Prevalence of Anxiety in Medical Students during the COVID-19 Pandemic: A Rapid Systematic Review with Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
2.3. Methodological Quality Assessment
2.4. Data Extraction and Statistical Analysis
2.5. Data Availability Statement
3. Results
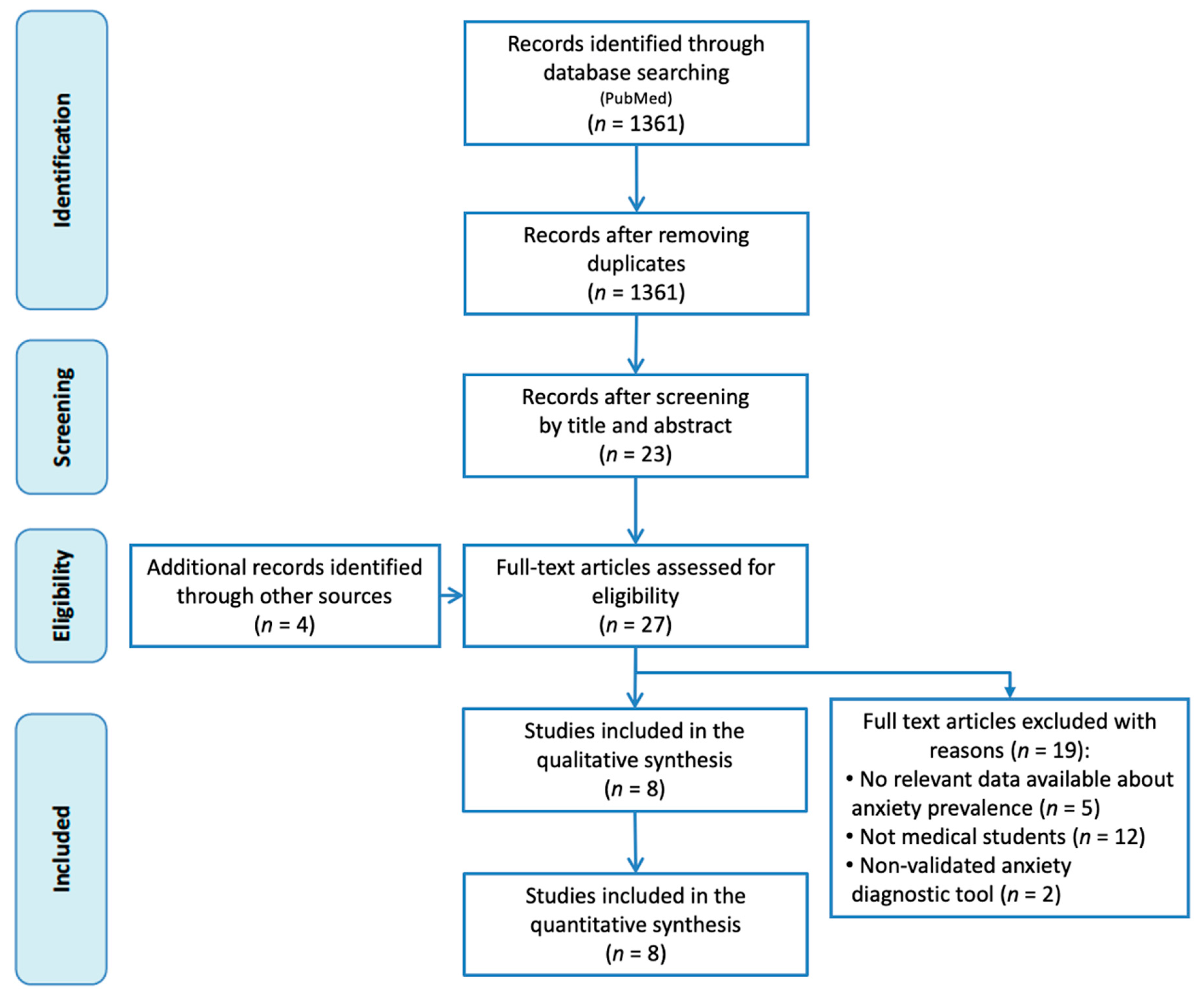
