Effects of a Person-Centered Nursing Intervention for Frailty among Prefrail Community-Dwelling Older Adults
Abstract
1. Introduction
2. Materials and Methods
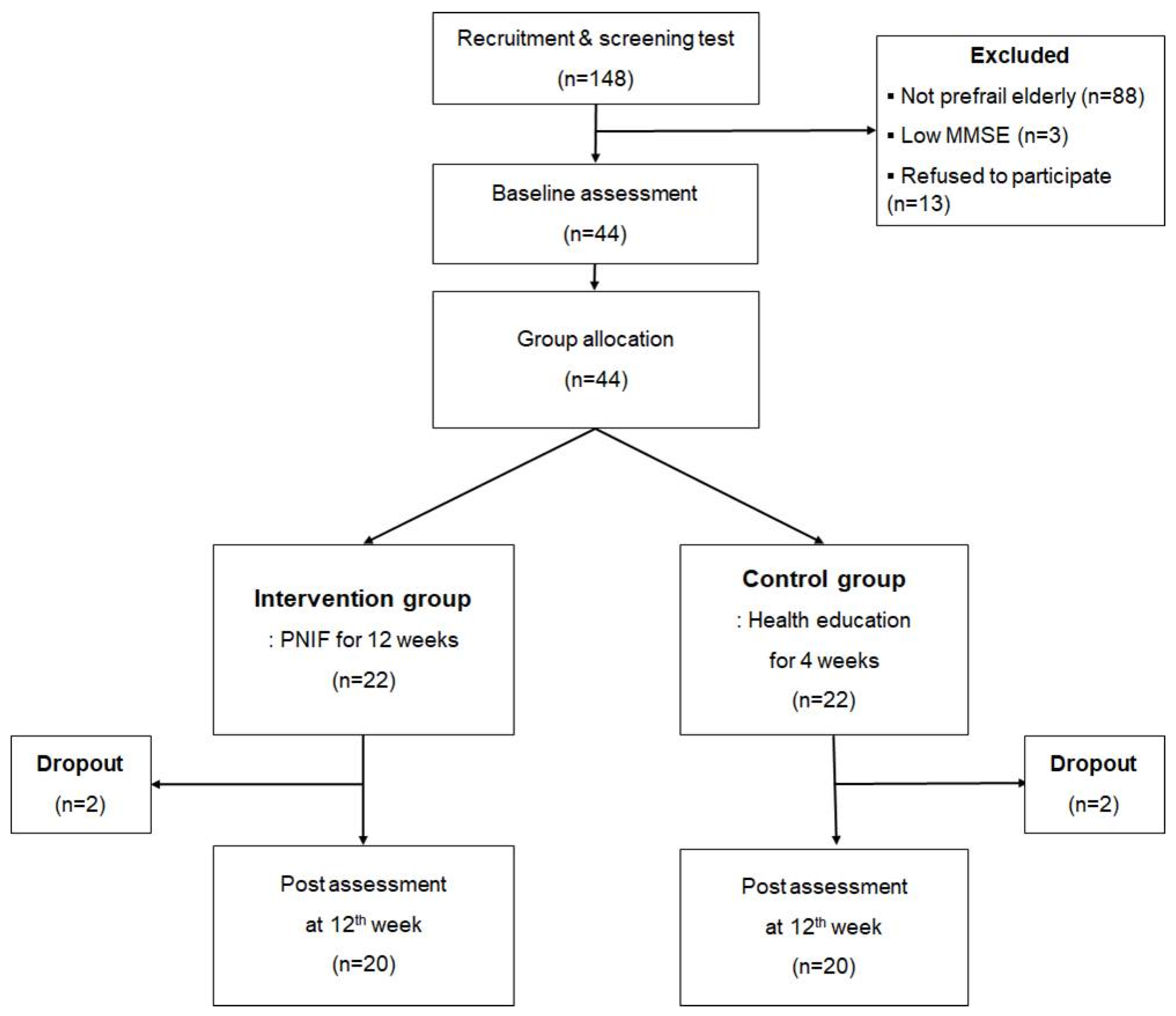
2.1. Study Design
2.2. Participants
2.3. Ethical Considerations
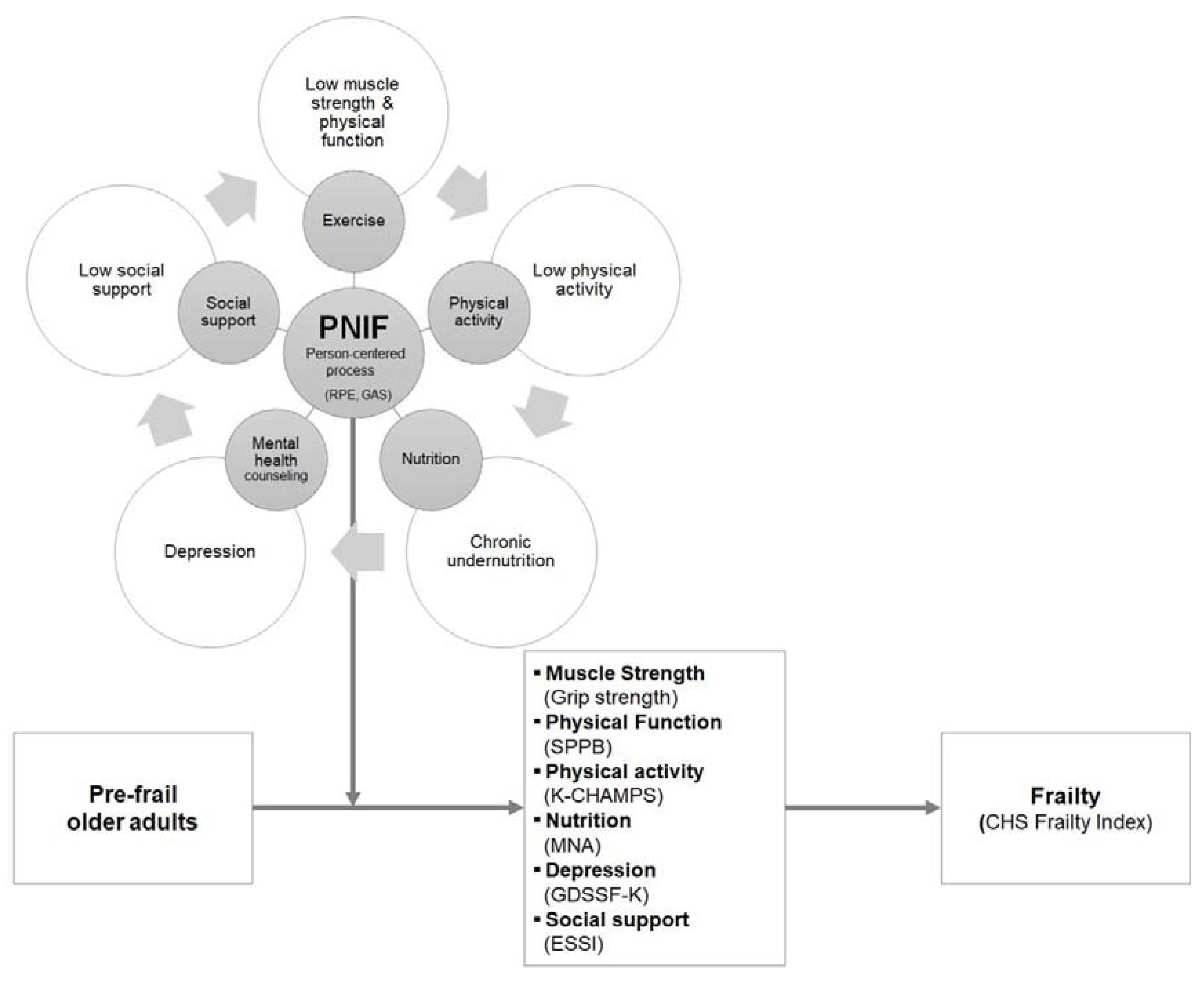
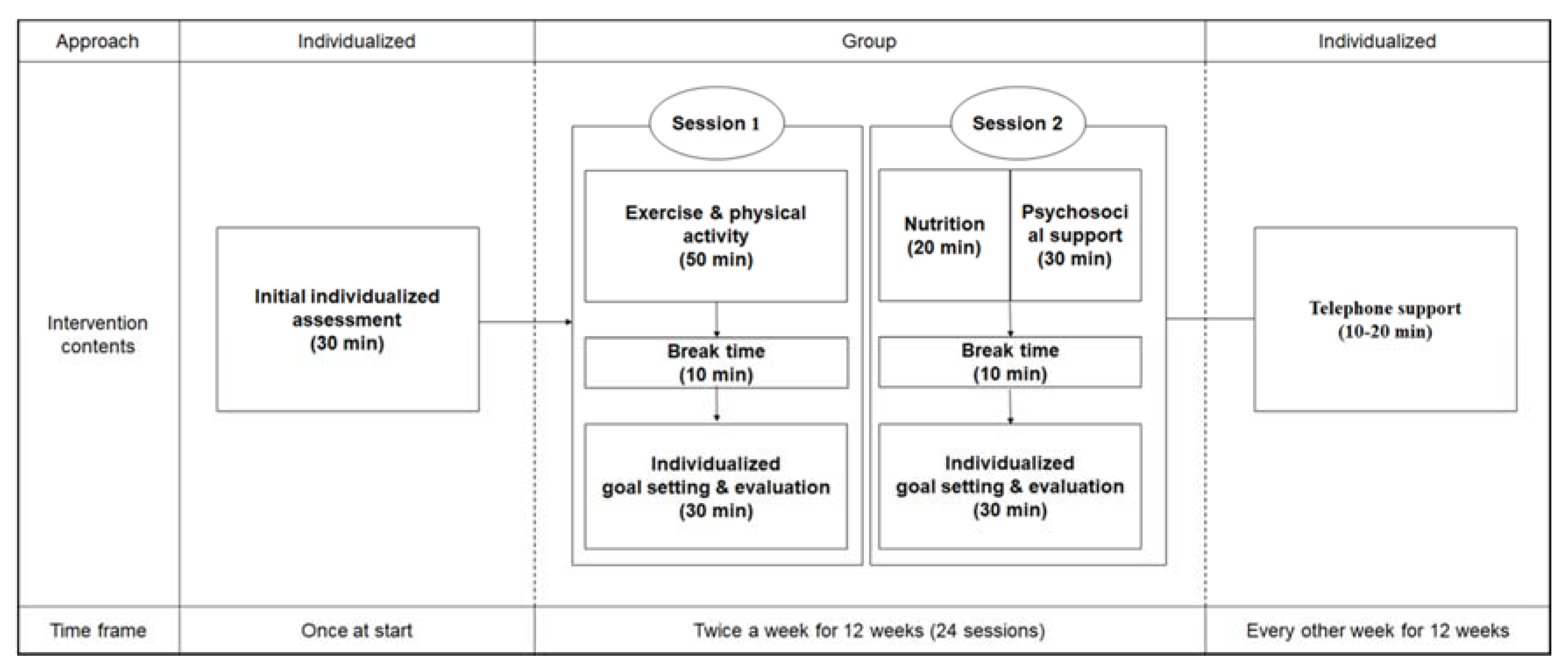
2.4. Intervention Program
2.4.1. Content of the PNIF
Exercise and Physical Activity Intervention (Session 1)
2.4.2. Control Group
2.5. Outcome Measurements
2.5.1. Demographic and Clinical Characteristics
2.5.2. Cardiovascular Health Study Frailty Index
2.5.3. Grip Strength
2.5.4. Short Physical Performance Battery
