Impact of Psycho-Social Factors on Fatigue among Breast Cancer Patients Who Are Currently Undergoing Radiotherapy
Abstract
1. Introduction
Background
2. The Study
2.1. Aims
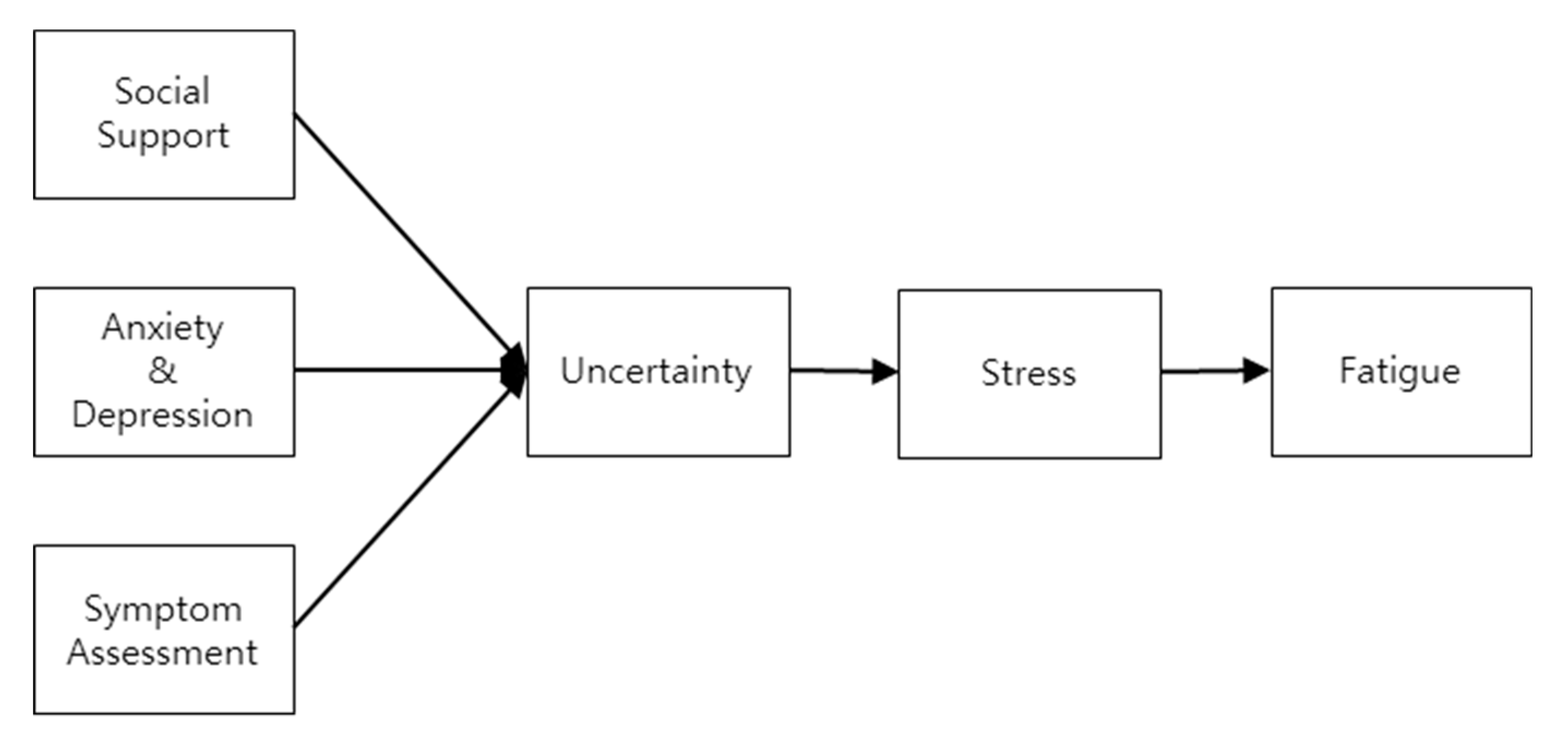
2.2. Design
2.3. Participants
- (1)
- Being a breast cancer survivor 18 years of age or older, diagnosed with breast cancer, and undergoing only radiotherapy and chemotherapy after surgery;
- (2)
- Understanding the questionnaire;
- (3)
- Voluntarily agreeing to participate in the research.
