Associations between 24 h Movement Behavior and Mental Health in Office Workers
Abstract
:1. Introduction
- To investigate whether the entire 24 h movement behavior composition, consisting of MVPA, LIPA, SED, and time in bed, is associated with mental health outcomes, i.e., depression or anxiety symptoms, burnout, mental wellbeing, and stress in a population of healthy office workers.
- To investigate associations between time spent in any of these movement-related behaviors, relative to the others, and the mental health outcomes.
- To investigate theoretical effects of reallocating time between the behaviors.
2. Materials and Methods
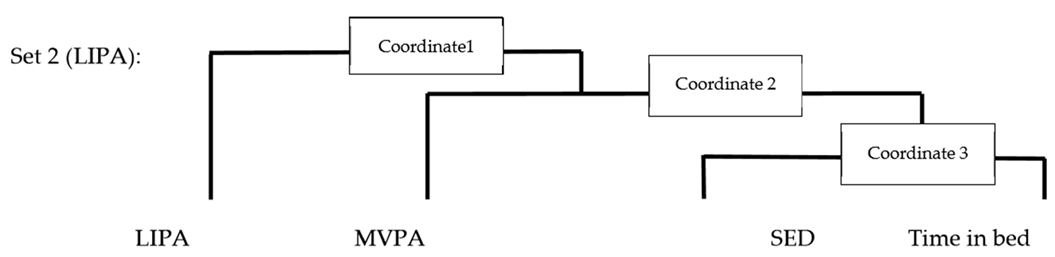
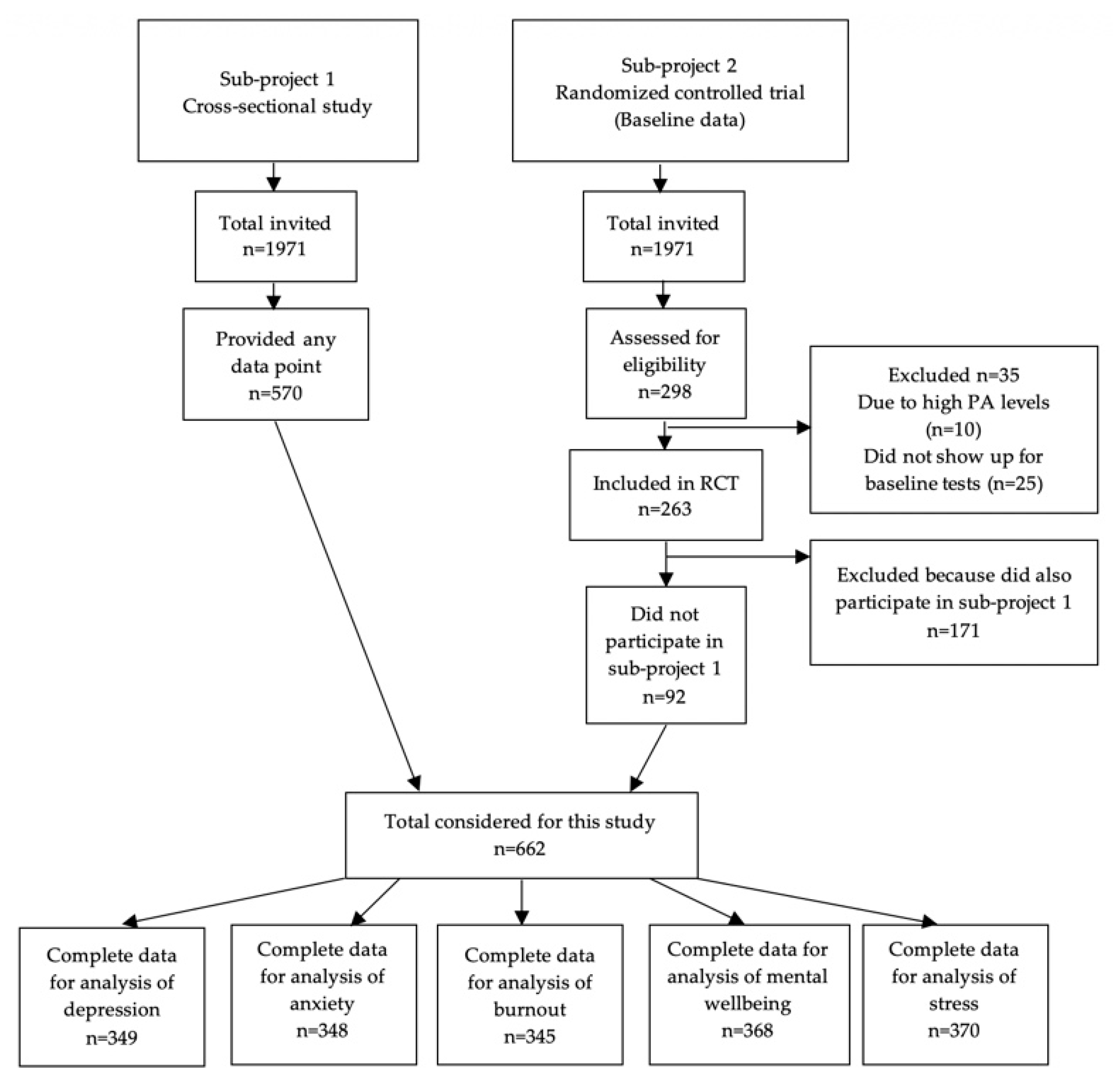
2.1. Participants
2.2. Mental Health Outcomes
2.3. Movement-Related Behaviors
2.4. Covariates
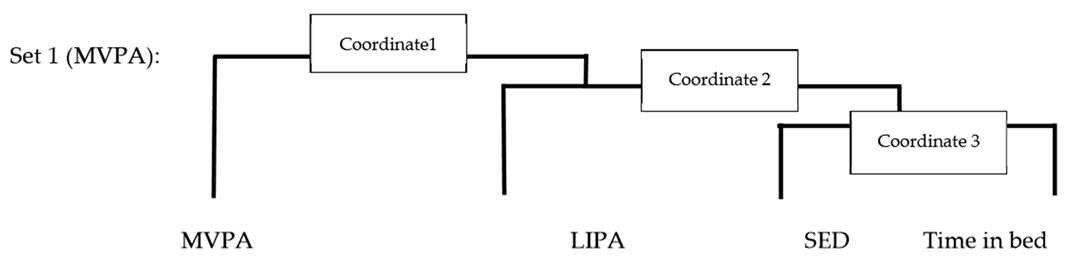
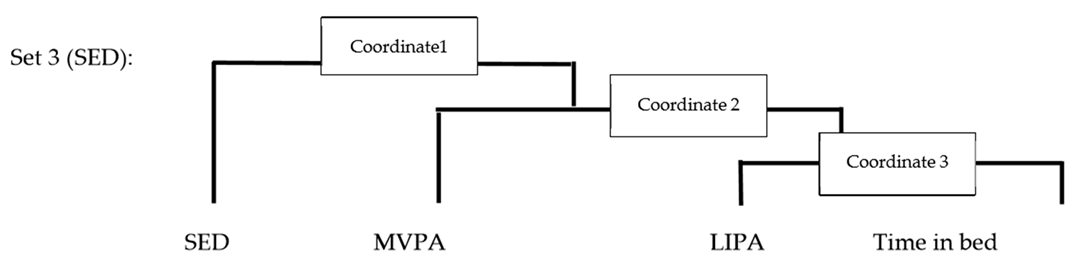
2.5. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A

Appendix B
| Movement-Related Behavior | Crude Model | Adjusted Model | Fully Adjusted Model |
|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | |
| MVPA | −0.02 (−0.98; 0.93) | 0.003 (−0.96; 0.97) | 0.18 (−0.79; 1.14) |
| LIPA | 0.40 (−1.18; 1.97) | 0.43 (−1.16; 2.02) | 0.71 (−0.87; 2.30) |
| SED | −0.66 (−2.69; 1.36) | −0.61 (−2.69; 1.47) | −0.76 (−2.86; 1.340 |
| Time in bed | 0.29 (−2.42; 3.0) | 0.17 (−2.59; 2.93) | −0.13 (−2.88; 2.62) |
| Movement-Related Behavior | Crude Model | Adjusted Model | Fully Adjusted Model |
|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | |
| MVPA | −0.03 (−1.23; 1.24) | −0.16 (−1.42; 1.10) | −0.08 (−1.36; 1.20) |
| LIPA | 1.0 (−1.10; 3.10) | 1.14 (−0.96; 3.24) | 1.3 (−0.81; 3.41) |
| SED | −1.28 (−3.95; 1.38) | −0.53 (−3.23; 2.18) | −0.57 (−3.33; 2.19) |
| Time in bed | 0.31 (−3.29; 3.91) | −0.45 (−4.07; 3.17) | −0.65 (−4.27; 2.98) |
| Movement-Related Behavior | Crude Model | Adjusted Model | Fully Adjusted Model |
|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | |
| MVPA | −0.23 (−0.50; 0.04) | −0.25 (−0.52; 0.02) | −0.20 (−0.47; 0.07) |
| LIPA | −0.07 (−0.52; 0.38) | −0.04 (−0.49; 0.41) | 0.02 (−0.43; 0.47) |
| SED | −0.24 (−0.79; 0.31) | −0.13 (−0.69; 0.44) | −0.21 (−0.78; 0.36) |
| Time in bed | 0.54 (−0.22; 1.29) | 0.42 (−0.35; 1.19) | 0.39 (−0.37; 1.16) |
| Movement-Related Behavior | Crude Model | Adjusted Model | Fully Adjusted Model |
|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | |
| MVPA | 7.01 * (1.16; 12.87) | 7.1 * (1.20; 13.0) | 5.48 (−0.38; 11.34) |
| LIPA | −3.69 (−13.48; 6.11) | −3.72 (−13.57; 6.13) | −6.14 (−15.89; 3.61) |
| SED | −1.61 (−13.64; 10.42) | −3.66 (−16.01; 8.70) | −0.49 (−12.86; 11.86) |
| Time in bed | −1.72 (−18.25; 14.82) | 0.28 (−16.52;17.08) | 1.15 (−15.40; 17.70) |
| Movement-Related Behavior | Crude Model | Adjusted Model | Fully Adjusted Model |
|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | |
| MVPA | 0.10 (−0.29; 0.50) | 0.10 (−0.30; 0.50) | 0.12 (−0.28; 0.52) |
| LIPA | −0.06 (−0.72; 0.60) | −0.07 (−0.73; 0.59) | −0.03 (−0.70; 0.64) |