2.5.5. Korean Version of the Community Healthy Activities Model Program for Seniors Questionnaire
2.5.6. Mini Nutritional Assessment
2.5.7. Geriatric Depression Scale Short Form-Korea Version
2.5.8. ENRICHD Social Support Instrument
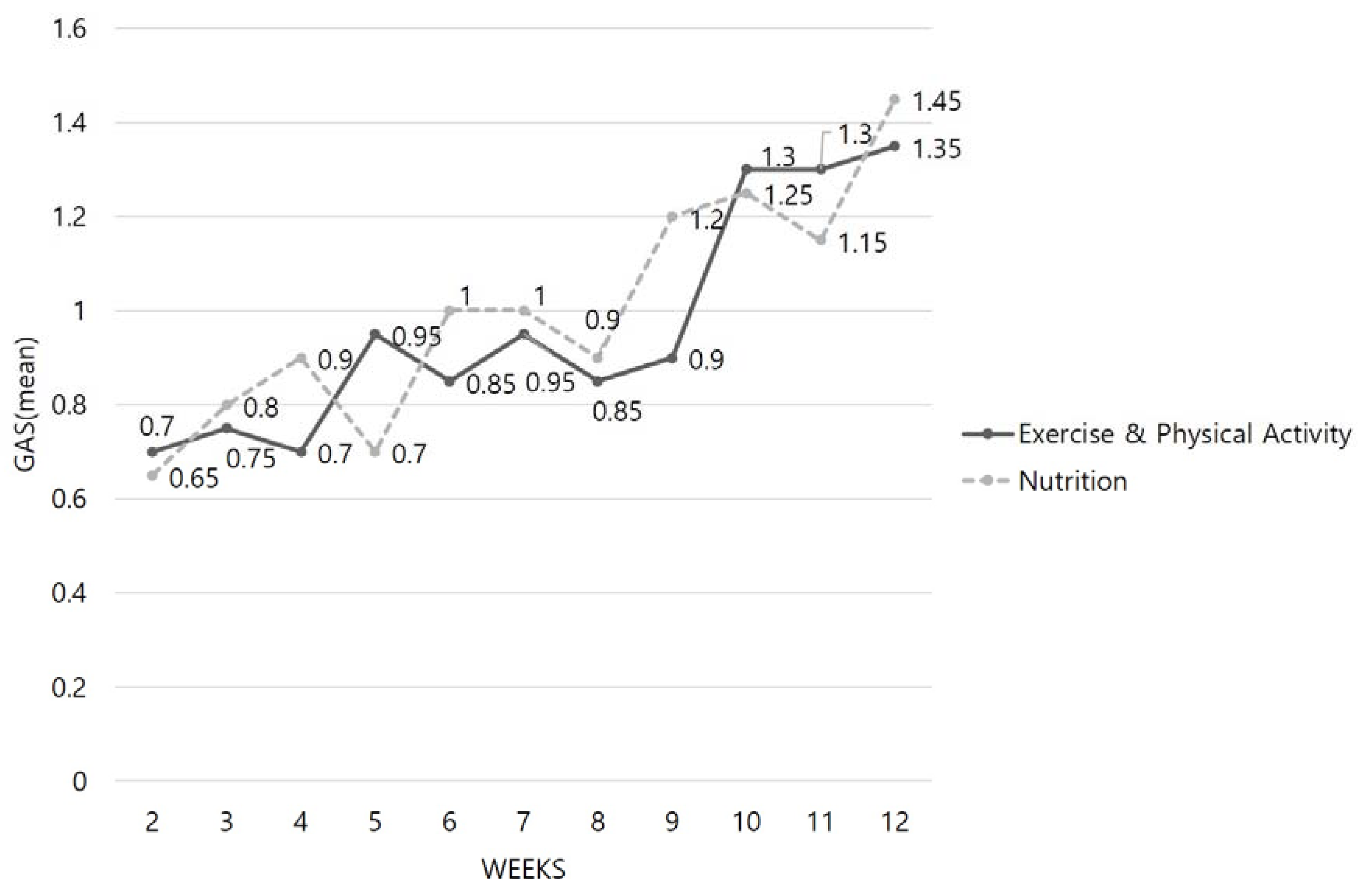
2.5.9. Goal Attainment Scale
2.6. Data Collection
2.7. Statistical Analysis
3. Results
3.1. Demographic, Clinical Characteristics and Outcome Variables at Baseline
3.2. Post-Intervention Outcome Comparison
3.2.1. Cardiovascular Health Study Frailty Index
3.2.2. Grip Strength
3.2.3. Short Physical Performance Battery
3.2.4. Korean Version of the Community Healthy Activities Model Program for Seniors Questionnaire