- (1)
- Currently diagnosed with a mental health disorder by a psychiatrist and not taking anti-psychotic medications;
- (2)
- Affected by any cancer other than breast cancer.
2.4. Sample Size
2.5. Measurements
2.5.1. Validity and Reliability
2.5.2. Symptom Assessment
2.5.3. Anxiety and Depression
2.5.4. Social Support
2.5.5. Uncertainty
2.5.6. Stress
2.5.7. Fatigue
2.6. Data Collection
2.7. Ethical Cconsideration
2.8. Statistical Analysis
3. Results
3.1. Demographic and Cancer-Related Participant Characteristics
3.2. Descriptive Analysis of Included Variables
3.3. Structural Model
4. Discussion
4.1. Clinical Implications
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- American Cancer Society. Survival Rates for Breast Cancer. 2020. Available online: https://www.cancer.org/cancer/breast-cancer/understanding-a-breast-cancer-diagnosis/breast-cancer-survival-rates.html (accessed on 2 April 2020).
- National Cancer Information Center. Statistics of Cancer. 2019. Available online: https://www.cancer.go.kr/lay1/S1T639C641/contents.do (accessed on 2 January 2019).
- Lee, J.A.; Yu, J.H.; Song, Y.M. Management of Long-Term Breast Cancer Survivors in Korea. J. Korean Med. Assoc. 2016, 59, 266–275. [Google Scholar] [CrossRef]
- Ligt, K.M.D.; Heins, M.; Verloop, J.; Smorenburg, C.H.; Korevaar, J.C.; Siesling, S. Patient-Reported Health Problems and Health Care Use After Treatment for Early Breast Cancer. Breast 2019, 46, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Whisenant, M.; Wong, B.; Mitchell, S.A.; Beck, S.L.; Mooney, K. Distinct Trajectories of Fatigue and Sleep Disturbance in Women Receiving Chemotherapy for Breast Cancer. Oncol. Nurs. Forum 2017, 44, 739–750. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Dong, J.N.; Sun, P.; Feng, C.; Liu, Y.C. Effect of Therapeutic Care for Treating Fatigue in Patients with Breast Cancer Receiving Chemotherapy. Medicine 2017, 96, e7750. [Google Scholar] [CrossRef] [PubMed]
- Ploos van Amstel, F.K.P.; van den Berg, S.W.; van Laarhoven, H.W.; Gielissen, M.F.; Prins, J.B.; Ottevanger, P.B. Distress Screening Remains Important During Follow-up After Primary Breast Cancer Treatment. Support. Care Cancer 2013, 21, 2107–2115. [Google Scholar] [CrossRef]
- Andic, F.; Miller, A.H.; Brown, G.; Chu, L.; Lin, J.; Liu, T.; Sertdemir, Y.; Torres, M.A. Instruments for Determining Clinically Relevant Fatigue in Breast Cancer Patients During Radiotherapy. Breast Cancer 2020, 27, 197–205. [Google Scholar] [CrossRef]
- Muszalik, M.; Kołucka-Pluta, M.; Kędziora-Kornatowska, K.; Robaczewska, J. Quality of Life of Women with Breast Cancer Undergoing Radiotherapy Using the Functional Assessment of Chronic Illness Therapy-Fatigue Questionnaire. Clin. Interv. Aging 2016, 11, 1489–1494. [Google Scholar] [CrossRef][Green Version]
- Abrahams, H.J.G.; Gielissen, M.F.M.; Verhagen, C.A.H.H.V.M.; Knoop, H. The Relationship of Fatigue in Breast Cancer Survivors with Quality of Life and Factors to Address in Psychological Interventions: A Systematic Review. Clin. Psychol. Rev. 2018, 63, 1–11. [Google Scholar] [CrossRef]
