Psychometric Proprieties of a Mobile Application to Measure the Craniovertebral Angle a Validation and Reliability Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
FHPapp
2.3. Measurement Procedure
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shumway-Cook, A.; Woollacott, M.H. Control Motor: Teoría y Aplicaciones Practices, 3rd ed.; Lippincott Williams and Wilkins: Baltimore, MD, USA, 2007. [Google Scholar]
- Ruivo, R.M.; Pezarat-Correia, P.; Carita, A.I. Intrarater and Interrater Reliability of Photographic Measurement of Upper-Body Standing Posture of Adolescents. J. Manip. Physiol. Ther. 2015, 38, 74–80. [Google Scholar] [CrossRef]
- Gadotti, I.C.; Biasotto-González, D.A. Sensitivity of clinical assessments of sagittal head posture. J. Eval. Clin. Pract. 2010, 16, 141–144. [Google Scholar] [CrossRef]
- Bosso, L.R.; Campos Golias, A.R. Rhythmic gymnastics athletes posture: Analysis through photometry. Rev. Bras. Med. Esporte. 2012, 18, 333–337. [Google Scholar] [CrossRef]
- Hospital Da Costa Burela, España, 2005. Cervicalgias y Cervicobraquialgias. Servicio de Traumatología y Cirugía Ortopédica. España. Available online: https://sogacot.org/Documentos/Montero_Cervical.pdf (accessed on 21 July 2020).
- ShaghayeghFard, B.; Ahmadi, A.; Maroufi, N.; Sarrafzadeh, J. Evaluation of forward head posture in sitting and standing positions. Eur. Spine J. 2016, 25, 3577–3582. [Google Scholar] [CrossRef]
- Boland, D.M.; Neufeld, E.V.; Ruddell, J.; Dolezal, B.A.; Cooper, C.B. Inter- and intra-rater agreement of static posture analysis using a mobile application. J. Phys. Ther. Sci. 2016, 28, 3398–3402. [Google Scholar] [CrossRef]
- Lee, C.H.; Lee, S.; Shin, G. Reliability of forward head posture evaluation while sitting, standing, walking and running. Hum. Mov. Sci. 2017, 55, 81–86. [Google Scholar] [CrossRef]
- Yong, M.; Lee, H.; Lee, M. Correlation between head posture and proprioceptive function in the cervical region. J. Phys. Ther. Sci. 2016, 28, 857–860. [Google Scholar] [CrossRef]
- Dunleavy, K.; Neil, J.; Tallon, A.; Adamo, D.E. Reliability and validity of cervical position measurements in individuals with and without chronic neck pain. J. Man. Manip. Ther. 2015, 23, 188–196. [Google Scholar] [CrossRef]
