on Job Performance of Vietnamese Food-Service employees. J. Int. Trade Comm. 2020, 16, 337–352. [Google Scholar] [CrossRef]
- Nilsson, J.; Engström, M.; Florin, J.; Gardulf, A.; Carlsson, M. A short version of the nurse professional competence scale for measuring nurses’ self-reported competence. Nurse Educ. Today 2018, 71, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Barton, A.J. Leadership and communication competencies in nursing: What are we missing? J. Nurs. Educ. 2018, 57, 259–260. [Google Scholar] [CrossRef]
- Donovan, L.M.; Mullen, L.K. Expanding nursing simulation programs with a standardized patient protocol on therapeutic communication. Nurs. Educ. Pract. 2019, 38, 126–131. [Google Scholar] [CrossRef]
- Kim, S.S.; Kim, E.J.; Lim, J.Y.; Kim, G.M.; Baek, H.C. Korean nursing students’ acquisition of evidence-based practice and critical thinking skills. J. Nurs. Educ. 2018, 57, 21–27. [Google Scholar] [CrossRef]
| Characteristics | Frequency (n) | Rate (%) | |
|---|---|---|---|
| Gender | Male | 11 | 6.5 |
| Female | 157 | 93.5 | |
| Age | 20~29 | 39 | 23.2 |
| 30~39 | 50 | 29.8 | |
| 40~49 | 41 | 24.4 | |
| 50~ | 38 | 22.6 | |
| Married | Single | 78 | 46.4 |
| Married | 90 | 53.6 | |
| Academic records | College degree | 90 | 53.6 |
| Bachelor’s degree | 78 | 46.4 | |
| Types of medical institutions | Secondary hospital (General hospital) | 142 | 84.5 |
| Third hospital (Advanced general hospital) | 26 | 15.5 | |
| Clinical Experience | <3 years | 33 | 19.6 |
| 3~7 years | 43 | 25.6 | |
| 7~11 years | 39 | 23.2 | |
| >11 years | 53 | 31.5 | |
| Department | Internal medicine ward | 96 | 57.1 |
| Surgical ward | 31 | 18.5 | |
| Pediatric ward | 4 | 2.4 | |
| Special department | 37 | 22.0 | |
| Position | General nurse | 145 | 86.3 |
| Charge nurse | 17 | 10.1 | |
| Head nurse | 6 | 3.6 | |
| Annual Income (1,000,000 won /(1000 US dollar) | <30/(25) | 46 | 27.4 |
| 30~40 /(25~34) | 65 | 38.7 | |
| 40~50 /(34~42) | 45 | 26.8 | |
| >50/(42) | 12 | 7.1 | |
| Total | 168 | 100 | |
| Factor Name | Factor Variable | Factor Loading | % of Variance (Eigen Value) | Communality | Reliability (Cronbach’s Alpha) |
|---|---|---|---|---|---|
| Understanding others’ perspectives | comm16 | 0.827 | 29.096 (3.783) | 0.688 | 0.779 |
| comm14 | 0.783 | 0.665 | |||
| comm15 | 0.751 | 0.659 | |||
| comm13 | 0.651 | 0.527 | |||
| Interpretation ability | comm 2 | 0.835 | 13.686 (1.779) | 0.709 | 0.731 |
| comm1 | 0.770 | 0.685 | |||
| comm 4 | 0.626 | 0.651 | |||
| Self-expression ability | comm 7 | 0.809 | 11.499 (1.495) | 0.682 | 0.658 |
| comm6 | 0.683 | 0.614 | |||
| comm 5 | 0.501 | 0.509 | |||
| Leading communication | comm10 | 0.740 | 8.875 (1.154) | 0.727 | 0.639 |
| comm9 | 0.725 | 0.664 | |||
| comm11 | 0.569 | 0.531 | |||
| Total | 63.156 | ||||
| Figure. | Factor Variable | Factor Loading | % of Variance (Eigen Value) | Communality | Reliability (Cronbach’s Alpha) |
|---|---|---|---|---|---|
| Constructive thinking | leadership12 | 0.796 | 33.568 (3.693) | 0.669 | 0.807 |
| leadership13 | 0.776 | 0.608 | |||
| leadership11 | 0.772 | 0.634 | |||
| leadership10 | 0.760 | 0.678 | |||
| Self-rewarding strategies | leadership8 | 0.804 | 18.357 (2.019) | 0.688 | 0.788 |
