What Protective Health Measures Are Americans Taking in Response to COVID-19? Results from the COVID Impact Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Settings
2.2. Measurements
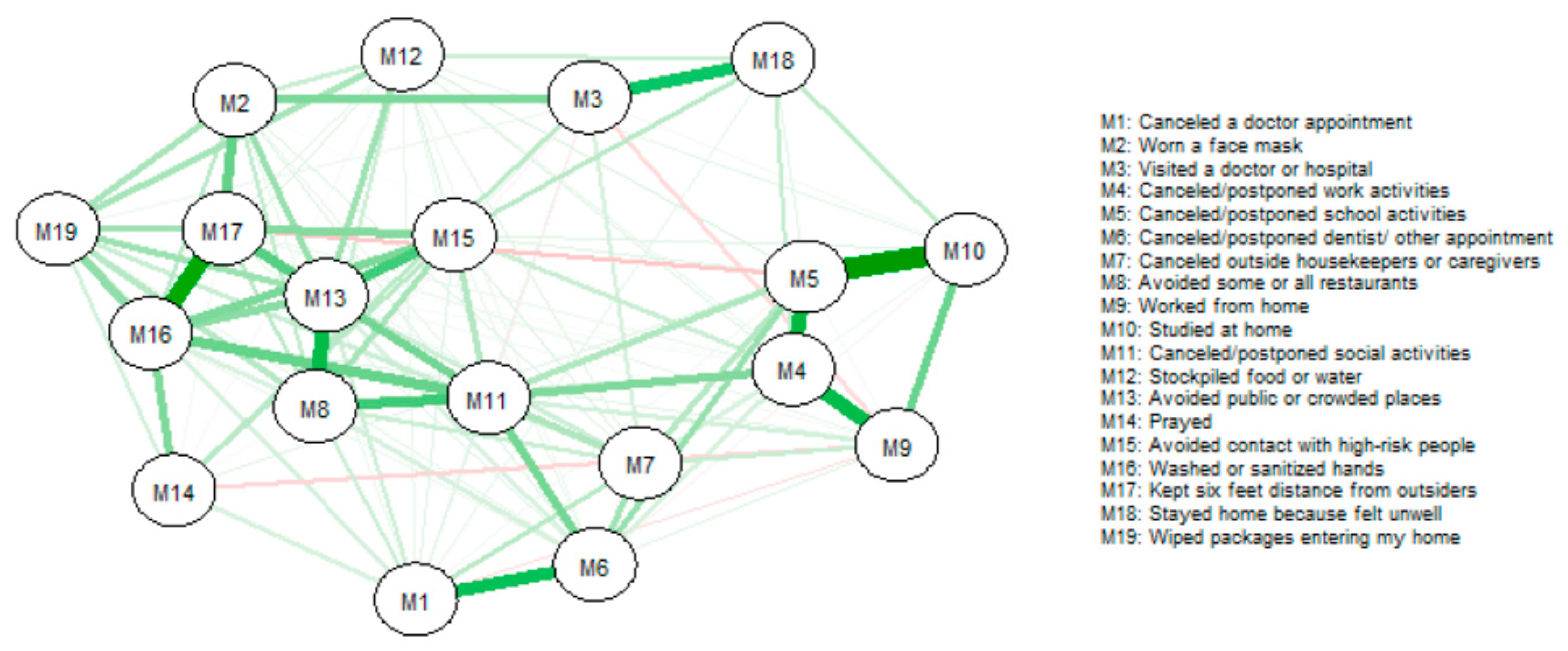
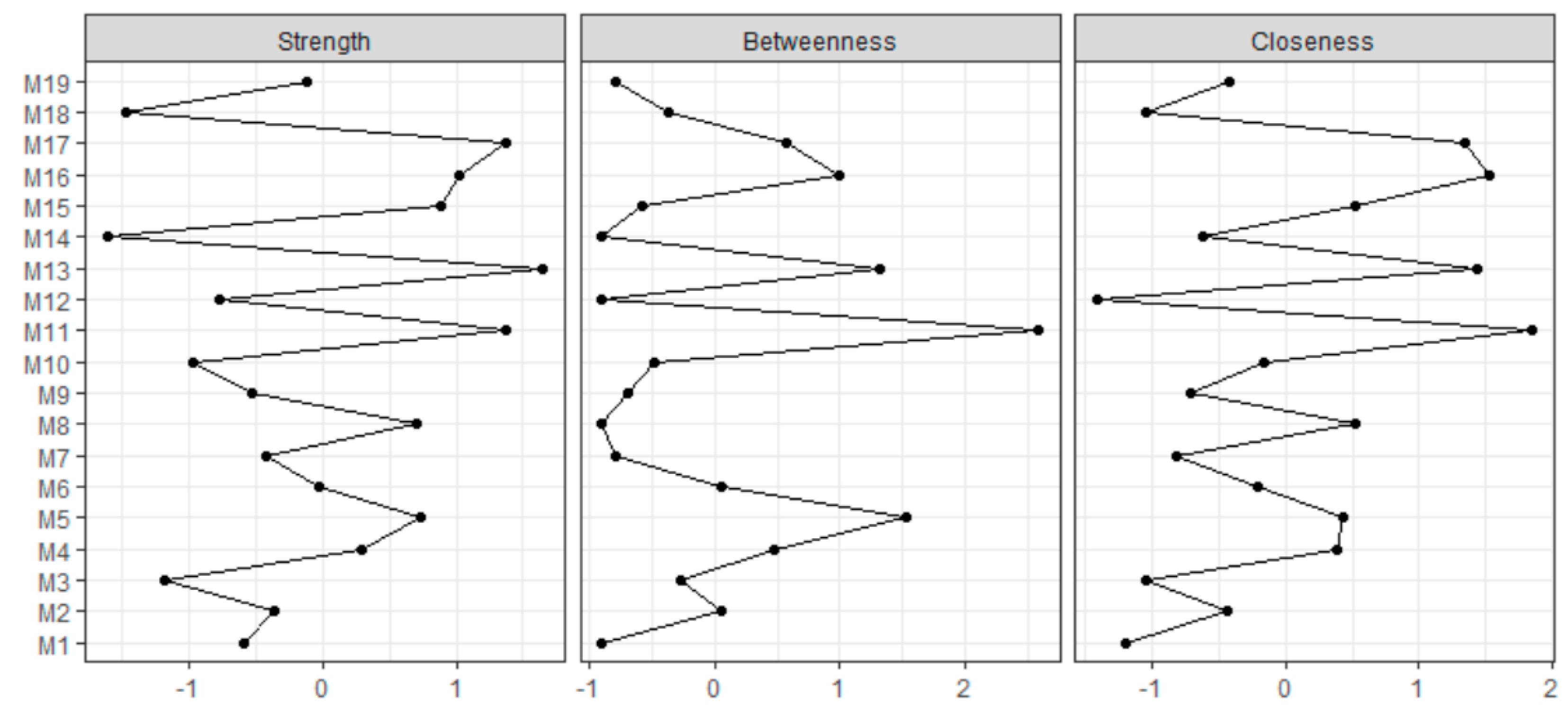
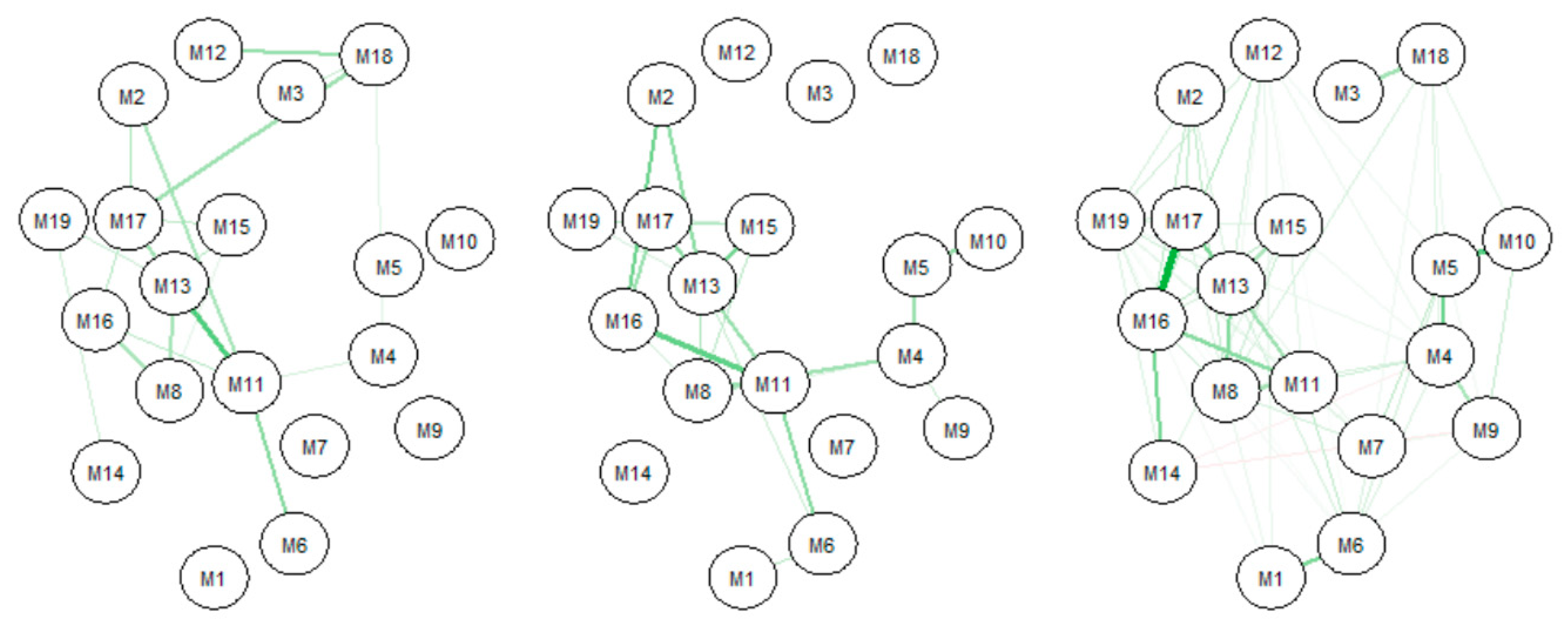
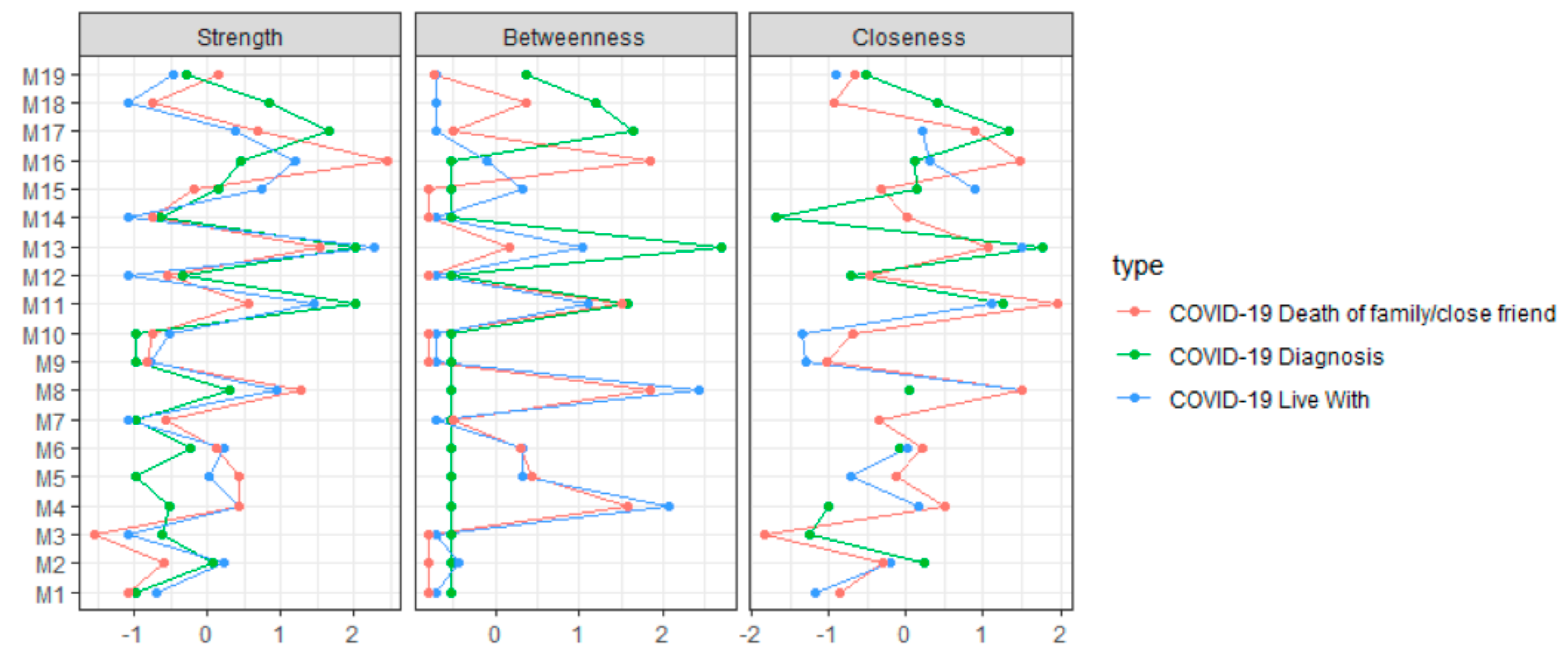
2.3. Statistical Analysis
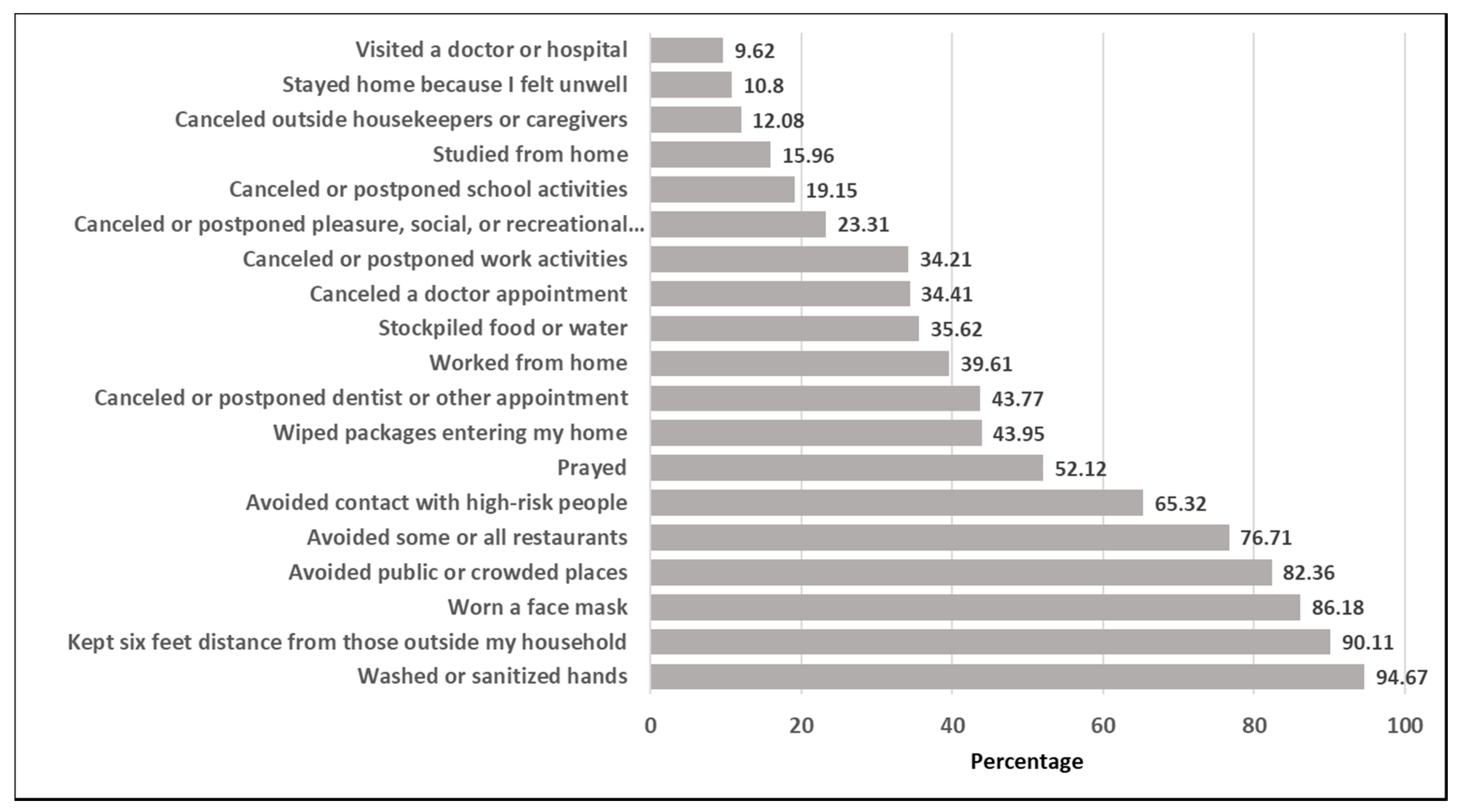
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Primary Outcome |
| COVID-19 measure counts |
| Sum of “Yes” indications across M1–M19 relating to COVID-19 measures taken |
| Exposures |
| Insurance |
| “Yes” if any of PHYS9A–PHYS9H were “Yes, otherwise “No” (relating to insurance types respondents have) |
| Plans having been changed over past 7 days |
| Sum of “Yes” indications across ECON8A–ECON8S relating to instances in which plans have been changed |
| Sought financial aid over past 7 days |
| Sum of all indications across ECON6A–ECON6L relating to applying for aid or trying to apply for aid |
