Medical Characteristics of Foreign Language Patients in Paramedic Care
Abstract
1. Introduction
2. Materials and Methods
3. Results
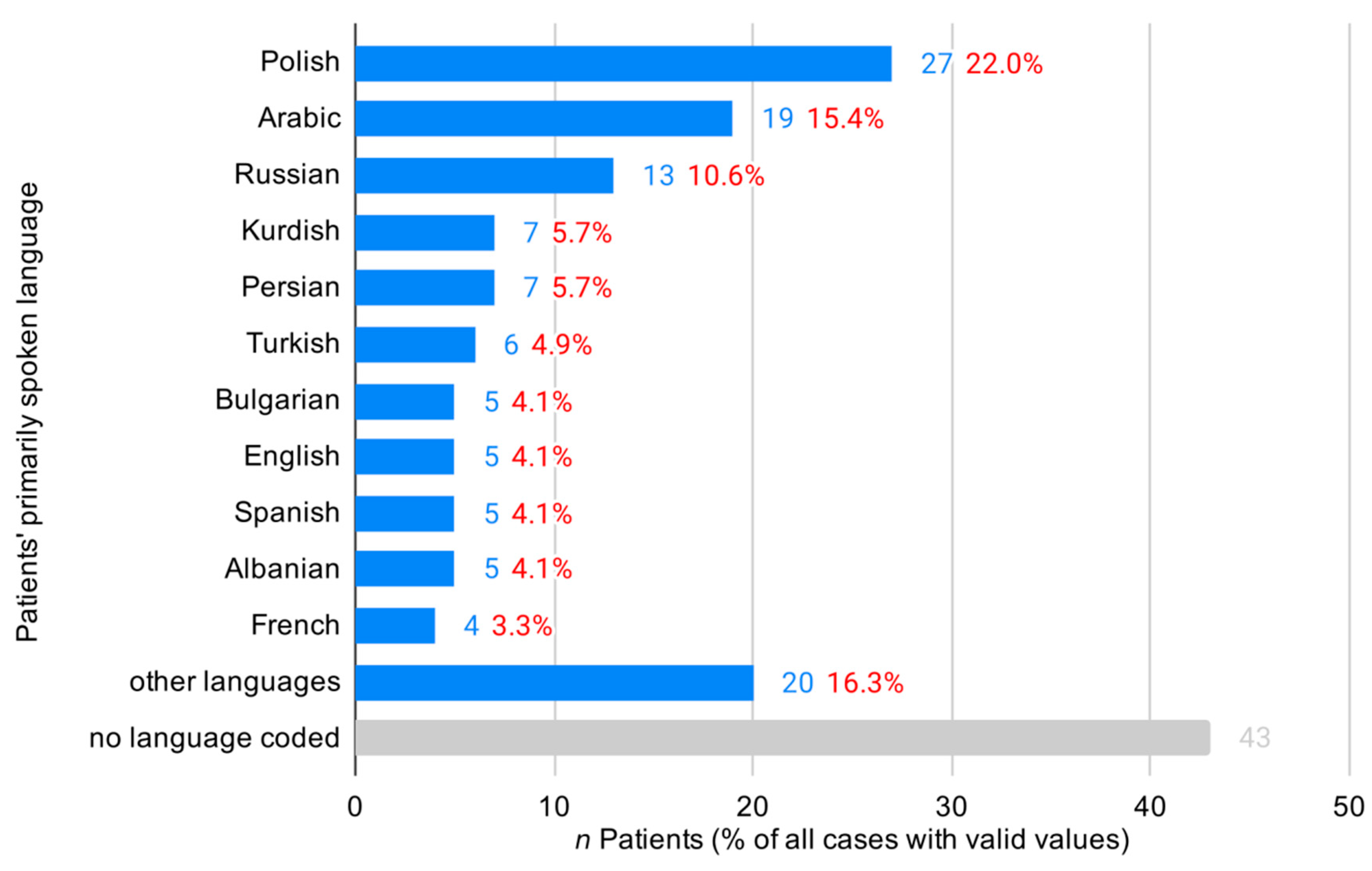
EMS Operations with Patients with Limited German Language Proficiency
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- German Federal Office for Migration and Refugees. The Federal Office in Figures 2019 [Das Bundesamt in Zahlen 2019]. Available online: https://www.bamf.de/SharedDocs/Anlagen/DE/Statistik/BundesamtinZahlen/bundesamt-in-zahlen-2019-asyl.pdf (accessed on 29 August 2020).