| leadership9 | 0.768 | 0.672 | |||
| leadership7 | 0.751 | 0.683 | |||
| leadership6 | 0.684 | 0.620 | |||
| Action-oriented strategies | leadership4 | 0.869 | 12.250 (1.348) | 0.793 | 0.652 |
| leadership3 | 0.823 | 0.701 | |||
| leadership2 | 0.538 | 0.613 | |||
| Total | 64.175 | ||||
| Factor Name | Factor Variable | Factor Loading | % of Variance (Eigen Value) | Communality | Reliability (Cronbach’s Alpha) |
|---|---|---|---|---|---|
| Knowledge and clinical skills | efficacy4 | 0.865 | 50.226 (5.525) | 0.840 | 0.898 |
| efficacy2 | 0.845 | 0.781 | |||
| efficacy3 | 0.831 | 0.799 | |||
| efficacy6 | 0.735 | 0.676 | |||
| Communicating with patients | efficacy10 | 0.826 | 12.667 (1.393) | 0.736 | 0.838 |
| efficacy11 | 0.823 | 0.712 | |||
| efficacy12 | 0.745 | 0.656 | |||
| efficacy9 | 0.668 | 0.634 | |||
| Nursing ethics | efficacy14 | 0.767 | 8.772 (0.965) | 0.744 | 0.754 |
| efficacy16 | 0.767 | 0.643 | |||
| efficacy15 | 0.714 | 0.658 | |||
| Total | 71.665 | ||||
| Factor Name | Factor Variable | Factor Loading | % of Variance (Eigen Value) | Communality | Reliability (Cronbach’s Alpha) |
|---|---|---|---|---|---|
| Application of nursing process | performance 11 | 0.858 | 54.244 (5.424) | 0.840 | 0.895 |
| performance 12 | 0.826 | 0.778 | |||
| performance 10 | 0.826 | 0.785 | |||
| performance 13 | 0.706 | 0.673 | |||
| Nursing competency | performance 2 | 0.865 | 11.332 (1.133) | 0.822 | 0.855 |
| performance 1 | 0.814 | 0.755 | |||
| performance 3 | 0.750 | 0.706 | |||
| Nursing attitudes | performance 9 | 0.407 | 9.364 (0.936) | 0.509 | 0.751 |
| performance 7 | 0.880 | 0.852 | |||
| performance 6 | 0.784 | 0.774 | |||
| Total | 74.940 | ||||
| Measurement Variables | Mean | Standard Deviation | Skewness | Kurtosis |
|---|---|---|---|---|
| Leading communication | 3.685 | 0.628 | 0.072 | −0.120 |
| Self-expression ability | 4.040 | 0.542 | 0.076 | −0.480 |
| Interpretation ability | 3.621 | 0.581 | 0.158 | 0.055 |
| Understanding others’ perspectives | 3.325 | 0.704 | 0.066 | −0.472 |
| Action-oriented strategies | 3.582 | 0.644 | −0.126 | −0.283 |
| Self-rewarding strategies | 3.781 | 0.622 | 0.023 | −0.245 |
| Constructive thinking | 2.911 | 0.682 | −0.299 | 0.659 |
| Nursing ethics | 3.787 | 0.682 | 0.108 | −0.838 |
| Communicating with patients | 3.933 | 0.562 | 0.202 | −0.698 |
| Knowledge and clinical skills | 3.980 | 0.592 | 0.007 | −0.634 |
| Nursing attitudes | 3.833 | 0.650 | 0.050 | −0.669 |
| Nursing competency | 4.065 | 0.545 | −0.171 | 0.292 |
| Application of nursing process | 3.988 | 0.601 | −0.218 | −0.789 |
| Latent Variable | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Communication ability | 1 | |||
| Self-leadership | 0.453 ** | 1 | ||
| Self-efficacy | 0.526 ** | 0.480 ** | 1 | |
| Nursing performance | 0.498 ** | 0.462 ** | 0.753 ** | 1 |
| Criteria | χ2 | df | p | CFI | GFI | TLI | RMSEA | RMR |
|---|---|---|---|---|---|---|---|---|
| Model fit | 94.846 | 51 | 0.000 | 0.953 | 0.924 | 0.928 | 0.072 | 0.021 |
| Criteria for fitness | ≥0.90 | ≥0.90 | ≥0.90 | ≤0.08 | ≤0.05 |
| Directions | Estimate (p) | Standardization Factor (β) | Standard Error (S.E.) | Critical Ratio (C.R.) | |