- Pinzón Ríos, I.D. Cabeza hacia adelante: Una mirada desde la biomecánica y sus implicaciones sobre el movimiento corporal humano. Rev. Univ. Ind. Santander. Salud. 2015, 47, 75–83. [Google Scholar]
- Nam, S.H.; Son, S.M.; Kwon, J.W.; Lee, N.K. The intra- and inter-rater reliabilities of the forward head posture assessment of normal healthy subjects. J. Phys. Ther. Sci. 2013, 25, 737–739. [Google Scholar] [CrossRef]
- Lee, K.; Han, H.; Cheon, S.; Park, S.; Yong, M. The effect of forward head posture on muscle activity during neck protraction and retraction. J. Phys. Ther. Sci. 2015, 27, 977–979. [Google Scholar] [CrossRef]
- Cheung Lau, H.M.; Wing Chiu, T.T.; Lam, T. Clinical measurement of craniovertebral angle by electronic head posture instrument: A test of reliability and validity. Man. Ther. 2009, 14, 363–368. [Google Scholar] [CrossRef]
- Salahzadeh, Z.; Maroufi, N.; Ahmadi, A.; Behtash, H.; Razmjoo, A.; Gohari, M.; Parnianpour, M. Assessment of forward head posture in females: Observational and photogrammetry methods. J. Back Musculoeskelet Rehabil. 2014, 27, 131–139. [Google Scholar]
- Furlanetto, T.S.; Sedrez, J.A.; Candotti, C.T.; Loss, J.F. Photogrammetry as a tool for the postural evaluation of the spine: A systematic review. World J. Orthop. 2015, 7, 136–148. [Google Scholar] [CrossRef] [PubMed]
- Guan, X.; Fan, G.; Wu, X.; Zeng, Y.; Su, H.; Gu, G.; Zhou, Q.; Gu, X.; Zhang, H.; He, S. Photographic measurement of head and cervical posture when viewing mobile phone: A pilot study. Eur. Spine. J. 2015, 24, 2892–2898. [Google Scholar] [CrossRef] [PubMed]
- Lau, K.T.; Cheung, K.Y.; Chan, K.B.; Chan, M.H.; Lo, K.Y.; Chiu, T.T. Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability. Man. Ther. 2010, 15, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Pita-Fernández, S.; Pértega-Díaz, S.; Maseda, E.R. La fiabilidad de las mediciones clínicas: El análisis de concordancia para variables numéricas. Cuad. Atención Primaria 2003, 10, 290–296. [Google Scholar]
- Weir, J.P. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar]
