How Health Habits Influence the Physiological Response During a Physical Activity in Extreme Temperatures?
Abstract
:1. Introduction
2. Materials and Methods
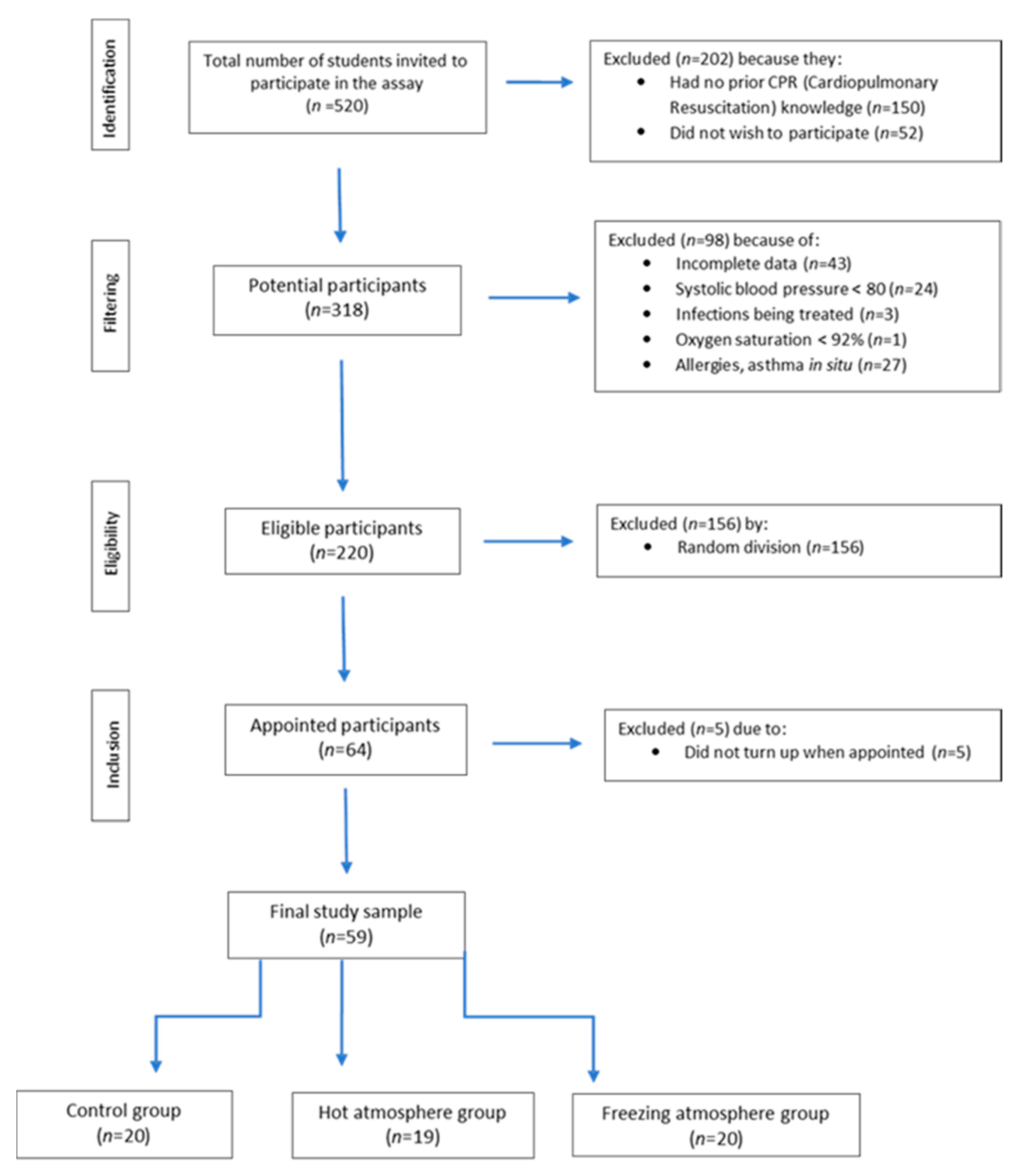
2.1. Study Design
2.2. Population
2.3. Study Protocol
2.4. Data Analysis
3. Results
3.1. Descriptive Data
3.2. Main Results and Outcome Data
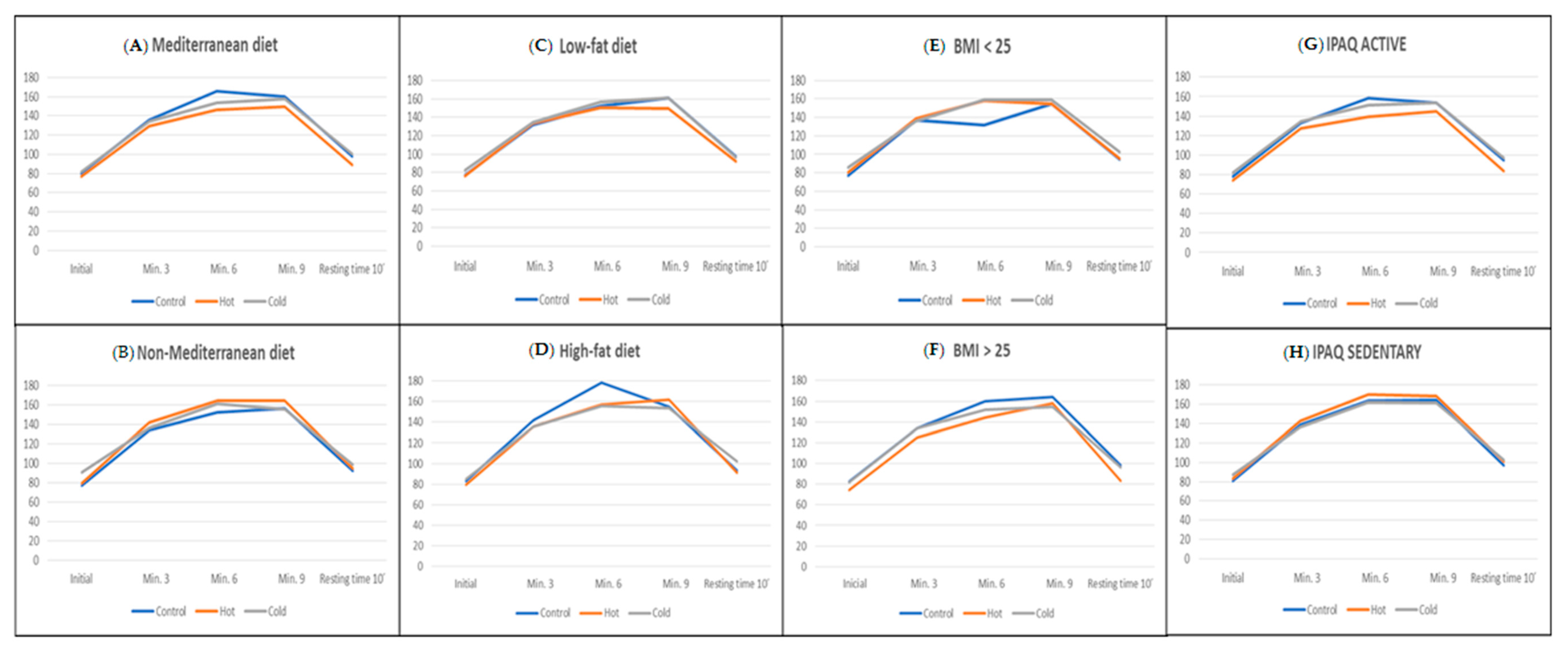
3.2.1. Analysis Based on Adherence to the Mediterranean Diet
3.2.2. Analysis Based on Adherence to a Low-Fat Diet
3.2.3. Analysis Based on Body Mass Index
3.2.4. Analysis Based on the Level of Activity According to IPAQ
3.3. Other Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Variables | Mediterranean Diet | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Control (n = 20) | Hot (n = 19) | Cold (n = 20) | |||||||
| Yes (n = 7) | No (n = 13) | Yes (n = 8) | No (n = 11) | Yes (n = 6) | No (n = 14) | ||||
| Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | |
| Heart Rate | |||||||||
| Initial | 80.5 ± 17.4 | 77.4 ± 11.7 | 0.679 | 77.2 ± 14.0 | 79.7 ± 12.4 | 0.696 | 81.5 ± 14.1 | 90.5 ± 16.1 | 0.227 |
| Min. 3 | 136.2 ± 17.6 | 134.5 ± 9.9 | 0.817 | 129.4 ± 19.4 | 142.1 ± 10.7 | 0.116 | 134.4 ± 18.1 | 136.9 ± 12.3 | 0.764 |
| Min. 6 | 165.5 ± 25.2 | 152.9 ± 28.6 | 0.323 | 146.1 ± 29.4 | 164.7 ± 24.5 | 0.165 | 153.4 ± 23.9 | 161.7 ± 17.1 | 0.451 |
| Min. 9 | 160.3 ± 17.9 | 156.2 ± 15.8 | 0.619 | 149.8 ± 23.2 | 164.3 ± 17.8 | 0.159 | 157.3 ± 23.0 | 155.6 ± 17.7 | 0.877 |
| Resting time 10 min. | 98.2 ± 12.6 | 92.1 ± 11.2 | 0.302 | 89.3 ± 18.2 | 94.7 ± 10.2 | 0.465 | 100.1 ± 16.9 | 98.6 ± 16.2 | 0.859 |
| Blood Lactate | |||||||||
| Initial | 2.3 ± 1.7 | 2.0 ± 1.1 | 0.708 | 1.7 ± 0.7 | 2.1 ± 1.4 | 0.505 | 1.8 ± 1.1 | 2.2 ± 1.4 | 0.473 |
| Min. 3 | 3.2 ± 1.7 | 5.1 ± 2.0 | 0.041 * | 7.9 ± 6.1 | 5.0 ± 4.0 | 0.206 | 3.1 ± 2.6 | 2.9 ± 2.0 | 0.883 |
| Min. 6 | 4.1 ± 2.5 | 6.3 ± 3.1 | 0.114 | 6.5 ± 4.5 | 6.0 ± 4.1 | 0.811 | 3.5 ± 2.3 | 9.2 ± 7.2 | 0.116 |
| Min. 9 | 3.5 ± 2.7 | 5.2 ± 2.3 | 0.206 | 4.3 ± 1.6 | 6.3 ± 4.6 | 0.266 | 3.6 ± 3.1 | 8.2 ± 4.9 | 0.021 * |
| Resting time 10 min. | 3.7 ± 1.5 | 3.3 ± 0.9 | 0.578 | 2.9 ± 1.5 | 2.8 ± 1.6 | 0.940 | 2.5 ± 2.0 | 3.6 ± 2.3 | 0.301 |
| Variables | Adherence to a Fat-Diet | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Control (n = 20) | Hot (n = 19) | Cold (n = 20) | |||||||
| Low (n = 13) | High (n = 7) | Low (n = 9) | High (n = 10) | Low (n = 9) | High (n = 11) | ||||
| Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | |
| Heart Rate | |||||||||
| Initial | 77.3 ± 13.4 | 83.2 ± 19.2 | 0.430 | 76.6 ± 9.0 | 79.8 ± 16.2 | 0.607 | 82.8 ± 16.3 | 85.2 ± 14.4 | 0.733 |
| Min. 3 | 132.1 ± 17.6 | 142.1 ± 4.9 | 0.161 | 133.7 ± 18.6 | 135.8 ± 16.7 | 0.799 | 134.4 ± 20.0 | 135.8 ± 13.6 | 0.858 |
| Min. 6 | 151.7 ± 26.0 | 178.6 ± 17.5 | 0.026 * | 150.3 ± 27.6 | 157.2 ± 30.1 | 0.613 | 156.3 ± 24.4 | 155.6 ± 21.0 | 0.947 |
| Min. 9 | 161.1 ± 17.2 | 154.9 ± 16.9 | 0.448 | 149.1 ± 19.6 | 162.1 ± 22.9 | 0.207 | 160.7 ± 24.3 | 153.6 ± 18.7 | 0.474 |
| Resting time 10 min. | 97.6 ± 10.9 | 93.2 ± 14.9 | 0.466 | 92.9 ± 12.1 | 90.9 ± 18.3 | 0.833 | 96.6 ± 18.4 | 102.1 ± 14.7 | 0.467 |
| Blood Lactate | |||||||||
| Initial | 2.4 ± 1.8 | 1.8 ± 1.0 | 0.470 | 1.7 ± 0.8 | 2.1 ± 1.2 | 0.412 | 2.0 ± 1.2 | 1.8 ± 1.1 | 0.742 |
| Min. 3 | 3.6 ± 2.0 | 4.4 ± 2.1 | 0.432 | 5.9 ± 4.9 | 7.3 ± 5.9 | 0.580 | 2.9 ± 2.3 | 3.1 ± 2.6 | 0.852 |
| Min. 6 | 4.2 ± 2.7 | 6.2 ± 2.6 | 0.126 | 6.7 ± 3.7 | 5.9 ± 4.8 | 0.702 | 5.1 ± 4.1 | 5.4 ± 5.7 | 0.892 |
| Min. 9 | 3.4 ± 2.6 | 5.4 ± 2.4 | 0.111 | 4.1 ± 1.8 | 6.1 ± 4.0 | 0.202 | 4.4 ± 3.7 | 5.4 ± 4.6 | 0.620 |
