The Perspectives of Professional Caregivers on Implementing Audio-Based Technology in Residential Dementia Care
Abstract
1. Introduction
2. Materials and Methods
2.1. Vita: Audio-Based Design Intervention
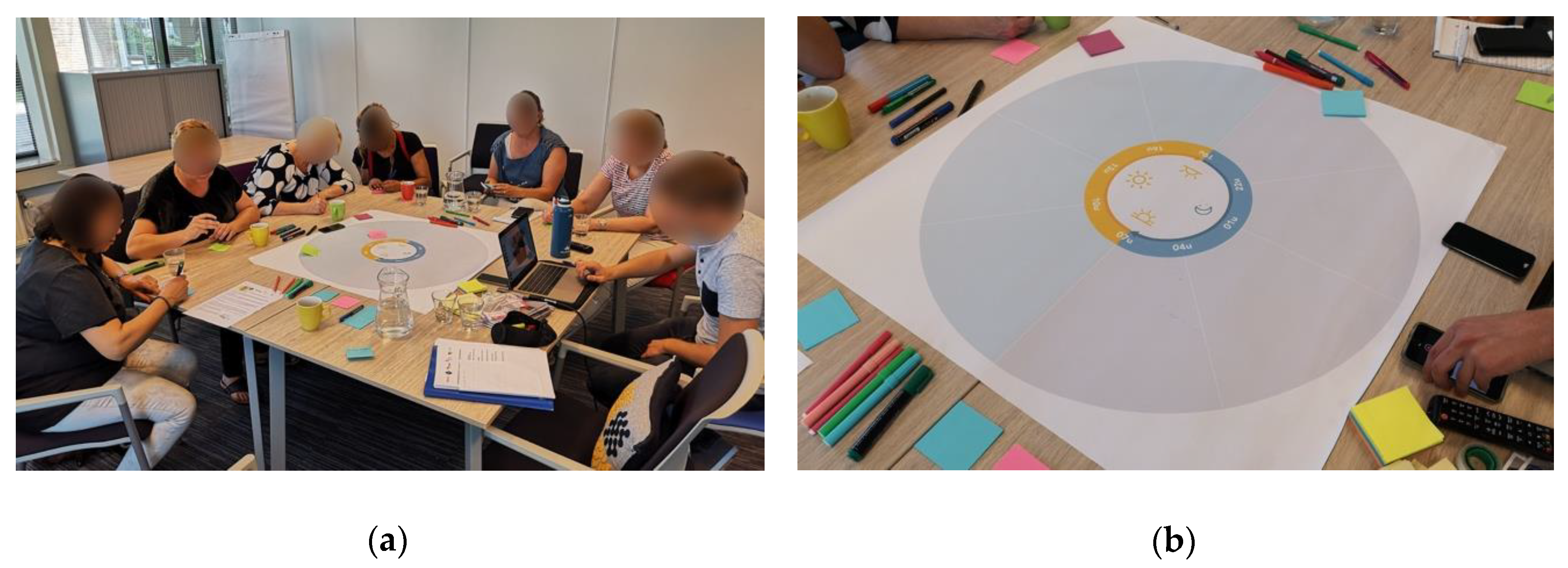
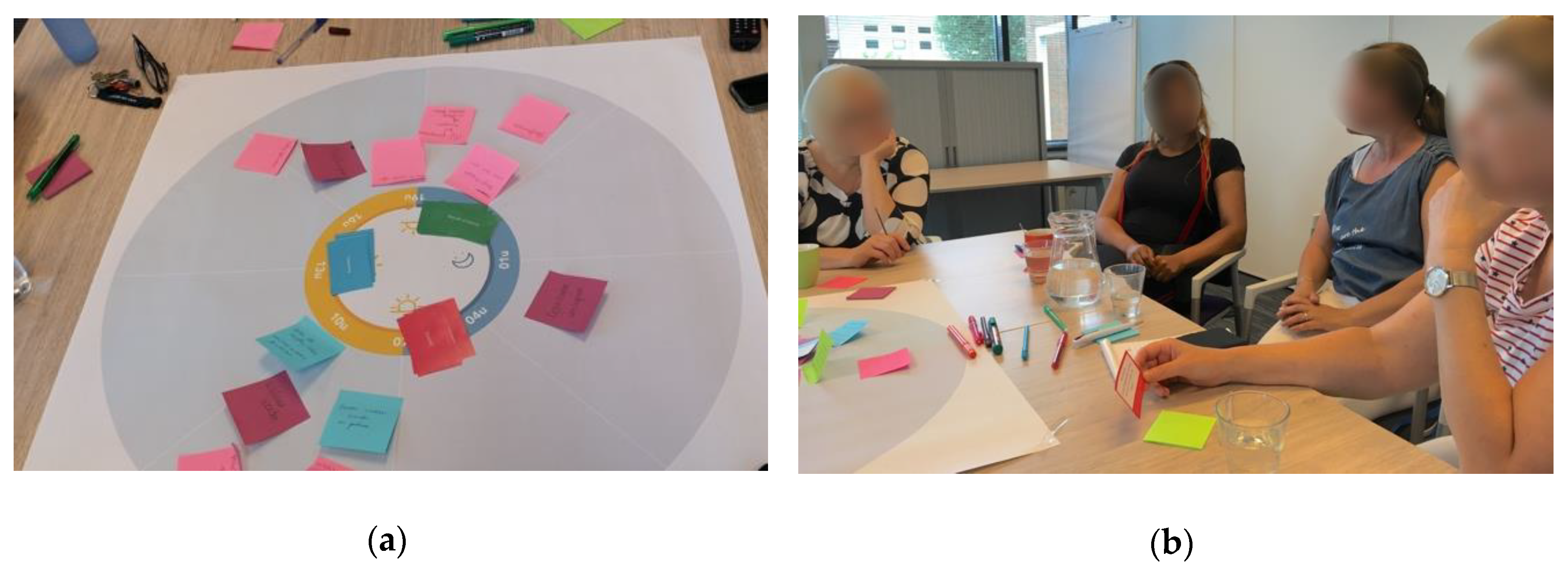
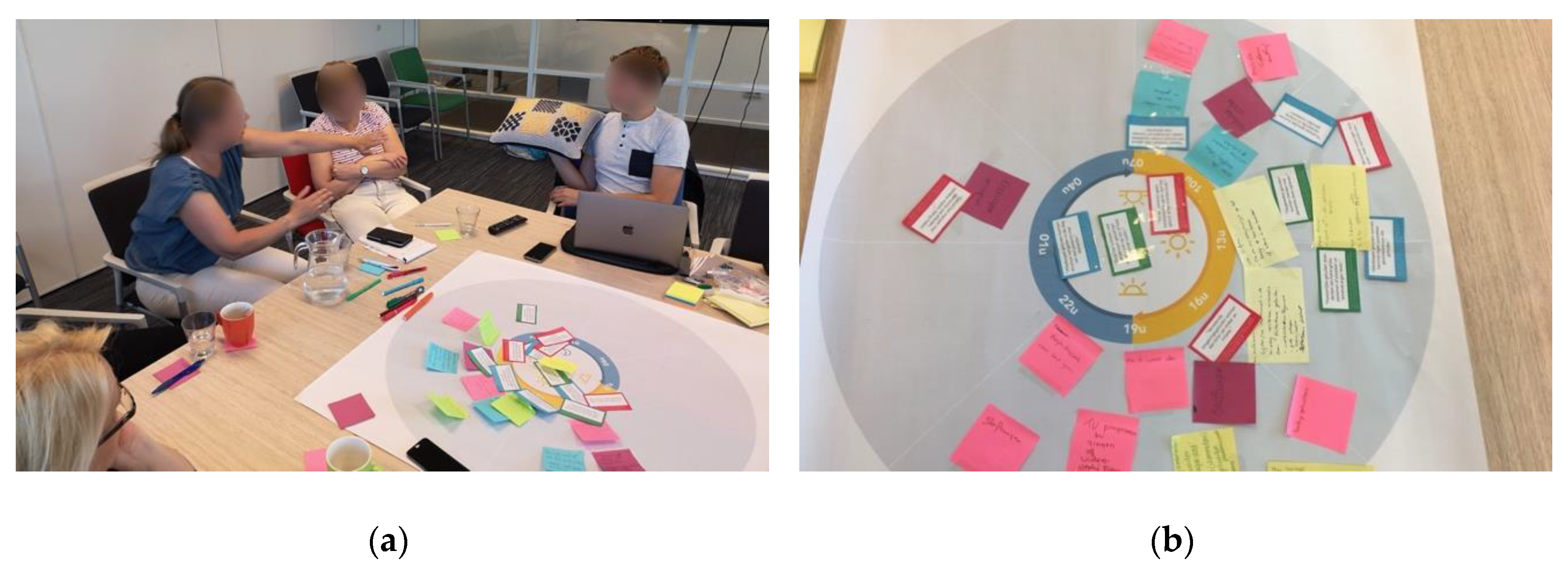
2.2. Workshop Procedure
2.2.1. Step 1: Mapping Everyday Activities in Care
2.2.2. Step 2: Relating Research to Everyday Care Activities
2.2.3. Step 3: Designing Scenarios for Audio-Based Technology
2.3. Participants and Setting
2.4. Data Analysis
2.5. Ethics
3. Results
- the added value of ABT in the residential dementia care process as ABT can provide rest and relieve from stress during the transition between activities, can initiate social connection during everyday care tasks; and can relieve boredom by supporting daytime activities and situational social experiences in the care space and
- how the successful integration of ABT in residential care requires a person-centered approach adapted to activities and habits specific to a care unit or healthcare team and tailored to the residents’ needs and preferences by exploring their individual responses.