3.1. Identification and Selection of Articles
3.2. Characteristics of the Studies Included
3.3. Quality Assessment
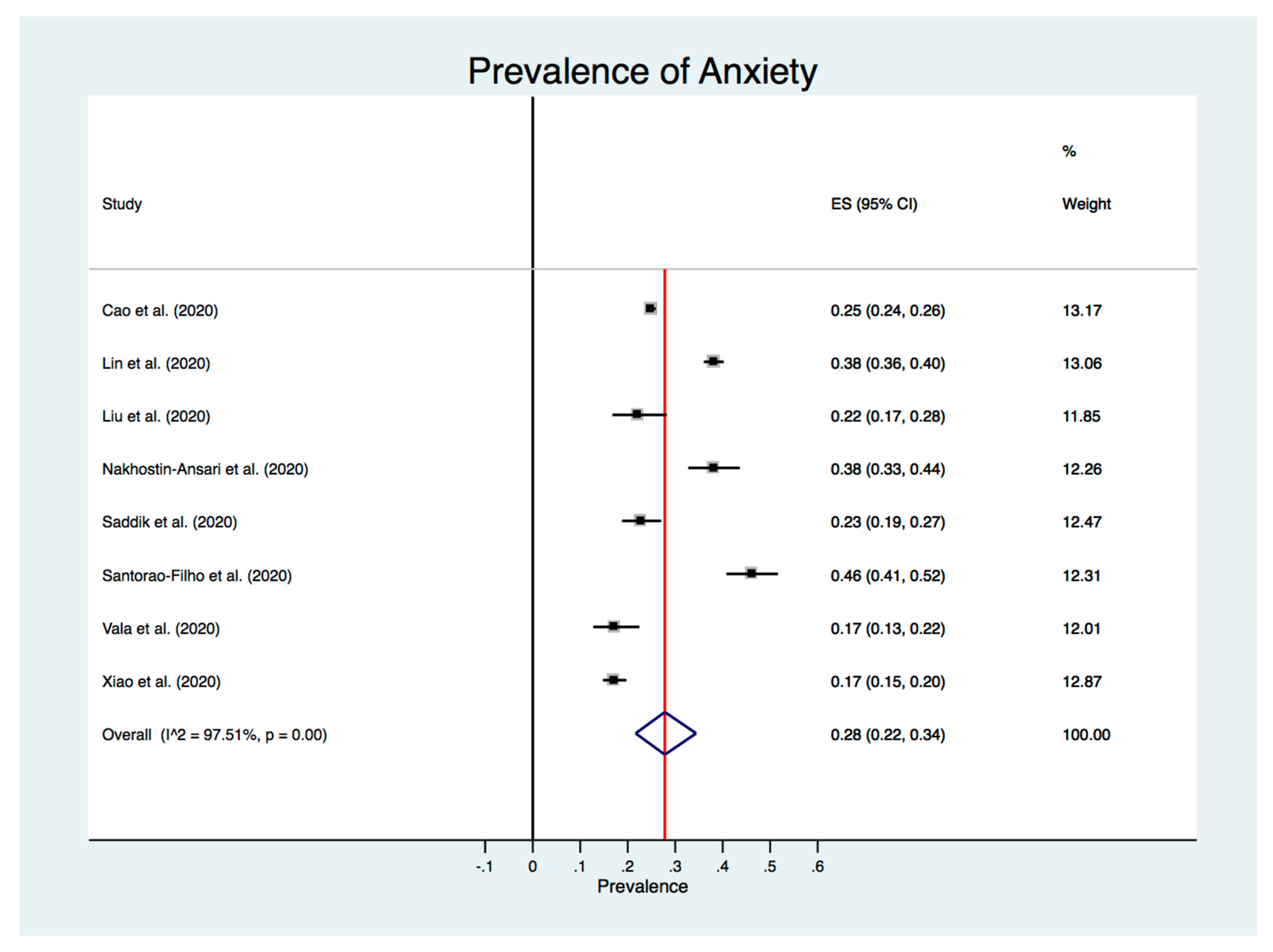
3.4. Meta-Analysis of the Prevalence of Anxiety
3.5. Meta-Regression and Subgroup Analysis
3.6. Sensitive Analysis
3.7. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 2 July 2020).