- UNHCR. UNHCR Population Statistics. Available online: http://popstats.unhcr.org/en/overview (accessed on 4 May 2020).
- German Federal Statistical Office. Tourism in Numbers 2017 [Tourismus in Zahlen]. Table 3.2. 2018. Available online: https://www.destatis.de/DE/Publikationen/Thematisch/BinnenhandelGastgewerbeTouris-mus/Tourismus/TourismusinZahlen1021500177005.xlsx?__blob=publicationFile (accessed on 20 March 2019).
- Günther, A.; Piest, B.; Herrmann, I.; Schulte, R.; Buhr-Riehm, R.; Siems, K.; Konstantin, K. Medical care in a reception facility for asylum seekers: The frequency of rescue service operations. Notarzt 2016, 32, 6–8. [Google Scholar] [CrossRef][Green Version]
- Meischke, H.; Chavez, D.; Bradley, S.; Rea, T.; Eisenberg, M. Emergency communications with limited-English-proficiency populations. Prehosp. Emerg. Care 2010, 14, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Yip, M.P.; Ong, B.N.; Meischke, H.W.; Feng, S.X.; Calhoun, R.; Painter, I.; Tu, S.-P. The role of self-efficacy in communication and emergency response in Chinese limited English proficiency (LEP) populations. Health Promot. Pract. 2013, 14, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Ong, B.N.; Yip, M.P.; Feng, S.; Calhoun, R.; Meischke, H.W.; Tu, S.-P. Barriers and facilitators to using 9-1-1 and emergency medical services in a limited English proficiency Chinese community. J. Immigr. Minor. Health 2012, 14, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Yip, M.-P.; Calhoun, R.E.; Painter, I.S.; Meischke, H.W.; Tu, S.-P. Emergency communications within the limited English proficient Chinese community. J. Immigr. Minor. Health 2014, 16, 769–771. [Google Scholar] [CrossRef] [PubMed]
- Watts, J.; Cowden, J.D.; Cupertino, A.P.; Dowd, M.D.; Kennedy, C. 911 (nueve once): Spanish-speaking parents’ perspectives on prehospital emergency care for children. J. Immigr. Minor. Health 2011, 13, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Grow, R.W.; Sztajnkrycer, M.D.; Moore, B.R. Language barriers as a reported cause of prehospital care delay in Minnesota. Prehosp. Emerg. Care 2008, 12, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Meischke, H.W.; Calhoun, R.E.; Yip, M.-P.; Tu, S.-P.; Painter, I.S. The effect of language barriers on dispatching EMS response. Prehosp. Emerg. Care 2013, 17, 475–480. [Google Scholar] [CrossRef] [PubMed]
- Tate, R.C.; Hodkinson, P.W.; Meehan-Coussee, K.; Cooperstein, N. Strategies Used by Prehospital Providers to Overcome Language Barriers. Prehosp. Emerg. Care 2016, 20, 404–414. [Google Scholar] [CrossRef] [PubMed]
- Tate, R.C. The Need for More Prehospital Research on Language Barriers: A Narrative Review. West. J. Emerg. Med. 2015, 16, 1094–1105. [Google Scholar] [CrossRef] [PubMed]
- Noack, E.M.; Kleinert, E.; Müller, F. Overcoming language barriers in paramedic care: A study protocol of the interventional trial ‘DICTUM rescue’ evaluating an app designed to improve communication between paramedics and foreign-language patients. BMC Health Serv. Res. 2020, 20, 223. [Google Scholar] [CrossRef] [PubMed]