3.2.5. Mini Nutritional Assessment
3.2.6. Geriatric Depression Scale Short Form-Korea Version
3.2.7. ENRICHD Social Support Instrument
3.3. Goal Attainment Scale Analysis Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Week | Nutritional Intervention Session | Psychosocial Support Intervention |
|---|---|---|
| 1 |
|
|
| 2 |
|
|
| 3 |
|
|
| 4 |
|
|
| 5 |
|
|
| 6 |
|
|
| 7 |
|
|
| 8 |
|
|
| 9 |
|
|
| 10 |
|
|
| 11 |
|
|
| 12 |
|
|
Appendix B
| Outcome Variables | Data Collection Method | Test-Retest Reliability or Cronbach’s Alpha | |
|---|---|---|---|
| 1 | CHS Frailty Index |
| |
| 2 | Grip strength (by JAMAR® hydraulic hand dynamometer) |
| 0.94 |
| 3 | SPPB |
| 0.97 |
| 4 | K-CHAMPS |
| 0.54 |
| 5 | MNA |
| 0.70 |
| 6 | GDSSF-K |
| 0.87 |
| 7 | ESSI |
| 0.73 |
| 8 | GAS |
|
References
- Ploeg, J.; Matthew-Maich, N.; Fraser, K.; Dufour, S.; McAiney, C.; Kaasalainen, S.; Markle-Reid, M.; Upshur, R.; Cleghorn, L.; Emili, A. Managing multiple chronic conditions in the community: A Canadian qualitative study of the experiences of older adults, family caregivers and healthcare providers. BMC Geriatr. 2017, 17, 1–15. [Google Scholar] [CrossRef]
- Data Portal. Available online: https://www.data.go.kr/data/15004296/fileData.do (accessed on 19 August 2020).