| Resting time 10 min. | 3.4 ± 1.6 | 3.8 ± 0.7 | 0.489 | 3.1 ± 1.5 | 2.6 ± 1.5 | 0.498 | 2.8 ± 2.2 | 2.8 ± 2.1 | 0.976 |
| Variables | BMI | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Control (n = 20) | Hot (n = 19) | Cold (n = 20) | |||||||
| <25 (n = 11) | >25 (n = 9) | <25 (n = 13) | >25 (n = 6) | <25 (n = 11) | >25 (n = 9) | ||||
| Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | |
| Heart Rate | |||||||||
| Initial | 76.7 ± 14.5 | 82.7 ± 16.7 | 0.398 | 80.2 ±12.5 | 74.1 ± 14.4 | 0.362 | 86.0 ± 14.3 | 81.8 ± 16.2 | 0.547 |
| Min. 3 | 136.8 ± 19.0 | 134.1 ± 9.1 | 0.710 | 139.2 ± 16.2 | 125.2 ± 16.5 | 0.102 | 136.0 ± 15.4 | 134.1 ± 18.2 | 0.803 |
| Min. 6 | 161.8 ± 27.7 | 160.2 ± 26.3 | 0.894 | 158.4 ± 28.4 | 144.2 ± 28.1 | 0.325 | 159.0 ± 22.0 | 152.1 ± 22.6 | 0.504 |
| Min. 9 | 154.7 ± 20.1 | 164.1 ± 10.9 | 0.224 | 154.9 ± 21.5 | 158.1 ± 24.6 | 0.781 | 158.9 ± 23.1 | 154.3 ± 19.3 | 0.640 |
| Resting time 10 min. | 94.5 ± 11.8 | 98.0 ± 13.1 | 0.545 | 95.3 ± 11.2 | 83.5 ± 20.5 | 0.118 | 102.3 ± 16.8 | 96.4 ± 15.9 | 0.434 |
| Blood Lactate | |||||||||
| Initial | 1.8 ± 0.7 | 2.7 ± 2.1 | 0.289 | 1.9 ± 1.0 | 1.9 ± 1.3 | 0.983 | 2.0 ± 1.4 | 1.9 ± 0.9 | 0.922 |
| Min. 3 | 3.8 ± 1.9 | 3.9 ± 2.3 | 0.942 | 5.4 ± 4.1 | 9.3 ± 7.2 | 0.273 | 3.7 ± 2.9 | 2.2 ± 1.2 | 0.165 |
| Min. 6 | 4.9 ± 2.9 | 4.9 ± 2.9 | 0.984 | 6.7 ± 4.0 | 5.4 ± 4.8 | 0.524 | 4.3 ± 2.7 | 6.4 ± 6.8 | 0.422 |
| Min. 9 | 4.2 ± 2.6 | 4.1 ± 2.9 | 0.944 | 5.5 ± 3.9 | 4.4 ± 1.1 | 0.545 | 5.2 ± 4.2 | 4.7 ± 4.3 | 0.787 |
| Resting time 10 min. | 3.9 ± 1.6 | 3.1 ± 0.9 | 0.256 | 2.9 ± 1.4 | 2.6 ± 1.8 | 0.695 | 2.8 ± 2.0 | 2.8 ± 2.3 | 0.959 |
| IPAQ | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Control (n = 20) | Hot (n = 19) | Cold (n = 20) | |||||||
| Active (n = 10) | Sedentary (n = 10) | Active (n = 9) | Sedentary (n = 10) | Active (n = 9) | Sedentary (n = 11) | ||||
| Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | |
| Heart rate | |||||||||
| Initial | 77.7 ± 15.4 | 81.2 ± 16.0 | 0.625 | 74.0 ± 12.7 | 83.1 ± 12.4 | 0.133 | 81.9 ± 13.5 | 87.0 ± 16.8 | 0.464 |
| Min. 3 | 132.7 ± 16.5 | 138.5 ± 13.7 | 0.401 | 127.6 ± 19.6 | 142.7 ± 9.8 | 0.052 * | 134.4 ± 15.9 | 136.0 ± 17.7 | 0.835 |
| Min. 6 | 158.5 ± 28.2 | 163.7 ± 25.8 | 0.668 | 139.6 ± 26.0 | 169.8 ± 22.6 | 0.016 * | 150.9 ± 25.3 | 162.0 ± 16.5 | 0.272 |
| Min. 9 | 153.5 ± 20.8 | 164.3 ± 10.3 | 0.167 | 144.9 ± 19.4 | 168.2 ± 18.1 | 0.016 * | 153.2 ± 25.5 | 161.1 ± 14.4 | 0.419 |
| Resting time 10 min. | 94.9 ± 12.9 | 97.3 ± 12.1 | 0.674 | 83.2 ± 14.3 | 101.0 ± 10.3 | 0.007 * | 97.1 ± 17.7 | 102.7 ± 14.8 | 0.460 |
| Blood Lactate | |||||||||
| Initial | 2.2 ± 1.8 | 2.1 ± 1.3 | 0.913 | 1.6 ± 0.6 | 2.3 ± 1.3 | 0.196 | 2.2 ± 1.4 | 1.6 ± 0.7 | 0.328 |
| Min. 3 | 4.3 ± 1.9 | 3.4 ± 2.0 | 0.332 | 7.2 ± 6.4 | 6.0 ± 4.2 | 0.655 | 3.6 ± 2.8 | 2.4 ± 1.8 | 0.269 |
| Min. 6 | 5.0 ± 3.0 | 4.8 ± 2.8 | 0.845 | 6.3 ± 4.8 | 6.3 ± 3.7 | 0.977 | 4.0 ± 2.4 | 6.8 ± 6.7 | 0.261 |
| Min. 9 | 4.6 ± 2.4 | 3.6 ± 2.9 | 0.449 | 3.7 ± 1.5 | 6.7 ± 4.1 | 0.049 * | 4.5 ± 3.6 | 5.5 ± 4.9 | 0.612 |
| Resting time 10 min. | 3.6 ± 1.8 | 3.4 ± 0.7 | 0.767 | 2.3 ± 1.2 | 3.5 ± 1.6 | 0.097 | 2.6 ± 2.0 | 3.1 ± 2.2 | 0.573 |
References
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- Reiner, M.; Niermann, C.; Jekauc, D.; Woll, A. Long-term health benefits of physical activity—A systematic review of longitudinal studies. BMC Public Health 2013, 13, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Grim, M.; Hortz, B.; Petosa, R.; Grim, M.; Hortz, B.; Petosa, R. Impact evaluation of a pilot web-based intervention to increase physical activity. Am. J. Health Promot. 2011, 25, 227–230. [Google Scholar] [CrossRef]
