On the Optimal Indoor Air Conditions for SARS-CoV-2 Inactivation. An Enthalpy-Based Approach
Abstract
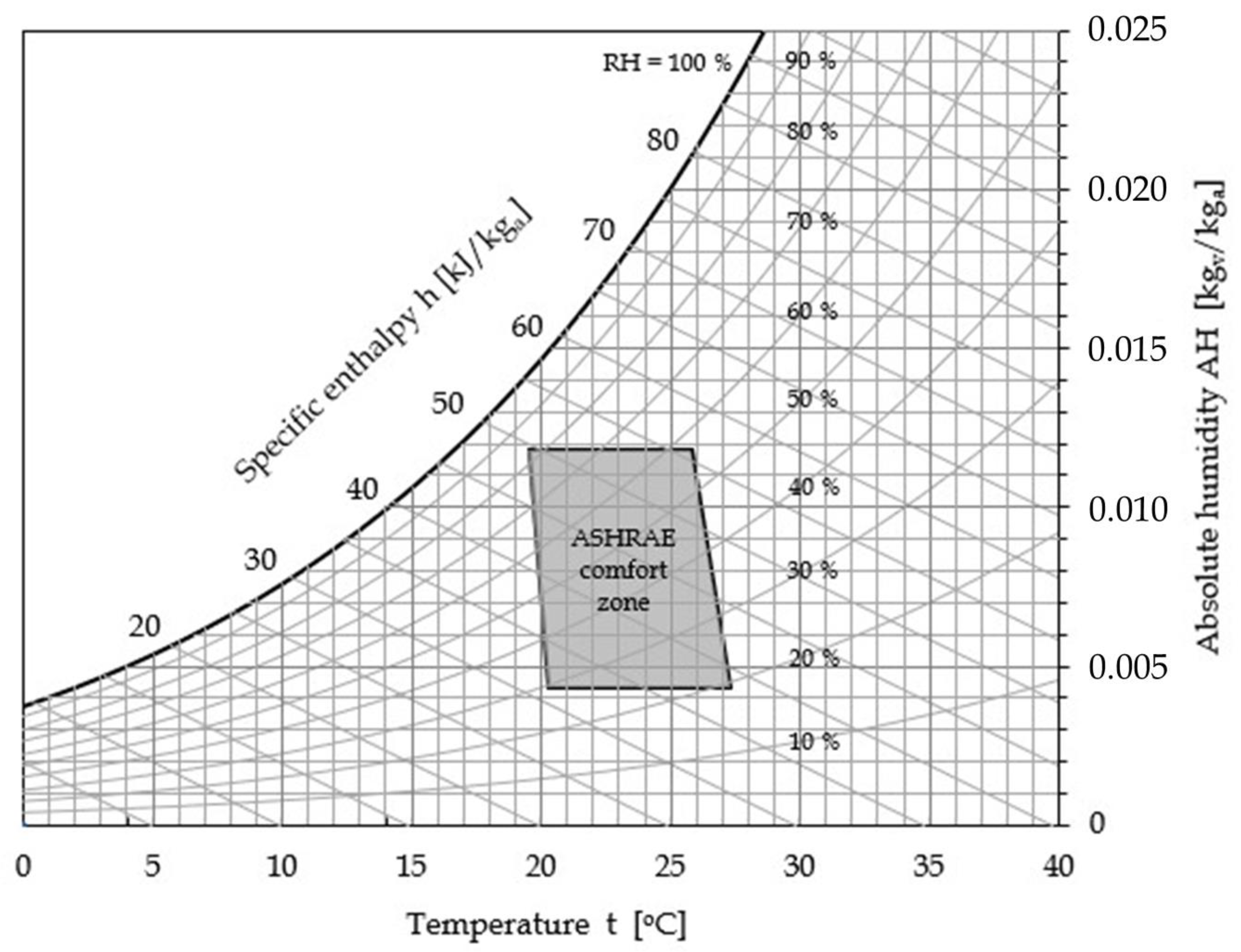
1. Introduction
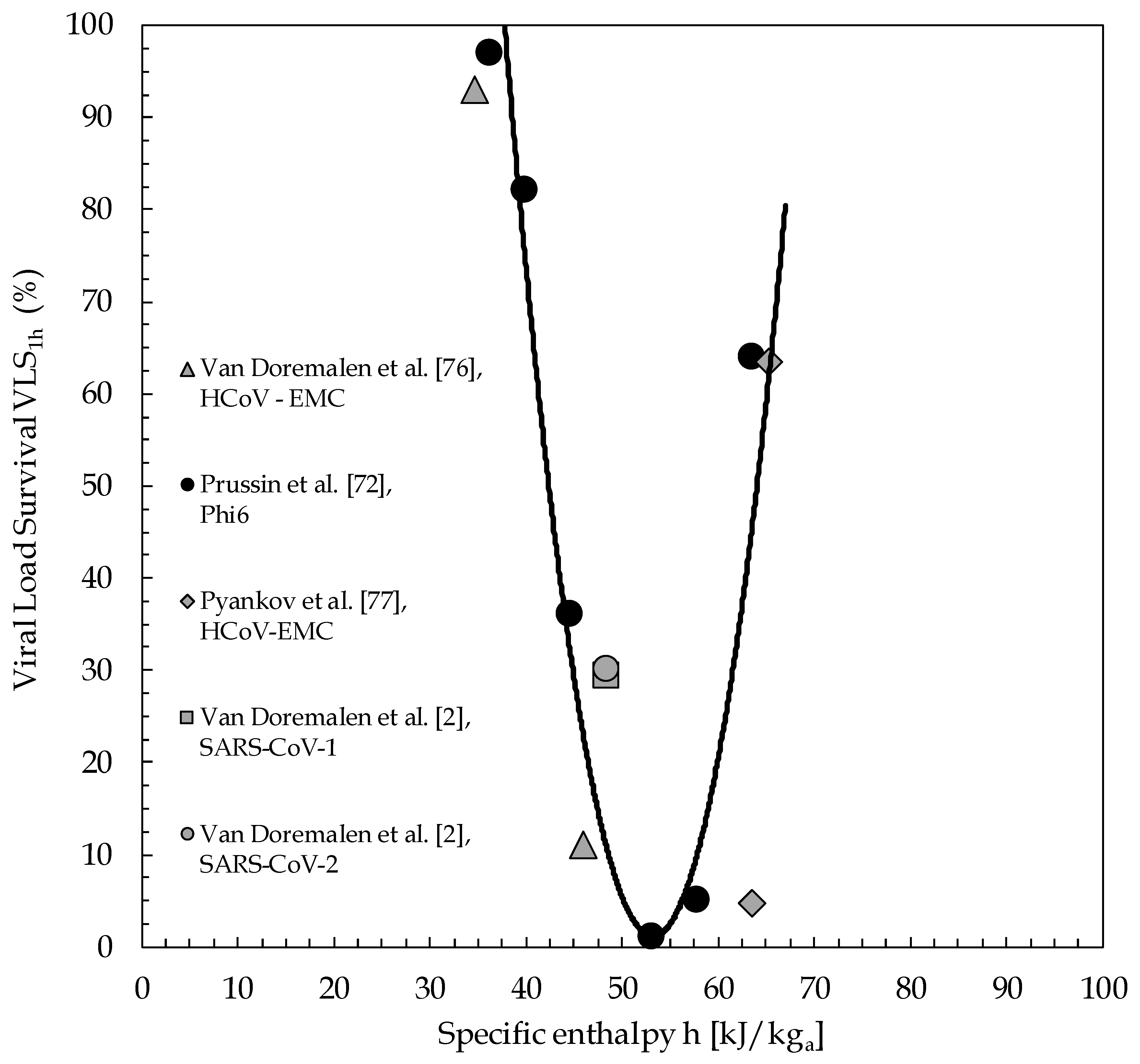
2. Material and Methods
2.1. Background
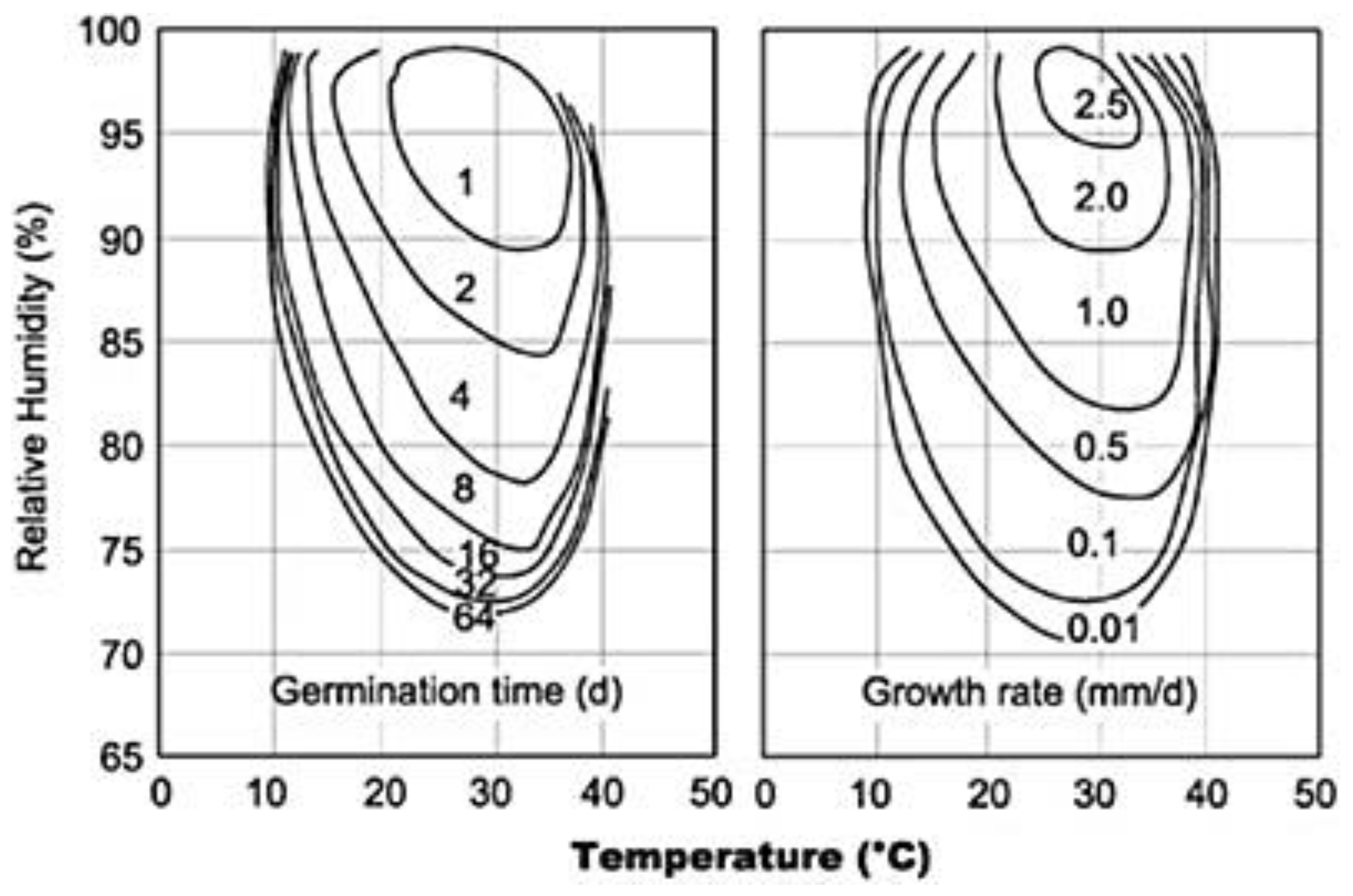
2.2. Literature Synopsis on Contributing Factors
2.2.1. Virus Survival and Transmission
- (i)
- RH may act at the level of the environment. Since a higher humidity implies a slower evaporation from large droplets, the faster evaporation occurring at low RHs would more rapidly change these into droplet nuclei (<5 micron), quickly enough before they fall. Thus, people inhale fewer droplets at a higher RH.