- Buckinx, F.; Rolland, Y.; Reginster, J.-Y.; Ricour, C.; Petermans, J.; Bruyère, O. Burden of frailty in the elderly population: Perspectives for a public health challenge. Arch. Public Health 2015, 73, 1–7. [Google Scholar] [CrossRef]
- Kim, C.O.; Lee, H.Y.; Ho, S.H.; Park, H.S.; Park, C.W. Effects of visiting prehabilitation program against functional decline in the frail elderly: A prospective randomized community trial. J. Korean Gerontol. Soc. 2010, 30, 1293–1309. [Google Scholar]
- Collard, R.M.; Boter, H.; Schoevers, R.A.; Oude Voshaar, R.C. Prevalence of frailty in community-dwelling older persons: A systematic review. J. Am. Geriatr. Soc. 2012, 60, 1487–1492. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.S.; Kwon, I.S.; Park, B.J.; Cho, B.; Yoon, J.L.; Won, C.W. The validity and reliability of Korean frailty index. J. Korean Geriatr. Soc. 2010, 14, 191–202. [Google Scholar] [CrossRef]
- Levers, M.J.; Estabrooks, C.A.; Ross Kerr, J.C. Factors contributing to frailty: Literature review. J. Adv. Nurs. 2006, 56, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Fairhall, N.; Kurrle, S.E.; Sherrington, C.; Lord, S.R.; Lockwood, K.; John, B.; Monaghan, N.; Howard, K.; Cameron, I.D. Effectiveness of a multifactorial intervention on preventing development of frailty in pre-frail older people: Study protocol for a randomised controlled trial. BMJ Open 2015, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Ferrucci, L.; Darer, J.; Williamson, J.D.; Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, M255–M263. [Google Scholar] [CrossRef]
- Subra, J.; Gillette-Guyonnet, S.; Cesari, M.; Oustric, S.; Vellas, B. The integration of frailty into clinical practice: Preliminary results from the Gerontopole. J. Nutr. Health Aging 2012, 16714–16720. [Google Scholar] [CrossRef]
- Lee, J.S.; Auyeung, T.W.; Leung, J.; Kwok, T.; Woo, J. Transitions in frailty states among community-living older adults and their associated factors. J. Am. Med. Dir. Assoc. 2014, 15, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Cameron, I.D.; Fairhall, N.; Langron, C.; Lockwood, K.; Monaghan, N.; Aggar, C.; Sherrington, C.; Lord, S.R.; Kurrle, S.E. A multifactorial interdisciplinary intervention reduces frailty in older people: Randomized trial. BMC Med. 2013, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Lee, Y.S.; Chan, D.C. Interventions targeting geriatric frailty: A systemic review. J. Clin. Gerontol. Geriatr. 2012, 3, 47–52. [Google Scholar] [CrossRef][Green Version]
- Lee, I.S.; Ko, Y.; Lee, K.O.; Yim, E.S. Evaluation of the effects of a frailty preventing multi-factorial program concentrated on local communities for high-risk younger and older elderly people. J. Korean Acad. Community Health Nurs. 2012, 23, 201–211. [Google Scholar] [CrossRef][Green Version]
- Kwon, S.M.; Park, J.S. The effect of health promotion program for frail elderly residents on health promoting behavior and health status. Korean J. Adult Nurs. 2013, 25, 194–206. [Google Scholar] [CrossRef]
- Beswick, A.D.; Rees, K.; Dieppe, P.; Ayis, S.; Gooberman-Hill, R.; Horwood, J.; Ebrahim, S. Complex interventions to improve physical function and maintain independent living in elderly people: A systematic review and meta-analysis. Lancet 2008, 371, 725–735. [Google Scholar] [CrossRef]
- Beck, C.; McSweeney, J.C.; Richards, K.C.; Roberson, P.K.; Tsai, P.-F.; Souder, E. Challenges in tailored intervention research. Nurs. Outlook 2010, 58, 104–110. [Google Scholar] [CrossRef]
- Brummel-Smith, K.; Butler, D.; Frieder, M.; Gibbs, N.; Henry, M.; Koons, E.; Loggers, E.; Porock, D.; Reuben, D.B.; Saliba, D.; et al. Person-centered care: A definition and essential elements. J. Am. Geriatr. Soc. 2016, 64, 15–18. [Google Scholar] [CrossRef]
- McCance, T.; McCormack, B.; Dewing, J. An exploration of person-centredness in practice. Online J. Issues Nurs. 2011, 16, 1–9. [Google Scholar] [CrossRef]