3.1. The Added Value of ABT in the Care Process
3.1.1. Relieve Moments of Stress and Boredom
“Her son always comes to visit on the weekends, but at some point, she becomes very restless when he is not there yet. Maybe a message [from her son] saying “see you mom, see you later” can help here”.(C9)
“Because, sometimes [I] walk into a living area, and then I think, ‘why is the TV on now?’—sometimes just on a children’s channel—and then there is a lot of sound! But, no one is watching, and the [terrible] things that are on TV … (sighs)”(C13)
3.1.2. Facilitating Playful and Engaging Daytime Activities
“Yes this is very personal, but I had quite a burnout myself, and when I had to come back to work for the first time, I was also very anxious because, over here, a resident was having a pedicure [and], over there, six people were wandering. The doors [to the hallway] were open. Someone had turned on the television because that is cozy, and there I was standing behind the counter as a frightened person thinking ‘what is going on here?’”(C16)
“I have someone who, uhm, when I always turn on the radio with jazz and blues, […] she immediately starts dancing then, and that reminds her of her past too”.(C1)
3.1.3. Support Social Interaction in the Care Process
“That can be related to hobbies or something—or to work—or baby sounds if you happen to have worked in child care […] when you have one-on-one conversations about their work, hobbies, or past, then you also come across those sounds”.(C15)
“With physical care, which is quite stressful or difficult for several people and annoying, music can certainly help. […] I often sing songs with the people while providing morning care because, then, you can get a lot more done. I make a song from the activity or task that I am doing at that moment, especially with people in the advanced phases, so you can still try to make some contact. […] The morning care of one of the residents is becoming increasingly difficult for her and us. [We could] accompany it with soft and friendly piano music, because she is very interested in that, to start the day off right”.(C15)
“Hearing is the last [sense] to disappear. […] You often see people whose dementia has progressed [being] involved in those activities [with sound] and they still respond by opening their eyes, but they can no longer speak. […] The hearing remains!”.(C2)
3.2. Need for a Person-Centered and Reflexive Approach
3.2.1. Person-Centered Approach
“Oh, I always put the radio on: when I get up, when I take a shower, sing[ing] along in the shower. Yes, I also think it depends on the culture too. There were always many people in my house, it was always busy, and I am not used to silence at all”.(C12)
C14: “Yes, sometimes, I just do not want any sounds at all. I do not have to have sound around me all day—or music”.
C12: “Oh, but I do, I prefer music all day long!”
C13: “Yes, but then, suppose that you two are sitting in one communal area room? That is the same with that television and radio [that is always on]!”
C16: “A world of difference between your home and ours, you cannot imagine it!”
C17: “Yes, with us, it just helps at breakfast to turn on music, to make them eat. That makes a huge difference!”
C15: “Yes, I find that so contradictory. That is not possible with us because, during dinner, you do not have music on, you sit at the table, eat with the people, [and] possibly talk, but you have no music in the background”.