- World Health Organization. Coronavirus Disease (COVID-19) Situation Dashboard. Available online: https://covid19.who.int/ (accessed on 2 September 2020).
- Yang, H.; Bin, P.; He, A.J. Opinions from the epicenter: An online survey of university students in Wuhan amidst the COVID-19 outbreak 1. J. Chin. Gov. 2020, 5, 234–248. [Google Scholar] [CrossRef]
- Li, H.Y.; Cao, H.; Leung, D.Y.P.; Mak, Y.W. The Psychological impacts of a COVID-19 outbreak on College students in China: A longitudinal study. Int. J. Environ. Res. Public Health 2020, 17, 3933. [Google Scholar] [CrossRef] [PubMed]
- Lei, L.; Huang, X.; Zhang, S.; Yang, J.; Yang, L.; Xu, M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med. Sci. Monit. 2020, 26, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Saddik, B.; Hussein, A.; Sharif-Askari, F.S.; Kheder, W.; Temsah, M.; Koutaich, R.A.; Haddad, E.S.; Al-Roub, N.M.; Marhoon, F.A.; Hamid, Q.; et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. medRxiv 2020, 1–17. [Google Scholar] [CrossRef]
- Zandifar, A.; Badrfam, R. Iranian mental health during the COVID-19 epidemic. Asian J. Psychiatry 2020, 51, 101990. [Google Scholar] [CrossRef] [PubMed]
- Huremović, D. (Ed.) Psychiatry of Pandemics A Mental Health Response to Infection Outbreak; Springer: Cham, Switzerland, 2019; ISBN 978-3-030-15346-5. [Google Scholar]
- Pfefferbaum, B.; North, C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020, 383. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Wong, T.W.; Gao, Y.; Tam, W.W.S. Anxiety among university students during the SARS epidemic in Hong Kong. Stress Health 2007, 23, 31–35. [Google Scholar] [CrossRef]
- Loh, L.C.; Ali, A.M.; Ang, T.H.; Chelliah, A. Impact of a spreading epidemic on medical students. Malays. J. Med. Sci. 2006, 13, 30–36. [Google Scholar]
- Quek, T.T.C.; Tam, W.W.S.; Tran, B.X.; Zhang, M.; Zhang, Z.; Ho, C.S.H.; Ho, R.C.M. The global prevalence of anxiety among medical students: A meta-analysis. Int. J. Environ. Res. Public Health 2019, 16, 2735. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Zhang, N.; Liu, J.; Zhu, B.; He, R.; Wang, X. A systematic review of depression and anxiety in medical students in China. BMC Med. Educ. 2019, 19, 327. [Google Scholar] [CrossRef] [PubMed]
- Hu, K.S.; Chibnall, J.T.; Slavin, S.J. Maladaptive perfectionism, impostorism, and cognitive distortions: Threats to the mental health of pre-clinical medical students. Acad. Psychiatry 2019, 43, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Komer, L. COVID-19 amongst the pandemic of medical student mental health. Int. J. Med. Stud. 2020, 8, 56–57. [Google Scholar] [CrossRef]
- Liu, J.; Zhu, Q.; Fan, W.; Makamure, J.; Zheng, C. Online mental health survey in a Medical College in China during the COVID-19 outbreak. Front. Psychiatry 2020, 11, 459. [Google Scholar] [CrossRef]
- Miller, D.G.; Pierson, L.; Doernberg, S. The role of medical students during the COVID-19 pandemic. Ann. Intern. Med. 2020, 173, 146. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Qureshi, P.; Mattis, P.; et al. Chapter 7: Systematic reviews of etiology and risk. In Joanna Briggs Institute Reviewer’s Manual; Aromataris, E., Munn, Z., Eds.; The Joanna Briggs Institute: Adelaide, Australia, 2017; pp. 219–226. [Google Scholar]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Singh, A.; Hussain, S.; Najmi, A.K. Number of studies, heterogeneity, generalisability, and the choice of method for meta-analysis. J. Neurol. Sci. 2017, 381, 347. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Updated March 2019); The Cochrane Collaboration: London, UK, 2019. [Google Scholar]