- (ii)
- RH may act at the level of the host. The activity of nasal mucosa strongly depends on the humidity and temperature of the inhaled air, on the exposure time, and on the health of the individual [38]. Lower or higher RH, compared to medium RH values, will alter the mucous viscosity and mucociliary activity. In general, extremely low humidities are reported as enabling the viruses’ settlement in human hosts. Moreover, the dryness of the respiratory epithelium, which plays an important role via the evaporation of water from its surface (desiccation), may increase bacterial adherence and allows for greater penetration of foreign species, such as particles [39]. The upper airways need to achieve moisture neutrality and maximum mucociliary transport as fast as possible. However, the corresponding saccharin mucociliary clearance time in the upper airways is a function of RH [9]. This leads to a recommendation of RH > 30% to avoid “dry eyes”, and RH > 10% to avoid nasal dryness.
- (iii)
- RH may act at the level of the virus particle, affecting its virulence. Virus stability in air may directly affect virus transmission, because virus particles need to remain viable long enough after being expelled from the host to be taken up by a novel host (indirect transmission) [3].
2.2.2. Indoor Environment Vulnerabilities
2.3. Challenging Trade-Off
2.4. A Parameter for Correlating Literature Data
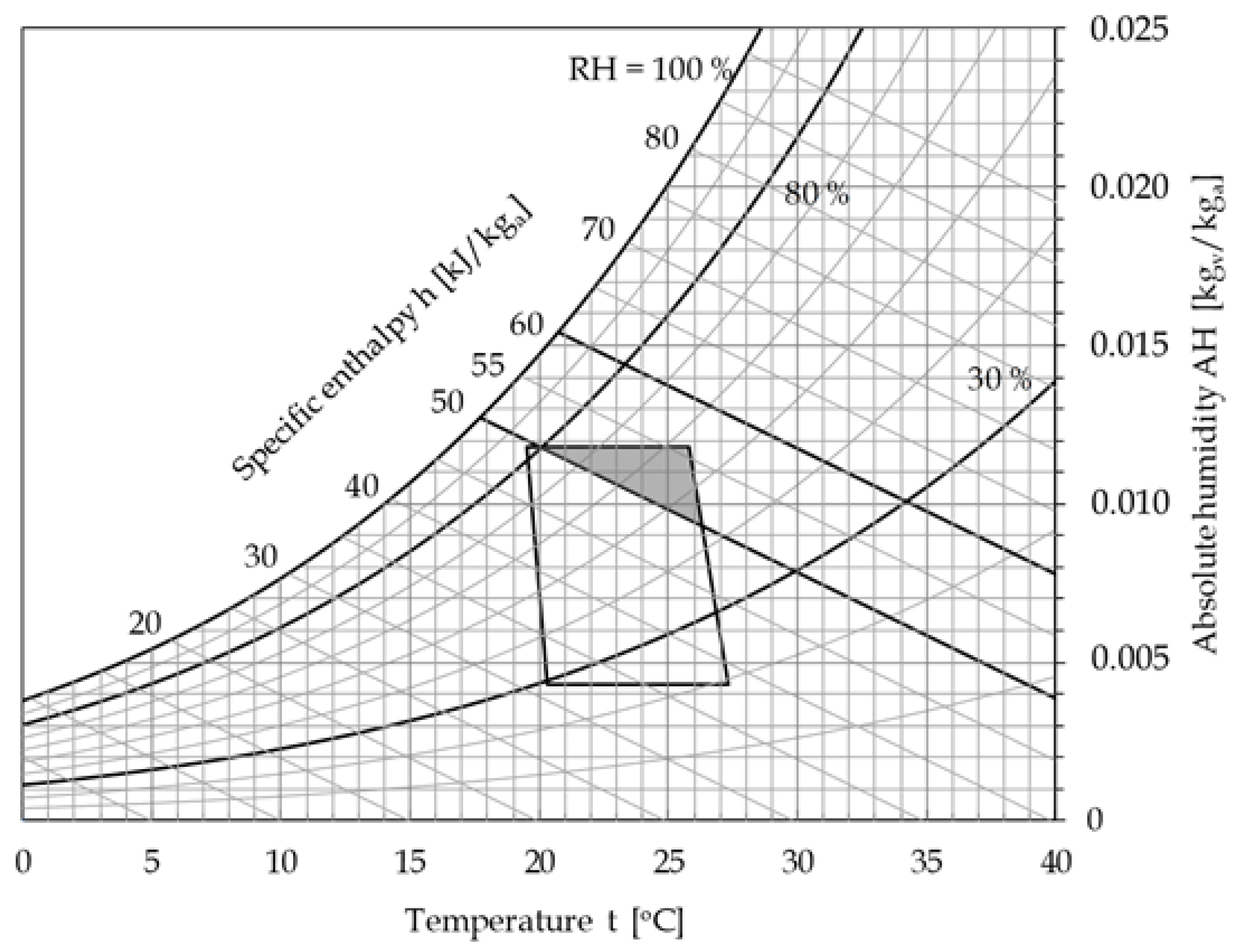
3. Results
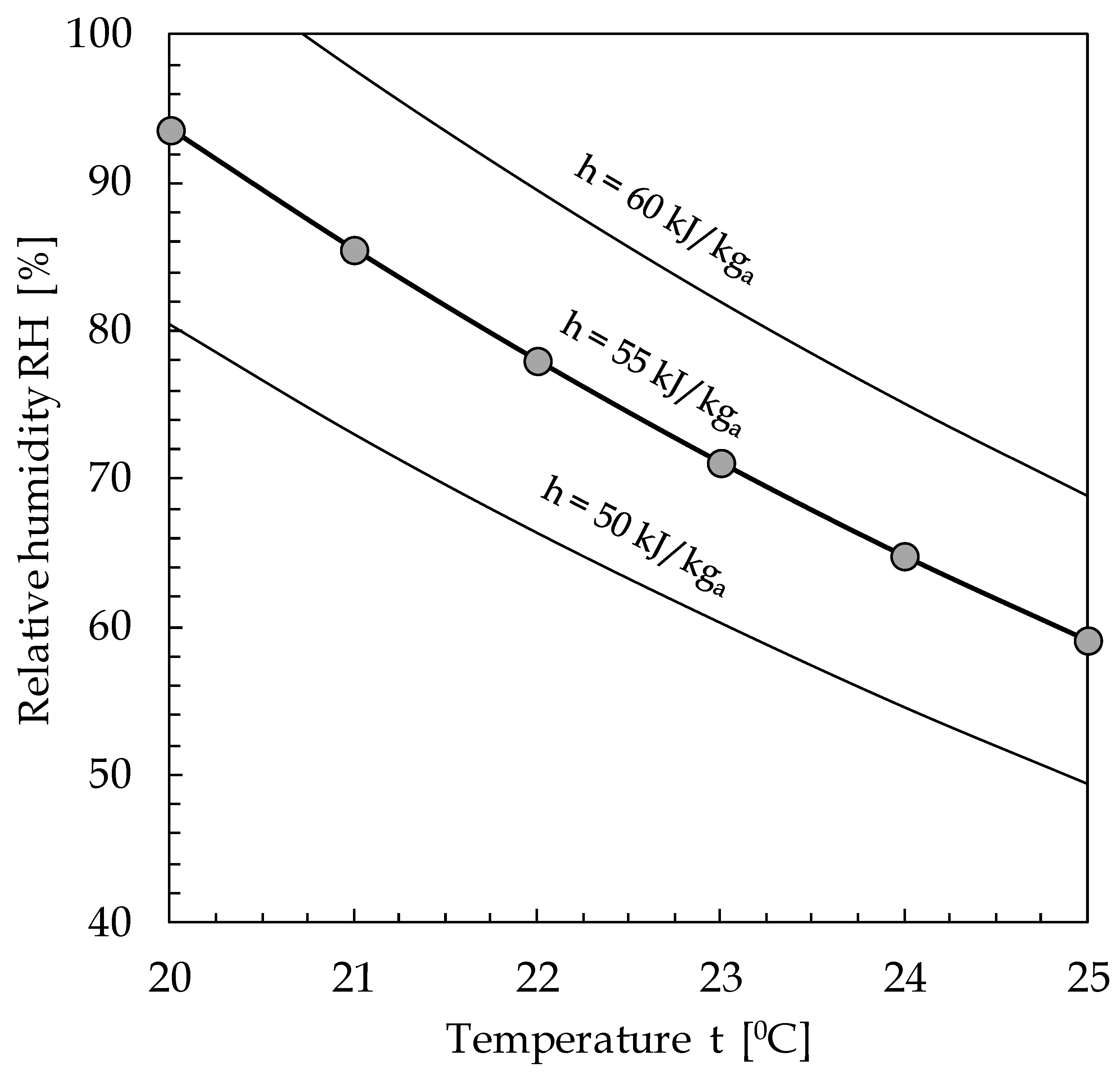
4. Discussion
4.1. Obtained Space of Viable Solutions—Preliminary Recommendations
4.2. HVAC Plants Optimal Setting
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Smieszek, T.; Lazzari, G.; Salathé, M. Assessing the dynamics and control of droplet and aerosol-transmitted influenza using an indoor positioning system. Nat. Sci. Rep. 2019, 9, 2185. [Google Scholar] [CrossRef] [PubMed]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Sun, W.; Huang, J.; Gamber, M.; Wu, J.; He, G. Indirect virus transmission in cluster of Covid-19 cases, Wenzhou, China. Emerg. Infectuos Dis. 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Stadnytskyi, V.; Bax, C.E.; Bax, A.; Anfinrud, P. The Airbourne Lifetime of Small Speech Droplets and Their Potential Importance in SARS-CoV-2 Trasmission. Available online: https://www.pnas.org/cqi/doi/10.1073/pnas.2006874117 (accessed on 25 May 2020).