3.2.2. Reflexivity and Continuous Assessment
“We try something with a resident, and today, it is going well and, tomorrow, it is not. The day after tomorrow, it works again, and after three weeks, it stops. There is nothing more variable than a person with dementia, and the group dynamics also change, depending on who of the caregivers is working. [There are] quite a lot of factors you cannot do much about”.(C15)
“I am curious how the residents [will] react to the pillow when they are restless or when they are just relaxed and at rest, if they then react differently”.(C3)
4. Discussion
4.1. Novel Opportunities for Integrating ABT in Residential Dementia Care
4.2. The Needs and Lived Experiences of Care Professionals
4.3. Grounded Motivation for Future Field Studies
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Prince, M.; Ali, G.-C.; Guerchet, M.; Prina, A.M.; Albanese, E.; Wu, Y.-T. Recent global trends in the prevalence and incidence of dementia, and survival with dementia. Alzheimer’s Res. Ther. 2016, 8, 23. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Disease Facts and Figures. Available online: https://www.alz.org/media/documents/alzheimers-facts-and-figures-2019-r.pdf (accessed on 25 July 2020).
- Olazaran, J.; Reisberg, B.; Clare, L.; Cruz, I.; Peña-Casanova, J.; Del Ser, T.; Woods, R.T.; Beck, C.; Auer, S.R.; Lai, C.K.Y.; et al. Nonpharmacological Therapies in Alzheimer’s Disease: A Systematic Review of Efficacy. Dement. Geriatr. Cogn. Disord. 2010, 30, 161–178. [Google Scholar] [CrossRef]
- Baird, A.; Samson, S. Music and dementia. In Progress in Brain Research; Elsevier BV: Amsterdam, The Netherlands, 2015; Volume 217, pp. 207–235. [Google Scholar]
- Gold, K. But does it do any good? Measuring the impact of music therapy on people with advanced dementia: (Innovative practice). Dementia 2013, 13, 258–264. [Google Scholar] [CrossRef]
- Raglio, A.; Filippi, S.; Bellandi, D.; Stramba-Badiale, M. Global music approach to persons with dementia: Evidence and practice. Clin. Interv. Aging 2014, 9, 1669–1676. [Google Scholar] [CrossRef] [PubMed]
- Morrissey, K.; Wood, G.; Green, D.; Pantidi, N.; McCarthy, J. ‘I’m a rambler, I’m a gambler, I’m a long way from home’: The Place of Props, Music, and Design in Dementia Care. In Proceedings of the 2016 ACM Conference on Designing Interactive Systems—DIS’16, Brisbane, Australia, 4–8 June 2016; pp. 1008–1020. [Google Scholar]
- Ihara, E.S.; Tompkins, C.J.; Inoue, M.; Sonneman, S. Results from a person-centered music intervention for individuals living with dementia. Geriatr. Gerontol. Int. 2018, 19, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Götell, E.; Brown, S.; Ekman, S.-L. The influence of caregiver singing and background music on vocally expressed emotions and moods in dementia care. Int. J. Nurs. Studies 2009, 46, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Baird, A.; Samson, S. Memory for Music in Alzheimer’s Disease: Unforgettable? Neuropsychol. Rev. 2009, 19, 85–101. [Google Scholar] [CrossRef]
- Lazar, A.; Thompson, H.; Demiris, G. A systematic review of the use of technology for reminiscence therapy. Health Educ. Behav. 2014, 41, 51S–61S. [Google Scholar] [CrossRef]
- Simmons-Stern, N.R.; Deason, R.G.; Brandler, B.J.; Frustace, B.S.; O’Connor, M.K.; Ally, B.A.; Budson, A.E. Music-based memory enhancement in Alzheimer’s disease: Promise and limitations. Neuropsychologia 2012, 50, 3295–3303. [Google Scholar] [CrossRef]
- Baird, A.; Thompson, W.F. The Impact of Music on the Self in Dementia. J. Alzheimer’s Dis. 2018, 61, 827–841. [Google Scholar] [CrossRef]
- Graham, M.E. Re-socialising sound: Investigating sound, selfhood and intersubjectivity among people living with dementia in long-term care. Sound Studies 2018, 5, 175–190. [Google Scholar] [CrossRef]