- Altıner, A.O.; Yeşil, S.T. Emergency Medical Service (EMS) Utilization by Syrian Refugees Residing in Ankara, Turkey. Prehosp. Disaster Med. 2018, 33, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Weiss, N.R.; Weiss, S.J.; Tate, R.; Oglesbee, S.; Ernst, A.A. Language disparities in patients transported by emergency medical services. Am. J. Emerg. Med. 2015, 33, 1737–1741. [Google Scholar] [CrossRef] [PubMed]
- Sterling, M.R.; Echeverria, S.E.; Merlin, M.A. The Effect of Language Congruency on the Out-of-Hospital Management of Chest Pain. World Med. Health Policy 2013, 5, 111–123. [Google Scholar] [CrossRef]
- Dopfer, C.; Vakilzadeh, A.; Happle, C.; Kleinert, E.; Müller, F.; Ernst, D.; Schmidt, R.E.; Behrens, G.M.N.; Merkesdal, S.; Wetzke, M.; et al. Pregnancy Related Health Care Needs in Refugees—A Current Three Center Experience in Europe. Int. J. Environ. Res. Public Health 2018, 15, 1934. [Google Scholar] [CrossRef] [PubMed]
- Nesterko, Y.; Jäckle, D.; Friedrich, M.; Holzapfel, L.; Glaesmer, H. Prevalence of post-traumatic stress disorder, depression and somatisation in recently arrived refugees in Germany: An epidemiological study. Epidemiol. Psychiatr. Sci. 2019, 29, e40. [Google Scholar] [CrossRef] [PubMed]
- Lindert, J.; von Ehrenstein, O.S.; Wehrwein, A.; Brähler, E.; Schäfer, I. Anxiety, Depression and Posttraumatic Stress Disorder in Refugees—A Systematic Review. Psychother. Psychosom. Med. Psychol. 2018, 68, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Kirmayer, L.J.; Narasiah, L.; Munoz, M.; Rashid, M.; Ryder, A.G.; Guzder, J.; Hassan, G.; Rousseau, C.; Pottie, K. Common mental health problems in immigrants and refugees: General approach in primary care. CMAJ 2011, 183, E959–E967. [Google Scholar] [CrossRef] [PubMed]


| Rescue Operations | Unit | All (n = 7494) | GSP (n = 7328) | LGP Patients (n = 166) | n Missing | p | |
|---|---|---|---|---|---|---|---|
| Sex | Male | n (%) | 3531 (52.0) | 3444 (51.9) | 87 (55.8) | 706 | 0.571 |
| Female | n (%) | 3246 (47.8) | 3177 (47.9) | 69 (44.2) | |||
| Other | n (%) | 11 (0.2) | 11 (0.2) | 0 (0.0) | |||
| Age | years; mean (SD) | 61.4 (24.8) | 61.9 (24.7) | 39.1 (20.6) | 532 | <0.001 | |
| Children (<18 years) | n (%) | 478 (6.4) | 458 (6.7) | 20 (12.4) | 532 | 0.005 | |
| Rescue Operations | Unit | All (n = 7494) | GSP (n = 7328) | LGP Patients (n = 166) | n Missing | p | P (Adjusted *) |
|---|---|---|---|---|---|---|---|
| Time en route (min) | Mean (SD) | 8.5 (4.9) | 8.5 (4.9) | 8.5 (4.7) | 893 | 0.908 | 0.816 |
| Median (IQR) | 7 (6) | 7 (6) | 8 (6) | ||||
| Time on scene (min) | Mean (SD) | 21.6 (12.2) | 21.7 (12.3) | 20.2 (10.3) | 1780 | 0.280 | 0.901 |
| Median (IQR) | 19 (13) | 19 (14) | 18.5 (13) | ||||
| Time to destination (min) | Mean (SD) | 15.9 (9.3) | 15.9 (9.4) | 16.0 (8.1) | 2121 | 0.426 | 0.983 |
| Median (IQR) | 15 (9) | 15 (9) | 17 (11) | ||||
| Dispatch at nighttime (20:00–07:00) | n (%) | 2527 (34.7) | 2469 (34.7) | 59 (36.2) | 219 | 0.692 | 0.992 |
