Increased Medical Visits and Mortality among Adults with Cardiovascular Diseases in Severely Affected Areas after Typhoon Morakot
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
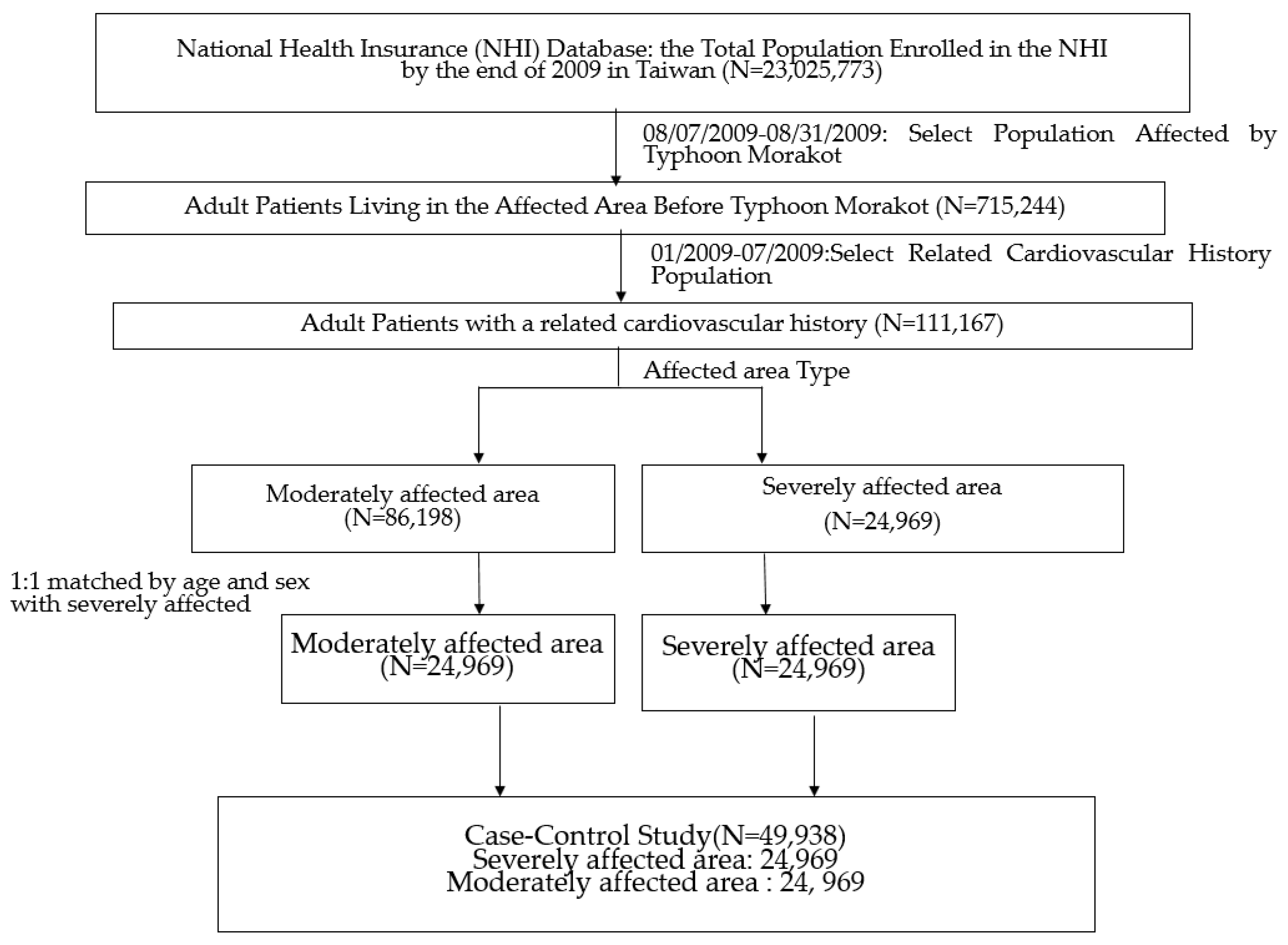
2.2. Study Design
2.3. Spatial-Temporal Analysis
2.4. Covariates
2.5. Statistical Analysis
2.6. Ethical Issues
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
Appendix A
| County | Severely Affected Townships |
|---|---|
| Kaohsiung County * | Jiaxian, Taoyuan, Namaxia, Maolin, Neimen, Liugui, Qishan, Dashu, Shanlin, Meinong |
| Pingtung County * | Jiadong, Linbian, Neipu, Sandimen, Gaoshu, Taiwu, Shizi, Chunri, Wutai, Laiyi, Mudan, Donggang Majia |
| Chiayi County * | Dongshi, Alishan, Meishan, Zhuqi, Fanlu, Dapu |
| Taitung County | Taimali, Jinfeng, Dawu, Daren, Haiduan |
| Tainan County * | Nanhua, Danei, Yujing, Madou, Xuejia |
| Nantou County | Xinyi, Ren’ai, Shuili, Guoxing |
| Yulin County | Gukeng, Kouhu, Yuanchang |
References
- Costello, A.; Abbas, M.; Allen, A.; Ball, S.; Bellamy, R.; Friel, S.; Groce, N.; Johnson, A.; Kett, M.; Lee, M.; et al. Managing the health effects of climate change. Lancet 2009, 373, 1693–1733. [Google Scholar] [CrossRef]
- Smith, K.R.; Woodward, A.; Campbell-Lendrum, D.; Chadee, D.D.; Honda, Y.; Liu, Q.; Olwoch, J.M.; Revich, B.; Sauerborn, R. Human health: Impacts, adaptation, and co-benefits. In Climate Change 2014: Impacts, Adaptation, and Vulnerability; Field, C.B., Barros, V.R., Dokken, D.J., Mach, K.J., Mastrandrea, M.D., Bilir, T.E., Chatterjee, M., Ebi, K.L., Estrada, Y.O., Genova, R.C., et al., Eds.; Cambridge University Press: Cambridge, UK, 2014; pp. 709–754. [Google Scholar]
- World Health Organization. Climate Change and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health (accessed on 15 March 2020).
- Regional Office for the Western Pacific World Health Organization. Emergencies and Disasters; Regional Office for the Western Pacific, World Health Organization: Manila, Philippines, 2005. [Google Scholar]