- Kogan, A.C.; Wilber, K.; Mosqueda, L. Person-centered care for older adults with chronic conditions and functional impairment: A systematic literature review. J. Am. Geriatr. Soc. 2016, 64, e1–e7. [Google Scholar] [CrossRef]
- Chatterji, S.; Byles, J.; Cutler, D.; Seeman, T.; Verdes, E. Health, functioning, and disability in older adults—Present status and future implications. Lancet 2015, 385, 563–575. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef] [PubMed]
- Best-Martini, E.; Jones-DiGenova, K. Exercise for Frail Elders, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2014; pp. 1–336. [Google Scholar]
- Hyun-ju, L. A Study on the application of goal attainment scaling in the evaluation of social work practice -focusing on the evaluation of the program for the improvement of daily living function of people with mental illness. Ment. Health Soc. Work 2011, 39, 120–154. [Google Scholar]
- Ensrud, K.E.; Ewing, S.K.; Taylor, B.C.; Fink, H.A.; Cawthon, P.M.; Stone, K.L.; Hillier, T.A.; Cauley, J.A.; Hochberg, M.C.; Rodondi, N.; et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch. Intern. Med. 2008, 168, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Peterson, M.J.; Giuliani, C.; Morey, M.C.; Pieper, C.F.; Evenson, K.R.; Mercer, V.; Cohen, H.J.; Visser, M.; Brach, J.S.; Kritchevsky, S.B.; et al. Physical activity as a preventative factor for frailty: The health, aging, and body composition study. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64A, 61–68. [Google Scholar] [CrossRef]
- Chen, L.K.; Liu, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Bahyah, K.S.; Chou, M.-Y.; Hsu, P.-S.; Krairit, O.; Lee, J.S.; et al. Sarcopenia in Asia: Consensus report of the Asian working group for sarcopenia. J. Am. Med. Dir. Assoc. 2014, 15, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Peolsson, A.; Hedlund, R.; Öberg, B. Intra-and inter-tester reliability and reference values for hand strength. J. Rehabil. Med. 2001, 33, 36–41. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef]
- Gómez, J.F.; Curcio, C.L.; Alvarado, B.; Zunzunegui, M.V.; Guralnik, J. Validity and reliability of the Short Physical Performance Battery (SPPB): A pilot study on mobility in the Colombian Andes. Colomb. Med. 2013, 44, 165–171. [Google Scholar] [CrossRef]
- Stewart, A.L.; Mills, K.M.; King, A.C.; Haskell, W.L.; Gillis, D.; Ritter, P.L. CHAMPS physical activity questionnaire for older adults: Outcomes for interventions. Med. Sci. Sports Exerc. 2001, 33, 1126–1141. [Google Scholar] [CrossRef]
- Lim, K.C. Reliability and validity of K-CHAMPS questionnaire for older Koreans. J. Korean Gerontol. Nurs. 2011, 13, 142–153. [Google Scholar]
- Rubenstein, L.Z.; Harker, J.O.; Salvà, A.; Guigoz, Y.; Vellas, B. Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF). J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef] [PubMed]
- Yesavage, J.A.; Sheikh, J.I. 9/Geriatric Depression Scale (GDS) recent evidence and development of a shorter version. Clin. Gerontol. 1986, 5, 165–173. [Google Scholar] [CrossRef]
- Kee, B.S. A preliminary study for the standardization of geriatric depression scale short form-Korea version. J. Korean Neuropsychiatr. Assoc. 1996, 35, 298–307. [Google Scholar]
- Jeon, G.S.; Jang, S.N.; Park, S. Social support, social network, and frailty in Korean elderly. J. Korean Geriatr. Soc. 2012, 16, 84–94. [Google Scholar] [CrossRef]
- Choi, K.W.; Jeon, G.S. Effects of frailty on health-related quality of life of rural community-dwelling elderly: Mediating and moderating effects of fall-related efficacy and social support. J. Korean Acad. Community Health Nurs. 2016, 27, 380–387. [Google Scholar] [CrossRef]