- Somsen, G.A.; van Rijn, C.; Kooij, S.; Bem, R.A.; Bonn, D. Small droplet aerosols in poorly ventilated spaces and SARS-CoV-2 transmission. Lancet Respir. Med. 2020, in press. [Google Scholar] [CrossRef]
- American Society of Heating Refrigerating Air Conditioning Engineers, ASHRAE Position Document on Airborne Infectious Diseases. Available online: https://www.ashrae.org/file%20library/about/position%20documents/airborne-infectious-diseases.pdf (accessed on 5 April 2020).
- World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019. Available online: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf (accessed on 5 April 2020).
- Weber, T.P.; Stilianakis, N.I. Inactivation of influenza a viruses in the environment and models of transmission. J. Infect. 2008, 57, 361–373. [Google Scholar] [CrossRef]
- Sunwoo, Y.; Chou, C.; Takeshita, J.; Murakami, M. Physiological and subjective responses to low relative humidity. J. Physiol. Anthropol. 2006, 25, 7–14. [Google Scholar] [CrossRef]
- Fang, L.; Wyon, D.P.; Clausen, G.; Fanger, P.O. Impact of indoor air temperature and humidity in an office on perceived air quality, SBS symptoms and performance. Indoor Air 2004, 14, 74–81. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines for Indoor Air Quality—Dampness and Mould. Available online: http://www.euro.who.int/__data/assets/pdf_file/0017/43325/E92645.pdf?ua=1 (accessed on 28 March 2020).
- Kettleson, E.M.; Ramaswami, B.; Hogan, C.J., Jr.; Lee, M.H.; Statyukha, G.A.; Biswas, P.; Angenent, L.T. Airborne virus capture and inactivation by an Electrostatic Particle Collector. Environ. Sci. Technol. 2009, 43, 5940–5946. [Google Scholar] [CrossRef]
- American Society of Heating. Refrigerating and Air-Conditioning Engineers: ANSI/ASHRAE Standard 62.1-2019 - Ventilation for acceptable Indoor Air Quality; ASHRAE: Atlanta, GA, USA, 2019. [Google Scholar]
- Yang, W.; Marr, L. Mechanisms by which ambient humidity may affect viruses in aerosols. Appl. Environ. Microbiol. 2012, 78, 6781–6788. [Google Scholar] [CrossRef]
- Yang, W.; Elankumuran, S.; Marr, L.C. Relationship between humidity and influenza A viability in droplets and implications for influenza’s seasonality. PLoS ONE 2012, 7, e46789. [Google Scholar] [CrossRef]
- Kormuth, K.A.; Lin, K.; Prussin, A.J.; Vejerano, E.P.; Tiwari, A.J.; Cox, S.S.; Myerburg, M.M.; Lakdawala, S.S.; Marr, L.C. Influenza virus infectivity is retained in aerosol and droplets independent on Relative Humidity. J. Infect. Dis. 2018, 218, 739–747. [Google Scholar] [CrossRef] [PubMed]
- Lowen, A.C.; Mubareka, S.; Steel, J.; Palese, P. Influenza virus transmission is dependent on Relative Humidity and temperature. PLoS Pathog. 2007, 3, e151. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.L.; Hu, Y.M.; Qian, F.P. Effects of air temperature and humidity on particle deposition. Chem. Eng. Res. Des. 2011, 89, 2063–2069. [Google Scholar] [CrossRef]
- Chan, K.H.; Peiris, J.S.M.; Lam, S.Y.; Poon, L.L.M.; Yuen, K.Y.; Seto, W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011, 2011, 734690. [Google Scholar] [CrossRef]
- Memarzadeh, F. Literature review of the effect of temperature and humidity on viruses. Ashrae Trans. 2012, 118, 1049–1060. [Google Scholar]
- Schaffer, F.L.; Soergel, M.E.; Straube, D.C. Survival of airborne influenza virus: Effects of propagating host, relative humidity, and composition of spray fluids. Arch. Virol. 1976, 51, 263–273. [Google Scholar] [CrossRef]
- Metz, J.A.; Finn, A. Influenza and humidity—Why a bit more damp may be good for you! J. Infect. 2015, 71, 554–558. [Google Scholar] [CrossRef]
- Yu, I.T.; Li, Y.; Wong, T.W.; Tam, W.; Chan, A.T.; Lee, J.H.; Leung, D.Y.; Ho, T. Evidence of airborne transmission of the SARS. N. Engl. J. Med. 2004, 350, 1731–1739. [Google Scholar] [CrossRef]
- Allen, J.G. Your building can make you sick or keep you well. N. Y. Times 2020, 98, 1095–1096. [Google Scholar]
- Donsgheng, D. From the smallest virus to the biggest gene: Marching towards gene therapy for duchenne muscular dystrophy. Discov. Med. 2006, 33, 103–108. [Google Scholar]
- International Committee on Taxonomy of Viruses, ICTV 9th Report 2011. Available online: https://talk.ictvonline.org/ictv-reports/ictv_9th_report/positive-sense-rna-viruses-2011/w/posrna_viruses/223/coronaviridae-figures (accessed on 28 March 2020).