- Bui, T.; Cho, S.; Sovereign, M. Negotiation issues in multinational humanitarian assistance/disaster relief. In Proceedings of the 32nd Annual Hawaii International Conference on Systems Sciences, Maui, HI, USA, 5–8 January 1999; HICSS-32. [CD-ROM]; Institute of Electrical and Electronics Engineers (IEEE): Piscataway Township, NJ, USA, 2003; p. 10. [Google Scholar]
- Bathi, J.R.; Das, H.S. Vulnerability of Coastal Communities from Storm Surge and Flood Disasters. Int. J. Environ. Res. Public Health 2016, 13, 239. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.R.; Wilson, S.; Brock-Martin, A.; Glover, S.; Svendsen, E.R. The Impact of Disasters on Populations With Health and Health Care Disparities. Disaster Med. Public Health Prep. 2010, 4, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P. What Are Health Disparities and Health Equity? We Need to Be Clear. Public Health Rep. 2014, 129, 5–8. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.E.; Mas, F.S.; Jacobson, H.E.; Harris, A.M.; Hunt, V.I.; Nkhoma, E.T. Public health preparedness of health providers: Meeting the needs of diverse, rural communities. J. Natl. Med. Assoc. 2006, 98, 1784–1791. [Google Scholar]
- Sharma, A.J.; Weiss, E.C.; Young, S.L.; Stephens, K.; Ratard, R.; Straif-Bourgeois, S.; Sokol, T.M.; Vranken, P.; Rubin, C.H. Chronic Disease and Related Conditions at Emergency Treatment Facilities in the New Orleans Area After Hurricane Katrina. Disaster Med. Public Health Prep. 2008, 2, 27–32. [Google Scholar] [CrossRef]
- Hasegawa, A.; Ohira, T.; Maeda, M.; Yasumura, S.; Tanigawa, K. Emergency Responses and Health Consequences after the Fukushima Accident. Clin. Oncol. 2016, 28, 237–244. [Google Scholar] [CrossRef]
- McCann, D.G. A Review of Hurricane Disaster Planning for the Elderly. World Med. Health Policy 2011, 3, 5–30. [Google Scholar] [CrossRef]
- Pelling, M.; Uitto, J.I. Small Island developing states: Natural disaster vulnerability and global change. Environ. Hazards 2001, 3, 49–62. [Google Scholar]
- Lamont-Doherty Earth Observatory Risk Analysis Reports over Half of World’s Population Exposed to One or More Major Natural Hazards. Available online: http://www.earth.columbia.edu/news/2005/story03-29-05.html (accessed on 11 December 2019).