- García-Meseguer, M.J.; Burriel, F.C.; García, C.V.; Serrano-Urrea, R. Adherence to Mediterranean diet in a Spanish university population. Appetite 2014, 78, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Ansari, W.E.; Stock, C.; Mikolajczyk, R. Relationships between food consumption and living arrangements among university students in four European countries—A cross-sectional study. Nutr. J. 2012, 11, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deliens, T.; Clarys, P.; Bourdeaudhuij, I.; Deforche, B. Weight, socio-demographics, and health behaviour related correlates of academic performance in first year university students. Nutr. J. 2013, 12, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanco-Rojo, R.; Sandoval-Insausti, H.; López-García, E.; Graciani, A.; Ordovás, J.M.; Banegas, J.R.; Rodríguez-Artalejo, F.; Guallar-Castillón, P. Consumption of ultra-processed foods and mortality: A national prospective cohort in Spain. Mayo Clin. Porc. 2019, 94, 2178–2188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baum, C.L. The effects of college on weight: Examining the “freshman 15” myth and other effects of college over the life cycle. Demography 2017, 54, 311–336. [Google Scholar] [CrossRef] [PubMed]
- Gotsis, E.; Anagnostis, P.; Mariolis, A.; Vlachou, A.; Katsiki, N.; Karagiannis, A. Health benefits of the Mediterranean diet: An update of research over the last 5 years. Angiology 2015, 66, 304–318. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Adherence to Mediterranean diet and risk of cancer: An updated systematic review and meta-analysis of observational studies. Cancer Med. 2015, 4, 1933–1947. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Missbach, B.; Konig, J.; Hoffmann, G. Adherence to a Mediterranean diet and risk of diabetes: A systematic review and meta-analysis. Public Health Nutr. 2015, 18, 1292–1299. [Google Scholar] [CrossRef] [Green Version]
- Trichopoulou, A.; Naska, A.; Orfanos, P.; Trichopoulos, D. Mediterranean diet in relation to body mass index and waist-to-hip ratio: The Greek European prospective investigation into cancer and nutrition study. Am. J. Clin. Nutr. 2005, 82, 935–940. [Google Scholar] [CrossRef] [PubMed]
- Widmer, R.J.; Flammer, A.J.; Lerman, L.O.; Lerman, A. The Mediterranean diet, its components, and cardiovascular disease. Am. J. Med. 2015, 128, 229–239. [Google Scholar] [CrossRef] [Green Version]
- Torjesen, I. High fat Mediterranean diet is not linked to greater weight gain than low fat diet. BMJ 2016, 353, i3171. [Google Scholar] [CrossRef]
- Mamplekou, E.; Bountziouka, V.; Psaltopoulou, T.; Zeimbekis, A.; Tsakoundakis, N.; Papaerakleous, N.; Gotsis, E.; Metallinos, G.; Pounis, G.; Polychronopoulos, E.; et al. Urban environment, physical inactivity and unhealthy dietary habits correlate to depression among elderly living in eastern Mediterranean islands: The MEDIS (MEDiterranean ISlands Elderly) study. J. Nutr. Health Aging 2010, 14, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A.; Garcia-Lopez, M.; Bes-Rastrollo, M.; Toledo, E.; Martinez-Lapiscina, E.H.; Delgado-Rodriguez, M.; Vazquez, Z.; Benito, S.; Beunza, J.J. Mediterranean diet and the incidence of cardiovascular disease: A Spanish cohort. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Abbate, R.; Gensini, G.F.; Casini, A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010, 92, 1189–1196. [Google Scholar] [CrossRef] [Green Version]
- Knox, E.; Muros, J.J. Association of lifestyle behaviours with self-esteem through health-related quality of life in Spanish adolescents. Eur. J. Pediatr. 2017, 176, 621–628. [Google Scholar] [CrossRef] [Green Version]