- Cox, C.S. Airborne bacteria and viruses. Sci. Prog. 1989, 73, 469–499. [Google Scholar] [PubMed]
- Yin, Y.; Wunderink, R.G. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology 2018, 23, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Wuhan City Health Committee, Wuhan Municipal Health Committee’s Report on Unexplained Viral Pneumonia 2020. Available online: http://wjw.wuhan.gov.cn/front/web/showDetail/2020010509020 (accessed on 15 March 2020).
- World Health Organization. WHO Statement Regarding Cluster of Pneumonia Cases in Wuhan, China. Available online: https://www.who.int/china/news/detail/09-01-2020-who-statement-regarding-cluster-of-pneumonia-cases-in-wuhan-china (accessed on 4 April 2020).
- Liu, Y.; Ning, Z.; Chen, Y.; Guo, M.; Liu, Y.; Gali, N.K.; Sun, L.; Duan, Y.; Cai, J.; Westerdahl, D.; et al. Aerodynamic characteristics and RNA Concentration of SARS-CoV-2 aerosol in Wuhan hospitals during CoViD-19 outbreak. Biorxiv Prepr. 2020. [Google Scholar] [CrossRef]
- World Health Organization. Novel Coronavirus—China. Geneva 2020. Available online: https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/ (accessed on 4 April 2020).
- Setti, L.; Passarini, F.; Gennaro, G.A.; Palmisani, J.; Buono, P. Relazione circa l’effetto dell’inquinamento da particolato atmosferico e la diffusione di virus nella popolazione. Position Pap. 2020. SIMA, Università degli Studi di Bari. Available online: https://www.simaonlus.it/wpsima/wp-content/uploads/2020/03/COVID19_Position-Paper_Relazione-circa-l%E2%80%99effetto-dell%E2%80%99inquinamento-da-particolato-atmosferico-e-la-diffusione-di-virus-nella-popolazione.pdf (accessed on 5 May 2020).
- Khare, P.; Marr, L.C. Simulation of vertical concentration gradient of influenza viruses in dust resuspended by walking. Indoor Air 2015, 25, 428–440. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; Ferro, A.R. Resuspension of dust particles in a chamber and associated environmental factors. Aerosol Sci. Technol. 2008, 42, 566–578. [Google Scholar] [CrossRef]
- Qian, J.; Peccia, J.; Ferro, A.R. Walking-induced particle resuspension in indoor environments. Atmos. Environ. 2014, 89, 464–481. [Google Scholar] [CrossRef]
- Hanley, B.P.; Borup, B. Aerosol influenza transmission risk contours: A study of humid tropics versus winter temperate zone. Virol. J. 2010, 7, 98. [Google Scholar] [CrossRef]
- Cruz, A.A.; Togias, A. Upper airway reactions to cold air. Curr. Allergy Asthma Rep. 2008, 8, 111–117. [Google Scholar] [CrossRef]
- Naclerio, R.M.; Pinto, J.; Assanasen, P.; Baroody, F.M. Observations on the ability of the nose to warm and humidify inspired air. Rhinology 2007, 45, 102–111. [Google Scholar]
- Shaman, J.; Kohn, M. Absolute humidity modulates influenza survival, transmission, and seasonality. Proc. Natl. Acad. Sci. USA 2009, 106, 3243–3248. [Google Scholar] [CrossRef] [PubMed]
- Shaman, J.; Pitzer, V.E.; Viboud, C.; Grenfell, B.T.; Lipsitch, M. Absolute humidity and the seasonal onset of influenza in the continental United States. PLoS Biol. 2010, 8, e1000316. [Google Scholar] [CrossRef]
- Jaakkola, K.; Saukkoriipi, A.; Jokelainen, J.; Juvonen, R.; Kauppila, J.; Vainio, O.; Ziegler, T.; Rönkkö, E.; Jaakkola, J.J.K.; Ikäheimo, T.M. Decline in temperature and humidity increases the occurrence of influenza in cold climate. Environ. Health 2014, 13, 22. [Google Scholar] [CrossRef] [PubMed]
- Lipsitch, M.; Viboud, C. Influenza seasonality: Lifting the fog. Proc. Natl. Acad. Sci. USA 2009, 106, 3645–3646. [Google Scholar] [CrossRef]
- Koep, T.H.; Enders, F.T.; Pierret, C.; Ekker, S.C.; Krageschmidt, D.; Neff, K.L.; Lipsitch, M.; Shaman, J.; Huskins, W.C. Predictors of indoor absolute humidity and estimated effects on influenza virus survival in grade schools. BMC Infect. Dis. 2013, 13, 71. [Google Scholar] [CrossRef]
- UUd-Dean, S.M.M. Structural explanation for the effect of humidity on persistence of airborne virus: Seasonality of influenza. J. Theoret. Biol. 2010, 264, 822–829. [Google Scholar] [CrossRef]
- Akers, T.G. Some aspects of the airborne inactivation of viruses. In Airborne Transmission and Airborne Infection; Hers, J.F.P., Winkler, K.C., Eds.; John Wiley & Sons: New York, NY, USA, 1973. [Google Scholar]