- Kaohsiung County Office The Official List of survivors in Kaohsiung during the Typhoon Morakot. Available online: http://88taiwan.blogspot.tw/2009/08/0815.html (accessed on 11 April 2020).
- National Science and Technology Center for Disaster Reduction, Disaster Survey and Analysis of Morakot Typhoon. National Science and Technology Center for Disaster Reduction Anual Report, 2010; National Science and Technology Center for Disaster Reduction: Taipei, Taiwan, 2010. [Google Scholar]
- Hsieh, C.-Y.; Su, C.-C.; Shao, S.-C.; Sung, S.-F.; Lin, S.-J.; Yang, Y.-H.K.; Lai, E.C.-C. Taiwan’s National Health Insurance Research Database: Past and future. Clin. Epidemiol. 2019, 11, 349–358. [Google Scholar] [CrossRef]
- Lee, T.C.; Yang, C.L.; Wang, T.M. Population Aging and NHI Expenditures in Taiwan. J. Popul. Stud. 2011, 43, 1–35. [Google Scholar]
- Center for Survey Research Academia Sinica Taiwan Social Change Survey. Available online: https://www2.ios.sinica.edu.tw/sc/en/home2.php (accessed on 10 January 2018).
- The World Medical Association Annexe 2. WMA Declaration of Taipei on ethical considerations regarding health databases and biobanks. J. Int. Bioethique Ethique Sci. 2017, 28, 113–117. [Google Scholar] [CrossRef]
- Aoki, T.; Fukumoto, Y.; Yasuda, S.; Sakata, Y.; Ito, K.; Takahashi, J.; Miyata, S.; Tsuji, I.; Shimokawa, H. The Great East Japan Earthquake Disaster and cardiovascular diseases. Eur. Hear. J. 2012, 33, 2796–2803. [Google Scholar] [CrossRef] [PubMed]
- Aoki, T.; Takahashi, J.; Fukumoto, Y.; Yasuda, S.; Ito, K.; Miyata, S.; Shinozaki, T.; Inoue, K.; Yagi, T.; Komaru, T.; et al. Effect of the Great East Japan Earthquake on cardiovascular diseases—Report from the 10 hospitals in the disaster area. Circ. J. 2013, 77, 490–493. [Google Scholar] [CrossRef] [PubMed]
- Swerdel, J.N.; Janevic, T.M.; Cosgrove, N.M.; Kostis, J.B. The Myocardial Infarction Data Acquisition System (MIDAS 24) Study Group the Effect of Hurricane Sandy on Cardiovascular Events in New Jersey. J. Am. Hear. Assoc. 2014, 3, 001354. [Google Scholar] [CrossRef]
- Tsai, C.-H.; Lung, F.-W.; Wang, S.-Y. The 1999 Ji-Ji (Taiwan) Earthquake as a Trigger for Acute Myocardial Infarction. J. Psychosom. Res. 2004, 45, 477–482. [Google Scholar] [CrossRef]
- Dedert, E.A.; Calhoun, P.S.; Watkins, L.L.; Sherwood, A.; Beckham, J.C. Posttraumatic Stress Disorder, Cardiovascular, and Metabolic Disease: A Review of the Evidence. Ann. Behav. Med. 2010, 39, 61–78. [Google Scholar] [CrossRef]
- Edmondson, D.; Cohen, B.E. Posttraumatic stress disorder and cardiovascular disease. Prog. Cardiovasc. Dis. 2013, 55, 548–556. [Google Scholar] [CrossRef]
- Onose, T.; Nochioka, K.; Sakata, Y.; Miura, M.; Tadaki, S.; Ushigome, R.; Yamauchi, T.; Sato, K.; Tsuji, K.; Abe, R.; et al. Predictors and Prognostic Impact of Post-Traumatic Stress Disorder After the Great East Japan Earthquake in Patients With Cardiovascular Disease. Circ. J. 2015, 79, 664–667. [Google Scholar] [CrossRef]