| Flu-like symptoms over past 7 days |
| Sum of “Yes” indications from PHYS1A–PHYS1Q relating to flu-like symptoms |
| Interest in COVID-19 management measures |
| Converted PHYS10A–PHYS10E into 5 point scale: “Extremely likely” to 5 and “Not likely at all” to 1, then averaged |
| Mental health issues over past 7 days |
| Converted SOC5A—SOC5E into 4 point scale: “5–7 days” to 4 and “not at all or less than 1 day” to 1, then averaged |
References
- Naming the Coronavirus Disease (COVID-19) and the Virus that Causes It. World Health Organization. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (accessed on 28 April 2020).
- Wang, R.; Zhang, X.; Irwin, D.M.; Shen, Y. Emergence of SARS-like coronavirus poses new challenge in China. J. Infect. 2020, 80, 350–371. [Google Scholar] [CrossRef] [PubMed]
- Bahl, P.; Doolan, C.; de Silva, C.; Chughtai, A.A.; Bourouiba, L.; MacIntyre, C.R. Airborne or droplet precautions for health workers treating COVID-19? J. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morawska, L.; Cao, J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environ. Int. 2020. [Google Scholar] [CrossRef] [PubMed]
- Burke, R.M. Active monitoring of persons exposed to patients with confirmed COVID-19—United States, January–February 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 245–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, J.F.-W.; Yuan, S.; Kok, K.-H.; To, K.K.-W.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.-Y.; Poon, R.W.-S.; et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef] [Green Version]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.; Lau, E.H.; Wong, J.Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef]
- Shereen, M.A.; Khan, S.; Kazmi, A.; Bashir, N.; Siddique, R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J. Adv. Res. 2020. [Google Scholar] [CrossRef]
- Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions: Scientific Brief, 09 July 2020; World Health Organization: Geneva, Switzerland, 2020.