- Lesaffre, M.; Moens, B.; Desmet, F. Monitoring Music and Movement Interaction in People with Dementia. In The Routledge Companion to Embodied Music Interaction; Informa UK Limited: London, UK, 2017; pp. 294–303. [Google Scholar]
- Unbehaun, D.; Taugerbeck, S.; Aal, K.; Vaziri, D.D.; Lehmann, J.; Tolmie, P.; Wieching, R.; Wulf, V. Notes of memories: Fostering social interaction, activity and reminiscence through an interactive music exergame developed for people with dementia and their caregivers. Hum.-Comput. Interact. 2020, 1–34. [Google Scholar] [CrossRef]
- Favilla, S.; Pedell, S. Touch screen ensemble music. In Proceedings of the 25th Australian Computer-Human Interaction Conference, Association for Computing Machinery (ACM), Adelaide, Australia, 25–29 November 2013; pp. 481–484. [Google Scholar]
- Frohlich, D.M.; Corrigan-Kavanagh, E.; Campbell, S.; Chrysanthaki, T.; Castro, P.; Zaine, I.; da Graça Campos Pimentel, M. Assistive Media for Well-being. In HCI and Design in the Context of Dementia; Brankaert , R., Kenning, G., Eds.; Human–Computer Interaction Series; Springer: Cham, Switzerland, 2020; pp. 189–205. [Google Scholar] [CrossRef]
- Houben, M.; Brankaert, R.; Bakker, S.; Kenning, G.; Bongers, I.; Eggen, B. Foregrounding Everyday Sounds in Dementia. In Proceedings of the 2019 on Designing Interactive Systems Conference, Association for Computing Machinery (ACM), San Diego, CA, USA, 23–28 June 2019; pp. 71–83. [Google Scholar]
- Campbell, S.; Frohlich, D.; Alm, N.; Vaughan, A. Sentimental Audio Memories: Exploring the Emotion and Meaning of Everyday Sounds. In Dementia Lab 2019. Making Design Work: Engaging with Dementia in Context. D-Lab 2019. Communications in Computer and Information Science; Brankaert, R., IJsselsteijn , W., Eds.; Springer: Cham, Switzerland, 2019; Volume 1117, pp. 73–81. [Google Scholar] [CrossRef]
- Luyten, T.; Braun, S.; Van Hooren, S.; De Witte, L. How groups of nursing home residents respond to “the CRDL”: A pilot study. J. Enabling Technol. 2018, 12, 145–154. [Google Scholar] [CrossRef]
- Houben, M.; Brankaert, R.; Bakker, S.; Kenning, G.; Bongers, I.; Eggen, B. The Role of Everyday Sounds in Advanced Dementia Care. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020; Volume 450, pp. 1–14. [Google Scholar]
- Graham, M.E. Long-term care as contested acoustical space: Exploring resident relationships and identities in sound. Build. Acoust. 2019, 27, 61–73. [Google Scholar] [CrossRef]
- Andringa, T.C.; Lanser, J.J.L. How Pleasant Sounds Promote and Annoying Sounds Impede Health: A Cognitive Approach. Int. J. Environ. Res. Public Health 2013, 10, 1439–1461. [Google Scholar] [CrossRef] [PubMed]
- Bosch, K.A.V.D.; Andringa, T.C.; Peterson, W.; Ruijssenaars, W.A.J.J.M.; Vlaskamp, C. A comparison of natural and non-natural soundscapes on people with severe or profound intellectual and multiple disabilities. J. Intellect. Dev. Disabil. 2016, 42, 301–307. [Google Scholar] [CrossRef]
- Andringa, T.C.; van den Bosch, K.A. Core affect and soundscape assessment: Fore-and background soundscape design for quality of life. In Proceedings of the 42nd International Congress and Exposition on Noise Control Engineering 2013: INTER-NOISE 2013: Noise Control for Quality of Life, Innsbruck, Australia, 15–18 September 2013; pp. 2273–2282. [Google Scholar]
- Bulsara, C.; Seaman, K.; Steuxner, S. Using sound therapy to ease agitation amongst persons with dementia: A pilot study. Aust. Nurs. Midwifery J. 2016, 23, 38–39. [Google Scholar]
- Devos, P.; Aletta, F.; Thomas, P.; Petrovic, M.; Mynsbrugge, T.V.; Van De Velde, D.; De Vriendt, P.; Botteldooren, D. Designing Supportive Soundscapes for Nursing Home Residents with Dementia. Int. J. Environ. Res. Public Health 2019, 16, 4904. [Google Scholar] [CrossRef]
- Lund, H.N.; Bertelsen, L.R.; Bonde, L.O. Sound and music interventions in psychiatry at Aalborg University Hospital. SoundEffects-Interdiscip. J. Sound Sound Exp. 2016, 6, 48–68. [Google Scholar] [CrossRef]
