Does the Addition of Manual Therapy Approach to a Cervical Exercise Program Improve Clinical Outcomes for Patients with Chronic Neck Pain in Short- and Mid-Term? A Randomized Controlled Trial
Abstract
1. Introduction
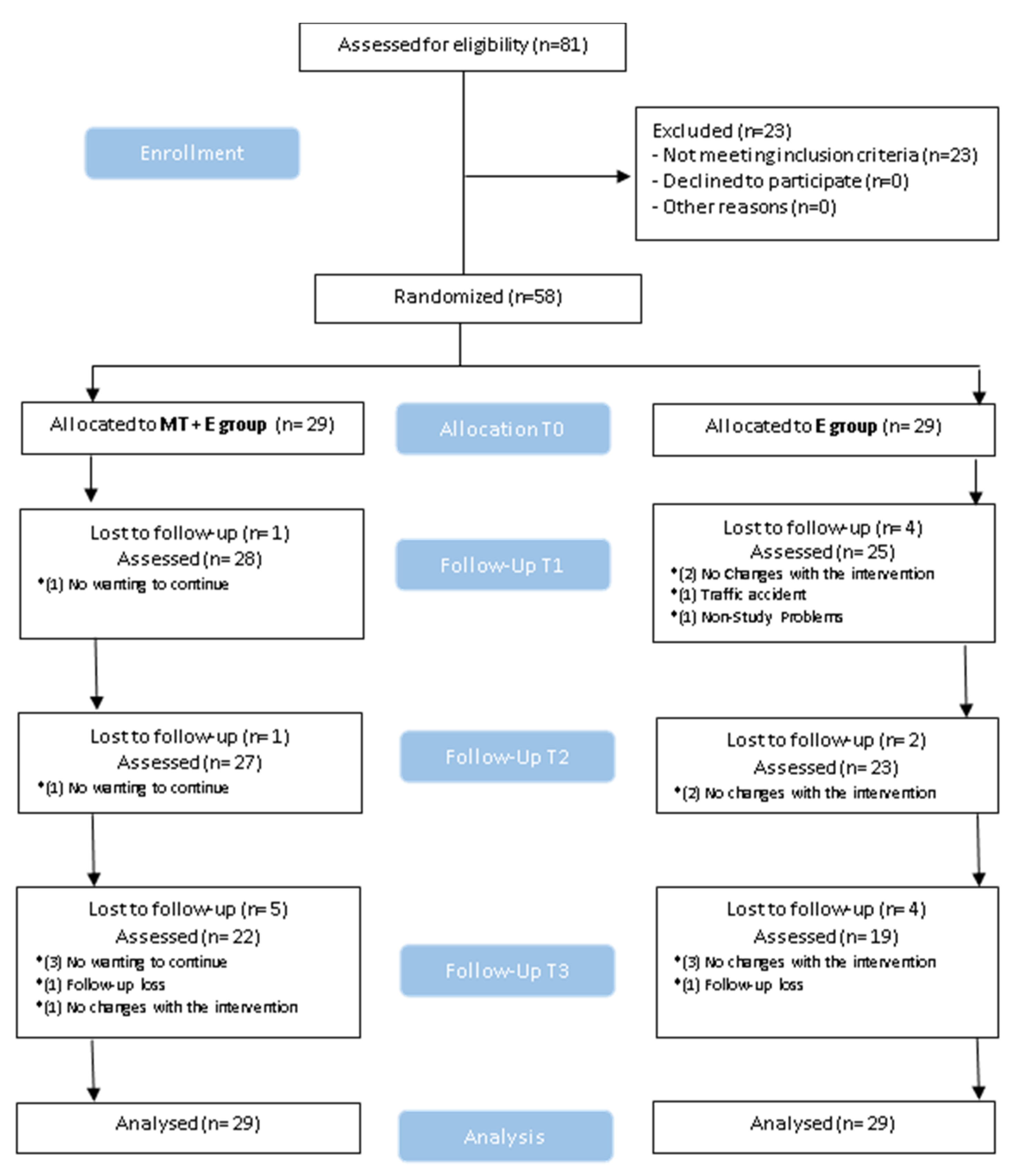
2. Methods
2.1. Study Design
2.2. Sample Size Calculation
2.3. Subjects
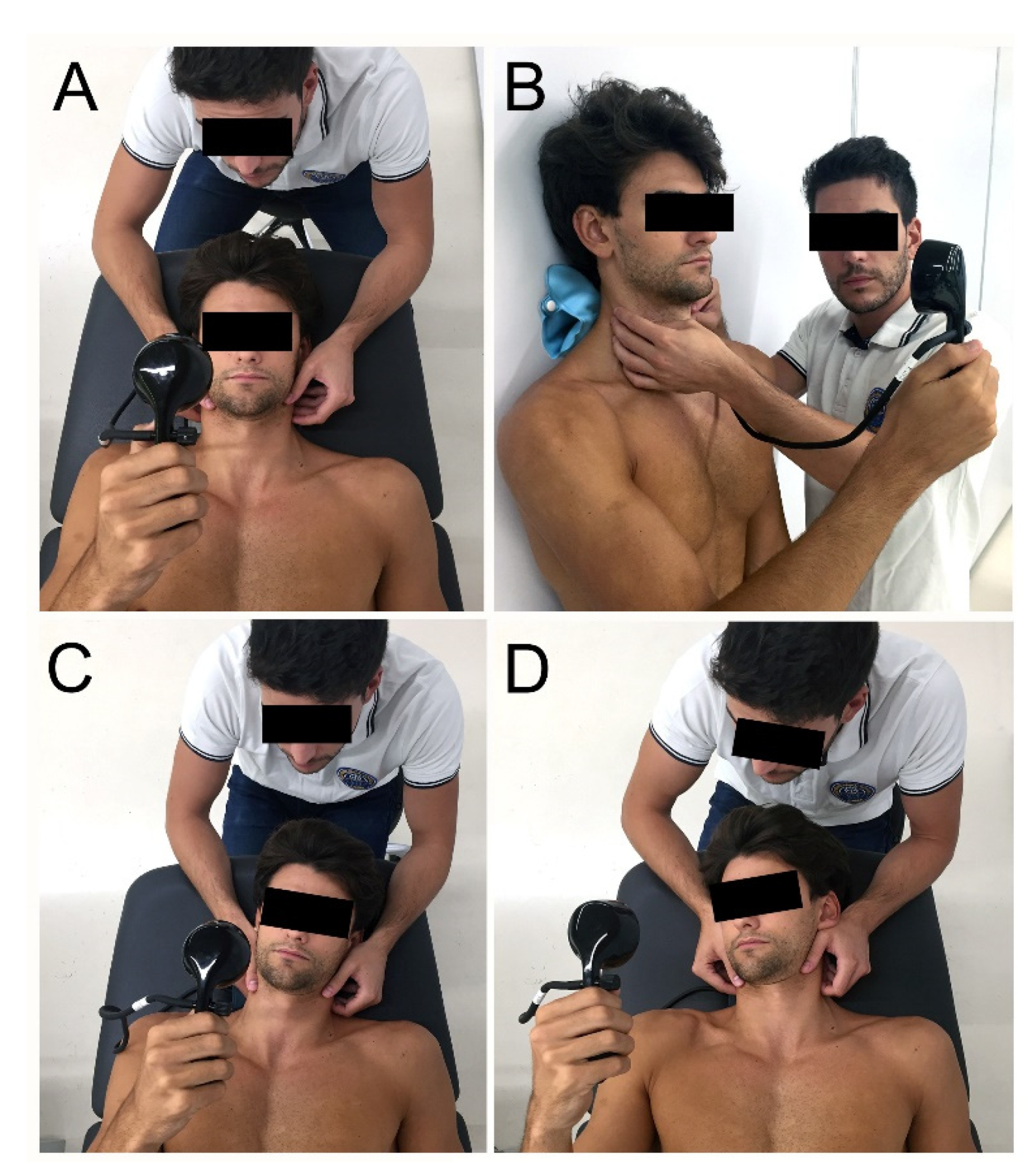
2.4. Measurements
2.5. Intervention
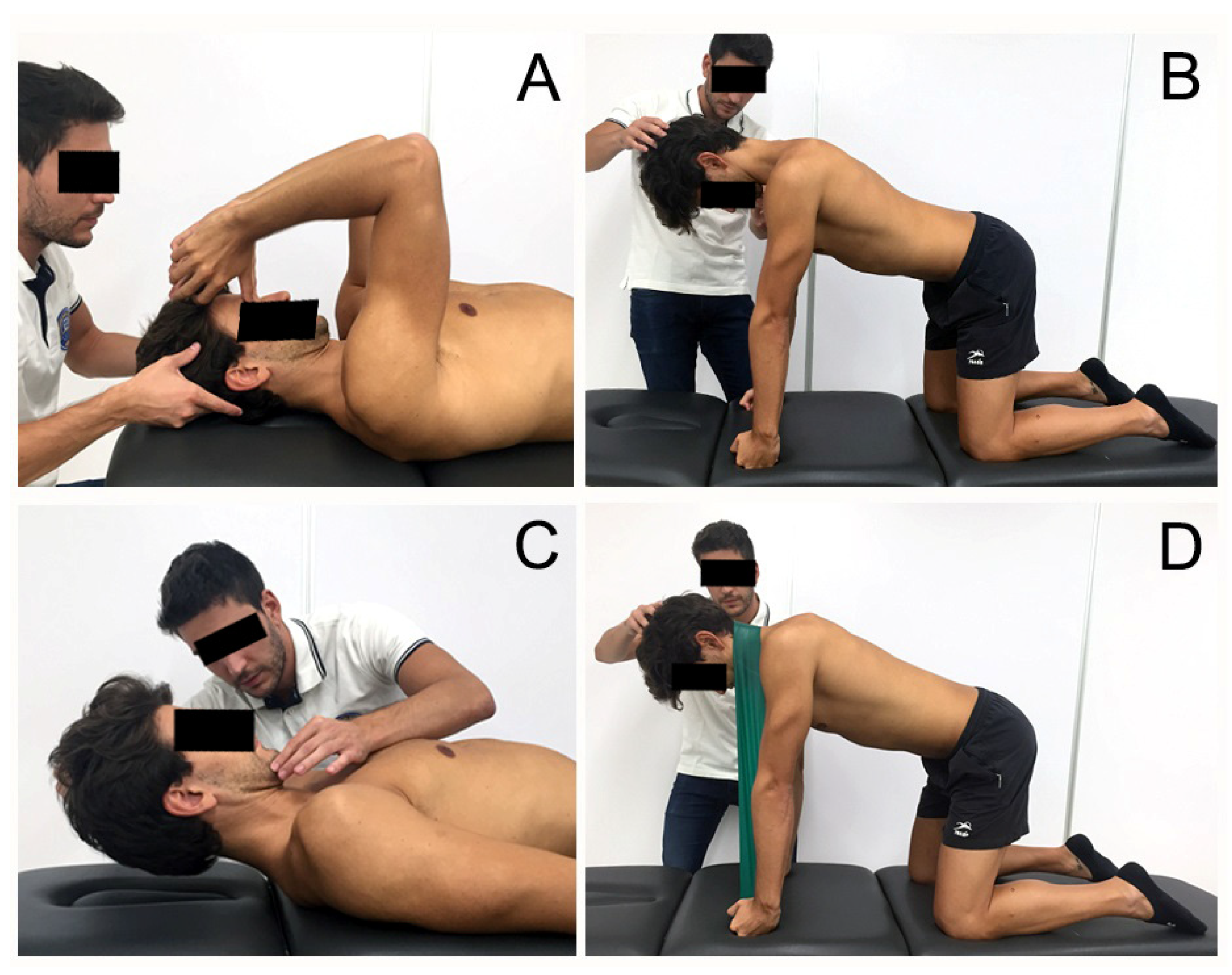
2.6. Exercise Group
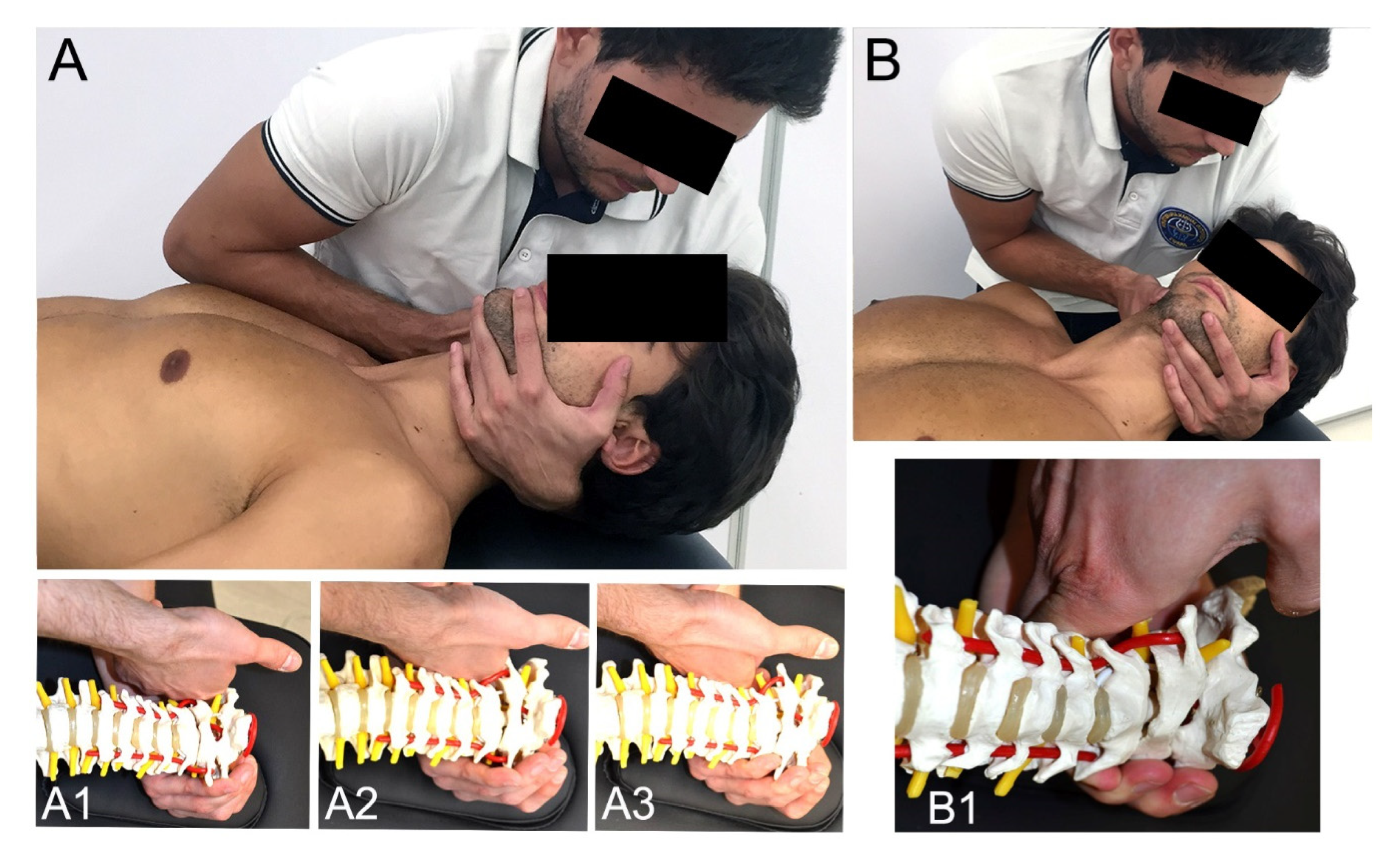
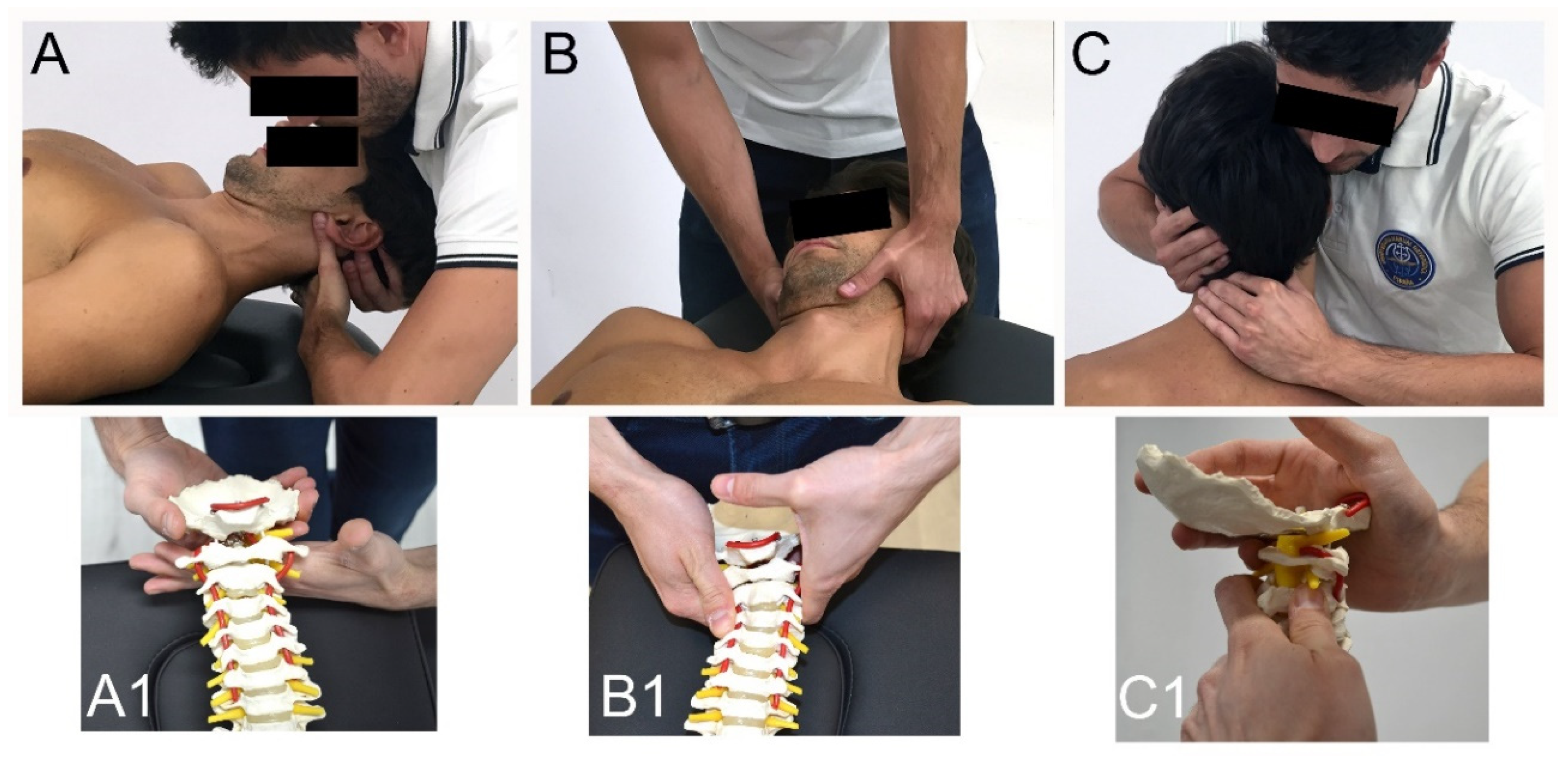
2.7. Manual Therapy + Exercise Group (MT + E)
2.8. Statistical Analysis
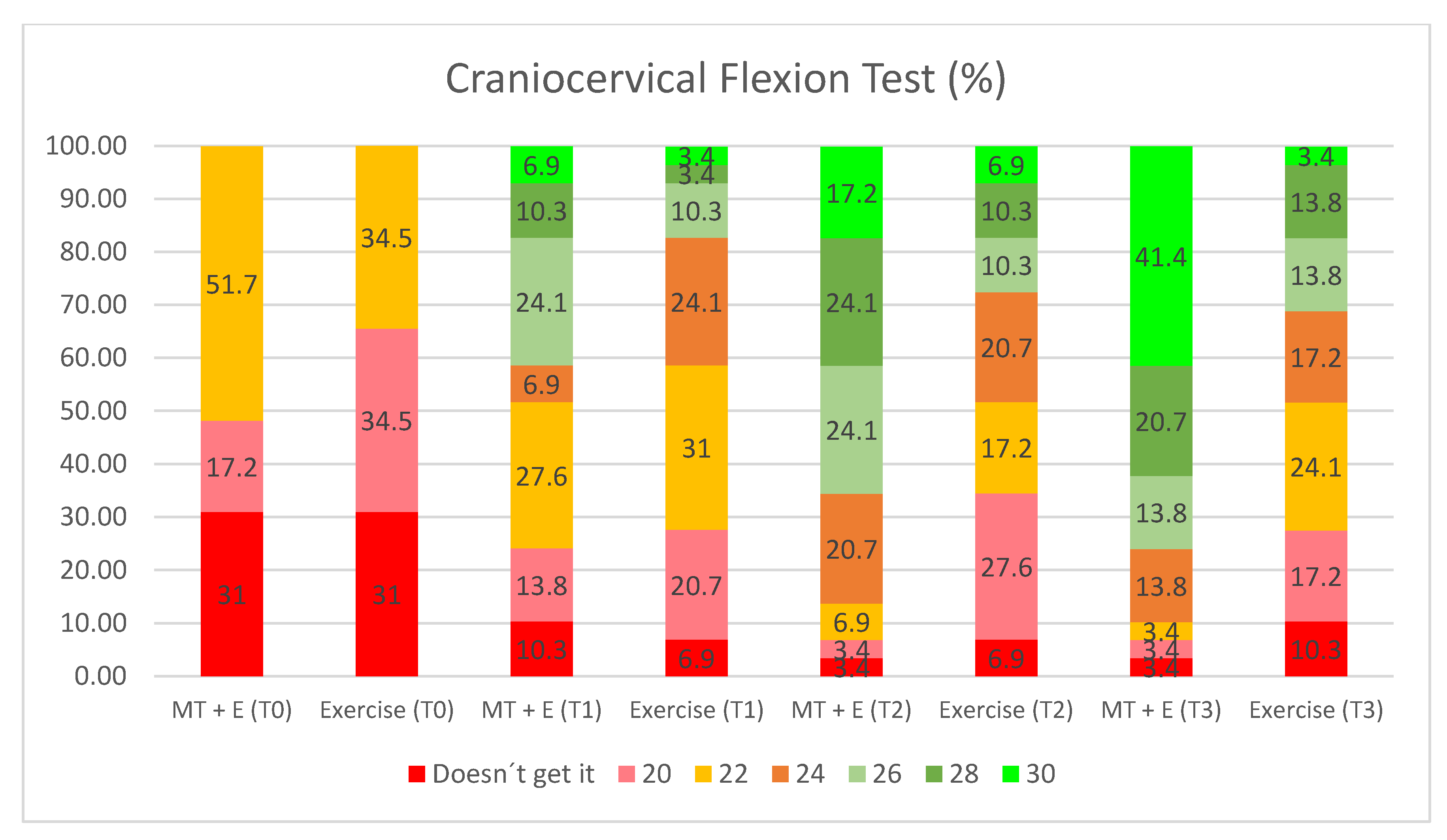
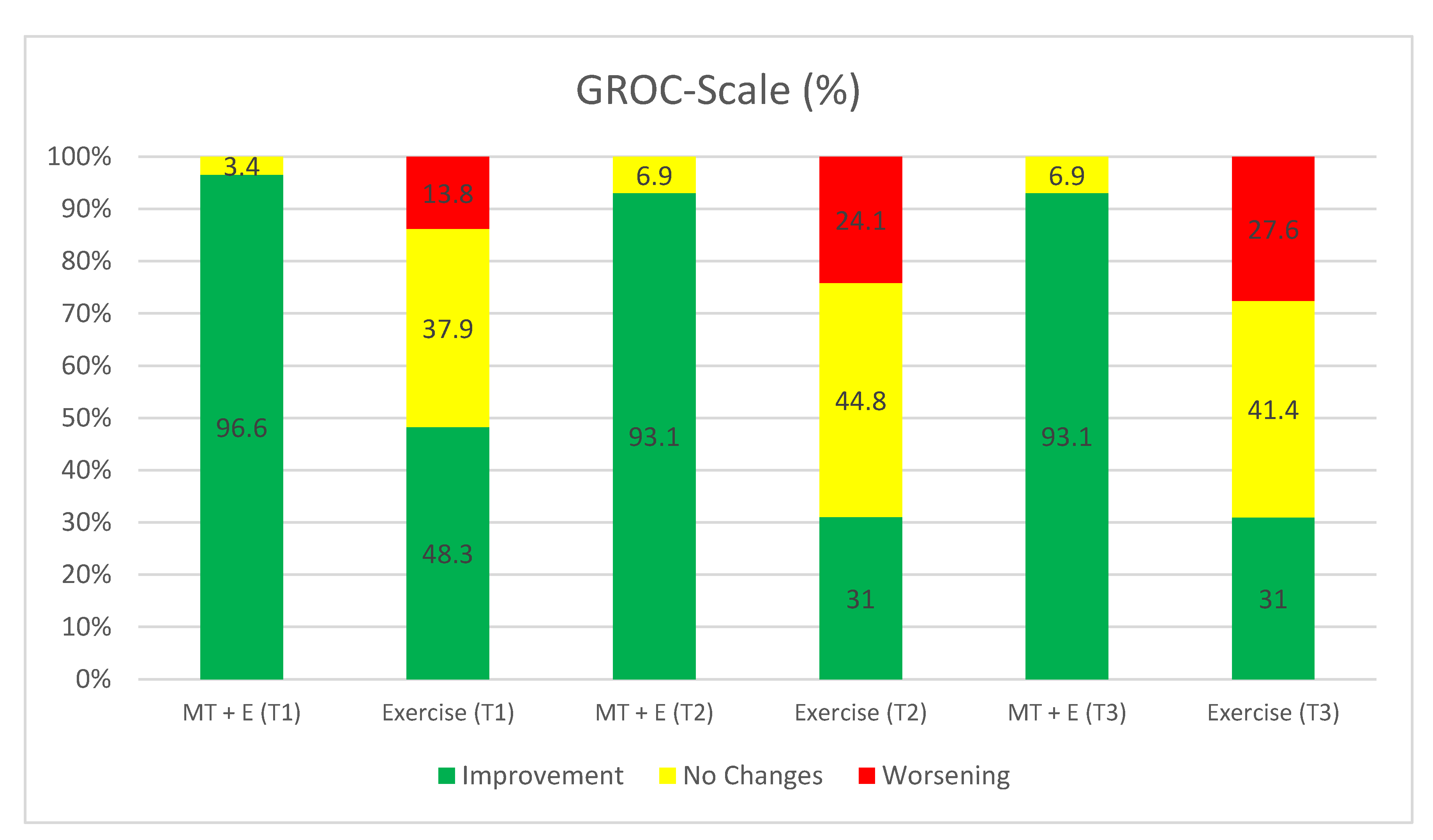
3. Results
3.1. End of the Intervention (T1)
3.2. 3-Month Follow Up (T2)
3.3. 6-Month Follow Up (T3)
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Availability
References
- Audette, I.; Dumas, J.-P.; Côté, J.N.; De Serres, S.J. Validity and between-day reliability of the Cervical Range of Motion (CROM) Device. J. Orthop. Sports Phys. Ther. 2010, 40, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sanz, J.; Carrasco, A.; Cabanillas-Barea, S.; Hidalgo-García, C.; Fanlo-Mazas, P.; Lucha-López, M.O.; Tricás-Moreno, J.M. Validity and reliability of two smartphone applications to measure the lower and upper cervical spine range of motion in subjects with chronic cervical pain. J. Back Musculoskelet. Rehabil. 2019, 32, 619–627. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-García, C.; Tricás-Moreno, J.M.; Lucha-López, O.; Miguel, E.E.; Bueno-Gracia, E.; Pérez-Guillén, S.; Fanlo-Mazas, P.; Ruiz-De-Escudero, A.; Krauss, J. Short term efficacy of C0-C1 mobilization in the cervical neutral position in upper cervical hypomobility: A randomized controlled trial. J. Int. Acad. Phys. Ther. Res. 2016, 7, 908–914. [Google Scholar] [CrossRef]
- Kay, T.M.; Gross, A.; Goldsmith, C.H.; Hoving, J.L.; Brønfort, G. Exercises for mechanical neck disorders. Cochrane Database Syst. Rev. 2005, CD004250. [Google Scholar] [CrossRef]
- Celenay, S.T.; Akbayrak, T.; Kaya, D.O. A comparison of the effects of stabilization exercises plus manual therapy to those of stabilization exercises alone in patients with nonspecific mechanical neck pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2016, 46, 44–55. [Google Scholar] [CrossRef]
- Blomgren, J.; Strandell, E.; Jull, G.; Vikman, I.; Roijezon, U. Effects of deep cervical flexor training on impaired physiological functions associated with chronic neck pain: A systematic review. BMC Musculoskelet. Disord. 2018, 19, 415. [Google Scholar] [CrossRef]
- Miller, J.; Gross, A.; D’Sylva, J.; Burnie, S.J.; Goldsmith, C.H.; Graham, N.; Haines, T.; Brønfort, G.; Hoving, J.L. Manual therapy and exercise for neck pain: A systematic review. Man. Ther. 2010, 15, 334–354. [Google Scholar] [CrossRef]
- Lluch, E.; Schomacher, J.; Gizzi, L.; Petzke, F.; Seegar, D.; Falla, D. Immediate effects of active cranio-cervical flexion exercise versus passive mobilisation of the upper cervical spine on pain and performance on the cranio-cervical flexion test. Man. Ther. 2014, 19, 25–31. [Google Scholar] [CrossRef]
- Aker, P.D.; Gross, A.R.; Goldsmith, C.H.; Peloso, P. Conservative management of mechanical neck pain: Systematic overview and meta-analysis. BMJ 1996, 313, 1291–1296. [Google Scholar] [CrossRef]
- Beltran-Alacreu, H.; López-De-Uralde-Villanueva, I.; Fernández-Carnero, J.; La Touche, R. Manual therapy, therapeutic patient education, and therapeutic exercise, an effective multimodal treatment of nonspecific chronic neck pain. Am. J. Phys. Med. Rehabil. 2015, 94, 887–897. [Google Scholar] [CrossRef]