- Lavie, C.J.; Gerber, T.C.; Lanier, W.L. Hurricane Katrina: The Infarcts beyond the Storm. Disaster Med. Public Health Prep. 2009, 3, 131–135. [Google Scholar] [CrossRef]
- Kivimäki, M.; Steptoe, A. Effects of stress on the development and progression of cardiovascular disease. Nat. Rev. Cardiol. 2017, 15, 215–229. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.N.; Moscona, J.C.; Katz, M.J.; DeAndrade, K.B.; Quevedo, H.C.; Tiwari, S.; Burchett, A.R.; Turnage, T.A.; Singh, K.Y.; Fomunung, E.N.; et al. Natural Disasters and Myocardial Infarction: The Six Years After Hurricane Katrina. Mayo Clin. Proc. 2014, 89, 472–477. [Google Scholar] [CrossRef] [PubMed]
- Epel, E.; Lin, J.; Wilhelm, F.H.; Wolkowitz, O.; Cawthon, R.; Adler, N.; Dolbier, C.; Mendes, W.; Blackburn, E. Cell aging in relation to stress arousal and cardiovascular disease risk factors. Psychoneuroendocrinology 2006, 31, 277–287. [Google Scholar] [CrossRef] [PubMed]
- Glynn, L.; Buckley, B.; Reddan, N.; Newell, J.; Hinde, J.; Dinneen, S.F.; Murphy, A.W. Multimorbidity and risk among patients with established cardiovascular disease: A cohort study. Br. J. Gen. Pr. 2008, 58, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Lekoubou, A.; Ovbiagele, B. Prevalence and influence of chronic obstructive pulmonary disease on stroke outcomes in hospitalized stroke patients. eNeurologicalSci 2017, 6, 21–24. [Google Scholar] [CrossRef]
- Yen, Y.-S.; Harnod, D.; Lin, C.-L.; Harnod, T.; Lin, C.-L. Long-Term Mortality and Medical Burden of Patients with Chronic Obstructive Pulmonary Disease with and without Subsequent Stroke Episodes. Int. J. Environ. Res. Public Health 2020, 17, 2550. [Google Scholar] [CrossRef]
- Strand, L.B.; Tsai, M.K.; Wen, C.P.; Chang, S.-S.; Brumpton, B.M. Is having asthma associated with an increased risk of dying from cardiovascular disease? A prospective cohort study of 446 346 Taiwanese adults. BMJ Open 2018, 8, e019992. [Google Scholar] [CrossRef]
- Sturgeon, K.M.; Deng, L.; Bluethmann, S.M.; Zhou, S.; Trifiletti, D.M.; Jiang, C.; Kelly, S.P.; Zaorsky, N.G. A population-based study of cardiovascular disease mortality risk in US cancer patients. Eur. Heart J. 2019, 40, 3889–3897. [Google Scholar] [CrossRef]
- Kim, D.; Adejumo, A.C.; Yoo, E.R.; Iqbal, U.; Li, A.A.; Pham, E.A.; Cholankeril, G.; Glenn, J.S.; Ahmed, A. Trends in Mortality From Extrahepatic Complications in Patients with Chronic Liver Disease, From 2007 Through 2017. Gastroenterology 2019, 157, 1055–1066. [Google Scholar] [CrossRef]
- Healthy People 2020. Disparities. Available online: https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities (accessed on 15 August 2020).