- Guan, W.-J.; Ni, Z.-Y.; Hu, Y.; Liang, W.-H.; Ou, C.-Q.; He, J.-X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, D.S. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Vaira, L.A.; Deiana, G.; Fois, A.G.; Pirina, P.; Madeddu, G.; De Vito, A.; Babudieri, S.; Petrocelli, M.; Serra, A.; Bussu, F. Objective evaluation of anosmia and ageusia in COVID-19 patients: Single-center experience on 72 cases. Head Neck 2020, 42, 1252–1258. [Google Scholar] [CrossRef]
- Gautier, J.F.; Ravussin, Y. A new symptom of COVID-19: Loss of taste and smell. Obesity 2020, 28, 848. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. Older Adults. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html (accessed on 28 April 2020).
- Novel, C.P. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi 2020, 41, 145. [Google Scholar]
- Centers for Disease Control and Prevention. People With Certain Medical Condition. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 28 April 2020).
- Haushofer, J.; Metcalf, J. Combining Behavioral Economics and Infectious Disease Epidemiology to Mitigate the COVID-19 Outbreak; Princeton University: Princeton, NJ, USA, 2020. [Google Scholar]
- Jernigan, D.B. Update: Public health response to the coronavirus disease 2019 outbreak—United States, February 24, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations: Scientific Brief, 27 March 2020; World Health Organization: Geneva, Switzerland, 2020.
- Rational Use of Personal Protective Equipment (PPE) for Coronavirus Disease (COVID-19): Interim Guidance, 19 March 2020; World Health Organization: Geneva, Switzerland, 2020.
- Centers for Disease Control Prevention. Use of Cloth Face Coverings to Help Slow the Spread of COVID-19. 2020, 12. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html (accessed on 28 April 2020).
- Gostin, L.O.; Hodge, J.G., Jr.; Wiley, L.F. Presidential powers and response to COVID-19. JAMA 2020, 323, 1547–1548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Public Health and Welfare. In U.S. Code; Section 5122, Title 42. Available online: https://www.law.cornell.edu/uscode/text/42 (accessed on 28 April 2020).
- Madhav, N.; Oppenheim, B.; Gallican, M.; Mulembakani, P.; Rubin, E.; Wolfe, N. Pandemics: Risks, impacts, and mitigation. In Disease Control Priorities, (Volume 9): Improving Health and Reducing Poverty; Jamison, D.T., Gelband, H., Horton, S., Jha, P., Laxminarayan, R., Mock, C.N., Nugent, R., Eds.; The World Bank: Washington, DC, USA, 2017. [Google Scholar]
- Holtz, D.; Zhao, M.; Benzell, S.G.; Cao, C.Y.; Rahimian, M.A.; Yang, J.; Allen, J.N.L.; Collis, A.; Moehring, A.V.; Sowrirajan, T. Interdependence and the Cost of Uncoordinated Responses to COVID-19. 2020. Available online: https://osf.io/b9psy/ (accessed on 28 April 2020). [CrossRef]
- Qeadan, F.; Honda, T.; Gren, L.H.; Dailey-Provost, J.; Benson, L.S.; VanDerslice, J.A.; Porucznik, C.A.; Waters, A.B.; Lacey, S.; Shoaf, K. Naive forecast for COVID-19 in Utah based on the South Korea and Italy models-the fluctuation between two extremes. Int. J. Environ. Res. Public Health 2020, 17, 2750. [Google Scholar] [CrossRef] [PubMed]
- Mervosh, S.; Lu, D.; Swales, V. See which states and cities have told residents to stay at home. New York Times 2020. [Google Scholar]
- Al-Hasan, A.; Yim, D.; Khuntia, J. Citizens’ adherence to COVID-19 mitigation recommendations by the government: A 3-country comparative evaluation using web-based cross-sectional survey data. J. Med Internet Res. 2020, 22, e20634. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.; Davila, A.; Regis, M.; Kraus, S. Predictors of COVID-19 voluntary compliance behaviors: An international investigation. Glob. Transit. 2020. [Google Scholar] [CrossRef]
- Jørgensen, F.J.; Bor, A.; Petersen, M.B. Compliance without fear: Predictors of protective behavior during the first wave of the COVID-19 pandemic. PsyArXiv. May 2020, 19. [Google Scholar] [CrossRef]
- Solomou, I.; Constantinidou, F. Prevalence and predictors of anxiety and depression symptoms during the CoViD-19 pandemic and compliance with precautionary measures: Age and sex matter. Int. J. Environ. Res. Public Health 2020, 17, 4924. [Google Scholar] [CrossRef]
- COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at John Hopkins University (JHU). 2020. Available online: https://coronavirus.jhu.edu/map.html (accessed on 28 April 2020).
- Khazaee-Pool, M.; Naghibi, S.A.; Pashaei, T.; Jahangiry, L.; Daneshnia, M.; Ponnet, K. Development and Initial Validation of a Scale for Assessing Affecting Factors on Preventive Behaviors of COVID-19 (AFPB-CO): Using the Protection Motivation Theory. 2020. Available online: https://www.researchsquare.com/article/rs-23051/v1 (accessed on 28 April 2020). [CrossRef]
- Yıldırım, M.; Güler, A. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Stud. 2020. [Google Scholar] [CrossRef]
- Borsboom, D.; Cramer, A.O. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fried, E.I.; Nesse, R.M. Depression sum-scores don’t add up: Why analyzing specific depression symptoms is essential. BMC Med. 2015, 13, 72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smeets, F.; Lataster, T.; Viechtbauer, W.; Delespaul, P.; G.R.O.U.P. Evidence that environmental and genetic risks for psychotic disorder may operate by impacting on connections between core symptoms of perceptual alteration and delusional ideation. Schizophr. Bull. 2014, 41, 687–697. [Google Scholar] [CrossRef]
- COVID Impact Survey. Available online: https://www.covid-impact.org/ (accessed on 6 April 2020).
- Wozniak, A.; Willey, J.; Benz, J.; Hart, N. COVID Impact Survey: Version 2 [Dataset]; National Opinion Research Center: Chicago, IL, USA, 2020. [Google Scholar]
- Network Analysis in R Cookbook. Available online: http://sachaepskamp.com/files/Cookbook.html (accessed on 28 April 2020).