- Galilea-Zabalza, I.; Buil-Cosiales, P.; Salas-Salvado, J.; Toledo, E.; Ortega-Azorín, C.; Díez-Espino, J.; Vázquez-Ruiz, Z.; Zomeño, M.D.; Vioque, J.; Martínez, J.A.; et al. Mediterranean diet and quality of life: Baseline cross-sectional analysis of the PREDIMED-PLUS trial. PLoS ONE 2018, 13, e0198974. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Lacoba, R.; Pardo-García, I.; Amo-Saus, E.; Escribano-Sotos, F. Social determinants of food group consumption based on Mediterranean diet pyramid: A cross-sectional study of university students. PLoS ONE 2020, 15, e0227620. [Google Scholar] [CrossRef] [Green Version]
- Idelson, P.I.; Scalfi, L.; Valerio, G. Adherence to the Mediterranean diet in children and adolescents: A systematic review. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 283–289. [Google Scholar] [CrossRef]
- Mariscal-Arcas, M.; Rivas, A.; Velasco, J.; Ortega, M.; Caballero, A.M.; Olea-Serrano, F. Evaluation of the Mediterranean Diet Quality Index (KIDMED) in children and adolescents in Southern Spain. Public Health Nutr. 2009, 12, 1408–1412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arcila-Agudelo, A.M.; Ferre-Svoboda, C.; Torres-Fernandez, T.; Farran-Codina, A. Determinants of adherence to healthy eating patterns in a population of children and adolescents: Evidence on the Mediterranean diet in the city of Mataro (Catalonia, Spain). Nutrients 2019, 11, 854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sahlin, K. Muscle energetics during explosive activities and potential effects of nutrition and training. Sports Med. 2014, 44, S167–S173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krystle, E. Influence of dietary acid load on exercise performance. Int. J. Sport Nutr. Exerc. Metab. 2017, 27, 213–219. [Google Scholar]
- Kwak, S.J.; Kim, Y.M.; Baek, H.J.; Kim, S.H.; Yim, H.W. Chest compression quality, exercise intensity, and energy expenditure during cardiopulmonary resuscitation using compression-to-ventilation ratios of 15:1 or 30:2 or chest compression only: A randomized, crossover manikin study. Clin. Exp. Emerg. Med. 2016, 3, 148–157. [Google Scholar] [CrossRef] [Green Version]
- Kleinman, M.E.; Goldberger, Z.D.; Rea, T.; Swor, R.A.; Bobrow, B.J.; Brennan, E.E.; Terry, M.; Hemphill, R.; Gazmuri, R.J.; Hazinski, M.F.; et al. 2017 American heart association focused update on adult basic life support and cardiopulmonary resuscitation quality: An update to the American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2018, 137, e7–e13. [Google Scholar] [CrossRef] [PubMed]
- Yamanaka, S.; Young Huh, J.; Nishiyama, K.; Hayashi, H. The optimal number of personnel for good quality of chest compressions: A prospective randomized parallel manikin trial. PLoS ONE 2017, 12, e0189412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin-Conty, J.L.; Martin-Rodríguez, F.; Criado-Álvarez, J.J.; Romo Barrientos, C.; Maestre-Miquel, C.; Viñuela, A.; Polonio-López, B.; Durantez-Fernández, C.; Marcos-Tejedor, F.; Mohedano-Moriano, A. Do rescuers’ physiological responses and anxiety influence quality resuscitation under extreme temperatures? Int. J. Environ. Res. Public Health 2020, 17, 4241. [Google Scholar] [CrossRef] [PubMed]
- Martin-Conty, J.L.; Polonio-López, B.; Maestre-Miquel, C.; Mohedano-Moriano, A.; Durantez-Fernández, C.; Mordillo-Mateos, L.; Jurado-Palomo, J.; Viñuela, A.; Bernal-Jiménez, J.J.; Martin-Rodríguez, F. Physiological response of quality cardiopulmonary resuscitation, crossover trial on mannequin in extreme temperature conditions. Int. J. Environ. Res. Public Health 2020, 17, 5835. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-Country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean diet quality index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davy, S.R.; Benes, B.A.; Driskell, J.A. Sex differences in dieting trends, eating habits, and nutrition beliefs of a group of midwestern college students. J. Am. Diet. Assoc. 2006, 106, 1673–1677. [Google Scholar] [CrossRef] [PubMed]