- Dunning, J.R.; Cleland, J.A.; Waldrop, M.A.; Arnot, C.; Young, I.; Turner, M.; Sigurdsson, G. Upper cervical and upper thoracic thrust manipulation versus nonthrust mobilization in patients with mechanical neck pain: A multicenter randomized clinical trial. J. Orthop. Sports Phys. Ther. 2012, 42, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Pérez, H.I.; Perez, J.L.A.; Gil-Martínez, A.; La Touche, R.; Lara, S.L.; Gonzalez, N.C.; Perez, H.A.; Bishop, M.; Fernández-Carnero, J. Is one better than another? A randomized clinical trial of manual therapy for patients with chronic neck pain. Man. Ther. 2014, 19, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Hall, T.M.; Robinson, K. The flexion–rotation test and active cervical mobility—A comparative measurement study in cervicogenic headache. Man. Ther. 2004, 9, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Ogince, M.; Hall, T.; Robinson, K.; Blackmore, A.M. The diagnostic validity of the cervical flexion-rotation test in C1-C2 related cariogenic headache. Man Ther. 2007, 12, 256–269. [Google Scholar] [CrossRef]
- Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devanet, L.L.; Clewley, D.; Walton, D.; Sparks, C.; Robertson, E. Neck pain: Revision. Clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association. J. Orthop. Sport. Phys. Ther. 2016, 46, 1–67. [Google Scholar]
- Zito, G.; Jull, G.; Story, I. Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Man. Ther. 2006, 11, 118–129. [Google Scholar] [CrossRef]
- Kaltenborn, F. Manual Mobilization of the Joints. Volume II: The Spine; OMT España: Oslo, Norway, 2012. [Google Scholar]
- Bier, J.D.; Scholten-Peeters, G.G.; Staal, J.B.; Pool, J.; Van Tulder, M.W.; Beekman, E.; Knoop, J.; Meerhoff, G.; Verhagen, A.P. Clinical practice guideline for physical therapy assessment and treatment in patients with nonspecific neck pain. Phys. Ther. 2017, 98, 162–171. [Google Scholar] [CrossRef]
- Rushton, A.; Rivett, D.; Carlesso, L.; Flynn, T.; Hing, W.; Kerry, R. International framework for examination of the cervical region for potential of cervical arterial dysfunction prior to orthopaedic manual therapy intervention. Man. Ther. 2014, 19, 222–228. [Google Scholar] [CrossRef]
- Rueda, V.G.; López-De–Celis, C.; Barra-López, M.; Uribarren, A.C.; Tomás, S.C.; Hidalgo-García, C. Effectiveness of a specific manual approach to the suboccipital region in patients with chronic mechanical neck pain and rotation deficit in the upper cervical spine: Study protocol for a randomized controlled trial. BMC Musculoskelet. Disord. 2017, 18, 384. [Google Scholar] [CrossRef]
- Ortega, J.A.A.; Delgado-Martínez, A.D.; Ruiz, R.A. Validación de una versión española del Índice de Discapacidad Cervical. Med. Clínica 2008, 130, 85–89. [Google Scholar] [CrossRef]
- Mawdsley, R.H.; Moran, K.A.; Conniff, L.A. Reliability of two commonly used pain scales with elderly patients. J. Geriatr. Phys. Ther. 2002, 25, 16–20. [Google Scholar] [CrossRef]
- Malo-Urriés, M.; Tricás-Moreno, J.M.; Estébanez-De-Miguel, E.; Hidalgo-García, C.; Carrasco, A.; Cabanillas-Barea, S. Immediate effects of upper cervical translatoric mobilization on cervical mobility and pressure pain threshold in patients with cervicogenic headache: A randomized controlled trial. J. Manip. Physiol. Ther. 2017, 40, 649–658. [Google Scholar] [CrossRef] [PubMed]
- Hall, T.M.; Robinson, K.W.; Fujinawa, O.; Akasaka, K.; Pyne, E.A. Intertester reliability and diagnostic validity of the cervical flexion-rotation test. J. Manip. Physiol. Ther. 2008, 31, 293–300. [Google Scholar] [CrossRef]