- Epskamp, S.; Fried, E.I. A tutorial on regularized partial correlation networks. Psychol. Methods 2018, 23, 617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Opsahl, T.; Agneessens, F.; Skvoretz, J. Node centrality in weighted networks: Generalizing degree and shortest paths. Soc. Netw. 2010, 32, 245–251. [Google Scholar] [CrossRef]
- Barr, M.; Raphael, B.; Taylor, M.; Stevens, G.; Jorm, L.; Giffin, M.; Lujic, S. Pandemic influenza in Australia: Using telephone surveys to measure perceptions of threat and willingness to comply. BMC Infect. Dis. 2008, 8, 117. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. Previous U.S. COVID-19 Case Data. Available online: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/previouscases.html (accessed on 28 July 2020).
- Blendon, R.J.; Koonin, L.M.; Benson, J.M.; Cetron, M.S.; Pollard, W.E.; Mitchell, E.W.; Weldon, K.J.; Herrmann, M.J. Public response to community mitigation measures for pandemic influenza. Emerg. Infect. Dis. 2008, 14, 778. [Google Scholar] [CrossRef]
- Liao, Q.; Cowling, B.J.; Lam, W.W.; Ng, D.M.; Fielding, R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: Ten cross-sectional surveys. BMC Infect. Dis. 2014, 14, 169. [Google Scholar] [CrossRef] [Green Version]
- Tang, C.S.; Wong, C.-Y. An outbreak of the severe acute respiratory syndrome: Predictors of health behaviors and effect of community prevention measures in Hong Kong, China. Am. J. Public Health 2003, 93, 1887–1888. [Google Scholar] [CrossRef]
- Balkhy, H.H.; Abolfotouh, M.A.; Al-Hathlool, R.H.; Al-Jumah, M.A. Awareness, attitudes, and practices related to the swine influenza pandemic among the Saudi public. BMC Infect. Dis. 2010, 10, 42. [Google Scholar] [CrossRef] [Green Version]
- Bults, M.; Beaujean, D.J.; de Zwart, O.; Kok, G.; van Empelen, P.; van Steenbergen, J.E.; Richardus, J.H.; Voeten, H.A. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: Results of three consecutive online surveys. BMC Public Health 2011, 11, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karademas, E.C.; Bati, A.; Karkania, V.; Georgiou, V.; Sofokleous, S. The association between pandemic influenza A (H1N1) public perceptions and reactions: A prospective study. J. Health Psychol. 2013, 18, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.T.F.; Griffiths, S.; Choi, K.C.; Tsui, H.Y. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect. Dis. 2010, 10, 139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sadique, M.Z.; Edmunds, W.J.; Smith, R.D.; Meerding, W.J.; De Zwart, O.; Brug, J.; Beutels, P. Precautionary behavior in response to perceived threat of pandemic influenza. Emerg. Infect. Dis. 2007, 13, 1307. [Google Scholar] [CrossRef] [PubMed]
| Total | 25,269 1 (100.00%) |
|---|---|
| Age (years) | |
| 18 to 29 | 3226 1 (20.79) 2 |
| 30–44 | 6117 (27.13) |
| 45–59 | 5981 (23.06) |
| 60+ | 9942 (29.01) |
| Gender | |