- Reinertsen, K.V.; Engebraaten, O.; Loge, J.H.; Cvancarova, M.; Naume, B.; Wist, E.; Edvardsen, H.; Wille, E.; Bjøro, T.; Kiserud, C.E. Fatigue During and After Breast Cancer Therapy a Prospective Study. J. Pain Symptom Manag. 2017, 53, 551–560. [Google Scholar] [CrossRef]
- Kagee, A.; Roomaney, R.; Knoll, N. Psychosocial Predictors of Distress and Depression Among South African Breast Cancer Patients. Psychooncology 2018, 27, 908–914. [Google Scholar] [CrossRef]
- Pahlevan Sharif, S.S.; Ahadzadeh, A.S.; Perdamen, H.K. Uncertainty and Quality of Life of Malaysian Women with Breast Cancer: Mediating Role of Coping Styles and Mood States. Appl. Nurs. Res. 2017, 38, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Fradelos, E.C.; Papathanasiou, I.V.; Veneti, A.; Daglas, A.; Christodoulou, E.; Zyga, S.; Kourakos, M. Psychological Distress and Resilience in Women Diagnosed with Breast Cancer in Greece. Asian Pac. J. Cancer Prev. 2017, 18, 2545–2550. [Google Scholar] [PubMed]
- Kishan, A.U.; Wang, P.C.; Sharif, J.; Kupelian, P.A.; Steinberg, M.L.; McCloskey, S.A. Clinical Indicators of Psycho- Social Distress Predict for Acute Radiation-Induced Fatigue in Patients Receiving Adjuvant Radiation Therapy for Breast Cancer: An Analysis of Patient-Reported Outcomes. Int. J. Radiat. Oncol. Biol. Phys. 2016, 95, 946–955. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.E.; Wiskemann, J.; Schneeweiss, A.; Potthoff, K.; Ulrich, C.M.; Steindorf, K. Determinants of Physical, Affective, and Cognitive Fatigue During Breast Cancer Therapy and 12 Months Follow-Up. Int. J. Cancer 2018, 142, 1148–1157. [Google Scholar] [CrossRef]
- Fagundes, C.P.; Lindgren, M.E.; Shapiro, C.L.; Kiecolt-Glaser, J.K. Child Maltreatment and Breast Cancer Survivors: Social Support Makes a Difference for Quality of Life, Fatigue and Cancer Stress. Eur. J. Cancer 2012, 48, 728–736. [Google Scholar] [CrossRef]
- Lipsett, A.; Barrett, S.; Haruna, F.; Mustian, K.; O’Donovan, A. The Impact of Exercise During Adjuvant Radiotherapy for Breast Cancer on Fatigue and Quality of Life: A Systematic Review and Meta-Analysis. Breast 2017, 32, 144–155. [Google Scholar] [CrossRef]
- Matias, M.; Baciarello, G.; Neji, M.; Di Meglio, A.; Michiels, S.; Partridge, A.H.; Bendiane, M.K.; Fizazi, K.; Ducreux, M.; Andre, F.; et al. Fatigue and Physical Activity in Cancer Survivors: A Cross-Sectional Population–Based Study. Cancer Med. 2019, 8, 2535–2544. [Google Scholar] [CrossRef]
- Bower, J.E.; Wiley, J.; Petersen, L.; Irwin, M.R.; Cole, S.W.; Ganz, P.A. Fatigue After Breast Cancer Treatment: Biobehavioral Predictors of Fatigue Trajectories. Health Psychol. 2018, 37, 1025–1034. [Google Scholar] [CrossRef]
- Pearson, E.J.M.; McKinstry, C.E.; Morris, M.E. Which Clinical Practice Guideline for Cancer-Related Fatigue Is the Most Suitable for Application in Australia? Asia Pac. J. Clin. Oncol. 2015, 11, 111. [Google Scholar]
- Andersen, E.R.; Eilertsen, G.; Myklebust, A.M.; Eriksen, S. Women’s Experience of Acute Skin Toxicity Following Radiation Therapy in Breast Cancer. J. Multidiscip. Healthc. 2018, 11, 139–148. [Google Scholar] [CrossRef]