| Emergency physician present | n (%) | 1830 (33.3) | 1798 (33.5) | 32 (26.7) | 1999 | 0.119 | 0.134 |
| Rural area | n (%) | 5168 (69.0) | 5052 (68.9) | 116 (69.9) | 0 | 0.796 | 0.601 |
| Patient rejected care | n (%) | 260 (3.5) | 257 (3.5) | 3 (1.8) | 0 | 0.237 | 0.105 |
| Rescue Operations | Unit | All (n = 7494) | GSP (n = 7328) | LGP Patients (n = 166) | n Missing | p | p (Adjusted *) | |
|---|---|---|---|---|---|---|---|---|
| Initial Assessment | ||||||||
| Glasgow Coma Scale (GCS) | Mean (SD) | 14.1 (2.6) | 14.1 (2.6) | 14.5 (2.1) | 597 | 0.012 | 0.176 | |
| NACA score # | Mean (SD) | 3.1 (1.3) | 3.1 (1.3) | 3.1 (1.2) | 4170 | 0.852 | 0.291 | |
| Psychiatric symptoms | n (%) | 789 (12.4) | 779 (12.5) | 10 (6.5) | 1128 | 0.034 | 0.519 | |
| Need for ventilation | n (%) | 102 (1.4) | 102 (1.4) | 0 (0.0) | 0 | 0.126 | 0.216 | |
| Preliminary Diagnosis | ||||||||
| Neurological disorders | n (%) | 729 (11.1) | 712 (11.1) | 17 (11.0) | 907 | 0.991 | 0.850 | |
| Cardiovascular disorders | n (%) | 1673 (25.4) | 1637 (25.4) | 36 (23.4) | 907 | 0.560 | 0.051 | |
| Respiratory disorders | n (%) | 592 (9.0) | 584 (9.1) | 8 (5.2) | 907 | 0.096 | 0.214 | |
| Metabolic disorders | n (%) | 427 (6.5) | 422 (6.6) | 5 (3.2) | 907 | 0.099 | 0.854 | |
| Psychiatric disorders | n (%) | 565 (8.6) | 546 (8.5) | 19 (13.0) | 907 | 0.048 | 0.871 | |
| Abdominal disorders | n (%) | 662 (10.1) | 646 (10.0) | 16 (10.4) | 907 | 0.887 | 0.646 | |
| Gynecological and obstetric disorders | n (%) | 79 (1.2) | 69 (1.1) | 10 (6.5) | 907 | <0.001 | <0.001 | |
| Other disorders | n (%) | 586 (8.9) | 573 (8.9) | 13 (8.4) | 907 | 0.841 | 0.868 | |
| Injuries | None | n (%) | 5902 (75.8) | 5767 (75.7) | 135 (81.2) | 907 | 0.117 | 0.007 |
| Slight | n (%) | 1037 (15.7) | 1014 (15.8) | 23 (14.9) | 907 | 0.781 | 0.153 | |
| moderate | n (%) | 493 (7.5) | 487 (7.6) | 6 (3.9) | 907 | 0.087 | 0.065 | |
| Severe | n (%) | 62 (0.9) | 62 (1.0) | 0 (0.0) | 907 | 0.505 | 0.157 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Müller, F.; Hummers, E.; Noack, E.M. Medical Characteristics of Foreign Language Patients in Paramedic Care. Int. J. Environ. Res. Public Health 2020, 17, 6306. https://doi.org/10.3390/ijerph17176306
Müller F, Hummers E, Noack EM. Medical Characteristics of Foreign Language Patients in Paramedic Care. International Journal of Environmental Research and Public Health. 2020; 17(17):6306. https://doi.org/10.3390/ijerph17176306
Chicago/Turabian StyleMüller, Frank, Eva Hummers, and Eva Maria Noack. 2020. "Medical Characteristics of Foreign Language Patients in Paramedic Care" International Journal of Environmental Research and Public Health 17, no. 17: 6306. https://doi.org/10.3390/ijerph17176306
APA StyleMüller, F., Hummers, E., & Noack, E. M. (2020). Medical Characteristics of Foreign Language Patients in Paramedic Care. International Journal of Environmental Research and Public Health, 17(17), 6306. https://doi.org/10.3390/ijerph17176306