| Male | 11,070 (48.73) |
| Female | 14,186 (51.27) |
| Race and Ethnicity | |
| Non-Hispanic White | 15,985 (49.77) |
| Non-Hispanic Black | 2290 (11.42) |
| Hispanic | 2258 (23.03) |
| Non-Hispanic Other | 1789 (9.69) |
| Unknown 3 | 2947 (6.10) |
| Household Income | |
| Under $10,000 | 1283 (8.63) |
| $10,000 to under $20,000 | 1809 (9.54) |
| $20,000 to under $30,000 | 2360 (12.03) |
| $30,000 to under $40,000 | 2240 (9.50) |
| $40,000 to under $50,000 | 1942 (8.08) |
| $50,000 to under $75,000 | 4526 (16.09) |
| $75,000 to under $100,000 | 3568 (12.19) |
| $100,000 to under $150,000 | 3866 (12.13) |
| $150,000 or more | 3055 (9.75) |
| Unknown | 620 (2.06) |
| Education | |
| No high school diploma | 885 (9.83) |
| High school graduate or equivalent | 3263 (28.65) |
| Some college | 7828 (30.26) |
| BA or above | 13,254 (31.26) |
| Household Size | |
| One person (I live by myself) | 7711 (28.15) |
| Two persons | 8860 (30.10) |
| Three persons | 3514 (15.82) |
| Four persons | 2638 (12.10) |
| Five persons | 1295 (7.00) |
| Six or more persons | 1203 (6.83) |
| Population Density | |
| Rural | 1445 (4.15) |
| Suburban | 3990 (12.96) |
| Urban | 19,829 (82.88) |
| Region | |
| Northeast | 3055 (13.52) |
| Midwest | 7036 (14.71) |
| South | 8161 (38.36) |
| West | 7017 (33.40) |
| Insurance | |
| No | 1805 (13.31) |
| Yes | 23,464 (86.69) |
| Total | 25,269 1 |
|---|---|
| Overall Self-Reported Health | |
| Excellent | 4992 1 (20.25) 2 |
| Very good | 10,443 (38.80) |
| Good | 6880 (28.34) |
| Fair | 2404 (10.01) |
| Poor | 522 (2.60) |
| COVID-19 positive | |
| Yes | 181 (0.84) |
| No | 24,899 (98.04) |
| Unknown 3 | 189 (1.12) |
| COVID-19 positive of someone living with | |
| Yes | 175 (0.98) |
| No | 24,714 (97.22) |
| Unknown | 380 (1.79) |
| COVID-19 or respiratory illness death of family member or close friend since 1 March 2020 | |
| Yes | 1121 (5.27) |
| No | 23,621 (92.13) |
| Unknown | 527 (2.60) |
| Plans having been changed due to COVID-19 4 mean (SD) | 6.89 (4.42) |
| Sought financial aid during COVID-19 4 mean (SD) | 1.07 (1.49) |
| Flu-like symptoms during COVID-19 4 mean (SD) | 2.12 (2.45) |
| Interest in COVID-19 management measures 5 mean (SD) | 2.98 (1.14) |
| Mental health issues during COVID-19 5 mean (SD) | 1.51 (0.64) |
| Diabetic | |
| Yes | 2803 (11.15) |
| No | 21,769 (85.43) |
| Unknown | 697 (3.41) |
| High blood pressure or Hypertension | |
| Yes | 8434 (29.53) |
| No | 16,114 (66.59) |
| Unknown | 721 (3.89) |
| Heart disease, heart attack, or stroke | |
| Yes | 2036 (6.77) |
| No | 22,435 (89.38) |
| Unknown | 798 (3.85) |
| Asthma | |
| Yes | 3429 (13.61) |
| No | 21,078 (82.54) |
| Unknown | 762 (3.85) |
| Chronic lung disease or COPD | |
| Yes | 1036 (4.09) |
| No | 23,631 (93.04) |
| Unknown | 602 (2.87) |
| Bronchitis or emphysema | |
| Yes | 2905 (10.41) |
| No | 21,777 (86.69) |
| Unknown | 587 (2.89) |