- DeJong, J.C. Decay Mechanism of Polio and EMC Viruses in Aerosols. In Proceedings of the Third International Symposium on Aerobiology; Silver, I.H., Ed.; Academic Press: New York, NY, USA, 1970. [Google Scholar]
- Morawska, L. Droplet fate in indoor environments, or can we prevent the spread of infection? Indoor Air 2006, 16, 335–347. [Google Scholar] [CrossRef]
- Ijaz, M.K.; Brunner, A.H.; Sattar, S.A.; Nair, R.C.; Johnson-Lussenburg, C.M. Survival characteristics of airborne human Coronavirus 229E. J. Gen. Virol. 1985, 66, 2743–2748. [Google Scholar] [CrossRef]
- Ikäheimo, T.M.; Jaakkola, K.; Jokelainen, J.; Saukkoriipi, A.; Roivainen, M.; Juvonen, R.; Vainio, O.; Jaakkola, J.J. A decrease in temperature and humidity precedes human rhinovirus infections in a cold climate. Viruses 2016, 8, E244. [Google Scholar] [CrossRef]
- Davis, R.E.; Dougherty, E.; McArthur, C. Cold, dry air is associated with influenza and pneumonia mortality in Auckland, New Zealand. Influenza Other Respir. Viruses 2016, 10, 310–313. [Google Scholar] [CrossRef]
- Fang, L.; Clausen, G.; Fanger, P.O. Impact of temperature and humidity on the perception of indoor air quality. Indoor Air 1998, 8, 80–90. [Google Scholar] [CrossRef]
- Fang, L.; Clausen, G.; Fanger, P.O. Impact of temperature and humidity on chemical and sensory emissions from building materials. Indoor Air 1999, 9, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Fechter, J.O.; Englund, F.; Lundin, A. Association between temperature, relative humidity and concentration of volatile organic compounds from wooden furniture in a model room. Wood Mater. Sci. Eng. 2006, 1, 69–75. [Google Scholar] [CrossRef]
- Dampness and Mold. Indoor Air Quality Scientific Findings Resource Bank. Available online: https://iaqscience.lbl.gov/dampness-summary (accessed on 5 May 2020).
- Morse, R. Indoor Air Quality and Mold Prevention of the Building Envelope, WBDG. 2017. Available online: https://www.wbdg.org/resources/indoor-air-quality-and-mold-prevention-building-envelope (accessed on 5 May 2020).
- European Centre for Disease Prevention and Control. 2020. Factsheet for Health Professionals on Coronaviruses. Available online: https://www.ecdc.europa.eu/en/facts (accessed on 5 May 2020).
- Noti, J.D.; Blachere, F.M.; McMillen, C.M.; Lindsley, W.G.; Kashon, M.L.; Slaughter, D.R.; Beezhold, D.H. High humidity leads to loss of infectious influenza virus from simulated coughs. PLoS ONE 2013, 8, e57485. [Google Scholar] [CrossRef]
- Blachere, F.M.; Lindsley, W.G.; Pearce, T.A.; Anderson, S.E.; Fisher, M.; Khakoo, R.; Meade, B.J.; Lander, O.; Davis, S.; Thewlis, R.E.; et al. Measurement of airborne influenza in a hospital emergency department. Clin. Infect. Dis. 2009, 48, 438–440. [Google Scholar] [CrossRef]
- Spena, A. Air Change Ratio Indoor & CoViD-19—Cambiate L’aria. 18 March 2020. Available online: http://astrolabio.amicidellaterra.it/node/2064 (accessed on 5 May 2020).
- Spena, A. Efficienza Energetica. Governare la Complessità Delle Opzioni più Avanzate; La Termotecnica: Milan, Italy, 2017; pp. 7–8. [Google Scholar]
- Spena, A. Efficienza energetica e igiene degli ambienti chiusi: What is past, is prologue. Nuova Energ. 2020, 2, 49–53. [Google Scholar]
- Janssen, J.E. Ventilation for acceptable indoor air quality. ASHRAE J. 1989, 31, 40–48. [Google Scholar]
- Seppänen, O.; Fisk, W.J.; Lei, Q.H. Ventilation and performance in office work. Indoor Air 2006, 16, 28–36. [Google Scholar] [CrossRef]
- Mazzenga, C.; Iaria, V.; Spena, V.A. On the misleading perception by the occupants of the indoor air renewals. First experimental evidences in densely occupied lecture halls. In Proceedings of The 51st AICARR International Conference on The Human Dimension of Building Energy Performance, Venice, Italy, 20–22 February 2019. [Google Scholar]
- Wolkoff, P. Indoor Air Humidity, Air Quality, and Health. Int. J. Hyg. Environ. Health 2018, 221, 376–390. [Google Scholar] [CrossRef]
- Tang, J.W. The effect of environmental parameters on the survival of airborne infectious agents. J. R. Soc. Interface 2009, 6, 737–746. [Google Scholar] [CrossRef]