| SED | −0.46 (−1.27; 0.35) | −0.27 (−1.10; 0.56) | −0.29 (−1.13; 0.56) |
| Time in bed | 0.42 (−0.69; 1.54) | 0.24 (−0.88; 1.37) | 0.20 (−0.93; 1.32) |
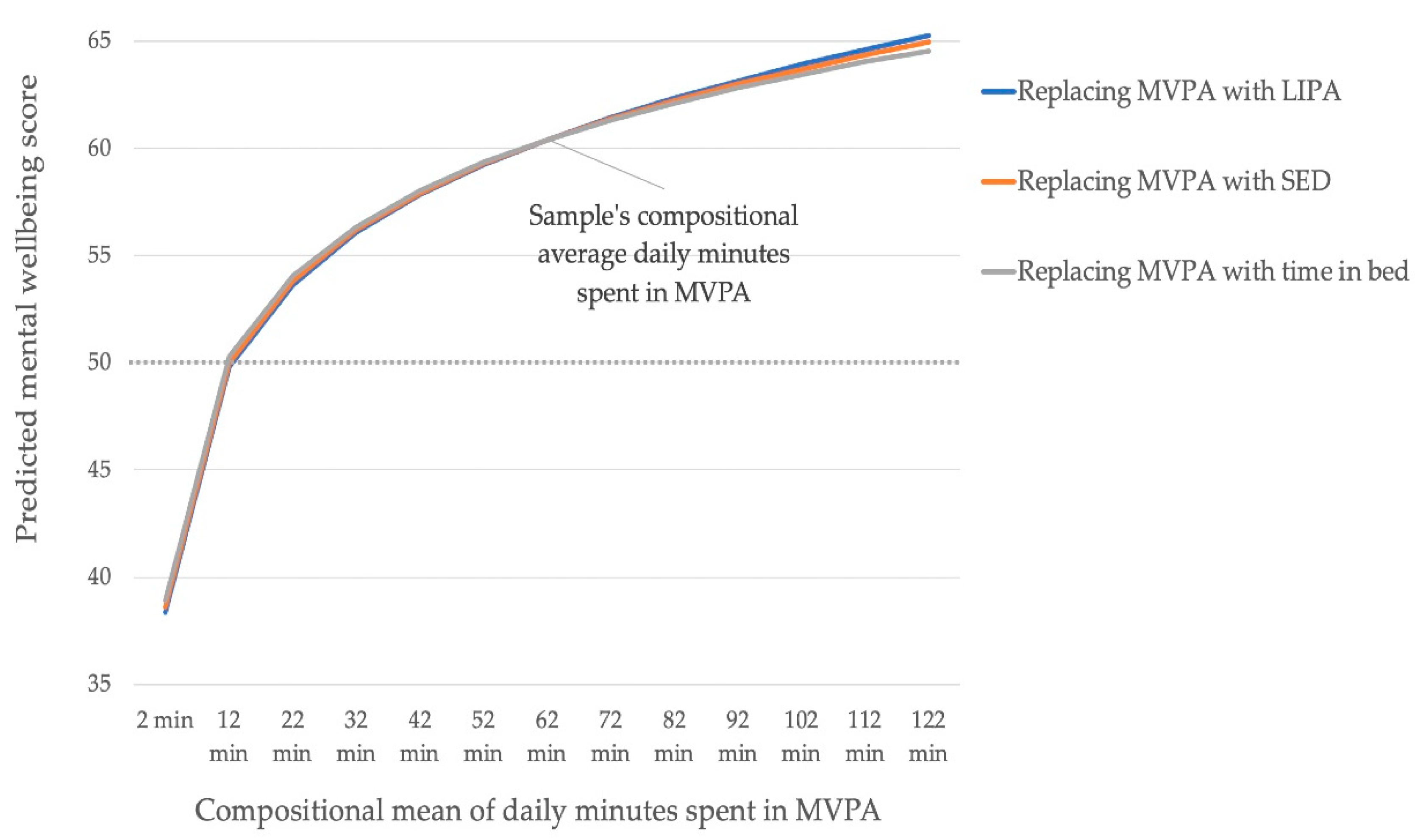
Appendix C
| Reallocations | Compositional Mean of Daily Minutes Spent in MVPA | Predicted Mental Wellbeing Score after Theoretically Replacing MVPA with LIPA (95% CI) | Predicted Mental Wellbeing Score after Theoretically Replacing MVPA with SED (95% CI) | Predicted Mental Wellbeing Score after Theoretically Replacing MVPA with Time in Bed (95% CI) |
|---|---|---|---|---|
| Theoretically reducing time spent in MVPA | 2 min | 38 (20; 57) | 39 (21; 57) | 39 (20; 57) |
| 12 min | 50 (41; 59) | 50 (41; 59) | 50 (41; 60) | |
| 22 min | 54 (47; 60) | 54 (48; 60) | 54 (48; 60) | |
| 32 min | 56 (51; 61) | 56 (52; 61) | 56 (52; 61) | |
| 42 min | 58 (54; 61) | 58 (55; 61) | 58 (55; 61) | |
| 52 min | 59 (56; 62) | 59 (56; 62) | 59 (56; 62) | |
| Samples average time spent in MVPA | 62 min | 60 (58; 63) | 60 (58; 63) | 60 (58; 63) |
| Theoretically increasing time spent in MVPA | 72 min | 61 (59; 64) | 61 (59; 64) | 61 (59; 64) |
| 82 min | 62 (59; 65) | 62 (59; 65) | 62 (59; 65) | |
| 92 min | 63 (60; 67) | 63 (60; 66) | 63 (59; 66) | |
| 102 min | 64 (60; 68) | 64 (60; 67) | 63 (59; 67) | |
| 112 min | 65 (60; 69) | 64 (60; 68) | 64 (59; 69) | |
| 122 min | 65 (60; 70) | 65 (61; 69) | 65 (59; 70) |
Appendix D
| Mental Health Outcome | Crude Model | Adjusted Model | Fully Adjusted Model |
|---|---|---|---|
| Mental wellbeing | 0.0059 | 0.0051 | 0.0963 |