- Basu, S.; Berkowitz, S.A.; Phillips, R.L.; Bitton, A.; Landon, B.E.; Phillips, R.S. Association of Primary Care Physician Supply With Population Mortality in the United States, 2005–2015. JAMA Intern. Med. 2019, 179, 506. [Google Scholar] [CrossRef]
- Ford, E.S.; Mokdad, A.H.; Link, M.W.; Garvin, W.S.; McGuire, L.C.; Jiles, R.B.; Balluz, L.S.; B., J.R. Chronic disease in health emergencies: In the eye of the hurricane. Prev. Chronic Dis. 2006, 3, A46. [Google Scholar] [PubMed]
- Cunningham, P.J.; Felland, L.E. Falling behind: Americans’ access to medical care deteriorates, 2003–2007. Track. Rep. 2008, 19, 1–5. [Google Scholar]
- Asaria, M.; Ali, S.; Doran, T.; Ferguson, B.; Fleetcroft, R.; Goddard, M.; Goldblatt, P.; Laudicella, M.; Raine, R.; Cookson, R. How a universal health system reduces inequalities: Lessons from England. J. Epidemiol. Community Health 2016, 70, 637–643. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.J.; Taylor, S. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Veugelers, P.; Yip, A.M. Socioeconomic disparities in health care use: Does universal coverage reduce inequalities in health? J. Epidemiol. Community Health 2003, 57, 424–428. [Google Scholar] [CrossRef]
- Aitsi-Selmi, A.; Murray, V. The Sendai framework: Disaster risk reduction through a health lens. Bull. World Health Organ. 2015, 93, 362. [Google Scholar] [CrossRef]
- Plough, A.; Fielding, J.E.; Chandra, A.; Williams, M.; Eisenman, D.; Wells, K.B.; Law, G.Y.; Fogleman, S.; Magana, A. Building community disaster resilience: Perspectives from a large urban county department of public health. Am. J. Public Health 2013, 103, 1190–1197. [Google Scholar] [CrossRef]
- Ministry of the Interior. Toward a Sustainable Taiwan: Summary National Spatial Plan. Taiwan. Available online: https://www.cpami.gov.tw/filesys/file/rp6/rp1081203e.pdf (accessed on 15 August 2020).
- United Nations. United Nations Sustainable Development Goals. Available online: https://sdgs.un.org/goals (accessed on 15 August 2020).
- Ministry of the Interior. Disaster Prevention and Protection Act. Available online: https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=D0120014 (accessed on 15 August 2020).