- Mitchell, P.H.; Powell, L.; Blumenthal, J.; Norten, J.; Ironson, G.; Pitula, C.R.; Froelicher, E.S.; Czajkowski, S.; Youngblood, M.; Huber, M.; et al. A short social support measure for patients recovering from myocardial infarction: The ENRICHD Social Support Inventory. J. Cardiopulm. Rehabil. Prev. 2003, 23, 398–403. [Google Scholar] [CrossRef]
- Kiresuk, T.J.; Sherman, M.R.E. Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Ment. Health J. 1968, 4, 443–453. [Google Scholar] [CrossRef]
- Choi, Y.J.; Kim, K.M.; Shin, Y.B.; Chang, M.Y. The effects of activities of daily living training based on neurodevelopmental treatment principles for the occupations of children with cerebral palsy. J. Korean Soc. Occup. Ther. 2011, 19, 55–67. [Google Scholar]
- De Vries, N.M.; Staal, J.B.; van der Wees, P.J.; Adang, E.M.; Akkermans, R.; Olde Rikkert, M.G.; Nijhuis-van der Sanden, M.W. Patient-centred physical therapy is (cost) effective in increasing physical activity and reducing frailty in older adults with mobility problems: A randomized controlled trial with 6 months follow-up. J. Cachexia Sarcopenia Muscle 2016, 7, 422–435. [Google Scholar] [CrossRef]
- Henwood, T.; Tuckett, A.; Edelstein, O.; Bartlett, H. Exercise in later life: The older adults’ perspective about resistance training. Ageing Soc. 2011, 31, 1330–1349. [Google Scholar] [CrossRef]
- Zech, A.; Drey, M.; Freiberger, E.; Hentschke, C.; Bauer, J.M.; Sieber, C.C.; Pfeifer, K. Residual effects of muscle strength and muscle power training and detraining on physical function in community-dwelling prefrail older adults: A randomized controlled trial. BMC Geriatr. 2012, 12, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Dedeyne, L.; Deschodt, M.; Verschueren, S.; Tournoy, J.; Gielen, E. Effects of multi-domain interventions in (pre) frail elderly on frailty, functional, and cognitive status: A systematic review. Clin. Interv. Aging 2017, 12, 873–896. [Google Scholar] [CrossRef] [PubMed]
- Gitlin, L.N. Introducing a new intervention: An overview of research phases and common challenges. Am. J. Occup. Ther. 2013, 67, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Park, Y.H. Predictors of physical activity in korean older adults: Distinction between urban and rural areas. J. Korean Acad. Nurs. 2010, 40, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Browning, C.; Sims, J.; Kendig, H.; Teshuva, K. Predictors of physical activity behavior in older community-dwelling adults. J. Allied Health 2009, 38, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.J.; Kim, J.H.; Park, O.J.; Lee, Y.M. A study on the needs for nutrition management program for elderly who use welfare facilities. Korean J. Community Nutr. 2016, 21, 65–74. [Google Scholar] [CrossRef]
- Mhaoláin, A.M.N.; Fan, C.W.; Romero-Ortuno, R.; Cogan, L.; Cunningham, C.; Kenny, R.A.; Lawlor, B. Frailty, depression, and anxiety in later life. Int. Psychogeriatr. 2012, 24, 1265–1274. [Google Scholar] [CrossRef] [PubMed]
- Andrew, M.K.; Mitnitski, A.B.; Rockwood, K. Social vulnerability, frailty and mortality in elderly people. PLoS ONE 2008, 3, e2232. [Google Scholar] [CrossRef]
- McCormack, B.; McCance, T.V. Person-Centred Nursing: Theory, Models and Methods, 1st ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2010; pp. 1–208. [Google Scholar]
- Olsson, L.E.; Ung, E.J.; Swedberg, K.; Ekman, I. Efficacy of person-centred care as an intervention in controlled trials—A systematic review. J. Clin. Nurs. 2012, 22, 456–465. [Google Scholar] [CrossRef]
| Characteristics | Intervention Group (n = 20) | Control Group (n = 20) | χ2 or t | p | |
|---|---|---|---|---|---|
| n (%) or Mean (SD) | n (%) or Mean (SD) | ||||
| Age (year) | 77.10 (6.40) | 79.30 (4.89) | −1.23 | 0.227 | |
| Sex | Male | 4 (20.0%) | 8 (40.0%) | 1.91 | 0.168 |
| Female | 16 (80.0%) | 12 (60.0%) | |||
| Educational level | None | 0 (0.0%) | 2 (10.0%) | 4.65 * | 0.320 |
| Elementary school | 5 (25.0%) | 8 (40.0%) | |||
| Middle school | 4 (20.0%) | 5 (25.0%) | |||
| High school | 7 (35.0%) | 3 (15.0%) | |||