- Hall, T.M.; Briffa, K.; Hopper, D.; Robinson, K. Long-term stability and minimal detectable change of the cervical flexion-rotation test. J. Orthop. Sports Phys. Ther. 2010, 40, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Takasaki, H.; Hall, T.M.; Oshiro, S.; Kaneko, S.; Ikemoto, Y.; Jull, G. Normal kinematics of the upper cervical spine during the flexion–rotation test—In Vivo measurements using magnetic resonance imaging. Man. Ther. 2011, 16, 167–171. [Google Scholar] [CrossRef]
- Strimpakos, N. The assessment of the cervical spine. Part 1: Range of motion and proprioception. J. Bodyw. Mov. Ther. 2011, 15, 114–124. [Google Scholar] [CrossRef]
- Jull, G.; O’Leary, S.; Falla, D. Clinical assessment of the deep cervical flexor muscles: The craniocervical flexion test. J. Manip. Physiol. Ther. 2008, 31, 525–533. [Google Scholar] [CrossRef]
- James, G.; Doe, T. The craniocervical flexion test: Intra-tester reliability in asymptomatic subjects. Physiother. Res. Int. 2010, 15, 144–149. [Google Scholar] [CrossRef]
- Fischer, A.A. Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain 1987, 30, 115–126. [Google Scholar] [CrossRef]
- Chesterton, L.S.; Sim, J.; Wright, C.C.; Foster, N.E. Inter-rater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin. J. Pain 2007, 23, 760–766. [Google Scholar] [CrossRef]
- Ayerbe-Gracia, J.; Sousa-Casasnovas, P. Outcome assessment in lumbar spine surgery: The patient’s perspective. Neurocirugía 2004, 15, 447–457. [Google Scholar] [CrossRef]
- Sullivan, M.D. The new subjective medicine: Taking the patient’s point of view on health care and health. Soc. Sci. Med. 2003, 56, 1595–1604. [Google Scholar] [CrossRef]
- Gross, A.; Paquin, J.; Dupont, G.; Blanchette, S.; LaLonde, P.; Cristie, T.; Graham, N.; Kay, T.; Burnie, S.; Gelley, G.; et al. Exercises for mechanical neck disorders: A Cochrane review update. Man. Ther. 2016, 24, 25–45. [Google Scholar] [CrossRef] [PubMed]
- Kamper, S.J.; Maher, C.G.; Mackay, G. Global rating of change scales: A review of strengths and weaknesses and considerations for design. J. Man. Manip. Ther. 2009, 17, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-las-Peñas, C.; Cleland, J.H.P. Síndromes Dolorosos en el Cuello y el Miembro Superior. Detección, Diagnóstico y Tratamiento Informados por la Evidencia; Elsevier: Churchill & Livingstone, UK, 2013. [Google Scholar]
- Jull, G.; Trott, P.; Potter, H.; Zito, G.; Niere, K.; Shirley, D.; Emberson, J.R.; Marschner, I.C.; Richardson, C. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine 2002, 27, 1835–1843. [Google Scholar] [CrossRef] [PubMed]
- Celenay, S.T.; Kaya, D.O.; Akbayrak, T. Cervical and scapulothoracic stabilization exercises with and without connective tissue massage for chronic mechanical neck pain: A prospective, randomised controlled trial. Man. Ther. 2016, 21, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Hansen, I.R.; Søgaard, K.; Christensen, R.; Thomsen, B.; Manniche, C.; Juul-Kristensen, B. Neck exercises, physical and cognitive behavioural-graded activity as a treatment for adult whiplash patients with chronic neck pain: Design of a randomised controlled trial. BMC Musculoskelet. Disord. 2011, 12, 274. [Google Scholar] [CrossRef]
- Falla, D.; Lindstrøm, R.; Rechter, L.; Boudreau, S.; Petzke, F. Effectiveness of an 8-week exercise programme on pain and specificity of neck muscle activity in patients with chronic neck pain: A randomized controlled study. Eur. J. Pain 2013, 17, 1517–1528. [Google Scholar] [CrossRef] [PubMed]
- Gallego-Izquierdo, T.; Pecos-Martín, D.; Girbés, E.L.; Plaza-Manzano, G.; Caldentey, R.; Melãos, R.; Mariscal, D.; Falla, D. Comparison of cranio-cervical flexion training versus cervical proprioception training in patients with chronic neck pain: A randomized controlled clinical trial. J. Rehabil. Med. 2016, 48, 48–55. [Google Scholar] [CrossRef]