- Hayne, M.J.; Fleming, R. Acoustic design guidelines for dementia care facilities. In Proceedings of the 43rd International Congress on Noise Control Engineering: Internoise 2014, Melbourne, Australia, 16–19 November 2014; pp. 1–10. [Google Scholar]
- Devos, P.; Aletta, F.; Thomas, P.; Filipan, K.; Petrovic, M.; Botteldooren, D.; Vander Mynsbrugge, T.; Van de Velde, D.; De Vriendt, P. Soundscape design for management of behavioral disorders: A pilot study among nursing home residents with dementia. In Proceedings of the Impact of Noise Control Engineering: Proceedings of Inter-Noise 2018, Chicago, IL, USA, 26–29 August 2018; p. 8. [Google Scholar]
- Craig, C.; Killick, J. Creativity and Communication in Persons with Dementia: A Practical Guide; Jessica Kingsley Publishers: London, UK, 2011. [Google Scholar]
- Chancellor, B.; Duncan, A.; Chatterjee, A. Art Therapy for Alzheimer’s Disease and Other Dementias. J. Alzheimer’s Dis. 2014, 39, 1–11. [Google Scholar] [CrossRef]
- Thoolen, M.; Brankaert, R.; Lu, Y. Sentic: A Tailored Interface Design for People with Dementia to Access Music. In The Companion Publication of the 2019 on Designing Interactive Systems Conference, Proceedings of the 2019 Companion—DIS’19 Companion; ACM Press: New York, NY, USA, 2019; pp. 57–60. [Google Scholar]
- Müller-Rakow, A.; Flechtner, R. Designing Interactive Music Systems with and for People with Dementia. Des. J. 2017, 20, S2207–S2214. [Google Scholar] [CrossRef][Green Version]
- Morrissey, K.; McCarthy, J. Creative and Opportunistic Use of Everyday Music Technologies in a Dementia Care Unit. In Proceedings of the 2015 ACM SIGCHI Conference on Creativity and Cognition, C&C’15, Glasgow, UK, 22–25 June 2015; pp. 295–298. [Google Scholar]
- Crowe, B.J.; Rio, R. Implications of Technology in Music Therapy Practice and Research for Music Therapy Education: A Review of Literature. J. Music. Ther. 2004, 41, 282–320. [Google Scholar] [CrossRef] [PubMed]
- Kenning, G.; Ilsar, A.; Brankaert, R.; Evans, M. Improvisation and Reciprocal Design: Soundplay for Dementia. In Dementia Lab 2019. Making Design Work: Engaging with Dementia in Context. D-Lab 2019. Communications in Computer and Information Science; Brankaert, R., IJsselsteijn , W., Eds.; Springer: Cham, Switzerland, 2019; Volume 1117, pp. 82–91. [Google Scholar] [CrossRef]
- Houben, M.; Lehn, B.; van den Brink, N.; Diks, S.; Verhoef, J.; Brankaert, R. Turnaround: Exploring Care Relations in Dementia Through Design. In Proceedings of the Extended Abstracts of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020. [Google Scholar]
- Bosch, K.A.V.D.; Andringa, T.C.; Baskent, D.; Vlaskamp, C. The Role of Sound in Residential Facilities for People with Profound Intellectual and Multiple Disabilities. J. Policy Pr. Intellect. Disabil. 2016, 13, 61–68. [Google Scholar] [CrossRef]
- Koumakis, L.; Chatzaki, C.; Kazantzaki, E.; Maniadi, E.; Tsiknakis, M. Dementia Care Frameworks and Assistive Technologies for Their Implementation: A Review. IEEE Rev. Biomed. Eng. 2019, 12, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Lourida, I.; A Abbott, R.; Rogers, M.; Lang, I.A.; Stein, K.; Kent, B.; Coon, J.T. Dissemination and implementation research in dementia care: A systematic scoping review and evidence map. BMC Geriatr. 2017, 17, 147. [Google Scholar] [CrossRef] [PubMed]
- Spinuzzi, C. The methodology of participatory design. Tech. Commun. 2005, 52, 163–174. [Google Scholar]
- Yoo, D. Stakeholder Tokens: A constructive method for value sensitive design stakeholder analysis. Ethic-Inf. Technol. 2018, 1–5. [Google Scholar] [CrossRef]
- Ward, M.E.; De Brún, A.; Beirne, D.; Conway, C.; Cunningham, U.; English, A.; Fitzsimons, J.; Furlong, E.P.; Kane, Y.; Kelly, A.; et al. Using Co-Design to Develop a Collective Leadership Intervention for Healthcare Teams to Improve Safety Culture. Int. J. Environ. Res. Public Health 2018, 15, 1182. [Google Scholar] [CrossRef]