| Movement-Related Behavior | Crude Model | Adjusted Model | Fully Adjusted Model | |||
|---|---|---|---|---|---|---|
| p-Value | β (95% CI) | p-Value | β (95% CI) | p-Value | β (95% CI) | |
| At least VPA | 0.0025 * | 3.44 (1.61; 5.28) | 0.0027 * | 3.49 (1.63; 5.35) | 0.0115 * | 2.50 (0.56; 4.44) |
| MPA | 0.8786 | −0.49 (−6.73; 5.76) | 0.9073 | −0.37 (−6.64; 5.90) | 0.8856 | 0.46 (−5.78; 6.69) |
| LIPA | 0.8575 | −0.87 (−10.44; 12.66) | 0.8288 | −1.06 (−10.66; 8.55) | 0.4315 | −3.87 (−13.51; 5.78) |
| SED | 0.8637 | 1.02 (−10.63; 12.67) | 0.8843 | −0.85 (−12.82; 11.11) | 0.8862 | 0.87 (−11.13; 12.88) |
| Time in bed | 0.7005 | −3.10 (−18.95; 12.74) | 0.8829 | −1.21 (−17.31; 14.89) | 0.9973 | 0.03 (−15.94; 15.99) |
References
- OECD/European Union. Health at a Glance: Europe 2018: State of Health in the EU Cycle. Chapter 1: Promoting Mental Health in Europe: Why and How? Available online: https://doi.org/10.1787/health_glance_eur-2018-en (accessed on 13 February 2020).
- Försäkringskassan. Sjukfrånvaros Utveckling 2016. Social Insurance Report 2016:7. Available online: https://www.forsakringskassan.se/wps/wcm/connect/a2001891-5c47-4b8a-b47b-64dfbbd48555/socialforsakringsrapport_2016_07.pdf?MOD=AJPERES (accessed on 13 February 2020).
- Försäkringskassan. Sjukfrånvarons Utveckling 2017. Socialförsäkringsrapport 2017:13. Available online: https://www.forsakringskassan.se/wps/wcm/connect/1596d32b-7ff7-4811-8215-d90cb9c2f38d/socialforsakringsrapport-2017-13.pdf?MOD=AJPERES&CVID= (accessed on 13 February 2020).