| Allergies | |
| Yes | 11,227 (41.42) |
| No | 13,327 (55.21) |
| Unknown | 715 (3.37) |
| Mental health condition | |
| Yes | 4062 (15.09) |
| No | 20,460 (80.92) |
| Unknown | 747 (3.99) |
| Cystic fibrosis | |
| Yes | 74 (0.50) |
| No | 24,807 (97.24) |
| Unknown | 388 (2.25) |
| Liver disease or end stage liver disease | |
| Yes | 327 (1.39) |
| No | 24,559 (96.62) |
| Unknown | 383 (1.99) |
| Cancer | |
| Yes | 2344 (6.40) |
| No | 22,443 (91.14) |
| Unknown | 482 (2.46) |
| Compromised immune system | |
| Yes | 1858 (6.62) |
| No | 22,713 (89.97) |
| Unknown | 698 (3.41) |
| Overweight or obese | |
| Yes | 8250 (30.12) |
| No | 16,469 (66.91) |
| Unknown | 550 (2.97) |
| Variables | April Adjusted IRR 2 (95% CI) | May Adjusted IRR 2 (95% CI) | June Adjusted IRR 2 (95% CI) |
|---|---|---|---|
| Age (years) | |||
| 18 to 29 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 30–44 | 1.03 (1.01, 1.05) | 1.05 (1.03, 1.08) | 1.03 (1.00 3, 1.06) |
| 45–59 | 1.04 (1.02, 1.07) | 1.00 (0.98, 1.03) | 1.02 (0.99, 1.05) |
| 60+ | 1.05 (1.02, 1.08) | 1.03 (1.00 3, 1.06) | 1.04 (1.01, 1.07) |
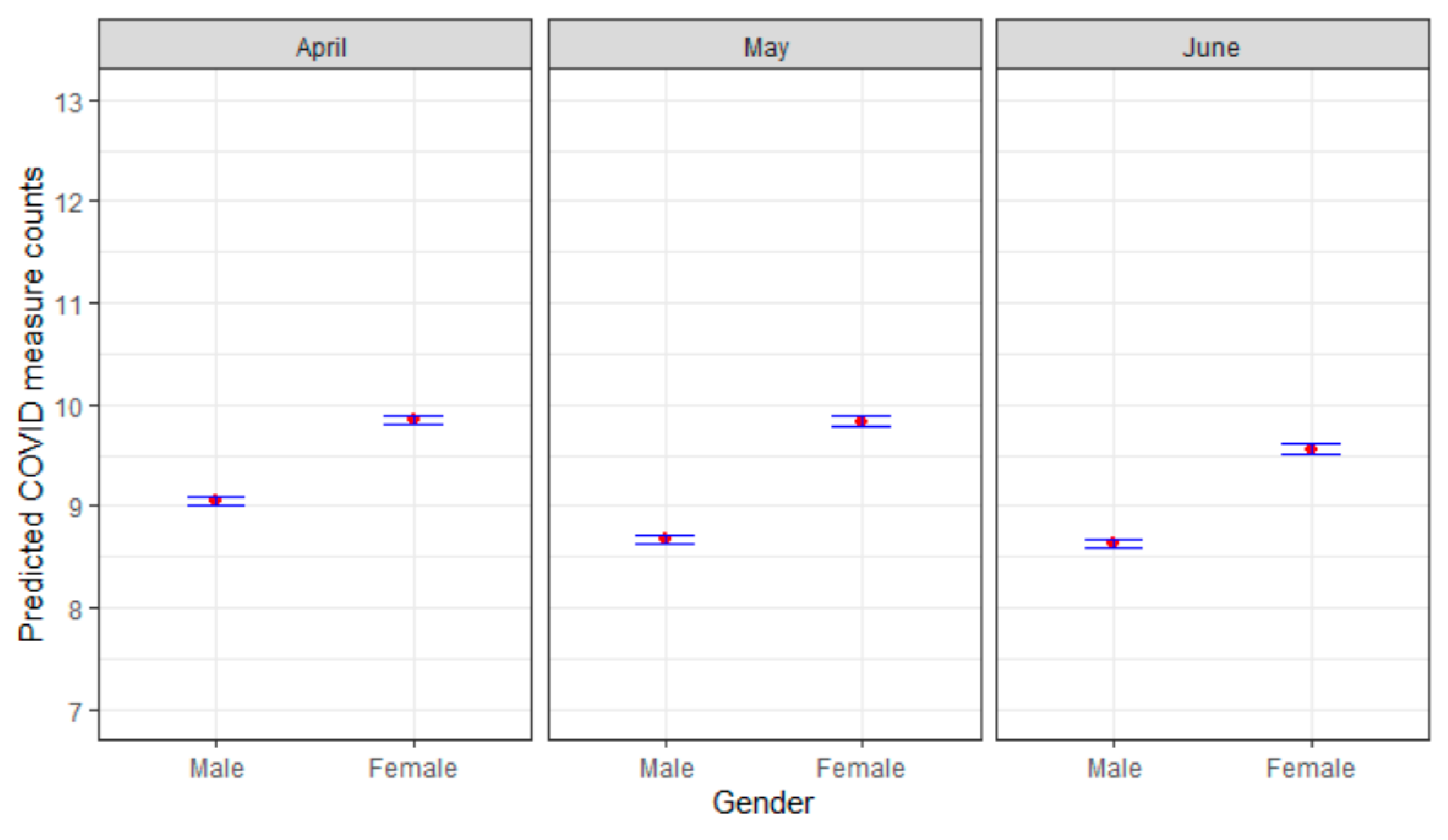
| Gender | |||
| Male | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Female | 1.08 (1.06, 1.09) | 1.12 (1.10, 1.14) | 1.09 (1.07, 1.11) |
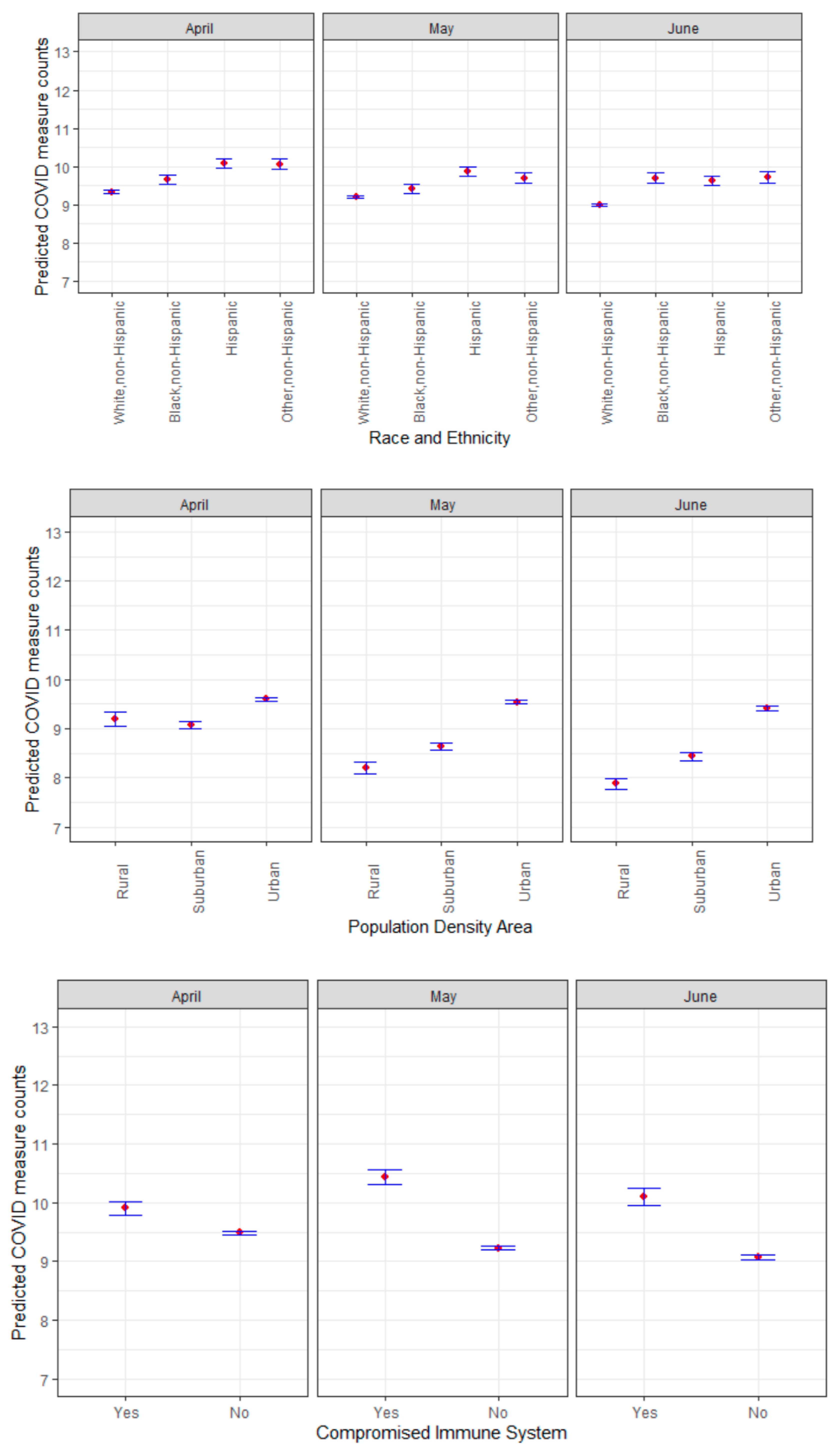
| Race and Ethnicity | |||
| Non-Hispanic White | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Non-Hispanic Black | 1.03 (1.01, 1.06) | 1.00 (0.97, 1.03) | 1.05 (1.02, 1.08) |
| Hispanic | 1.09 (1.07, 1.12) | 1.06 (1.04, 1.08) | 1.06 (1.03, 1.08) |
| Non-Hispanic Other | 1.07 (1.04, 1.10) | 1.04 (1.01, 1.07) | 1.06 (1.03, 1.09) |
| Household income | 1.01 (1.01, 1.01) | 1.02 (1.01, 1.02) | 1.02 (1.01, 1.02) |
| Education | |||
| No high school diploma | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| High school graduate or equivalent | 1.08 (1.04, 1.11) | 0.99 (0.96, 1.02) | 0.98 (0.95, 1.02) |
| Some college | 1.10 (1.07, 1.14) | 1.03 (1.00 3, 1.07) | 1.02 (0.99, 1.06) |
| BA or above | 1.16 (1.12, 1.20) | 1.11 (1.07, 1.14) | 1.09 (1.05, 1.13) |
| Household size | 1.02 (1.01, 1.03) | 1.01 (1.00 3, 1.01) | 1.01 (1.01, 1.02) |
| Population density | |||
| Urban | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Suburban | 0.98 (0.95, 1.00 3) | 0.95 (0.93, 0.98) | 0.94 (0.92, 0.97) |
| Rural | 1.02 (0.97, 1.06) | 0.92 (0.88, 0.96) | 0.91 (0.87, 0.96) |
| Region | |||
| South | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Northeast | 1.02 (1.00 3, 1.05) | 0.99 (0.97, 1.02) | 0.98 (0.95, 1.01) |
| Midwest | 0.98 (0.95, 1.00 3) | 0.97 (0.95, 1.00 3) | 0.99 (0.96, 1.02) |
| West | 0.99 (0.97, 1.01) | 0.95 (0.93, 0.97) | 0.95 (0.93, 0.97) |
| Insurance | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.15 (1.12, 1.18) | 1.08 (1.05, 1.11) | 1.09 (1.06, 1.12) |