| University or above | 4 (20.0%) | 2 (10.0%) | |||
| Mean (SD) | 10.10 (4.10) | 7.45 (4.72) | 1.90 | 0.066 | |
| Marital status | Married | 8 (40.0%) | 7 (35.0%) | 0.28 * | 1.000 |
| Widowed | 10 (50.0%) | 11 (55.0%) | |||
| Divorced | 0 (0.0%) | 0 (0.0%) | |||
| Separated | 2 (10.0%) | 2 (10.0%) | |||
| Not married | 0 (0.0%) | 0 (0.0%) | |||
| Family type | Solitary | 10 (50.0%) | 6 (30.0%) | 2.60 | 0.295 |
| Spouse | 7 (35.0%) | 7 (35.0%) | |||
| Others | 3 (15.0%) | 7 (35.0%) | |||
| Religion | Yes | 19 (95.0%) | 18 (90.0%) | 7.21 * | 0.050 |
| No | 1 (5.0%) | 2 (10.0%) | |||
| Perceived economic status | Upper | 0 (0.0%) | 0 (0.0%) | 3.60 | 0.058 |
| Middle | 13 (65.0%) | 7 (35.0%) | |||
| Lower | 7 (35.0%) | 13 (65.0%) | |||
| Number of chronic diseases | 4.20 (2.33) | 3.80 (2.40) | −0.52 a | 0.620 | |
| MMSE-KC | 26.25 (0.68) | 25.75 (0.52) | 0.59 b | 0.562 | |
| CHS frailty index | 1.45 (0.51) | 1.25 (0.44) | −1.31 a | 0.289 | |
| Grip strength | Left | 22.40 (7.16) | 21.05 (7.19) | 0.60 b | 0.556 |
| Right | 21.70 (7.84) | 21.10 (7.25) | 0.25 b | 0.803 | |
| SPPB | 10.30 (1.49) | 9.70 (1.81) | −1.07 a | 0.301 | |
| K-CHAMPS (Kcal/week) | 2582.53 (1569.18) | 1631.43 (1360.46) | −1.84 a | 0.068 | |
| MNA | 22.50 (3.48) | 21.68 (4.26) | −0.91 a | 0.369 | |
| GDSSF-K | 6.15 (3.80) | 4.35 (3.39) | 1.58 b | 0.122 | |
| ESSI | 5.25 (1.12) | 5.00 (1.34) | −0.52 a | 0.640 | |
| Characteristics | Group | Pretest | Posttest | Difference | t/Z | p |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||||
| CHS frailty index | Intervention group (n = 20) | 1.45 (0.51) | 0.70 (0.73) | −0.75 (0.85) | −3.558 a | <0.001 |
| Control group (n = 20) | 1.25 (0.44) | 1.80 (1.01) | 0.55 (1.10) | |||
| Grip strength, Left-hand (kg) | Intervention group | 22.40 (7.16) | 25.05 (5.07) | 2.65 (4.63) | 2.387 b | 0.022 |
| Control group | 21.05 (7.19) | 19.70 (7.36) | −1.35 (5.90) | |||
| Grip strength, Right-hand (kg) | Intervention group | 21.70 (7.84) | 26.75 (4.72) | 5.05 (5.72) | 2.733 b | 0.009 |
| Control group | 21.10 (7.25) | 21.85 (6.69) | 0.75 (4.10) | |||
| SPPB | Intervention group | 10.30 (1.49) | 10.90 (1.52) | 0.60 (1.27) | −2.741 a | 0.007 |
| Control group | 9.70 (1.81) | 9.10 (1.94) | −0.60 (1.35) | |||
| K-CHAMPS | Intervention group | 2582.53 (1569.18) | 3471.19 (1990.50) | 888.65 (1858.09) | −2.570 a | 0.009 |
| Control group | 1631.43 (1360.46) | 1457.44 (1393.20) | −174.00 (810.74) | |||
| MNA | Intervention group | 22.50 (3.48) | 25.08 (2.44) | 2.58 (2.42) | −2.361 a | 0.018 |
| Control group | 21.68 (4.26) | 22.25 (4.54) | 0.57 (2.07) | |||
| GDSSF-K | Intervention group | 6.15 (3.80) | 4.75 (3.80) | −1.40 (2.30) | −3.750 b | 0.001 |
| Control group | 4.35 (3.39) | 5.65 (4.18) | 1.30 (2.25) | |||
| ESSI | Intervention group | 5.25 (1.12) | 5.10 (1.29) | −0.15 (1.42) | −0.322 a | 0.779 |
| Control group | 5.00 (1.34) | 4.60 (1.70) | −0.40 (1.88) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ha, J.; Park, Y.-H. Effects of a Person-Centered Nursing Intervention for Frailty among Prefrail Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 6660. https://doi.org/10.3390/ijerph17186660
Ha J, Park Y-H. Effects of a Person-Centered Nursing Intervention for Frailty among Prefrail Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health. 2020; 17(18):6660. https://doi.org/10.3390/ijerph17186660
Chicago/Turabian StyleHa, Jiyeon, and Yeon-Hwan Park. 2020. "Effects of a Person-Centered Nursing Intervention for Frailty among Prefrail Community-Dwelling Older Adults" International Journal of Environmental Research and Public Health 17, no. 18: 6660. https://doi.org/10.3390/ijerph17186660
APA StyleHa, J., & Park, Y.-H. (2020). Effects of a Person-Centered Nursing Intervention for Frailty among Prefrail Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health, 17(18), 6660. https://doi.org/10.3390/ijerph17186660