- Haberman, S.; Luffey, D. Weighing in college students’ diet and exercise behaviors. J. Am. Coll. Health 1998, 46, 189–191. [Google Scholar] [CrossRef] [PubMed]
- Von Bothmer, M.I.; Fridlund, B. Gender differences in health habits and in motivation for a healthy lifestyle among Swedish university students. Nurs. Health Sci. 2005, 7, 107–118. [Google Scholar] [CrossRef] [PubMed]
- McKinney, C.E. Assessment of Dietary Behaviors of College Students Participating in the Health Promotion Program BUCS: Live Well. Master’s Thesis, Department of Allied Health Science, East Tennessee State University, Johnson City, TN, USA, May 2013. [Google Scholar]
- Papadaki, S.; Mavrikaki, E. Greek adolescents and the Mediterranean diet: Factors affecting quality and adherence. Nutrition 2015, 31, 345–349. [Google Scholar] [CrossRef]
- Tektonidis, T.G.; Akesson, A.; Gigante, B.; Wolk, A.; Larsson, S.C. Adherence to a Mediterranean diet is associated with reduced risk of heart failure in men. Eur. J. Heart Fail. 2016, 18, 253–259. [Google Scholar] [CrossRef] [Green Version]
- Papadaki, A.; Martinez-Gonzalez, M.A.; Alonso-Gomez, A.; Rekondo, J.; Salas-Salvado, J.; Corella, D.; Ros, E.; Fito, M.; Estruch, R.; Lapetra, J.; et al. Mediterranean diet and risk of heart failure: Results from the PREDIMED randomized controlled trial. Eur. J. Heart Fail. 2017, 19, 1179–1185. [Google Scholar] [CrossRef]
- Wirth, J.; di Giuseppe, R.; Boeing, H.; Weikert, C. A Mediterranean-style diet, its components and the risk of heart failure: A prospective population-based study in a non-Mediterranean country. Eur. J. Clin. Nutr. 2016, 70, 1015–1021. [Google Scholar] [CrossRef]
- Levitan, E.B.; Lewis, C.E.; Tinker, L.F.; Eaton, C.B.; Ahmed, A.; Manson, J.E.; Snetselaar, L.G.; Martin, L.W.; Trevisan, M.; Howard, B.V.; et al. Mediterranean and DASH diet scores and mortality in women with heart failure: The Women’s health initiative. Circ. Heart Fail. 2013, 6, 1116–1123. [Google Scholar] [CrossRef] [Green Version]
- Miro, O.; Estruch, R.; Martin-Sanchez, F.J.; Gil, V.; Jacob, J.; Herrero-Puente, P.; Herrera-Mateo, S.; Aguirre, A.; Andueza, J.A.; Llorens, P. Adherence to Mediterranean diet and all-cause mortality after an episode of acute heart failure: Results of the MEDIT-AHF study. JACC Heart Fail. 2018, 6, 52–62. [Google Scholar] [CrossRef] [PubMed]
- Chrysohoou, C.; Panagiotakos, D.B.; Aggelopoulos, P.; Kastorini, C.M.; Kehagia, I.; Pitsavos, C.; Stefanadis, C. The Mediterranean diet contributes to the preservation of left ventricular systolic function and to the long-term favorable prognosis of patients who have had an acute coronary event. Am. J. Clin. Nutr. 2010, 92, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Robergs, R.A.; Ghiasvand, F.; Parker, D. Biochemistry of exercise-induced metabolic acidosis. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2004, 287, 502–516. [Google Scholar] [CrossRef] [PubMed]
- Enderle, B.; Moser, I.; Kannan, C.; Schwab, K.O.; Urban, G. Interstitial glucose and lactate levels are inversely correlated with the body mass index: Need for in vivo calibration of glucose sensor results with blood values in obese patients. J. Diabetes Sci. Technol. 2018, 12, 341–348. [Google Scholar] [CrossRef] [Green Version]