- Radvansky, L.J.; Pace, M.B.; Siddiqui, A. Prevention and Management of Radiation-Induced Dermatitis, Mucositis, and Xerostomia. Am. J. Health Syst. Pharm. 2013, 70, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Brosschot, J.F.; Verkuil, B.; Thayer, J.F. Exposed to Events That Never Happen: Generalized Unsafety, the Default Stress Response, and Prolonged Autonomic Activity. Neurosci. Biobehav. Rev. 2017, 74, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Bae, S.H.; Chun, M.; Jung, Y.S.; Jung, Y.M. Factors Influencing Elevated Distress Scores at the End of Primary Treatment of Breast Cancer. Asian Oncol. Nurs. 2015, 15, 132–139. [Google Scholar] [CrossRef]
- Oh, Y.K.; Hwang, S.Y. Impact of Uncertainty on the Quality of Life of Young Breast Cancer Patients: Focusing on Mediating Effect of Marital Intimacy. J. Korean Acad. Nurs. 2018, 48, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Shand, L.K.; Cowlishaw, S.; Brooker, J.E.; Burney, S.; Ricciardelli, L.A. Correlates of Post Traumatic Stress Symptoms and Growth in Cancer Patients: A Systematic Review and Meta-Analysis. Psychooncology 2015, 24, 624–634. [Google Scholar] [CrossRef]
- Weston, R.; Gore, P.A., Jr. A Brief Guide to Structural Equation Modeling. Couns. Psychol. 2006, 34, 719–751. [Google Scholar] [CrossRef]
- Chang, V.T.; Hwang, S.S.; Feuerman, M.; Kasimis, B.S.; Thaler, H.T. The Memorial Symptom Assessment Scale Short Form(MSAS-SF) Validity and Reliability. Cancer 2000, 89, 1162–1171. [Google Scholar] [CrossRef]
- Nho, J.H.; Kim, S.R.; Chang, V.T.; Nam, J.H. Reliability and Validity of the Korean Memorial Symptom Assessment Scale-Short Form in Gynecological Cancer Patients. J. Pain Symptom Manag. 2018, 55, 101–107. [Google Scholar] [CrossRef]
- Thompson, P. The Relationship of Fatigue and Meaning in Life in Breast Cancer Survivors. Oncol. Nurs. Forum 2007, 34, 653–660. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Oh, S.M.; Min, K.J.; Park, D. A Study on the Standardization of the Hospital Anxiety and Depression Scale for Koreans. J. Korean Neuropsychiatr. Assoc. 1999, 38, 289–296. [Google Scholar]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Shin, J.S.; Lee, Y.B. The Effects of Social Supports on Psychosocial Well-Being of the Unemployed. Korean J. Soc. Welf. 1999, 37, 241–269. [Google Scholar]
- Kim, H.Y.; So, H.S. A Structural Model for Psychosocial Adjustment in Patients with Early Breast Cancer. J. Korean Acad. Nurs. 2012, 42, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Mishel, M.H. The Measurement of Uncertainty in Illness. Nurs. Res. 1981, 30, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kessler, R.C.; Gordon, L.U. Measuring Stress: A Guide for Health and Social Scientists; Oxford University Press on Demand: New York, NY, USA, 1997. [Google Scholar]
- Lee, J.; Shin, C.; Ko, Y.H.; Lim, J.; Joe, S.H.; Kim, S.; Jung, I.K.; Han, C. The Reliability and Validity Studies of the Korean Version of the Perceived Stress Scale. Korean J. Psychosom. Med. 2012, 20, 127–134. [Google Scholar]
- Hur, J. AMOS for Structural Equation Model; Hanarae Academy: Seoul, Korea, 2013. [Google Scholar]