- Galway, K.; Forbes, T.; Mallon, S.; Santin, O.; Best, P.; Neff, J.; Leavey, G.; Pitman, A. Adapting Digital Social Prescribing for Suicide Bereavement Support: The Findings of a Consultation Exercise to Explore the Acceptability of Implementing Digital Social Prescribing within an Existing Postvention Service. Int. J. Environ. Res. Public Health 2019, 16, 4561. [Google Scholar] [CrossRef]
- Berry, A.B.; Lim, C.; Hartzler, A.L.; Hirsch, T.; Ludman, E.J.; Wagner, E.H.; Ralston, J.D. Creating Conditions for Patients’ Values to Emerge in Clinical Conversations. In Proceedings of the 2017 Conference on Interaction Design and Children-IDC’17, Stanford, CA, USA, 27–30 June 2017; Volume 2017, pp. 1165–1174. [Google Scholar]
- Sanders, E.B.-N.; Stappers, P.J. Co-creation and the new landscapes of design. CoDesign 2008, 4, 5–18. [Google Scholar] [CrossRef]
- Buskermolen, D.O.; Terken, J. Co-constructing stories. In Proceedings of the 12th Participatory Design Conference, Roskildem, Denmark, 12–16 August 2012; Volume 2, p. 33. [Google Scholar]
- Visser, F.S.; Stappers, P.J.; Van Der Lugt, R.; Sanders, E.B.-N. Contextmapping: Experiences from practice. CoDesign 2005, 1, 119–149. [Google Scholar] [CrossRef]
- Kankainen, A.; Vaajakallio, K.; Kantola, V.; Mattelmäki, T. Storytelling Group—A co-design method for service design. Behav. Inf. Technol. 2012, 31, 221–230. [Google Scholar] [CrossRef]
- Schelle, K.J.; Gomez Naranjo, C.; ten Bhömer, M.; Tomico, O.; Wensveen, S. Tactile Dialogues: Personalization of Vibrotactile Behavior to Trigger Interpersonal Communication. In Proceedings of the Ninth International Conference on Tangible, Embedded, and Embodied Interaction-TEI’14, Stanford, CA, USA, 15–19 January 2015; pp. 637–642. [Google Scholar]
- Ijsselsteijn, W.; Tummers-Heemels, A.; Brankaert, R. Warm Technology: A Novel Perspective on Design for and with People Living with Dementia. In HCI and Design in the Context of Dementia; Brankaert , R., Kenning, G., Eds.; Human–Computer Interaction Series; Springer: Cham, Switzerland, 2020; pp. 33–47. [Google Scholar] [CrossRef]
- Halskov, K.; Dalsgård, P. Inspiration card workshops. In Proceedings of the 6th ACM Conference on Electronic Commerce—EC’05, Vancouver, BC, Canada, 5–8 June 2006; p. 2. [Google Scholar]
- Gaver, W.W. How Do We Hear in the World? Explorations in Ecological Acoustics. Ecol. Psychol. 1993, 5, 285–313. [Google Scholar] [CrossRef]
- Aletta, F.; Mynsbrugge, T.V.; Van De Velde, D.; De Vriendt, P.; Thomas, P.; Filipan, K.; Botteldooren, D.; Devos, P. Awareness of ‘sound’ in nursing homes: A large-scale soundscape survey in Flanders (Belgium). Build. Acoust. 2017, 25, 43–59. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Campbell, P.S. Music, the universal language: Fact or fallacy? Int. J. Music. Educ. 1997, 32–39. [Google Scholar] [CrossRef]
- Miller, E.; Devlin, N.; Buys, L.; Donoghue, G. The happiness initiative: Changing organizational culture to make ‘brilliance’ mainstream in aged care. J. Manag. Organ. 2019, 26, 296–308. [Google Scholar] [CrossRef]
- De Groot, W.; Houben, M.; Hengeveld, B. Exploring How an Interactive Placemat Can Influence Eating Activities for People with Dementia BT—Dementia Lab 2019. Making Design Work: Engaging with Dementia in Context; Brankaert, R., IJsselsteijn, W., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 92–100. [Google Scholar]
- Devos, P.; Aletta, F.; Thomas, P.; Mynsbrugge, T.V.; Petrovic, M.; Van De Velde, D.; De Vriendt, P.; Botteldooren, D. Application of a Prediction Model for Ambient Noise Levels and Acoustical Capacity for Living Rooms in Nursing Homes Hosting Older People with Dementia. Appl. Sci. 2020, 10, 4205. [Google Scholar] [CrossRef]