- Mammen, G.; Faulkner, G. Physical activity and the prevention of depression. Am. J. Prev. Med. 2013, 45, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Cooper, K.; Barton, G. An exploration of physical activity and wellbeing in university employees. Perspect. Public Health 2016, 136, 152–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamer, M.; Biddle, S.; Stamatakis, E. Weekend warrior physical activity pattern and common mental disorder: A population wide study of 108,011 British adults. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.B.; Silva, E.S.; Hallgren, M.; De Leon, A.P.; Dunn, A.L.; Deslandes, A.; et al. Physical activity and incident depression: A meta-analysis of prospective cohort studies. Am. J. Psychiatry 2018, 175, 631–648. [Google Scholar] [CrossRef] [PubMed]
- De Moor, M.H.M.; Beem, A.; Stubbe, J.; Boomsma, D.; De Geus, E.J.C. Regular exercise, anxiety, depression and personality: A population-based study. Prev. Med. 2006, 42, 273–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stubbs, B.; Koyanagi, A.; Hallgren, M.; Firth, J.; Richards, J.; Schuch, F.B.; Rosenbaum, S.; Mugisha, J.; Veronese, N.; Lahti, J.; et al. Physical activity and anxiety: A perspective from the World Health Survey. J. Affect. Disord. 2017, 208, 545–552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Mello, M.T.; Lemos, V.A.; Antunes, H.K.M.; Bittencourt, L.; Santos-Silva, R.; Tufik, S. Relationship between physical activity and depression and anxiety symptoms: A population study. J. Affect. Disord. 2013, 149, 241–246. [Google Scholar] [CrossRef]
- LZhai, Y.; Zhang, Y.; Zhang, D. Sedentary behaviour and the risk of depression: A meta-analysis. Br. J. Sports Med. 2015, 49, 705–709. [Google Scholar]
- Teychenne, M.; Costigan, S.A.; Parker, K.E. The association between sedentary behaviour and risk of anxiety: A systematic review. BMC Public Health 2015, 15, 513. [Google Scholar] [CrossRef] [Green Version]
- Naczenski, L.M.; De Vries, J.D.; Van Hooff, M.L.M.; Kompier, M.A.J. Systematic review of the association between physical activity and burnout. J. Occup. Health 2017, 59, 477–494. [Google Scholar] [CrossRef] [Green Version]
- Kalmbach, D.A.; Arnedt, J.T.; Song, P.X.; Guille, C.; Sen, S. Sleep disturbance and short sleep as risk factors for depression and perceived medical errors in first-year residents. Sleep 2017, 40, zsw073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, M.-S.; Shin, J.-S.; Lee, J.; Lee, M.S.; Kim, M.-R.; Park, K.B.; Shin, D.; Cho, J.-H.; Ha, I.-H. The association between mental health, chronic disease and sleep duration in Koreans: A cross-sectional study. BMC Public Health 2015, 15, 1200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harvey, S.B.; Øverland, S.; Hatch, S.L.; Wessely, S.; Mykletun, A.; Hotopf, M. Exercise and the Prevention of Depression: Results of the HUNT Cohort Study. Am. J. Psychiatry 2018, 175, 28–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prince, S.A.; Adamo, K.B.; Hamel, M.E.; Hardt, J.; Gorber, S.C.; Tremblay, M. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 56. [Google Scholar] [CrossRef] [Green Version]
- Chastin, S.; Palarea-Albaladejo, J.; Dontje, M.L.; Skelton, D.A. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: A novel compositional data analysis approach. PLoS ONE 2015, 10, e0139984. [Google Scholar] [CrossRef] [Green Version]
- Pedišić, Ž. Measurement issues and poor adjustments for physical activity and sleep undermine sedentary behaviour research—The focus should shift to the balance between sleep, sedentary behaviour, standing and activity. Kinesiology 2014, 46, 135–146. [Google Scholar]
- Dumuid, D.; Pedisic, Z.; Palarea-Albaladejo, J.; Martín-Fernández, J.; Hron, K.; Olds, T.S. Compositional data analysis in time-use epidemiology: What, why, how. Int. J. Environ. Res. Public Health 2020, 17, 2220. [Google Scholar] [CrossRef] [Green Version]
- Epstein, L.H.; Roemmich, J.N. Reducing sedentary behavior: Role in modifying physical activity. Exerc. Sport Sci. Rev. 2001, 29, 103–108. [Google Scholar] [CrossRef]