- Kaltenborn, F. Fisioterapia Manual. Volumen III: Manipulación-Tracción de las Extremidades y la Columna; OMT España: Zaragoza, Spain, 2009. [Google Scholar]
- Krauss, J.; Evjenth, O.C. Manipulación Vertebral Translatoria; OMT España: Zaragoza, Spain, 2009. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Treleaven, J.; Peterson, G.; Ludvigsson, M.L.; Kammerlind, A.-S.; Peolsson, A. Balance, dizziness and proprioception in patients with chronic whiplash associated disorders complaining of dizziness: A prospective randomized study comparing three exercise programs. Man. Ther. 2016, 22, 122–130. [Google Scholar] [CrossRef]
- Cho, J.; Lee, E.; Lee, S. Upper thoracic spine mobilization and mobility exercise versus upper cervical spine mobilization and stabilization exercise in individuals with forward head posture: A randomized clinical trial. BMC Musculoskelet. Disord. 2017, 18, 525. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.C.; Walton, D.M.; Avery, S.; Blanchard, A.; Etruw, E.; McAlpine, C.; Goldsmith, C.H. Measurement properties of the neck disability index: A systematic review. J. Orthop. Sports Phys. Ther. 2009, 39, 400–C12. [Google Scholar] [CrossRef] [PubMed]
- Llach, X.B.; Tudela, L.L. Reflexiones sobre la investigación de resultados en salud. Atención Primaria 2002, 30, 388–391. [Google Scholar] [CrossRef][Green Version]
- Higginson, I.J.; Carr, A.J. Measuring quality of life: Using quality of life measures in the clinical setting. BMJ 2001, 322, 1297–1300. [Google Scholar] [CrossRef] [PubMed]
- Donabedian, A. The end results of health care: Ernest codman’s contribution to quality assessment and beyond. Milbank Q. 1989, 67, 233. [Google Scholar] [CrossRef] [PubMed]
- González Rueda, V. Efectividad del Abordaje Específico de la Región Suboccipital en Pacientes con Cervicalgia Mecánica Crónica con Déficit de Rotación Cervical Superior; Universidad de Zaragoza: Zaragoza, Spain, 2018. [Google Scholar]
- Carrasco-Uribarren, A. Efectividad de un Protocolo de Manipulación Tracción en Posición de Reposo de la Columna Cervical Superior en Pacientes con Mareo Cervicogénico; Universidad de Zaragoza: Zaragoza, Spain, 2018. [Google Scholar]
- Walker, M.J.; Boyles, R.E.; Young, B.A.; Strunce, J.B.; Garber, M.B.; Whitman, J.M.; Deyle, G.; Wainner, R.S. The effectiveness of manual physical therapy and exercise for mechanical neck pain. Spine 2008, 33, 2371–2378. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-García, C.; Cabanillas-Barea, S.; Malo-Urriés, M.; Fanlo-Mazas, P.; Jiménez-Del-Barrio, S.; Uribarren, A.C. Estudio descriptivo de la relación entre la inclinación cervical y rotación cervical superior en sujetos con hipomovilidad cervical superior. Cuest. Fisioter. Rev. Univ. Inf. Investig. Fisioter. 2015, 44, 143–150. [Google Scholar]
- Kim, D.-H.; Kim, S.-Y. Comparison of immediate effects of sling-based manual therapy on specific spine levels in subjects with neck pain and forward head posture: A randomized clinical trial. Disabil. Rehabil. 2019, 1–8, 1–8. [Google Scholar] [CrossRef]
- Galindez-Ibarbengoetxea, X.; Chourraut, I.S.; Ramírez-Vélez, R.; Andersen, L.L.; González-Izal, M.; Crespo, A.J.; Crespo, M.I. Immediate effects of osteopathic treatment versus therapeutic exercise on patients with chronic cervical pain. Altern. Ther. Heal. Med. 2017, 24, 24–32. [Google Scholar]
- Beer, A.; Treleaven, J.; Jull, G. Can a functional postural exercise improve performance in the cranio-cervical flexion test? A preliminary study. Man. Ther. 2012, 17, 219–224. [Google Scholar] [CrossRef]