- Lundgaard, S.S.; Nielsen, P.A. Personalised Soundscapes in Homes. In Proceedings of the 2019 on Designing Interactive Systems Conference, Association for Computing Machinery (ACM), San Diego, CA, USA, 23–28 June 2019; pp. 813–822. [Google Scholar] [CrossRef]
- Dixon, E.; Lazar, A. Approach Matters: Linking Practitioner Approaches to Technology Design for People with Dementia. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020; pp. 1–15. [Google Scholar]
- Unbehaun, D.; Aal, K.; Vaziri, D.D.; Tolmie, P.D.; Wieching, R.; Randall, D.; Wulf, V. Social Technology Appropriation in Dementia: Investigating the Role of Caregivers in Engaging People with Dementia with a Videogame-Based Training System. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020. [Google Scholar]
- Bannigan, K.; Moores, A. A Model of Professional Thinking: Integrating Reflective Practice and Evidence Based Practice. Can. J. Occup. Ther. 2009, 76, 342–350. [Google Scholar] [CrossRef]
- Mann, K.; Gordon, J.; MacLeod, A. Reflection and reflective practice in health professions education: A systematic review. Adv. Health Sci. Educ. 2007, 14, 595. [Google Scholar] [CrossRef]
- Ossebaard, H.C.; Van Gemert-Pijnen, L. eHealth and quality in health care: Implementation time. Int. J. Qual. Health Care 2016, 28, 415–419. [Google Scholar] [CrossRef]
- Karabi, C.B.; Darla, P.; Jason, S. Management attitudes and technology adoption in long-term care facilities. J. Health Organ. Manag. 2014, 28, 344–365. [Google Scholar]
- Brankaert, R.; Ouden, E.D.; Brombacher, A. Innovate dementia: The development of a living lab protocol to evaluate interventions in context. Info 2015, 17, 40–52. [Google Scholar] [CrossRef]
- Müller, C.; Neufeldt, C.; Randall, D.; Wulf, V. ICT-development in residential care settings. In Proceedings of the 2012 ACM Annual Conference, Cambridge, UK, 11–14 November 2012; p. 2639. [Google Scholar]

| Category | Statements from Literature | Ref. |
|---|---|---|
| Red cards: potential nuisance of sound in a care environment. |
| [55] |
| [30] | |
| [29] | |
| [56] | |
| Blue cards: application areas of ABT. |
| [30] |
| [21] | |
| [40] | |
| [19] | |
| Green cards: emotional and behavioral responses to sound. |
| [27] |
| [14] | |
| [24] | |
| [28] |
| Care Facility A | Care Facility B | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 | Session 2 | Session 3 | |||||||||||||||
| C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | C10 | C11 | C12 | C13 | C14 | C15 | C16 | C17 | C18 |
| A | N | A | N | A | A | A | A | N | N | N | N | A | A | N | N | N | A |
| f | f | f | f | f | f | f | f | f | f | f | f | f | f | f | f | f | m |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Houben, M.; Brankaert, R.; Kenning, G.; Eggen, B.; Bongers, I. The Perspectives of Professional Caregivers on Implementing Audio-Based Technology in Residential Dementia Care. Int. J. Environ. Res. Public Health 2020, 17, 6333. https://doi.org/10.3390/ijerph17176333
Houben M, Brankaert R, Kenning G, Eggen B, Bongers I. The Perspectives of Professional Caregivers on Implementing Audio-Based Technology in Residential Dementia Care. International Journal of Environmental Research and Public Health. 2020; 17(17):6333. https://doi.org/10.3390/ijerph17176333
Chicago/Turabian StyleHouben, Maarten, Rens Brankaert, Gail Kenning, Berry Eggen, and Inge Bongers. 2020. "The Perspectives of Professional Caregivers on Implementing Audio-Based Technology in Residential Dementia Care" International Journal of Environmental Research and Public Health 17, no. 17: 6333. https://doi.org/10.3390/ijerph17176333
APA StyleHouben, M., Brankaert, R., Kenning, G., Eggen, B., & Bongers, I. (2020). The Perspectives of Professional Caregivers on Implementing Audio-Based Technology in Residential Dementia Care. International Journal of Environmental Research and Public Health, 17(17), 6333. https://doi.org/10.3390/ijerph17176333