- Pedišić, Ž.; Dumuid, D.; Olds, T.S. Integrating sleep, sedentary behaviour, and physical activity research in the emerging field of time-use epidemiology: Definitions, concepts, statistical methods, theoretical framework, and future directions. Kinesiology 2017, 49, 1–18. [Google Scholar]
- Olds, T.; Burton, N.W.; Sprod, J.; Maher, C.A.; Ferrar, K.; Brown, W.J.; Van Uffelen, J.; Dumuid, D. One day you’ll wake up and won’t have to go to work: The impact of changes in time use on mental health following retirement. PLoS ONE 2018, 13, e0199605. [Google Scholar] [CrossRef]
- Janurek, J.; Hadi, S.A.; Mojzisch, A.; Häusser, J.A. The association of the 24 hour distribution of time spent in physical activity, work, and sleep with emotional exhaustion. Int. J. Environ. Res. Public Health 2018, 15, 1927. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGregor, D.; Carson, V.; Palarea-Albaladejo, J.; Dall, P.; Tremblay, M.; Chastin, S. Compositional analysis of the associations between 24-h movement behaviours and health indicators among adults and older adults from the canadian health measure survey. Int. J. Environ. Res. Public Health 2018, 15, 1779. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del Pozo-Cruz, B.; Alfonso-Rosa, R.M.; McGregor, D.; Chastin, S.F.; Palarea-Albaladejo, J.; Del Pozo-Cruz, J. Sedentary behaviour is associated with depression symptoms: Compositional data analysis from a representative sample of 3233 US adults and older adults assessed with accelerometers. J. Affect. Disord. 2020, 265, 59–62. [Google Scholar] [CrossRef] [PubMed]
- Curtis, R.G.; Dumuid, D.; Olds, T.; Plotnikoff, R.; Vandelanotte, C.; Ryan, J.; Edney, S.; Maher, C. The association between time-use behaviors and physical and mental well-being in adults: A compositional isotemporal substitution analysis. J. Phys. Act. Health 2020, 17, 197–203. [Google Scholar] [CrossRef]
- Clemes, S.; O’connell, S.E.; Edwardson, C.L. Office workers’ objectively measured sedentary behavior and physical activity during and outside working hours. J. Occup. Environ. Med. 2014, 56, 298–303. [Google Scholar] [CrossRef] [Green Version]
- Parry, S.; Straker, L. The contribution of office work to sedentary behaviour associated risk. BMC Public Health 2013, 13, 296. [Google Scholar] [CrossRef] [Green Version]
- Thorp, A.A.; Healy, G.N.; Winkler, E.A.H.; Clark, B.K.; Gardiner, P.A.; Owen, N.; Dunstan, D.W. Prolonged sedentary time and physical activity in workplace and non-work contexts: A cross-sectional study of office, customer service and call centre employees. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 128. [Google Scholar] [CrossRef] [Green Version]
- Rosenberger, M.E.; Fulton, J.E.; Buman, M.P.; Troiano, R.P.; Grandner, M.A.; Buchner, D.M.; Haskell, W.L. The 24-hour activity cycle. Med. Sci. Sports Exerc. 2019, 51, 454–464. [Google Scholar] [CrossRef]
- Nooijen, C.F.J.; Blom, V.; Ekblom, Ö.; Ekblom, M.M.; Kallings, L.V. Improving office workers’ mental health and cognition: A 3-arm cluster randomized controlled trial targeting physical activity and sedentary behavior in multi-component interventions. BMC Public Health 2019, 19, 266. [Google Scholar] [CrossRef] [Green Version]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Shirom, A.; Melamed, S. A comparison of the construct validity of two burnout measures in two groups of professions. Int. J. Stress Manag. 2006, 13, 176–200. [Google Scholar] [CrossRef]
- Bech, P.; Olsen, L.R.; Kjoller, M.; Rasmussen, N.K. Measuring well-being rather than the absence of distress symptoms: A comparison of the SF-36 mental health subscale and the WHO-Five well-being scale. Int. J. Methods Psychiatr. Res. 2006, 12, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Elo, A.; Leppänen, A.; Jahkola, A. Validity of a single-item measure of stress symptoms O riginal article. Scand. J. Work Environ. Health 2003, 2003, 444–451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibbs, B.B.; Kline, C.E. When does sedentary behavior become sleep? A proposed framework for classifying activity during sleep-wake transitions. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 81. [Google Scholar] [CrossRef]