- Falla, D.; Campbell, C.D.; Fagan, A.E.; Thompson, D.C.; Jull, G. Relationship between cranio-cervical flexion range of motion and pressure change during the cranio-cervical flexion test. Man. Ther. 2003, 8, 92–96. [Google Scholar] [CrossRef]
- De Jesus-Moraleida, F.R.; Ferreira, P.H.; Pereira, L.S.; Vasconcelos, C.M.; Ferreira, M.L. Ultrasonographic analysis of the neck flexor muscles in patients with chronic neck pain and changes after cervical spine mobilization. J. Manip. Physiol. Ther. 2011, 34, 514–524. [Google Scholar] [CrossRef] [PubMed]
- Farooq, M.N.; Mohseni-Bandpei, M.A.; Gilani, S.A.; Ashfaq, M.; Mahmood, Q. The effects of neck mobilization in patients with chronic neck pain: A randomized controlled trial. J. Bodyw. Mov. Ther. 2018, 22, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Choi, J.-H.; Lee, K.-W. Immediate effects of active stretching versus passive mobilization of the upper cervical spine on patients with neck pain and ROM. J. Korean Soc. Phys. Med. 2016, 11, 27–32. [Google Scholar] [CrossRef]
- River, Y.; Levital, T.; Belgrade, M. Computerized mobilization of the cervical spine for the treatment of chronic neck pain. Clin. J. Pain 2012, 28, 790–796. [Google Scholar] [CrossRef]
- Wright, A. Hypoalgesia post-manipulative therapy: A review of a potential neurophysiological mechanism. Man. Ther. 1995, 1, 11–16. [Google Scholar] [CrossRef]
- Grant, R.; Exelby, L. Physical therapy of the cervical and thoracic spine (clinics in physical therapy). Physiotherapy 1994, 80, 870. [Google Scholar] [CrossRef]
- Vicenzino, B.; Collins, D.; Wright, A. The initial effects of a cervical spine manipulative physiotherapy treatment on the pain and dysfunction of lateral epicondylalgia. Pain 1996, 68, 69–74. [Google Scholar] [CrossRef]
- Pickar, J.G. Neurophysiological effects of spinal manipulation. Spine J. 2002, 2, 357–371. [Google Scholar] [CrossRef]
- Haas, M.; Groupp, E.; Panzer, D.; Partna, L.; Lumsden, S.; Aickin, M. Efficacy of cervical endplay assessment as an indicator for spinal manipulation. Spine 2003, 28, 1091–1096. [Google Scholar] [CrossRef]
- Vicenzino, B.; Paungmali, A.; Buratowski, S.; Wright, A. Specific manipulative therapy treatment for chronic lateral epicondylalgia produces uniquely characteristic hypoalgesia. Man. Ther. 2001, 6, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Skyba, A.D.; Radhakrishnan, R.; Rohlwing, J.J.; Wright, A.; Sluka, A.K.; Skyba, D.; Sluka, K. Joint manipulation reduces hyperalgesia by activation of monoamine receptors but not opioid or GABA receptors in the spinal cord. Pain 2003, 106, 159–168. [Google Scholar] [CrossRef]
- Oliva-Pascual-Vaca, Á.; González-González, C.; Oliva-Pascual-Vaca, J.; Piña-Pozo, F.; Ferragut-Garcías, A.; Fernández-Domínguez, J.C.; Heredia-Rizo, A.M. Visceral Origin: An Underestimated Source of Neck Pain. A Systematic Scoping Review. Diagnostics 2019, 9, 186. [Google Scholar] [CrossRef] [PubMed]
| Clinical Features | E Group (n = 29) | MT + E Group (n = 29) |
|---|---|---|
| Age (years) | 49.72 ± 17.56 | 48.76 ± 14.53 |
| Sex | 7 M; 22 F | 10 M; 19 F |
| Duration of Symptoms (months) | 124.38 ± 148.17 | 96.97 ± 96.73 |
| Visual Analogue Scale (centimeters) | 3.76 ± 2.53 | 3.36 ± 1.97 |
| Upper Cervical Flexion (°) | 10.59 ± 4.39 | 11.45 ± 4.24 |
| Neck Disability Index | 15.24 ± 6.99 | 12.55 ± 6.25 |
| Doesn’t get it | 51.70% | 34.50% |
| 20 mmHg | 17.20% | 34.50% |
| 22 mmHg | 31% | 31% |
| Flexion-rotation test (°) | ||
| (+) | 12.80 ± 6.04 | 17.26 ± 7.90 |
| (-) | 22.91 ± 10.52 | 27.12 ± 9.19 |
| Pressure Pain Threshold (kPa) | ||
| First MCJ (R) | 359.14 ± 175.98 | 395.93 ± 195.23 |