- Lin, Y.; Hu, Z.; Alias, H.; Wong, L.P. Influence of mass and social media on psychobehavioral responses among medical students during the downward trend of COVID-19 in Fujian, China: Cross-Sectional study. J. Med. Internet Res. 2020, 22, e19982. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Shu, W.; Li, M.; Li, Z.; Fangbiao, T.; Xiaoyan, W.; Yizhen, Y. Social distancing among Medical students during the 2019 Coronavirus disease pandemic in China: Disease awareness, anxiety disorder, depression, and behavioral activities. Int. J. Environ. Res. Public Health 2020, 17, 5047. [Google Scholar] [CrossRef] [PubMed]
- Nakhostin-Ansari, A.; Sherafati, A.; Aghajani, F.; Khonji, M.; Aghajani, R.; Shahmansouri, N. Depression and anxiety among Iranian Medical Students during COVID-19 pandemic. Iran. J. Psychiatry 2020, 15, 228–235. [Google Scholar] [CrossRef]
- Sartorão-Filho, C.I.; de Las Villas Rodrigues, W.C.; de Castro, R.B.; Marçal, A.A.; Pavelqueires, S.; Takano, L.; de Oliveira, W.L.; Sartorão-Neto, C.I. Impact of Covid-19 pandemic on mental health of Medical students: A cross-sectional study using GAD-7 and PHQ-9 questionnaires. medRxiv 2020. [Google Scholar] [CrossRef]
- Vala, N.H.; Vachhani, M.V.; Sorani, A.M. Study of anxiety, stress, and depression level among medical students during COVID-19 pandemic phase in Jamnagar city. Natl. J. Physiol. Pharm. Pharmacol. 2020, 10. [Google Scholar] [CrossRef]
- Dyrbye, L.N.; Thomas, M.R.; Shanafelt, T.D. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad. Med. 2006, 81, 354–373. [Google Scholar] [CrossRef] [PubMed]
- Zeng, W.; Chen, R.; Wang, X.; Zhang, Q.; Deng, W. Prevalence of mental health problems among medical students in China: A meta-analysis. Medicine 2019, 98. [Google Scholar] [CrossRef]
- Yusoff, M.S.B.; Abdul Rahim, A.F.; Baba, A.A.; Ismail, S.B.; Mat Pa, M.N.; Esa, A.R. Prevalence and associated factors of stress, anxiety and depression among prospective medical students. Asian J. Psychiatry 2013, 6, 128–133. [Google Scholar] [CrossRef]
- Rapaport, M.H.; Clary, C.; Fayyad, R.; Endicott, J. Quality-of-Life impairment in depressive and anxiety disorders. Am. J. Psychiatry 2005, 162, 1171–1178. [Google Scholar] [CrossRef]
- Pankiewicz, P.; Majkowicz, M.; Krzykowski, G. Anxiety disorders in intimate partners and the quality of their relationship. J. Affect. Disord. 2012, 140, 176–180. [Google Scholar] [CrossRef]
- Jacobson, N.C.; Newman, M.G. Anxiety and depression as bidirectional risk factors for one another: A meta-analysis of longitudinal studies. Psychol. Bull. 2017, 143, 1155–1200. [Google Scholar] [CrossRef]
- Al-Rabiaah, A.; Temsah, M.-H.; Al-Eyadhy, A.A.; Hasan, G.M.; Al-Zamil, F.; Al-Subaie, S.; Alsohime, F.; Jamal, A.; Alhaboob, A.; Al-Saadi, B.; et al. Middle East Respiratory Syndrome-Corona Virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. J. Infect. Public Health 2020, 13, 687–691. [Google Scholar] [CrossRef] [PubMed]