- Antonopoulou, M.; Mantzorou, M.; Serdari, A.; Bonotis, K.; Vasios, G.; Pavlidou, E.; Trifonos, C.; Vadikolias, K.; Petridis, D.; Giaginis, C. Evaluating Mediterranean diet adherence in university student populations: Does this dietary pattern affect students’ academic performance and mental health? Int. J. Health Plan. Manag. 2020, 35, 5–21. [Google Scholar] [CrossRef]
- Bonaccio, M.; Di Castelnuovo, A.; Bonanni, A.; Costanzo, S.; De Lucia, F.; Pounis, G.; Zito, F.; Donati, M.B.; De Gaetano, G.; Iacoviello, L. Adherence to a Mediterranean diet is associated with a better health-relatedquality of life: A possible role of high dietary antioxidant content. BMJ Open 2013, 3, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Henriquez, S.P.; Ruano, C.; de Irala, J.; Ruiz-Canela, M.; Martinez-Gonzalez, M.A.; Sanchez-Villegas, A. Adherence to the Mediterranean diet and quality of life in the SUN Project. Eur. J. Clin. Nutr. 2012, 66, 360–368. [Google Scholar] [CrossRef]
- Pérez-Tasigchana, R.F.; León-Muñoz, L.M.; Lopez-Garcia, E.; Banegas, J.R.; Rodríguez-Artalejo, F.; Guallar-Castillón, P. Mediterranean diet and health-related quality of life in two cohorts of community-dwelling older adults. PLoS ONE 2016, 11, e0151596. [Google Scholar]
- Zaragoza-Martí, A.; Ferrer-Cascales, R.; Hurtado-Sánchez, J.A.; Laguna-Pérez, A.; Cabañero-Martínez, M.J. Relationship between adherence to the mediterranean diet and health-related quality of life and life satisfaction among older adults. J. Nutr. Health Aging 2018, 22, 89–96. [Google Scholar] [CrossRef]
- Munoz, M.A.; Fito, M.; Marrugat, J.; Covas, M.I.; Schroder, H. Adherence to the Mediterranean diet is associated with better mental and physical health. Br. J. Nutr. 2009, 101, 1821–1827. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milte, C.M.; Thorpe, M.G.; Crawford, D.; Ball, K.; McNaughton, S.A. Associations of diet quality with health-related quality of life in older Australian men and women. Exp. Gerontol. 2015, 64, 8–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variables | Control | Hot | Cold | Total | p-Value | ||
|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n | ||||
| IPAQ | Sedentary | 10 | 9 | 9 | 28 | 0.951 | |
| 35.7% | 32.1% | 32.1% | |||||
| Active | 10 | 10 | 11 | 31 | |||
| 32.3% | 32.3% | 35.5% | |||||
| BMI | Normal weight | 11 | 13 | 11 | 35 | 0.618 | |
| 31.4% | 37.1% | 31.4% | |||||
| Excess weight | 9 | 6 | 9 | 24 | |||
| 37.5% | 25% | 37.5% | |||||
| Mediterranean diet | No | 7 | 8 | 6 | 21 | 0.731 | |
| 33.3% | 38.1% | 28.6% | |||||
| Yes | 13 | 11 | 14 | 38 | |||
| 34.2% | 28.9% | 36.8% | |||||
| Fat diet | High | 7 | 10 | 11 | 28 | 0.386 | |
| 25% | 35.7% | 39.3% | |||||
| Low | 13 | 9 | 9 | 31 | |||
| 41.9% | 29% | 29% | |||||
| Mediterranean Diet | Adherence to a Fat Diet | BMI | IPAQ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 38) | No (n = 21) | Low (n = 31) | High (n = 28) | <25 (n = 35) | >25 (n = 24) | Active (n = 31) | Sedentary (n = 28) | |||||
| Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value | |
| Heart Rate | ||||||||||||
| Initial | 79.9 ± 15.0 | 82.0 ± 13.8 | 0.599 | 78.7 ± 13.1 | 82.8 ± 15.8 | 0.289 | 80.9 ± 13.8 | 80.2 ± 15.7 | 0.862 | 78.0 ± 13.8 | 83.6 ± 14.9 | 0.135 |
| Min. 3 | 133.6 ± 18.0 | 138.1 ± 10.9 | 0.305 | 133.2 ± 18.0 | 137.4 ± 13.2 | 0.322 | 137.4 ± 16.5 | 131.9 ± 14.8 | 0.194 | 131.7 ± 17.0 | 139.1 ± 13.8 | 0.074 |
| Min. 6 | 155.4 ± 26.5 | 159.9 ± 23.5 | 0.519 | 152.6 ± 25.3 | 161.9 ± 25.1 | 0.164 | 159.7 ± 25.6 | 153.2 ± 25.1 | 0.340 | 149.7 ± 26.7 | 165.1 ± 21.5 | 0.019 * |
| Min. 9 | 156.2 ± 21.3 | 159.1 ± 16.8 | 0.584 | 157.5 ± 20.2 | 156.9 ± 19.6 | 0.918 | 156.1 ± 21.0 | 158.9 ± 17.9 | 0.595 | 150.6 ± 21.8 | 164.5 ± 14.2 | 0.005 * |