| C2-3 (R) | 173.76 ± 87.92 | 208.69 ± 114.53 |
| Suboccipital (R) | 186.10 ± 75.34 | 211.45 ± 91.57 |
| First MCJ (L) | 364.34 ± 155.47 | 339.90 ± 184.74 |
| C2-3 (L) | 174.59 ± 90.02 | 206.38 ± 113.72 |
| Suboccipital (L) | 180.59 ± 79.85 | 207.90 ± 105.33 |
| Group | Variable | T0 | T1 | T2 | T3 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 1 Month | Difference between Baseline | 3 Months | Difference between Baseline | 6 Months | Difference between Baseline | |||||||||||
| Mean ± SD | Mean ± SD | Mean ± SD | F | p-ValueRA | d | Mean ± SD | Mean ± SD | F | p-ValueRA | d | Mean ± SD | Mean ± SD | F | p-ValueRA | d | ||
| Exercise Group | Visual Analogue Scale (centimeters) | 3.76 ± 2.53 | 2.89 ± 2.44 | −0.87 ± 0.09 | 2.89 | >0.661 | 0.35 | 3.87 ± 2.71 | 0.11 ± 0.18 | 2.89 | >1.000 | 0.04 | 3.91 ± 2.84 | 0.15 ± 0.31 | 2.89 | >1.000 | 0.06 |
| Upper Cervical Flexion (°) | 10.59 ± 4.39 | 10.59 ± 5.21 | 0.00 ± 0.82 | 2.57 | >1.000 | 0.00 | 9.03 ± 5.27 | −1.56 ± 0.88 | 2.57 | >0.406 | 0.32 | 8.93 ± 4.76 | −1.66 ± 0.37 | 2.57 | >0.177 | 0.36 | |
| Neck Disability Index | 15.24 ± 6.99 | 11.03 ± 6.74 | −4.21 ± 0.25 | 6.39 | <0.001 | 0.61 | 12.83 ± 8.09 | −2.41 ± 1.10 | 6.39 | >0.116 | 0.32 | 13.10 ± 8.58 | −2.14 ± 1.59 | 6.39 | >0.420 | 0.27 | |
| Flexion-rotation test + (°) | 12.80 ± 6.04 | 15.48 ± 10.34 | 2.68 ± 4.30 | 2.27 | >0.489 | 0.32 | 12.76 ± 7.77 | −0.04 ± 1.73 | 2.27 | >1.000 | 0.01 | 12.83 ± 9.10 | 0.03 ± 3.06 | 2.27 | >1.000 | 0.00 | |
| Flexion-rotation test-(°) | 22.91 ± 10.52 | 23.59 ± 11.21 | 0.68 ± 0.69 | 8.52 | >1.000 | 0.06 | 17.21 ± 8.54 | −5.70 ± 1.98 | 8.52 | <0.002 | 0.60 | 18.03 ± 10.42 | −4.88 ± 0.10 | 8.52 | <0.024 | 0.47 | |
| Pressure Pain Threshold (kpa) | |||||||||||||||||
| First MCJ (R) | 359.14 ± 175.98 | 351.24 ± 168.84 | −7.90 ± 7.14 | 2.24 | >1.000 | 0.05 | 310.21 ± 133.37 | −48.93 ± 42.61 | 2.24 | >0.145 | 0.31 | 304.66 ± 121.12 | −54.48 ± 54.86 | 2.24 | >0.198 | 0.36 | |
| C2-3 (R) | 173.76 ± 87.92 | 166.48 ± 78.91 | −7.28 ± 9.01 | 2.06 | >1.000 | 0.09 | 149.76 ± 77.08 | −24.00 ± 10.84 | 2.06 | >0.542 | 0.29 | 145.93 ± 65.41 | −27.83 ± 22.51 | 2.06 | >0.258 | 0.36 | |
| Suboccipital (R) | 186.10 ± 75.34 | 180.79 ± 81.65 | −5.31 ± 6.31 | 0.97 | >1.000 | 0.07 | 161.59 ± 79.99 | −24.51 ± 4.65 | 0.97 | >0.722 | 0.32 | 163.97 ± 76.99 | −22.13 ± 1.65 | 0.97 | >0.943 | 0.29 | |
| First MCJ (L) | 364.34 ± 155.47 | 343.45 ± 177.71 | −20.89 ± 22.24 | 1.35 | >1.000 | 0.13 | 339.93 ± 171.41 | −24.41 ± 15.94 | 1.35 | >1.000 | 0.15 | 323.41 ± 148.53 | −40.93 ± 6.94 | 1.35 | >0.289 | 0.27 | |
| C2-3 (L) | 174.59 ± 90.02 | 185.90 ± 80.34 | 11.31 ± 9.68 | 1.91 | >1.000 | 0.13 | 159.97 ± 80.15 | −14.62 ± 9.87 | 1.91 | >1.000 | 0.17 | 168.76 ± 76.65 | −5.83 ± 13.37 | 1.91 | >1.000 | 0.07 | |
| Suboccipital (L) | 180.59 ± 79.85 | 196.90 ± 79.97 | 16.31 ± 0.08 | 0.61 | >1.000 | 0.20 | 181.90 ± 67.35 | 1.31 ± 12.50 | 0.61 | >1.000 | 0.02 | 182.45 ± 65.61 | 1.86 ± 14.24 | 0.61 | >1.000 | 0.03 | |
| Manual Therapy + Exercise Group | Visual Analogue Scale (centimeters) | 3.36 ± 1.97 | 0.75 ± 1.42 | −2.61 ± 0.55 | 13.91 | <0.001 | 1.52 | 0.80 ± 1.30 | −2.56 ± 1.42 | 13.91 | <0.001 | 1.53 | 0.98 ± 1.49 | −2.38 ± 0.48 | 13.91 | <0.001 | 1.36 |
| Upper Cervical Flexion (°) | 11.45 ± 4.24 | 13.55 ± 4.13 | 2.10 ± 0.11 | 10.84 | >0.074 | 0.50 | 14.83 ± 4.63 | 3.38 ± 0.39 | 10.84 | <0.022 | 0.76 | 16.90 ± 4.83 | 5.45 ± 0.59 | 10.84 | <0.001 | 1.20 | |
| Neck Disability Index | 12.55 ± 6.25 | 5.45 ± 5.53 | −7.10 ± 0.72 | 19.26 | <0.001 | 1.20 | 4.66 ± 5.62 | −7.89 ± 0.63 | 19.26 | <0.001 | 1.33 | 4.76 ± 5.96 | −7.79 ± 0.29 | 19.26 | <0.001 | 1.28 | |