- Haley, S.M.; Fragala-Pinkham, M.A. Interpreting change scores of tests and measures used in physical therapy. Phys. Ther. 2006, 86, 735–743. [Google Scholar] [CrossRef]
- Cerda, J.; Cifuentes, L. Using ROC curves in clinical investigation: Theoretical and practical issues. Rev. Chilena. Infectol. 2012, 29, 138–141. [Google Scholar] [CrossRef]
- Bethoux, F.; Bennett, S. Evaluating walking in patients with multiple sclerosis: Which assessment tools are useful in clinical practice? Int. J. MS Care 2011, 13, 4–14. [Google Scholar] [CrossRef]
- Szucs, K.A.; Donoso Brown, E.V. Rater reliability and construct validity of a mobile application for posture analysis. J. Phys. Ther. Sci. 2018, 30, 30–36. [Google Scholar] [CrossRef]
- Quek, J.; Brauer, S.G.; Treleaven, J.; Pua, Y.H.; Mentiplay, B.; Clark, R.A. Validity and intra-rater reliability of an Android phone application to measure cervical range-of-motion. J. Neuroeng. Rehab. 2014, 11, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Youssef, A.R.; Gumaa, M. Validity and reliability of smartphone applications for clinical assessment of the neuromusculoskeletal system. Expert. Rev. Med. Devices 2017, 14, 481–493. [Google Scholar] [CrossRef] [PubMed]
| Variable | Female n = 21 | Male n = 23 | Total n = 44 |
|---|---|---|---|
| Age (Years) | 22.62 (±4.37) [20.63–24.61] | 23.91 (±4.52) [21.96–25.87] | 23.30 (±4.44) [21.94–24.65] |
| Weight (kg) | 66.15 (±16.02) [58.86-73.45] | 75.31 (±10.76) [70.66–79.97] | 70.94 (±14.14) [66.54–75.24] |
| Height (cm) | 166.64 (±5.98) [163.91–169.36] | 177.15 (±5.04) [174.97–179.33] | 172.13 (±7.60) [169.82–174.44] |
| Body Mass Index (BMI) (kg/m2) | 23.84 (±5.99) [21.11–26.57] | 23.93 (±2.68) [22.77–25.09] | 23.88 (±4.51) [22.51–25.26] |
| Cervical Pain | 13 (61.90%) | 9 (39.13%) | n = 22 (50%) |
| Visual Analog Scale (VAS) (cm) Only Cervical Pain | 2.65 (±1.20) [1.92–3.38] | 4.43 (±1.12) [3.57–5.30] | 3.38 (±1.45) [2.73–4.02] |
| Physical Activity Practice | 15 (71.42%) | 21 (91.30%) | n = 36 (81.81%) |
| Physical Activity (h/week) Only Physical Activity | 5.43 (±3.39) [3.55–7.31] | 5.45 (±2.06) [4.51–6.39] | 5.44 (±2.65) [4.54–6.34] |
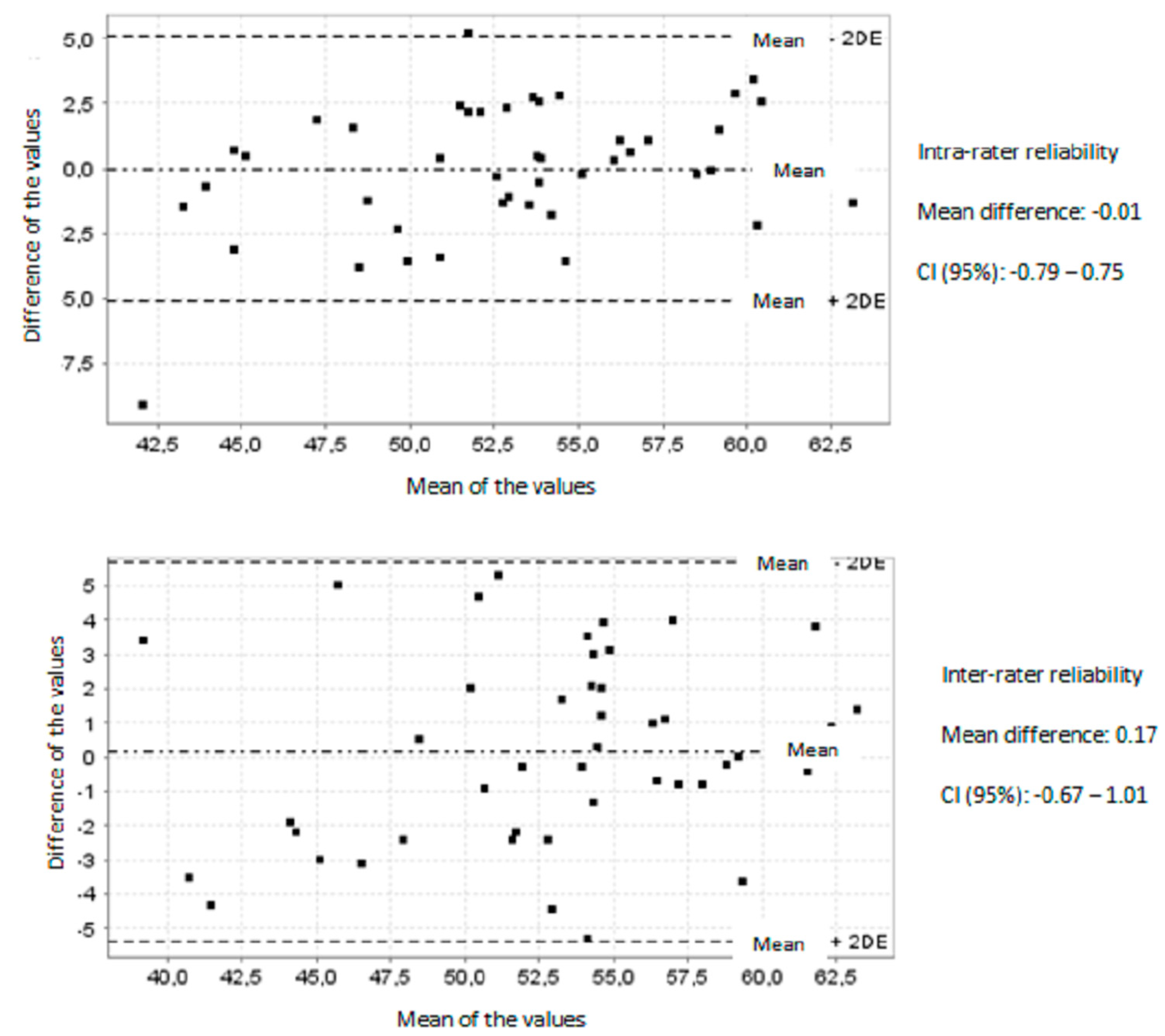
| Observer | Mean (SD) | ICC (95% CI) | SEM | MDC | |
|---|---|---|---|---|---|