- So, W.K.; Leung, D.Y.; Ho, S.S.; Lai, E.T.; Sit, J.W.; Chan, C.W. Associations Between Social Support, Prevalent Symptoms and Health-Related Quality of Life in Chinese Women Undergoing Treatment for Breast Cancer: A Cross-Sectional Study Using Structural Equation Modelling. Eur. J. Oncol. Nurs. 2013, 17, 442–448. [Google Scholar] [CrossRef]
- Kim, K.; Lee, M.; Kwak, Y.; Kim, J. Factors Affecting the Fatigue of Hospitalized Women Cancer Patients Receiving Chemotherapy. Asian Oncol. Nurs. 2014, 14, 182–190. [Google Scholar] [CrossRef][Green Version]
- Edib, Z.; Kumarasamy, V.; Binti Abdullah, N.; Rizal, A.M.; Al-Dubai, S.A.R. Most prevalent unmet supportive care needs and quality of life of breast cancer patients in a tertiary hospital in Malaysia. Health Qual. Life Outcomes 2016, 14, 14–26. [Google Scholar] [CrossRef]
- Hall, D.L.; Mishel, M.H.; Germino, B.B. Living with Cancer-Related Uncertainty: Associations with Fatigue, Insomnia, and Affect in Younger Breast Cancer Survivors. Support. Care Cancer 2014, 22, 2489–2495. [Google Scholar] [CrossRef]
- Harvey, S.B.; Modini, M.; Joyce, S.; Milligan-Saville, J.S.; Tan, L.; Mykletun, A.; Bryant, R.A.; Christensen, H.; Mitchell, P.B. Can Work Make You Mentally Ill? A Systematic Meta Review of Work Related Risk Factors for Common Mental Health Problems. Occup. Environ. Med. 2017, 74, 301–310. [Google Scholar] [PubMed]
- Levkovich, I.; Cohen, M.; Alon, S.; Kuchuk, I.; Nissenbaum, B.; Evron, E.; Pollack, S.; Fried, G. Symptom Cluster of Emotional Distress, Fatigue and Cognitive Difficulties Among Young and Older Breast Cancer Survivors: The Mediating Role of Subjective Stress. J. Geriatr. Oncol. 2018, 9, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Juvet, L.K.; Thune, I.; Elvsaas, I.K.Ø.; Fors, E.A.; Lundgren, S.; Bertheussen, G.; Leivseth, G.; Oldervoll, L.M. The Effect of Exercise on Fatigue and Physical Functioning in Breast Cancer Patients During and After Treatment and at 6 Months Follow-up: A Meta-Analysis. Breast 2017, 33, 166–177. [Google Scholar] [CrossRef] [PubMed]
- Van Vulpen, J.K.; Peeters, P.H.; Velthuis, M.J.; van der Wall, E.; May, A.M. Effects of Physical Exercise During Adjuvant Breast Cancer Treatment on Physical and Psychosocial Dimensions of Cancer-Related Fatigue: A Meta-Analysis. Maturitas 2016, 85, 104–111. [Google Scholar] [CrossRef]

| Variables | Classification | n(%) Mean ± SD |
|---|---|---|
| Age | 48.09 ± 8.50 | |
| Spouse | Yes | 178 (84.8) |
| No | 32 (15.2) | |
| Education Level | <=middle school | 7 (3.3) |
| High school | 37 (17.6) | |
| University | 137 (65.2) | |
| >=Graduate school | 29 (13.8) | |
| Job | Have | 103 (49.0) |
| None | 107 (51.0) | |
| Cancer Stage | 0 | 2 (1.0) |
| 1 | 104 (49.5) | |
| 2 | 82 (39.4) | |
| 3 | 18 (8.7) | |
| 4 | 2 (1.0) | |
| Type of Mastectomy | Total | 47 (22.4) |
| Partial | 163 (77.6) | |
| Radiation therapy (week) | 1st | 16 (8.2) |
| 2nd | 46 (23.5) | |
| 3rd | 68 (34.7) | |
| 4th | 48 (24.5) | |
| over 5th | 18 (9.2) |
| Variables | Mean ± SD | Range | Skewness | Kurtosis | |
|---|---|---|---|---|---|
| SA | Physical symptoms | 1.01 ± 0.67 | 0–4 | 1.64 | 3.26 |
| Psychological symptoms | 1.84 ± 1.10 | 0–4 | 0.00 | −0.98 | |
| HADS | Anxiety | 1.24 ± 0.58 | 0–3 | 0.20 | −0.27 |