| Flexion-rotation test + (°) | 17.26 ± 7.90 | 37.79 ± 10.48 | 20.53 ± 2.58 | 42.51 | <0.001 | 2.21 | 35.83 ± 9.61 | 18.57 ± 1.71 | 42.51 | <0.001 | 2.25 | 34.48 ± 12.04 | 17.22 ± 4.14 | 42.51 | <0.001 | 1.69 | |
| Flexion-rotation test-(°) | 27.12 ± 9.19 | 41.97 ± 9.47 | 14.85 ± 0.28 | 31.50 | <0.001 | 1.59 | 40.07 ± 8.16 | 12.95 ± 1.03 | 31.50 | <0.001 | 1.49 | 38.66 ± 9.42 | 11.54 ± 0.23 | 31.50 | <0.001 | 1.24 | |
| Pressure Pain Threshold (Kpa) | |||||||||||||||||
| First MCJ (R) | 395.93 ± 195.23 | 417.14 ± 194.94 | 21.21 ± 0.29 | 3.72 | >1.000 | 0.11 | 431.00 ± 193.54 | 35.07 ± 1.69 | 3.72 | >1.000 | 0.18 | 479.00 ± 214.95 | 83.07 ± 19.72 | 3.72 | >0.182 | 0.41 | |
| C2-3 (R) | 208.69 ± 114.53 | 250.83 ± 113.26 | 42.14 ± 1.27 | 4.56 | >0.108 | 0.33 | 277.86 ± 135.35 | 19.17 ± 20.82 | 4.56 | <0.016 | 0.49 | 305.83 ± 162.70 | 97.14 ± 48.17 | 4.56 | <0.004 | 0.69 | |
| Suboccipital (R) | 211.45 ± 91.57 | 257.55 ± 112.31 | 46.10 ± 20.74 | 10.35 | <0.016 | 0.45 | 297.72 ± 117.74 | 86.27 ± 26.17 | 10.35 | <0.001 | 0.82 | 344.48 ± 171.01 | 133.03 ± 79.44 | 10.35 | <0.001 | 0.97 | |
| First MCJ (L) | 339.90 ± 184.74 | 397.97 ± 172.87 | 58.07 ± 11.87 | 6.12 | >0.387 | 0.33 | 421.72 ± 178.22 | 81.82 ± 6.52 | 6.12 | >0.120 | 0.45 | 483.52 ± 198.00 | 143.62 ± 13.26 | 6.12 | <0.003 | 0.75 | |
| C2-3 (L) | 206.38 ± 113.72 | 279.76 ± 167.66 | 73.38 ± 53.94 | 10.19 | <0.004 | 0.51 | 298.14 ± 161.58 | 91.76 ± 47.86 | 10.19 | <0.001 | 0.66 | 332.52 ± 166.91 | 126.14 ± 53.19 | 10.19 | <0.001 | 0.88 | |
| Suboccipital (L) | 207.90 ± 105.33 | 267.00 ± 116.26 | 59.10 ± 10.93 | 15.22 | <0.002 | 0.53 | 314.14 ± 155.73 | 106.24 ± 50.40 | 15.22 | <0.001 | 0.80 | 380.66 ± 198.09 | 172.76 ± 92.76 | 15.22 | <0.001 | 1.09 | |
| Variable | Group | T0 | T1 | T2 | T3 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 1 Month | Difference between Groups | 3 Months | Difference between Groups | 6 Months | Difference between Groups | |||||||||||
| Mean ± SD | Mean ± SD | Mean ± SD | F | p-Value OA | d | Mean ± SD | Mean ± SD | F | p-Value OA | d | Mean ± SD | Mean ± SD | F | p-Value OA | d | ||
| Visual Analogue Scale (centimeters) | E Group | 3.76 ± 2.53 | 2.89 ± 2.44 | 2.14 ± 1.02 | 6.23 | <0.016 | 0.78 | 3.87 ± 2.71 | 3.07 ± 1.41 | 15.50 | <0.001 | 1.44 | 3.91 ± 2.84 | 2.93 ± 1.35 | 14.73 | <0.001 | 1.29 |
| MT + E Group | 3.36 ± 1.97 | 0.75 ± 1.42 | 0.80 ± 1.30 | 0.98 ± 1.49 | |||||||||||||
| Upper Cervical Flexion (°) | E Group | 10.59 ± 4.39 | 10.59 ± 5.21 | 2.96 ± 1.08 | 3.74 | >0.058 | 0.63 | 9.03 ± 5.27 | 5.80 ± 0.64 | 13.47 | <0.001 | 1.17 | 8.93 ± 4.76 | 7.97 ± 0.07 | 36.33 | <0.001 | 1.66 |
| MT + E Group | 11.45 ± 4.24 | 13.55 ± 4.13 | 14.83 ± 4.63 | 16.90 ± 4.83 | |||||||||||||
| Neck Disability Index | E Group | 15.24 ± 6.99 | 11.03 ± 6.74 | 5.58 ± 1.21 | 4.35 | <0.042 | 0.74 | 12.83 ± 8.09 | 8.17 ± 2.47 | 14.78 | <0.001 | 1.17 | 13.10 ± 8.58 | 8.34 ± 2.62 | 12.21 | <0.001 | 1.13 |
| MT + E Group | 12.55 ± 6.25 | 5.45 ± 5.53 | 4.66 ± 5.62 | 4.76 ± 5.96 | |||||||||||||
| Flexion-rotation test + (°) | E Group | 12.80 ± 6.04 | 15.48 ± 10.34 | 22.31 ± 0.14 | 53.47 | <0.001 | 2.14 | 12.76 ± 7.77 | 23.07 ± 1.84 | 78.84 | <0.001 | 2.64 | 12.83 ± 9.10 | 21.65 ± 2.94 | 45.55 | <0.001 | 2.03 |
| MT + E Group | 17.26 ± 7.90 | 37.79 ± 10.48 | 35.83 ± 9.61 | 34.48 ± 12.04 | |||||||||||||
| Flexion-rotation test-(°) | E Group | 22.91 ± 10.52 | 23.59 ± 11.21 | 18.38 ± 1.74 | 44.37 | <0.001 | 1.77 | 17.21 ± 8.54 | 22.86 ± 0.38 | 70.91 | <0.001 | 2.74 | 18.03 ± 10.42 | 20.63 ± 1.00 | 59.36 | <0.001 | 2.08 |
| MT + E Group | 27.12 ± 9.19 | 41.97 ± 9.47 | 40.07 ± 8.16 | 38.66 ± 9.42 | |||||||||||||
| Pressure Pain Threshold (Kpa) | |||||||||||||||||