- Matricciani, L.; Bin, Y.S.; Lallukka, T.; Kronholm, E.; Wake, M.; Paquet, C.; Dumuid, D.; Olds, T. Rethinking the sleep-health link. Sleep Health 2018, 4, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Cole, R.J.; Kripke, D.F.; Gruen, W.; Mullaney, D.J.; Gillin, J.C. Automatic sleep/wake identification from wrist activity. Sleep 1992, 15, 461–469. [Google Scholar] [CrossRef]
- Aili, K.; Åström-Paulsson, S.; Stoetzer, U.; Svartengren, M.; Hillert, L. Reliability of actigraphy and subjective sleep measurements in adults: The design of sleep assessments. J. Clin. Sleep Med. 2017, 13, 39–47. [Google Scholar] [CrossRef]
- Aguilar-Farias, N.; Brown, W.J.; Peeters, G.M.E.E. ActiGraph GT3X+ cut-points for identifying sedentary behaviour in older adults in free-living environments. J. Sci. Med. Sport 2014, 17, 293–299. [Google Scholar] [CrossRef]
- Sasaki, J.; John, D.; Freedson, P.S. Validation and comparison of ActiGraph activity monitors. J. Sci. Med. Sport 2011, 14, 411–416. [Google Scholar] [CrossRef]
- Migueles, J.H.; Cadenas-Sanchez, C.; Ekelund, U.; Nyström, C.D.; Mora-Gonzalez, J.; Löf, M.; Labayen, I.; Ruiz, J.R.; Ortega, F.B. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: A systematic review and practical considerations. Sports Med. 2017, 47, 1821–1845. [Google Scholar] [CrossRef]
- Björkman, F.; Ekblom-Bak, E.; Ekblom, Örjan; Ekblom, B. Validity of the revised Ekblom Bak cycle ergometer test in adults. Eur. J. Appl. Physiol. 2016, 116, 1627–1638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dumuid, D.; Pedisic, Z.; Stanford, T.E.; Martín-Fernández, J.; Hron, K.; Maher, C.A.; Lewis, L.K.; Olds, T. The compositional isotemporal substitution model: A method for estimating changes in a health outcome for reallocation of time between sleep, physical activity and sedentary behaviour. Stat. Methods Med Res. 2019, 28, 846–857. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2013. [Google Scholar]
- Van den Boogaart, K.; Tolosana-Delgado, R. “Compositions”: A unified R package to analyze compositional data. Comput. Geosci. 2008, 34, 320–338. [Google Scholar] [CrossRef]
- Norman, G. Likert scales, levels of measurement and the “laws” of statistics. Adv. Health Sci. Educ. 2010, 15, 625–632. [Google Scholar] [CrossRef]
- Loe, H.; Rognmo, Ø.; Saltin, B.; Wisløff, U. Aerobic capacity reference data in 3816 healthy men and women 20–90 Years. PLoS ONE 2013, 8, e64319. [Google Scholar] [CrossRef]
- Hagströmer, M.; Oja, P.; Sjöström, M. Physical activity and inactivity in an adult population assessed by accelerometry. Med. Sci. Sports Exerc. 2007, 39, 1502–1508. [Google Scholar] [CrossRef]
- Rebar, A.L.; Stanton, R.; Geard, D.; Short, C.E.; Duncan, M.J.; Vandelanotte, C. A Meta-Meta-Analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol. Rev. 2015, 9, 366–378. [Google Scholar] [CrossRef]
- Lewthwaite, H.; Olds, T.S.; Williams, M.T.; Effing, T.W.; Dumuid, D. Use of time in chronic obstructive pulmonary disease: Longitudinal associations with symptoms and quality of life using a compositional analysis approach. PLoS ONE 2019, 14, e0214058. [Google Scholar] [CrossRef] [Green Version]
- Tremblay, M.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.; Altenburg, T.M.; Chinapaw, M.J.; on behalf of SBRN Terminology Consensus Project Participants. Sedentary behavior research network (SBRN)—Terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [Green Version]
- Teychenne, M.; White, R.L.; Richards, J.; Schuch, F.B.; Rosenbaum, S.; Bennie, J. Do we need physical activity guidelines for mental health: What does the evidence tell us? Ment. Health Phys. Act. 2020, 18, 100315. [Google Scholar] [CrossRef]
| Depression N = 349 | Anxiety N = 348 | Burnout N = 345 | Mental Wellbeing N = 370 | Stress N = 368 | ||