| Depression | 1.54 ± 0.64 | 0–3 | −0.07 | −0.83 | |
| Social support | Family | 3.98 ± 0.81 | 1–5 | −0.817 | 0.72 |
| Friends | 2.89 ± 1.08 | 1–5 | 0.07 | −0.70 | |
| Significant others | 2.69 ± 1.21 | 1–5 | 0.21 | −1.05 | |
| Uncertainty | Ambiguity | 3.28 ± 0.78 | 1–5 | −0.33 | −0.36 |
| Complexity | 3.08 ± 0.67 | 1–5 | −0.27 | −0.01 | |
| Unpredictability | 3.09 ± 0.68 | 1–5 | −0.36 | −0.21 | |
| Stress | 2.30 ± 0.78 | 0–4 | −0.08 | −0.28 | |
| Fatigue | 2.47 ± 0.94 | 0–4 | −0.54 | −0.51 | |
| Endogenous Variables | Predictor Variables | SEW (ß) | SE | CR (p) | Direct Effect (p) | Indirect Effect (p) | Total Effect (p) | SMC |
|---|---|---|---|---|---|---|---|---|
| SA | AD | 0.63 | 0.10 | 4.77 (<0.001) | 0.63 (0.004) | - | 0.63 (0.004) | 0.315 |
| Social support | 0.21 | 0.04 | 2.03 (0.053) | 0.21 (0.217) | −0.30 (0.004) | −0.08 (0.615) | ||
| AD | Social support | −0.47 | 0.05 | −4.32 (<0.001) | −0.47 (0.004) | - | −0.47 (0.004) | 0.220 |
| Uncertainty | SA | 0.35 | 0.18 | 4.22 (<0.001) | 0.35 (0.004) | - | 0.35 (0.004) | 0.567 |
| AD | 0.47 | 0.15 | 5.17 (<0.001) | 0.47 (0.004) | 0.22 (0.004) | 0.69 (0.004) | ||
| Social support | −0.08 | 0.06 | −1.04 (0.301) | −0.08 (0.576) | −0.25 (0.006) | −0.33 (0.005) | ||
| Stress | SA | 0.29 | 0.17 | 3.74 (<0.001) | 0.29 (0.004) | 0.13 (0.004) | 0.42 (.004) | 0.646 |
| AD | 0.26 | 0.13 | 3.24 (0.001) | 0.26 (0.007) | 0.43 (0.004) | 0.69 (0.004) | ||
| Social support | −0.06 | 0.06 | −0.85 (0.398) | −0.06 (0.532) | −0.26 (0.004) | −0.32 (0.016) | ||
| Uncertainty | 0.36 | 0.08 | 4.69 (<0.001) | 0.36 (0.004) | - | 0.36 (0.004) | ||
| Fatigue | SA | 0.22 | 0.20 | 2.91 (0.004) | 0.22 (0.012) | 0.17 (0.005) | 0.39 (0.004) | 0.672 |
| AD | 0.26 | 0.15 | 3.46 (<0.001) | 0.26 (0.020) | 0.46 (0.004) | 0.72 (0.004) | ||
| Social support | −0.03 | 0.06 | −0.41 (0.680) | −0.03 (0.835) | −0.029 (0.007) | −0.32 (0.004) | ||
| Uncertainty | 0.29 | 0.09 | 3.95 (<0.001) | 0.29 (0.004) | 0.06 (0.044) | 0.36 (0.004) | ||
| Stress | 0.17 | 0.09 | 2.29 (0.022) | 0.17 (0.044) | - | 0.17 (0.044) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, H.; Kim, K. Impact of Psycho-Social Factors on Fatigue among Breast Cancer Patients Who Are Currently Undergoing Radiotherapy. Int. J. Environ. Res. Public Health 2020, 17, 6092. https://doi.org/10.3390/ijerph17176092
Park H, Kim K. Impact of Psycho-Social Factors on Fatigue among Breast Cancer Patients Who Are Currently Undergoing Radiotherapy. International Journal of Environmental Research and Public Health. 2020; 17(17):6092. https://doi.org/10.3390/ijerph17176092
Chicago/Turabian StylePark, Hyesun, and Kisook Kim. 2020. "Impact of Psycho-Social Factors on Fatigue among Breast Cancer Patients Who Are Currently Undergoing Radiotherapy" International Journal of Environmental Research and Public Health 17, no. 17: 6092. https://doi.org/10.3390/ijerph17176092
APA StylePark, H., & Kim, K. (2020). Impact of Psycho-Social Factors on Fatigue among Breast Cancer Patients Who Are Currently Undergoing Radiotherapy. International Journal of Environmental Research and Public Health, 17(17), 6092. https://doi.org/10.3390/ijerph17176092