| Resting time 10 min. | 96.3 ± 16.2 | 95.0 ± 12.1 | 0.738 | 95.8 ± 13.5 | 95.9 ± 16.4 | 0.982 | 97.3 ± 13.4 | 93.7 ± 16.6 | 0.375 | 91.9 ± 15.9 | 100.2 ± 12.3 | 0.030 * |
| Blood Lactate | ||||||||||||
| Initial | 1.9 ± 1.3 | 2.1 ± 1.2 | 0.643 | 2.1 ± 1.4 | 1.9 ± 1.1 | 0.672 | 1.9 ± 1.0 | 2.2 ± 1.5 | 0.385 | 2.0 ± 1.4 | 2.0 ± 1.1 | 0.940 |
| Min. 3 | 4.5 ± 4.2 | 4.4 ± 3.0 | 0.946 | 4.1 ± 3.3 | 4.9 ± 4.3 | 0.386 | 4.4 ± 3.2 | 4.6 ± 4.6 | 0.825 | 5.0 ± 4.3 | 3.9 ± 3.2 | 0.287 |
| Min. 6 | 4.6 ± 3.3 | 7.0 ± 4.9 | 0.053 * | 5.2 ± 3.5 | 5.8 ± 4.6 | 0.561 | 5.4 ± 3.4 | 5.6 ± 4.9 | 0.881 | 5.0 ± 3.5 | 5.9 ± 4.6 | 0.418 |
| Min. 9 | 3.8 ± 2.6 | 6.5 ± 4.1 | 0.011 * | 3.9 ± 2.7 | 5.6 ± 3.8 | 0.051 * | 5.0 ± 3.6 | 4.4 ± 3.1 | 0.525 | 4.3 ± 2.6 | 5.2 ± 4.1 | 0.300 |
| Resting time 10 min. | 3.0 ± 1.7 | 3.2 ± 1.6 | 0.682 | 3.1 ± 1.7 | 3.0 ± 1.6 | 0.743 | 3.2 ± 1.7 | 2.9 ± 1.7 | 0.538 | 2.8 ± 1.8 | 3.3 ± 1.5 | 0.243 |
| Variables | Total (n = 59) | Control (n = 20) | Hot (n = 19) | Cold (n = 20) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value | |
| Initial weight (kg) | 71.59 ± 15.58 | 0.000 * | 72.76 ± 14.65 | 0.007 * | 67.71 ± 10.93 | 0.022 * | 74.10 ± 19.74 | 0.268 |
| Final weight (kg) | 71.36 ± 15.41 | 72.49 ± 14.51 | 67.44 ± 10.71 | 73.97 ± 19.54 | ||||
| Initial muscle mass (kg) | 47.21 ± 6.17 | 0.018 * | 46.47 ± 5.95 | 0.500 | 46.44 ± 4.90 | 0.001 * | 48.68 ± 7.40 | 0.527 |
| Final muscle mass (kg) | 47.90 ± 5.90 | 46.90 ± 6.22 | 47.83 ± 4.38 | 48.96 ± 6.88 | ||||
| Initial body water (%) | 51.99 ± 8.53 | 0.087 | 49.20 ± 11.82 | 0.288 | 54.21 ± 4.86 | 0.000 * | 52.67 ± 6.82 | 0.996 |
| Final body water (%) | 53.36 ± 6.32 | 51.46 ± 5.38 | 56.10 ± 4.95 | 52.66 ± 7.62 | ||||
| Initial bone mass (kg) | 2.54 ± 0.31 | 0.203 | 2.50 ± 0.29 | 0.725 | 2.48 ± 0.24 | 0.006 * | 2.62 ± 0.37 | 0.781 |
| Final bone mass (kg) | 2.56 ± 0.29 | 2.51 ± 0.29 | 2.55 ± 0.22 | 2.61 ± 0.35 | ||||
| Initial body fat (%) | 29.07 ± 8.17 | 0.000 * | 31.48 ± 7.49 | 0.054 | 26.62 ± 6.92 | 0.001 * | 29.00 ± 9.50 | 0.092 |
| Final body fat (%) | 27.56 ± 8.68 | 30.13 ± 8.16 | 24.39 ± 7.01 | 28.00 ± 9.98 | ||||
| Initial visceral fat | 3.74 ± 2.90 | 0.000 * | 4.30 ± 2.79 | 0.019 * | 2.71 ± 1.79 | 0.001 * | 4.15 ± 3.65 | 0.101 |
| Final visceral fat | 3.25 ± 2.53 | 3.68 ± 2.33 | 2.32 ± 1.78 | 3.73 ± 3.13 | ||||
| Initial BMI | 24.76 ± 4.44 | 0.001 * | 25.22 ± 4.67 | 0.007 * | 23.64 ± 2.90 | 0.027 * | 25.37 ± 5.35 | 0.433 |
| Final BMI | 24.68 ± 4.38 | 25.12 ± 4.59 | 23.55 ± 2.83 | 25.34 ± 5.29 | ||||
| Variables | Mediterranean Diet | Adherence to a Fat Diet | BMI | IPAQ | ||||
|---|---|---|---|---|---|---|---|---|
| Yes (n = 38) | No (n = 21) | Low (n = 31) | High (n = 28) | <25 (n = 35) | >25 (n = 24) | Active (n = 31) | Sedentary (n = 28) | |
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| Initial weight (kg) | 74.76 ± 16.19 | 65.85 ± 12.83 | 71.55 ± 11.70 | 71.63 ± 19.21 | 62.62 ± 8.04 | 84.67 ± 14.68 | 68.84 ± 13.98 | 74.64 ± 16.94 |
| Final weight (kg) | 74.50 ± 16.02 | 65.69 ± 12.73 | 71.38 ± 11.66 | 71.34 ± 18.95 | 62.56 ± 8.05 | 84.20 ± 14.60 | 68.70 ± 13.92 | 74.31 ± 16.67 |
| p-value | 0.004 * | 0.041 * | 0.041 * | 0.005 * | 0.336 | 0.000 * | 0.132 | 0.000 * |
| Initial muscle mass (kg) | 48.19 ± 6.30 | 45.44 ± 5.67 | 47.45 ± 5.59 | 46.94 ± 6.86 | 44.65 ± 4.53 | 50.94 ± 6.43 | 47.10 ± 6.14 | 47.33 ± 6.32 |
| Final muscle mass (kg) | 49.07 ± 6.22 | 45.78 ± 4.71 | 47.86 ± 4.76 | 47.93 ± 7.05 | 45.77 ± 4.53 | 51.00 ± 6.37 | 48.00 ± 5.78 | 47.78 ± 6.14 |
| p-value | 0.002 * | 0.600 | 0.375 | 0.003 * | 0.002 * | 0.895 | 0.002 * | 0.390 |