- Pan, Y.-J.; Yeh, L.-L.; Chan, H.-Y.; Chang, C.-K. Transformation of excess mortality in people with schizophrenia and bipolar disorder in Taiwan. Psychol. Med. 2017, 47, 2483–2493. [Google Scholar] [CrossRef]
- Chiu, Y.-W.; Wu, C.-S.; Chen, P.-C.; Wei, Y.-C.; Hsu, L.-Y.; Wang, S.-H. Risk of acute mesenteric ischemia in patients with diabetes: A population-based cohort study in Taiwan. Atherosclerosis 2020, 296, 18–24. [Google Scholar] [CrossRef]
- Kario, K. Disaster hypertension—Its characteristics, mechanism, and management. Circ. J. 2012, 76, 553–562. [Google Scholar] [CrossRef]
- Messerli, F.H.; Panjrath, G.S. The J-Curve between Blood Pressure and Coronary Artery Disease or Essential Hypertension. J. Am. Coll. Cardiol. 2009, 54, 1827–1834. [Google Scholar] [CrossRef] [PubMed]
- Zhou, N.; Xi, B.; Zhao, M.; Wang, L.; Veeranki, S.P. Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: The NHANES III Linked Mortality Study. Sci. Rep. 2018, 8, 9418. [Google Scholar] [CrossRef]
- Shin, S.; Song, H.; Oh, S.-K.; Choi, K.E.; Kim, H.; Jang, S. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertens. Res. 2013, 36, 1000–1005. [Google Scholar] [CrossRef]
- Kim, S.; Shin, D.W.; Yun, J.M.; Hwang, Y.; Park, S.K.; Ko, Y.-J.; Cho, B.L. Medication Adherence and the Risk of Cardiovascular Mortality and Hospitalization Among Patients With Newly Prescribed Antihypertensive Medications. Hypertension 2016, 67, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Chang, A.; Ritchey, M.D.; Loustalot, F. Antihypertensive Medication Adherence and Risk of Cardiovascular Disease among Older Adults: A Population-Based Cohort Study. J. Am. Hear. Assoc. 2017, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Bowling, C.B.; Davis, B.R.; Luciano, A.; Simpson, L.M.; Sloane, R.; Pieper, C.F.; Einhorn, P.T.; Oparil, S.; Muntner, P. Sustained blood pressure control and coronary heart disease, stroke, heart failure, and mortality: An observational analysis of ALLHAT. J. Clin. Hypertens. 2019, 21, 451–459. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Adults Living in the Affected Area | |||
|---|---|---|---|---|
| Moderately Affected | Severely Affected | Total | Chi2-Test p Value | |
| (n = 574,089) | (n = 141,155) | (n = 715,244) | ||
| No. (%) | No. (%) | No. (%) | ||
| Sex | ||||
| Female | 321,697 (56) | 77,122 (55) | 398,819 (56) | <0.0001 |
| Age (years) | ||||
| Mean ± SD * | 51.69 ± 17.87 | 55.29 ± 17.64 | 52.40 ± 17.88 | |
| Age Group | ||||
| Elderly | 151,801 (26) | 48,190 (34) | 199,991 (28) | <0.0001 |
| Related Cardiovascular History (January 2008–July 2009) | ||||
| Either of the following | 86,198 (15) | 24,969 (18) | 111,167 (16) | <0.0001 |
| Ischemic heart diseases | 59,226 (10) | 17,093 (12) | 76,319 (11) | <0.0001 |
| Acute cerebrovascular diseases | 36,559 (6) | 11,003 (8) | 47,562 (7) | <0.0001 |
| Socioeconomic Status (USD/month) | ||||
| Low < $750 USD | 301,416 (53) | 93,431 (66) | 394,847 (55) | |
| Location | ||||
| Urban | 150,232 (26) | 0 (0) | 150,232 (21) | <0.0001 |
| Suburban | 276,951 (48) | 47,890 (34) | 324,841 (45) | |