|---|---|---|---|---|---|---|
| Mental health outcomes | Global score (mean ± SD) | 3.2 ± 2.8 | 6.3 ± 3.7 | 2.0 ± 0.8 | 60.8 ± 17.8 | 2.7 ± 1.2 |
| N (%) | Normal: 320 (91.7%) Borderline abnormal: 21 (6%) Abnormal: 8 (2.3%) | Normal: 226 (64.9%) Borderline abnormal: 73 (21%) Abnormal: 49 (14.1%) | Healthy: 279 (80.9%) Low burnout: 64 (18.6%) High burnout: 2 (0.6%) | Good mood: 277 (74.9%) Low mood: 69 (18.6%) Likely depression: 24 (6.5%) | Less than a few times per month or never: 61 (16.6%) A few times per month: 116 (31.5%) Once per week: 86 (23.4%) Several times per week: 77 (20.9%) Every day: 28 (7.6%) | |
| Covariates | Age (years) (mean ± SD) | 41 ± 9 | 41 ± 9 | 41 ± 9 | 41 ± 9 | 41 ± 9 |
| Sex (male), N (%) | 111 (32) | 111 (32) | 109 (32) | 117 (32) | 116 (32) | |
| Education, N (%) Primary school Gymnasium University or higher academic education | 8 (2.3) 105 (30.1) 236 (67.6) | 7 (2.0) 104 (29.9) 237 (68.1) | 5 (1.4) 104 (30.1) 236 (68.4) | 8 (2.2) 112 (30.3) 250 (67.6) | 8 (2.2) 112 (30.4) 248 (67.4) | |
| Fitness (ml kg−1 min−1) (mean ± SD) | 39.7 ± 8 | 39.8 ± 8 | 39.6 ± 8 | 39.5 ± 8 | 39.5 ± 8 | |
| Sleep efficiency (mean ± SD) | 90.2 ± 4 | 90.3 ± 4 | 90.3 ± 4 | 90.2 ± 4 | 90.2 ± 4 | |
| Compositional mean for movement-related behaviors in minutes (% of 24 h) | MVPA | 62 (4%) | 62 (4%) | 61 (4%) | 62 (4%) | 62 (4%) |
| LIPA | 326 (22%) | 326 (23%) | 327 (23%) | 327 (23%) | 327 (23%) | |
| SED | 577 (40%) | 576 (40%) | 576 (40%) | 575 (40%) | 575 (40%) | |
| Time in bed | 475 (33%) | 476 (33%) | 475 (33%) | 476 (33%) | 476 (33%) | |
| Mental Health Outcomes | Crude Model | Adjusted Model | Fully Adjusted Model |
|---|---|---|---|
| Depression | 0.867 | 0.873 | 0.627 |
| Anxiety | 0.574 | 0.717 | 0.635 |
| Burnout | 0.282 | 0.266 | 0.459 |
| Mental wellbeing | 0.126 | 0.105 | 0.261 |
| Stress | 0.653 | 0.869 | 0.837 |
| Mental Health Outcomes | Crude Model | Adjusted Model | Fully Adjusted Model | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MVPA | LIPA | SED | Time in Bed | MVPA | LIPA | SED | Time in Bed | MVPA | LIPA | SED | Time in Bed | |
| Depression | −0.02 (0.964) | 0.40 (0.621) | −0.66 (0.520) | 0.29 (0.834) | 0.003 (0.995) | 0.43 (0.593) | -0.61 (0.567) | 0.17 (0.904) | 0.18 (0.721) | 0.71 (0.377) | −0.76 (0.478) | −0.13 (0.926) |
| Anxiety | −0.03 (0.966) | 1.0 (0.350) | −1.28 (0.343) | 0.31 (0.866) | −0.16 (0.799) | 1.14 (0.286) | −0.53 (0.703) | −0.45 (0.807) | −0.08 (0.899) | 1.30 (0.227) | −0.57 (0.684) | −0.645 (0.727) |
| Burnout | −0.23 (0.094) | −0.07 (0.769) | −0.24 (0.389) | 0.54 (0.163) | −0.25 (0.065) | −0.04 (0.851) | −0.13 (0.661) | 0.42 (0.280) | −0.20 (0.148) | 0.02 (0.944) | −0.21 (0.472) | 0.39 (0.312) |
| Mental wellbeing | 7.01 * (0.019) | −3.69 (0.460) | −1.61 (0.793) | −1.72 (0.838) | 7.1 * (0.018) | −3.72 (0.458) | −3.66 (0.561) | 0.28 (0.974) | 5.48 (0.0668 | −6.14 (0.217) | −0.49 (0.938) | 1.15 (0.891) |
| Stress | 0.10 (0.614) | −0.06 (0.851) | −0.46 (0.262) | 0.42 (0.454) | 0.10 (0.621) | −0.07 (0.834) | −0.27 (0.517) | 0.24 (0.670) | 0.12 (0.553) | −0.03 (0.930) | −0.29 (0.50) | 0.20 (0.734) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Larisch, L.-M.; Kallings, L.V.; Hagströmer, M.; Desai, M.; von Rosen, P.; Blom, V. Associations between 24 h Movement Behavior and Mental Health in Office Workers. Int. J. Environ. Res. Public Health 2020, 17, 6214. https://doi.org/10.3390/ijerph17176214
Larisch L-M, Kallings LV, Hagströmer M, Desai M, von Rosen P, Blom V. Associations between 24 h Movement Behavior and Mental Health in Office Workers. International Journal of Environmental Research and Public Health. 2020; 17(17):6214. https://doi.org/10.3390/ijerph17176214
Chicago/Turabian StyleLarisch, Lisa-Marie, Lena V. Kallings, Maria Hagströmer, Manisha Desai, Philip von Rosen, and Victoria Blom. 2020. "Associations between 24 h Movement Behavior and Mental Health in Office Workers" International Journal of Environmental Research and Public Health 17, no. 17: 6214. https://doi.org/10.3390/ijerph17176214