| Intra-Observer Reliability | 1 2 | 52.90° (±5.52) 52.79° (±5.17) | 0.85 (0.74–0.91) 0.88 (0.79–0.93) | 2.13° 1.79° | 5.90° 4.96° |
| Session | Mean (SD) | ICC (95% CI) | SEM | MDC | |
| Inter-Observer Reliability | 1 2 | 52.87° (±5.89) 52.82° (±4.74) | 0.89 (0.80–0.93) 0.88 (0.80–0.93) | 1.95° 1.64° | 5.40° 4.54° |
| ICC (95% CI) | SEM | MDC | |
|---|---|---|---|
| FHP1 vs. KIN1 | 0.85 (0.78–0.90) | 2.11° | 5.84° |
| FHP2 vs. KIN2 | 0.88 (0.82–0.91) | 1.83° | 5.07° |
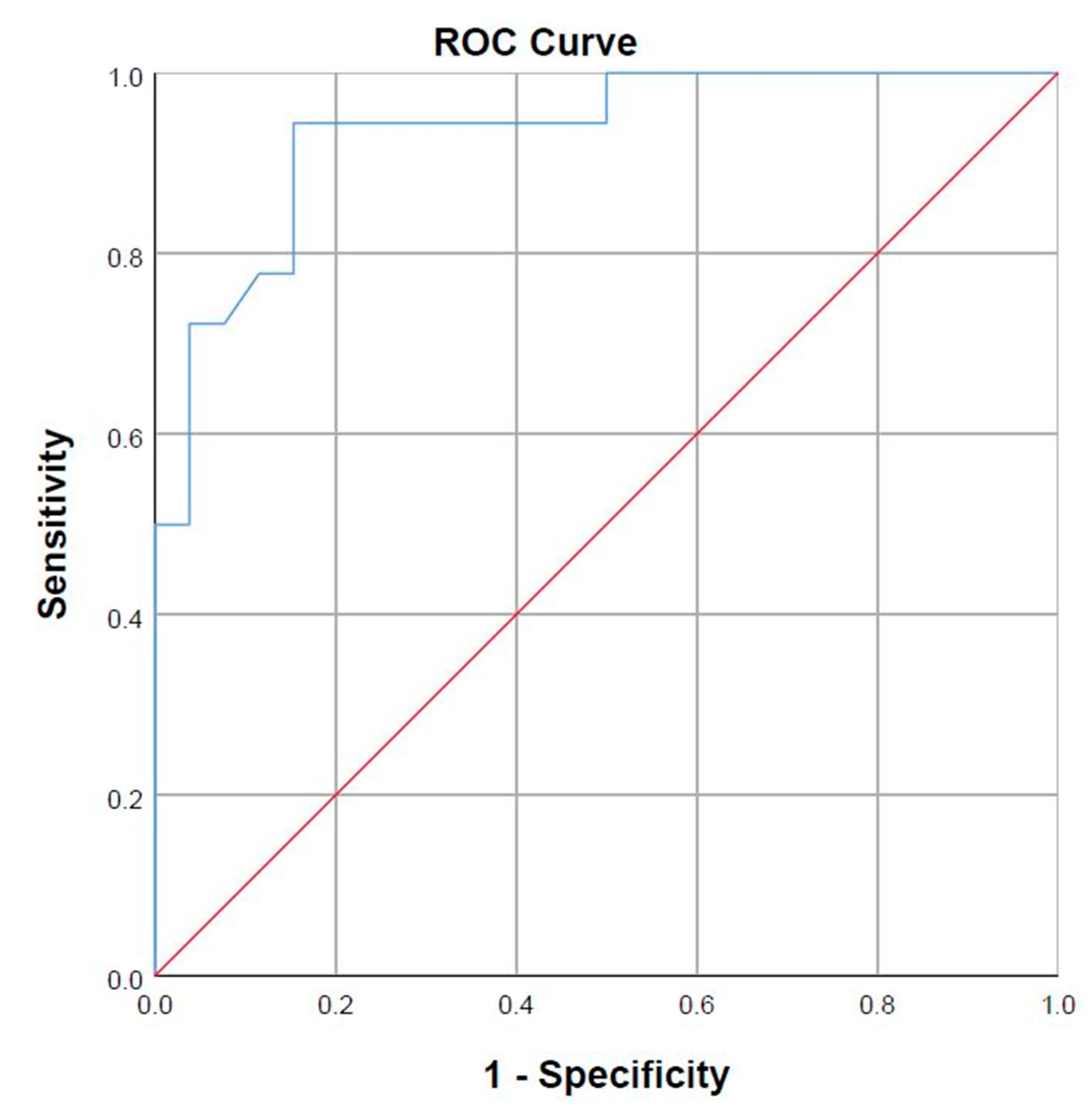
| FHP Application | Correct Percentage (%) | |||
|---|---|---|---|---|
| No FHP | FHP | |||
| Photometry | No FHP | 22 | 4 | 84.6 |
| FHP | 1 | 17 | 94.4 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gallego-Izquierdo, T.; Arroba-Díaz, E.; García-Ascoz, G.; Val-Cano, M.d.A.; Pecos-Martin, D.; Cano-de-la-Cuerda, R. Psychometric Proprieties of a Mobile Application to Measure the Craniovertebral Angle a Validation and Reliability Study. Int. J. Environ. Res. Public Health 2020, 17, 6521. https://doi.org/10.3390/ijerph17186521
Gallego-Izquierdo T, Arroba-Díaz E, García-Ascoz G, Val-Cano MdA, Pecos-Martin D, Cano-de-la-Cuerda R. Psychometric Proprieties of a Mobile Application to Measure the Craniovertebral Angle a Validation and Reliability Study. International Journal of Environmental Research and Public Health. 2020; 17(18):6521. https://doi.org/10.3390/ijerph17186521
Chicago/Turabian StyleGallego-Izquierdo, Tomas, Enrique Arroba-Díaz, Gema García-Ascoz, María del Alba Val-Cano, Daniel Pecos-Martin, and Roberto Cano-de-la-Cuerda. 2020. "Psychometric Proprieties of a Mobile Application to Measure the Craniovertebral Angle a Validation and Reliability Study" International Journal of Environmental Research and Public Health 17, no. 18: 6521. https://doi.org/10.3390/ijerph17186521
APA StyleGallego-Izquierdo, T., Arroba-Díaz, E., García-Ascoz, G., Val-Cano, M. d. A., Pecos-Martin, D., & Cano-de-la-Cuerda, R. (2020). Psychometric Proprieties of a Mobile Application to Measure the Craniovertebral Angle a Validation and Reliability Study. International Journal of Environmental Research and Public Health, 17(18), 6521. https://doi.org/10.3390/ijerph17186521