| Rural | 146,906 (26) | 93,265 (66) | 240,171 (34) | |
| CCI † | ||||
| 0 | 338,653 (59) | 77,717 (55) | 416,370 (58) | <0.0001 |
| 1–2 | 183,175 (32) | 49,034 (35) | 232,209 (32) | |
| >2 | 52,261 (9) | 14,404 (10) | 66,665 (9) | |
| Underlying diseases | ||||
| DM | 79,653 (14) | 21,886 (16) | 101,539 (14) | <0.0001 |
| Hypertension | 143,332 (26) | 45,940 (33) | 189,272 (26) | <0.0001 |
| CKD | 12,959 (2) | 3058 (2) | 16,017 (2) | 0.04 |
| Heart disease | 57,835 (10) | 17,171 (12) | 75,006 (10) | <0.0001 |
| COPD & asthma | 25,612 (4) | 8116 (6) | 33,728 (6) | <0.0001 |
| Liver cirrhosis | 9570 (2) | 2007 (1) | 11,577 (1) | 0.02 |
| Neoplasms | 32,304 (6) | 7341 (5) | 39,645 (6) | 0.01 |
| Characteristics | Adult Patients with a Related Cardiovascular History (January 2008–July 2009) | |||||
|---|---|---|---|---|---|---|
| Pre-Match | Post-Match | |||||
| Moderately Affected | Severely Affected | Moderately Affected | Severely Affected | |||
| (n = 86,198) | (n = 24,969) | Chi2 Test | (n = 24,969) | (n = 24,969) | Chi2 Test | |
| No. (%) | No. (%) | p Value | No. (%) | No. (%) | p Value | |
| Sex | ||||||
| Female | 45,030 (52) | 13,257 (53) | 0.02 | 13,257 (53) | 13,257 (53) | 1.00 |
| Age (years) | ||||||
| Mean ± SD * | 66.84 ± 12.76 | 67.72 ± 12.37 | 67.52 ± 12.63 | 67.72 ± 12.37 | ||
| Age Group | ||||||
| Elderly | 51,724 (60) | 15,814 (63) | <0.0001 | 15,814 (63) | 15,814 (63) | 1.00 |
| Related Cardiovascular History (January 2008–July 2009) | ||||||
| Ischemic heart disease | 59,226 (69) | 17,093(68) | 0.45 | 17,158 (69) | 17,093 (68) | 0.53 |
| Acute cerebrovascular diseases | 36,559 (42) | 11,003 (44) | <0.0001 | 10,568 (42) | 11,003 (44) | <0.0001 |
| Socioeconomic Status (USD/month) | ||||||
| Low < $750 USD | 51,230 (59) | 18,169 (73) | <0.0001 | 14,985 (60) | 18,169 (73) | <0.0001 |
| Location | ||||||
| Urban | 21,279 (25) | 0 (0) | 6213 (25) | 0 (0) | <0.0001 | |
| Suburban | 36,826 (42) | 7267 (29) | <0.0001 | 10,650 (43) | 7267 (29) | |
| Rural | 28,093 (33) | 17,702 (71) | 8106 (32) | 17,702 (71) | ||
| CCI † | ||||||
| 0 | 17,928 (21) | 4918 (20) | 0.0007 | 5102 (20) | 4918 (20) | 0.11 |
| 1–2 | 44,003 (51) | 12,911 (52) | 12,744 (51) | 12,911 (52) | ||
| > 2 | 24,267 (28) | 7140 (29) | 7123 (29) | 7140 (29) | ||
| Underlying diseases | ||||||
| DM | 24,863 (29) | 7063 (28) | 0.09 | 7225 (29) | 7063 (28) | 0.11 |
| Hypertension | 49,642 (58) | 15,468 (62) | <0.0001 | 14,430 (58) | 15,468 (62) | <0.0001 |
| CKD | 4613 (5.4) | 1195 (4.8) | 0.0004 | 1372 (5.5) | 1195 (4.8) | 0.0003 |
| Heart disease | 41,546 (48) | 12,326 (49) | 0.0012 | 12,111 (48) | 12326 (49) | 0.05 |
| COPD & asthma | 8891 (10) | 2933 (12) | <0.0001 | 2662 (11) | 2933 (12) | 0.0001 |
| Liver cirrhosis | 1946 (2.3) | 424 (1.6) | <0.0001 | 553 (2.2) | 424 (1.7) | <0.0001 |
| Neoplasms | 6520 (7.6) | 1748 (7.0) | 0.0028 | 1933 (7.7) | 1748 (7.0) | 0.0015 |
| Characteristics | Adult Patients with a Related Cardiovascular History (January 2008–July 2009/) | |||
|---|---|---|---|---|
| Post-Match | ||||