- Frajerman, A.; Morvan, Y.; Krebs, M.-O.; Gorwood, P.; Chaumette, B. Burnout in medical students before residency: A systematic review and meta-analysis. Eur. Psychiatry 2019, 55, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatry 2020, 51, 102076. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.; Yuan, Y.; Wang, D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao 2020, 40, 171–176. [Google Scholar] [CrossRef]
- Salman, M.; Asif, N.; Mustafa, Z.U.; Khan, T.M.; Shehzadi, N.; Hussain, K.; Tahir, H.; Raza, M.H.; Khan, M.T. Psychological impact of COVID-19 on Pakistani University students and how they are coping. medRxiv 2020. [Google Scholar] [CrossRef]
- Goulia, P.; Mantas, C.; Dimitroula, D.; Mantis, D.; Hyphantis, T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A / H1N1 influenza pandemic. BMC Infect. Dis. 2010, 10, 322. [Google Scholar] [CrossRef]
- Sögüt, S.; Dolu, İ.; Cangöl, E. The relationship between COVID-19 knowledge levels and anxiety states of midwifery students during the outbreak: A cross-sectional web-based survey. Perspect. Psychiatr. Care 2020, 1–7. [Google Scholar] [CrossRef]
- Ullah, R.; Amin, S. The psychological impact of COVID-19 on medical students [Letter]. Psychiatry Res. 2020, 288, 113020. [Google Scholar] [CrossRef]
- van der Merwe, L.J.; Botha, A.; Joubert, G. Resilience and coping strategies of undergraduate medical students at the University of the Free State. S. Afr. J. Psychiatry 2020, 26. [Google Scholar] [CrossRef]
- Chi, X.; Becker, B.; Yu, Q.; Willeit, P.; Jiao, C.; Huang, L.; Hossain, M.M.; Grabovac, I.; Yeung, A.; Lin, J.; et al. Prevalence and psychosocial correlates of mental health outcomes among Chinese College students during the Coronavirus Disease (COVID-19) pandemic. Front. Psychiatry 2020, 11, 803. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Logan, J.R.; Bian, F. Family values and coresidence with married children in urban China. Soc. Forces 1999, 77, 1253–1282. [Google Scholar] [CrossRef]
- Behar-Zusman, V.; Chavez, J.V.; Gattamorta, K. Developing a measure of the impact of COVID-19 social distancing on household conflict and cohesion. Fam. Process 2020, 1–15. [Google Scholar] [CrossRef]
- Huckins, J.F.; DaSilva, A.W.; Wang, W.; Hedlund, E.; Rogers, C.; Nepal, S.K.; Wu, J.; Obuchi, M.; Murphy, E.I.; Meyer, M.L.; et al. Mental health and behavior of College students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. J. Med. Internet Res. 2020, 22, e20185. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, H.; Ma, X.; Di, Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: A longitudinal study of College students in China. Int. J. Environ. Res. Public Health 2020, 17, 3722. [Google Scholar] [CrossRef]
- Huang, J.; Nigatu, Y.T.; Smail-Crevier, R.; Zhang, X.; Wang, J. Interventions for common mental health problems among university and college students: A systematic review and meta-analysis of randomized controlled trials. J. Psychiatr. Res. 2018, 107, 1–10. [Google Scholar] [CrossRef]
- Sun, L.; Sun, L.-N.; Sun, Y.-H.; Yang, L.-S.; Wu, H.-Y.; Zhang, D.-D.; Cao, H.-Y.; Sun, Y. Correlations between psychological symptoms and social relationships among medical undergraduates in Anhui Province of China. Int. J. Psychiatry Med. 2011, 42, 29–47. [Google Scholar] [CrossRef]
- Shek, D.T.L. The Chinese version of the State-Trait Anxiety Inventory: Its relationship to different measures of psychological well-being. J. Clin. Psychol. 1993, 49, 349–358. [Google Scholar] [CrossRef]