|---|---|---|---|---|---|
| Leading communication | Communication ability | 1.000 | 0.524 | ||
| Self-expression ability | 0.723 | 0.460 | 0.169 | 4.270 *** | |
| Interpretation ability | 0.858 | 0.586 | 0.169 | 5.080 *** | |
| Understanding others’ perspectives | 0.888 | 0.523 | 0.187 | 4.753 *** | |
| Action-oriented strategies | Self-leadership | 1.000 | 0.013 | ||
| Self-rewarding strategies | 0.565 | 0.581 | 0.216 | 0.149 | |
| Constructive thinking | 0.766 | 0.714 | 0.926 | 0.148 | |
| Nursing ethics | Self-efficacy | 1.000 | 0.720 | ||
| Communicating with patients | 0.941 | 0.714 | 0.102 | 9.182 *** | |
| Knowledge and clinical skills | 1.274 | 0.797 | 0.124 | 10.297 *** | |
| Nursing attitudes | Nursing performance | 1.000 | 0.795 | ||
| Nursing competency | 0.821 | 0.719 | 0.082 | 9.995 *** | |
| Application of nursing process | 1.090 | 0.804 | 0.095 | 11.524 *** | |
| Criteria | χ2 | df | p | CFI | GFI | TLI | RMSEA | RMR |
|---|---|---|---|---|---|---|---|---|
| Model fit | 87.051 | 50 | 0.000 | 0.960 | 0.931 | 0.938 | 0.067 | 0.019 |
| Criteria for fitness | ≥0.90 | ≥0.90 | ≥0.90 | ≤0.08 | ≤0.05 |
| Directions | Estimate (p) | Standardization Factor (β) | Standard Error (S.E.) | Critical Ratio (C.R.) |
|---|---|---|---|---|
| Communication ability → Self-leadership | 1.512 | 1.049 | 0.304 | 4.969 *** |
| Communication ability → Self-efficacy | 0.899 | 0.899 | 0.257 | 4.935 *** |
| Self-leadership → Nursing performance | −0.263 | −0.263 | 0.875 | −0.357 |
| Self-efficacy → Nursing performance | 0.464 | 0.464 | 0.532 | 3.300 *** |
| Communication ability → Nursing performance | −0.185 | −0.185 | 1.185 | −0.267 |
| Directions | Direct Effects | Indirect Effects | Gross Effects |
|---|---|---|---|
| Communication ability → Self-efficacy | 0.899 | - | 0.899 |
| Self-efficacy → Nursing performance | 0.464 | - | 0.464 |
| Communication ability → Nursing performance | - | 0.417 *** | 0.417 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, A.Y.; Sim, I.O. Mediating Factors in Nursing Competency: A Structural Model Analysis for Nurses’ Communication, Self-Leadership, Self-Efficacy, and Nursing Performance. Int. J. Environ. Res. Public Health 2020, 17, 6850. https://doi.org/10.3390/ijerph17186850
Kim AY, Sim IO. Mediating Factors in Nursing Competency: A Structural Model Analysis for Nurses’ Communication, Self-Leadership, Self-Efficacy, and Nursing Performance. International Journal of Environmental Research and Public Health. 2020; 17(18):6850. https://doi.org/10.3390/ijerph17186850
Chicago/Turabian StyleKim, Ae Young, and In Ok Sim. 2020. "Mediating Factors in Nursing Competency: A Structural Model Analysis for Nurses’ Communication, Self-Leadership, Self-Efficacy, and Nursing Performance" International Journal of Environmental Research and Public Health 17, no. 18: 6850. https://doi.org/10.3390/ijerph17186850
APA StyleKim, A. Y., & Sim, I. O. (2020). Mediating Factors in Nursing Competency: A Structural Model Analysis for Nurses’ Communication, Self-Leadership, Self-Efficacy, and Nursing Performance. International Journal of Environmental Research and Public Health, 17(18), 6850. https://doi.org/10.3390/ijerph17186850