| Moderately Affected (n = 24,969) No. (%) | Severely Affected (n = 24,969) No. (%) | OR 95% CI | Chi2-Test p Value | |
| Acute ischemic heart diseases | 2607 (10) | 2896 (12) | 1.096 * (1.037–1.16) | <0.0001 |
| Acute cerebrovascular diseases | 1852 (7.4) | 2118 (8.4) | 1.129 * (1.058–1.205) | <0.0001 |
| Heart failure | 1399 (5.6) | 1633 (6.5) | 1.152 * (1.07–1.24) | <0.0001 |
| Infection | 4661 (19) | 5301 (21) | 1.123 * (1.075–1.173) | <0.0001 |
| Trauma and injury | 1238 (4.9) | 1456 (5.8) | 1.161 * (1.074–1.255) | <0.0001 |
| Cerebrovascular Disease History † (n = 21,571) | Ischemic Heart Disease History † (n = 34,251) | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis | Univariate Analysis | Multivariate Analysis | |||||
| HR | 95% CI | aHR | 95% CI | HR | 95% CI | aHR | 95% CI | |
| Location (Ref = Nonrural) | ||||||||
| Rural | 0.93 | 0.86–1.00 | 1.01 | 0.93–1.09 | ||||
| DM (Ref = No) | ||||||||
| Yes | 1.43 * | 1.32–1.56 | 1.40 * | 1.29–1.52 | 1.58 * | 1.46–1.71 | 1.55 * | 1.43–1.68 |
| Hypertension (Ref = No) | ||||||||
| Yes | 0.96 | 0.88–1.04 | 0.85 * | 0.79–0.92 | 0.84 * | 0.77–0.91 | ||
| CKD (Ref = No) | ||||||||
| Yes | 2.24 * | 1.97–2.54 | 2.05 * | 1.81–2.33 | 2.60 * | 2.32–2.91 | 2.40 * | 2.15–2.69 |
| COPD & asthma (Ref = No) | ||||||||
| Yes | 1.88 * | 1.71–2.07 | 1.89 * | 1.72–2.08 | 1.69 * | 1.54–1.86 | 1.69 * | 1.54–1.85 |
| Liver cirrhosis (Ref = No) | ||||||||
| 2.35 * | 1.88–2.93 | 2.23 * | 1.79–2.79 | 3.18 * | 2.64–3.82 | 2.76 * | 2.29–3.32 | |
| Neoplasms (Ref = No) | ||||||||
| 1.61 * | 1.42–1.82 | 1.51 * | 1.33–1.71 | 2.07 * | 1.85–2.31 | 1.87 * | 1.67–2.09 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shih, H.-I.; Chao, T.-Y.; Huang, Y.-T.; Tu, Y.-F.; Sung, T.-C.; Wang, J.-D.; Chang, C.-M. Increased Medical Visits and Mortality among Adults with Cardiovascular Diseases in Severely Affected Areas after Typhoon Morakot. Int. J. Environ. Res. Public Health 2020, 17, 6531. https://doi.org/10.3390/ijerph17186531
Shih H-I, Chao T-Y, Huang Y-T, Tu Y-F, Sung T-C, Wang J-D, Chang C-M. Increased Medical Visits and Mortality among Adults with Cardiovascular Diseases in Severely Affected Areas after Typhoon Morakot. International Journal of Environmental Research and Public Health. 2020; 17(18):6531. https://doi.org/10.3390/ijerph17186531
Chicago/Turabian StyleShih, Hsin-I, Tzu-Yuan Chao, Yi-Ting Huang, Yi-Fang Tu, Tzu-Ching Sung, Jung-Der Wang, and Chia-Ming Chang. 2020. "Increased Medical Visits and Mortality among Adults with Cardiovascular Diseases in Severely Affected Areas after Typhoon Morakot" International Journal of Environmental Research and Public Health 17, no. 18: 6531. https://doi.org/10.3390/ijerph17186531
APA StyleShih, H.-I., Chao, T.-Y., Huang, Y.-T., Tu, Y.-F., Sung, T.-C., Wang, J.-D., & Chang, C.-M. (2020). Increased Medical Visits and Mortality among Adults with Cardiovascular Diseases in Severely Affected Areas after Typhoon Morakot. International Journal of Environmental Research and Public Health, 17(18), 6531. https://doi.org/10.3390/ijerph17186531