- He, X.Y.; Li, C.; Quian, J.; Cui, H.S.; Wu, W.Y. Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Arch. Psychiatry 2010, 22, 200–203. [Google Scholar] [CrossRef]
- Sawaya, H.; Atoui, M.; Hamadeh, A.; Zeinoun, P.; Nahas, Z. Adaptation and initial validation of the Patient Health Questionnaire—9 (PHQ-9) and the Generalized Anxiety Disorder—7 Questionnaire (GAD-7) in an Arabic speaking Lebanese psychiatric outpatient sample. Psychiatry Res. 2016, 239, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Demetriou, C.; Ozer, B.U.; Essau, C.A. Self-Report Questionnaires. In The Encyclopedia of Clinical Psychology; Cautin, R.L., Lilienfeld, S.O., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2015; pp. 1–6. [Google Scholar]
| Author (Year) | Country | Females (%) | Sample Size (n) | Response Rate (%) | Sampling Method | Anxiety Assessment | Prevalence of Anxiety (%) | Quality Score |
|---|---|---|---|---|---|---|---|---|
| Cao et al. (2020) [26] | China | 69.65% | 7143 | 100% | Cluster sampling | GAD-7 1 | 24.9% | 9 |
| Lin et al. (2020) [25] | China | Not reported | 2086 | Not reported | Convenience sampling | STAI-6 2 | 38.1% | 6 |
| Liu et al. (2020) [18] | China | 41.5% | 217 | Not reported | Convenience sampling | GAD-7 1 | 22.1% | 7 |
| Nakhostin-Ansari et al. (2020) [28] | Iran | 52.3% | 323 | 64.6% | Random sampling | BAI 3 | 38.1% | 8 |
| Saddik et al. (2020) [6] | United Arab Emirates | Not reported | 418 | Not reported | Convenience sampling | GAD-7 1 | 22.7% | 7 |
| Sartorao-Filho et al. (2020) [29] | Brazil | 73.80% | 340 | 97.98% | Convenience sampling | GAD-7 1 | 46.17% | 9 |
| Vala et al. (2020) [30] | India | 56% | 250 | Not reported | Convenience sampling | DASS-21 4 | 17.20% | 6 |
| Xiao et al. (2020) [27] | China | 70.1% | 933 | 96.2% | Convenience sampling | GAD-7 1 | 17.1% | 9 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lasheras, I.; Gracia-García, P.; Lipnicki, D.M.; Bueno-Notivol, J.; López-Antón, R.; de la Cámara, C.; Lobo, A.; Santabárbara, J. Prevalence of Anxiety in Medical Students during the COVID-19 Pandemic: A Rapid Systematic Review with Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6603. https://doi.org/10.3390/ijerph17186603
Lasheras I, Gracia-García P, Lipnicki DM, Bueno-Notivol J, López-Antón R, de la Cámara C, Lobo A, Santabárbara J. Prevalence of Anxiety in Medical Students during the COVID-19 Pandemic: A Rapid Systematic Review with Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(18):6603. https://doi.org/10.3390/ijerph17186603
Chicago/Turabian StyleLasheras, Isabel, Patricia Gracia-García, Darren M. Lipnicki, Juan Bueno-Notivol, Raúl López-Antón, Concepción de la Cámara, Antonio Lobo, and Javier Santabárbara. 2020. "Prevalence of Anxiety in Medical Students during the COVID-19 Pandemic: A Rapid Systematic Review with Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 18: 6603. https://doi.org/10.3390/ijerph17186603
APA StyleLasheras, I., Gracia-García, P., Lipnicki, D. M., Bueno-Notivol, J., López-Antón, R., de la Cámara, C., Lobo, A., & Santabárbara, J. (2020). Prevalence of Anxiety in Medical Students during the COVID-19 Pandemic: A Rapid Systematic Review with Meta-Analysis. International Journal of Environmental Research and Public Health, 17(18), 6603. https://doi.org/10.3390/ijerph17186603