| Initial body water (%) | 50.62 ± 9.64 | 54.46 ± 5.40 | 52.56 ± 5.40 | 51.35 ± 11.10 | 56.09 ± 4.21 | 46.01 ± 9.73 | 54.31 ± 5.94 | 49.42 ± 10.21 |
| Final body water (%) | 52.83 ± 6.04 | 54.32 ± 6.84 | 53.23 ± 5.94 | 53.51 ± 6.83 | 56.87 ± 4.83 | 48.24 ± 4.51 | 55.44 ± 5.70 | 51.06 ± 6.27 |
| p-value | 0.043 * | 0.903 | 0.041 * | 0.196 | 0.231 | 0.204 | 0.002 * | 0.324 |
| Initial bone mass (kg) | 2.59 ± 0.31 | 2.44 ± 0.29 | 2.54 ± 0.26 | 2.53 ± 0.36 | 2.42 ± 0.23 | 2.71 ± 0.34 | 2.54 ± 0.30 | 2.54 ± 0.32 |
| Final bone mass (kg) | 2.62 ± 0.30 | 2.45 ± 0.24 | 2.55 ± 0.24 | 2.56 ± 0.34 | 2.45 ± 0.22 | 2.71 ± 0.32 | 2.56 ± 0.29 | 2.56 ± 0.29 |
| p-value | 0.133 | 0.706 | 0.587 | 0.213 | 0.123 | 0.883 | 0.405 | 0.345 |
| Initial body fat (%) | 30.57 ± 8.36 | 26.36 ± 7.24 | 29.26 ± 7.42 | 28.86 ± 9.07 | 24.38 ± 5.57 | 35.91 ± 6.34 | 27.08 ± 8.03 | 31.28 ± 7.89 |
| Final body fat (%) | 28.87 ± 8.56 | 25.20 ± 8.58 | 28.19 ± 8.35 | 26.87 ± 9.13 | 22.10 ± 5.12 | 35.53 ± 6.30 | 25.04 ± 7.93 | 30.35 ± 8.75 |
| p-value | 0.000 * | 0.205 | 0.056 | 0.000 * | 0.000 * | 0.516 | 0.000 * | 0.107 |
| Initial visceral fat | 3.99 ± 2.78 | 3.29 ± 3.12 | 3.84 ± 2.73 | 3.63 ± 3.13 | 2.00 ± 1.13 | 6.27 ± 2.85 | 2.94 ± 2.22 | 4.63 ± 3.33 |
| Final visceral fat | 3.66 ± 2.69 | 2.52 ± 2.08 | 3.24 ± 2.03 | 3.27 ± 3.02 | 1.73 ± 1.00 | 5.48 ± 2.44 | 2.68 ± 2.12 | 3.89 ± 2.82 |
| p-value | 0.000 * | 0.028 * | 0.011 * | 0.000 * | 0.000 * | 0.008 * | 0.000 * | 0.005 * |
| Initial BMI | 25.59 ± 4.75 | 23.27 ± 3.46 | 24.56 ± 3.40 | 24.99 ± 5.43 | 21.96 ± 1.71 | 28.85 ± 4.01 | 23.69 ± 3.52 | 25.95 ± 5.09 |
| Final BMI | 25.49 ± 4.66 | 23.22 ± 3.45 | 24.50 ± 3.37 | 24.89 ± 5.33 | 21.94 ± 1.72 | 28.69 ± 3.97 | 23.65 ± 3.50 | 25.84 ± 4.99 |
| p-value | 0.006 * | 0.076 | 0.059 | 0.008 * | 0.400 | 0.000 * | 0.169 | 0.001 * |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martin-Conty, J.L.; Martin-Rodríguez, F.; Criado-Álvarez, J.J.; Castillo-Sarmiento, C.A.; Maestre-Miquel, C.; Mohedano-Moriano, A.; Polonio-López, B.; Durantez-Fernández, C.; Castro-Villamor, M.Á.; Viñuela, A. How Health Habits Influence the Physiological Response During a Physical Activity in Extreme Temperatures? Int. J. Environ. Res. Public Health 2020, 17, 6374. https://doi.org/10.3390/ijerph17176374
Martin-Conty JL, Martin-Rodríguez F, Criado-Álvarez JJ, Castillo-Sarmiento CA, Maestre-Miquel C, Mohedano-Moriano A, Polonio-López B, Durantez-Fernández C, Castro-Villamor MÁ, Viñuela A. How Health Habits Influence the Physiological Response During a Physical Activity in Extreme Temperatures? International Journal of Environmental Research and Public Health. 2020; 17(17):6374. https://doi.org/10.3390/ijerph17176374
Chicago/Turabian StyleMartin-Conty, José Luis, Francisco Martin-Rodríguez, Juan José Criado-Álvarez, Carlos Alberto Castillo-Sarmiento, Clara Maestre-Miquel, Alicia Mohedano-Moriano, Begoña Polonio-López, Carlos Durantez-Fernández, Miguel Ángel Castro-Villamor, and Antonio Viñuela. 2020. "How Health Habits Influence the Physiological Response During a Physical Activity in Extreme Temperatures?" International Journal of Environmental Research and Public Health 17, no. 17: 6374. https://doi.org/10.3390/ijerph17176374
APA StyleMartin-Conty, J. L., Martin-Rodríguez, F., Criado-Álvarez, J. J., Castillo-Sarmiento, C. A., Maestre-Miquel, C., Mohedano-Moriano, A., Polonio-López, B., Durantez-Fernández, C., Castro-Villamor, M. Á., & Viñuela, A. (2020). How Health Habits Influence the Physiological Response During a Physical Activity in Extreme Temperatures? International Journal of Environmental Research and Public Health, 17(17), 6374. https://doi.org/10.3390/ijerph17176374