| First MCJ (R) | E Group | 359.14 ± 175.98 | 351.24 ± 168.84 | 65.90 ± 26.10 | 0.53 | >0.471 | 0.36 | 310.21 ± 133.37 | 120.79 ± 60.17 | 4.14 | <0.047 | 0.73 | 304.66 ± 121.12 | 174.34 ± 93.83 | 9.88 | <0.003 | 1.00 |
| MT + E Group | 395.93 ± 195.23 | 417.14 ± 194.94 | 431.00 ± 193.54 | 479.00 ± 214.95 | |||||||||||||
| C2-3 (R) | E Group | 173.76 ± 87.92 | 166.48 ± 78.91 | 84.35 ± 34.35 | 5.74 | <0.020 | 0.86 | 149.76 ± 77.08 | 128.10 ± 58.27 | 13.89 | <0.001 | 1.16 | 145.93 ± 65.41 | 159.90 ± 97.29 | 19.01 | <0.001 | 1.29 |
| MT + E Group | 208.69 ± 114.53 | 250.83 ± 113.26 | 277.86 ± 135.35 | 305.83 ± 162.70 | |||||||||||||
| Suboccipital (R) | E Group | 186.10 ± 75.34 | 180.79 ± 81.65 | 76.76 ± 30.66 | 7.35 | <0.009 | 0.78 | 161.59 ± 79.99 | 136.13 ± 37.15 | 25.37 | <0.001 | 1.35 | 163.97 ± 76.99 | 180.51 ± 94.02 | 28.23 | <0.001 | 1.36 |
| MT + E Group | 211.45 ± 91.57 | 257.55 ± 112.31 | 297.72 ± 117.74 | 344.48 ± 171.01 | |||||||||||||
| First MCJ (L) | E Group | 364.34 ± 155.47 | 343.45 ± 177.71 | 54.52 ± 4.84 | 4.10 | <0.048 | 0.31 | 339.93 ± 171.41 | 81.79 ± 6.81 | 7.15 | <0.010 | 0.47 | 323.41 ± 148.53 | 160.11 ± 49.47 | 20.24 | <0.001 | 0.92 |
| MT + E Group | 339.90 ± 184.74 | 397.97 ± 172.87 | 421.72 ± 178.22 | 483.52 ± 198.00 | |||||||||||||
| C2-3 (L) | E Group | 174.59 ± 90.02 | 185.90 ± 80.34 | 93.86 ± 87.32 | 7.47 | <0.008 | 0.71 | 159.97 ± 80.15 | 138.17 ± 81.43 | 20.91 | <0.001 | 1.08 | 168.76 ± 76.65 | 163.76 ± 90.26 | 26.36 | <0.001 | 1.26 |
| MT + E Group | 206.38 ± 113.72 | 279.76 ± 167.66 | 298.14 ± 161.58 | 332.52 ± 166.91 | |||||||||||||
| Suboccipital (L) | E Group | 180.59 ± 79.85 | 196.90 ± 79.97 | 70.10 ± 36.29 | 4.64 | <0.036 | 0.70 | 181.90 ± 67.35 | 132.24 ± 88.35 | 16.92 | <0.001 | 1.10 | 182.45 ± 65.61 | 198.21 ± 132.48 | 28.06 | <0.001 | 1.34 |
| MT + E Group | 207.90 ± 105.33 | 267.00 ± 116.26 | 314.14 ± 155.73 | 380.66 ± 198.09 | |||||||||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Sanz, J.; Malo-Urriés, M.; Corral-de-Toro, J.; López-de-Celis, C.; Lucha-López, M.O.; Tricás-Moreno, J.M.; Lorente, A.I.; Hidalgo-García, C. Does the Addition of Manual Therapy Approach to a Cervical Exercise Program Improve Clinical Outcomes for Patients with Chronic Neck Pain in Short- and Mid-Term? A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 6601. https://doi.org/10.3390/ijerph17186601
Rodríguez-Sanz J, Malo-Urriés M, Corral-de-Toro J, López-de-Celis C, Lucha-López MO, Tricás-Moreno JM, Lorente AI, Hidalgo-García C. Does the Addition of Manual Therapy Approach to a Cervical Exercise Program Improve Clinical Outcomes for Patients with Chronic Neck Pain in Short- and Mid-Term? A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2020; 17(18):6601. https://doi.org/10.3390/ijerph17186601
Chicago/Turabian StyleRodríguez-Sanz, Jacobo, Miguel Malo-Urriés, Jaime Corral-de-Toro, Carlos López-de-Celis, María Orosia Lucha-López, José Miguel Tricás-Moreno, Ana I Lorente, and César Hidalgo-García. 2020. "Does the Addition of Manual Therapy Approach to a Cervical Exercise Program Improve Clinical Outcomes for Patients with Chronic Neck Pain in Short- and Mid-Term? A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 17, no. 18: 6601. https://doi.org/10.3390/ijerph17186601
APA StyleRodríguez-Sanz, J., Malo-Urriés, M., Corral-de-Toro, J., López-de-Celis, C., Lucha-López, M. O., Tricás-Moreno, J. M., Lorente, A. I., & Hidalgo-García, C. (2020). Does the Addition of Manual Therapy Approach to a Cervical Exercise Program Improve Clinical Outcomes for Patients with Chronic Neck Pain in Short- and Mid-Term? A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 17(18), 6601. https://doi.org/10.3390/ijerph17186601