| High blood pressure or Hypertension | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.04 (1.02, 1.06) | 1.03 (1.01, 1.05) | 1.02 (1.00 3, 1.04) |
| Asthma | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.05 (1.03, 1.07) | 1.05 (1.02, 1.07) | 1.04 (1.02, 1.07) |
| Chronic lung disease or COPD | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.04 (1.00 3, 1.08) | 1.01 (0.96, 1.06) | 1.00 (0.96, 1.04) |
| A mental health condition | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.00 (0.98, 1.03) | 1.01 (0.98, 1.03) | 1.01 (0.98, 1.04) |
| A compromised immune system | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.03 (0.99, 1.06) | 1.10 (1.06, 1.13) | 1.08 (1.04, 1.11) |
| Overweight or obese | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.04 (1.02, 1.06) | 1.05 (1.03, 1.07) | 1.02 (1.00 3, 1.04) |
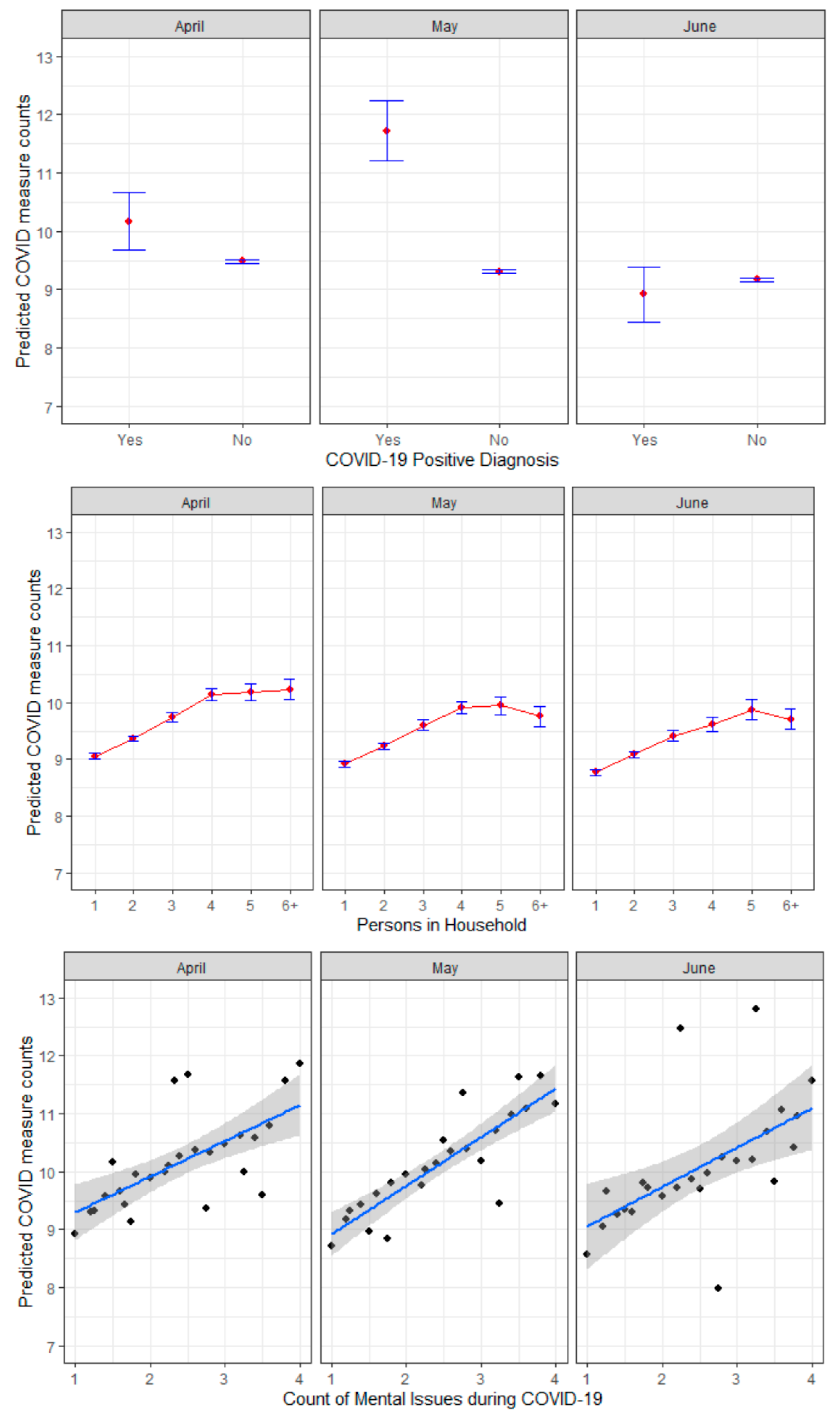
| COVID-19 positive diagnosis | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.00 (0.91, 1.11) | 1.18 (1.09, 1.28) | 0.89 (0.81, 0.97) |
| COVID-19/respiratory illness death of friend or close friend since March 1, 2020 | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.04 (1.00 3, 1.08) | 1.02 (0.99, 1.06) | 1.16 (1.11, 1.20) |
| Plans having been changed due to COVID-19 | 1.02 (1.02, 1.03) | 1.02 (1.02, 1.03) | 1.02 (1.02, 1.02) |
| Mental health issues during COVID-19 | 1.07 (1.05, 1.08) | 1.06 (1.04, 1.07) | 1.07 (1.05, 1.08) |
| R 2 | 20% | 19% | 17% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qeadan, F.; Akofua Mensah, N.; Tingey, B.; Bern, R.; Rees, T.; Talboys, S.; Pal Singh, T.; Lacey, S.; Shoaf, K. What Protective Health Measures Are Americans Taking in Response to COVID-19? Results from the COVID Impact Survey. Int. J. Environ. Res. Public Health 2020, 17, 6295. https://doi.org/10.3390/ijerph17176295
Qeadan F, Akofua Mensah N, Tingey B, Bern R, Rees T, Talboys S, Pal Singh T, Lacey S, Shoaf K. What Protective Health Measures Are Americans Taking in Response to COVID-19? Results from the COVID Impact Survey. International Journal of Environmental Research and Public Health. 2020; 17(17):6295. https://doi.org/10.3390/ijerph17176295
Chicago/Turabian StyleQeadan, Fares, Nana Akofua Mensah, Benjamin Tingey, Rona Bern, Tracy Rees, Sharon Talboys, Tejinder Pal Singh, Steven Lacey, and Kimberley Shoaf. 2020. "What Protective Health Measures Are Americans Taking in Response to COVID-19? Results from the COVID Impact Survey" International Journal of Environmental Research and Public Health 17, no. 17: 6295. https://doi.org/10.3390/ijerph17176295
APA StyleQeadan, F., Akofua Mensah, N., Tingey, B., Bern, R., Rees, T., Talboys, S., Pal Singh, T., Lacey, S., & Shoaf, K. (2020). What Protective Health Measures Are Americans Taking in Response to COVID-19? Results from the COVID Impact Survey. International Journal of Environmental Research and Public Health, 17(17), 6295. https://doi.org/10.3390/ijerph17176295