- Teller, R. Aerosol transmission of influenza a virus: A review of new studies. J. R. Soc. Med. 2009, 6, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Wolkoff, P. External eye symptoms in indoor environments. Indoor Air 2017, 27, 246–260. [Google Scholar] [CrossRef] [PubMed]
- Handbook-Fundamentals AS. American Society of Heating Refrigerating Air Conditioning Engineers; ANSI/ASHRAE Standard 55-2013; Thermal Environmental Conditions for Human Occupancy, ASHRAE: Atlanta, GA, USA, 2013. [Google Scholar]
- Wulff, N.H.; Tzatzaris, M.; Young, P.J. Monte Carlo simulation of the Spearman-Kaerber TCID50. J. Clin. Bioinform. 2012, 2, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Prussin, A.J.; Schwake, D.O.; Lin, K.; Gallagher, D.L.; Buttling, L.; Marr, L.C. Survival of the enveloped virus Phi6 in droplets as a function of relative humidity, absolute humidity, and temperature. Appl. Environ. Microbiol. 2018, 84. [Google Scholar] [CrossRef]
- Adcock, N.J.; Rice, E.W.; Sivaganesan, M.; Brown, J.D.; Stallknecht, D.E.; Swayne, D.E. The use of bacteriophages of the family Cystoviridae as surrogates for H5N1 highly pathogenic avian influenza viruses in persistence and inactivation studies. J. Environ. Sci. Health 2009, 44, 1362–1366. [Google Scholar] [CrossRef]
- Turgeon, N.; Toulouse, M.J.; Martel, B.; Moineau, S.; Duchaine, C. Comparison of five bacteriophages as models for viral aerosol studies. Appl. Environ. Microbiol. 2014, 80, 4242–4250. [Google Scholar] [CrossRef]
- Casanova, L.M.; Jeon, S.; Rutala, W.A.; Weber, D.J.; Sobsey, M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010, 76, 2712–2717. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Munster, V.J. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Eurosurveillance 2013, 18, 20590. [Google Scholar] [CrossRef]
- Pyankov, O.V.; Bodnev, A.S.; Pyankova, O.G.; Agranovski, I.E. Survival of aerosolized coronavirus in the ambient air. J. Aerosol Sci. 2018, 115, 158–163. [Google Scholar] [CrossRef]
- ASHRAE Handbook of Fundamentals. In Ch. 6—Psychrometrics; American Society of Heating, Refrigeration and Air-Conditioning Engineers: Atlanta, GA, USA, 2005.
- Hyland, R.W.; Wexler, A. Formulations for the Thermodynamic Properties of the Saturated Phases of H2O from 173.15 K to 473.15 K; ASHRAE Transactions: San Diego, CA, USA, 1983; Volume 89, pp. 500–519. [Google Scholar]
- Sajadi, M.M.; Habibzadeh, P.; Vintzileos, A.; Shokouhi, S.; Miralles-Wilhelm, F.; Amoroso, A. Temperature, humidity, and latitude analysis to predict potential spread and seasonality for COVID-19. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
| Temperature [°C] | RH (%) | VLS1h | Virus Type | AH [kgvap/kgdry-air] | H [kJ/kgdry-air] | |
|---|---|---|---|---|---|---|
| Pyankov et al. [77]-2018 | 25 | 79 | 0.634 | HCoV-EMC | 0.0158 | 65.32 |
| Pyankov et al. [77]-2018 | 38 | 24 | 0.046 | HCoV-EMC | 0.0099 | 63.77 |
| Van Doremalen et al. [2]-2020 | 22 | 65 | 0.300 | SARS-CoV-2 | 0.0107 | 49.44 |
| Van Doremalen et al. [2]-2020 | 22 | 65 | 0.293 | SARS-CoV-1 | 0.0107 | 49.44 |
| Van Doremalen et al. [76]-2013 | 20 | 40 | 0.930 | HCoV-EMC | 0.0058 | 34.84 |
| Van Doremalen et al. [76]-2013 | 20 | 70 | 0.110 | HCoV-EMC | 0.0102 | 46.06 |
| Prussin et al. [72]-2018 | 22 | 33 | 0.970 | Phi6 | 0.0054 | 35.88 |
| Prussin et al. [72]-2018 | 22 | 43 | 0.820 | Phi6 | 0.0071 | 40.09 |
| Prussin et al. [72]-2018 | 22 | 55 | 0.360 | Phi6 | 0.0091 | 45.18 |
| Prussin et al. [72]-2018 | 22 | 75 | 0.010 | Phi6 | 0.0124 | 53.72 |
| Prussin et al. [72]-2018 | 22 | 85 | 0.050 | Phi6 | 0.0141 | 58.03 |
| Prussin et al. [72]-2018 | 22 | 98 | 0.640 | Phi6 | 0.0163 | 63.66 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spena, A.; Palombi, L.; Corcione, M.; Carestia, M.; Spena, V.A. On the Optimal Indoor Air Conditions for SARS-CoV-2 Inactivation. An Enthalpy-Based Approach. Int. J. Environ. Res. Public Health 2020, 17, 6083. https://doi.org/10.3390/ijerph17176083
Spena A, Palombi L, Corcione M, Carestia M, Spena VA. On the Optimal Indoor Air Conditions for SARS-CoV-2 Inactivation. An Enthalpy-Based Approach. International Journal of Environmental Research and Public Health. 2020; 17(17):6083. https://doi.org/10.3390/ijerph17176083
Chicago/Turabian StyleSpena, Angelo, Leonardo Palombi, Massimo Corcione, Mariachiara Carestia, and Vincenzo Andrea Spena. 2020. "On the Optimal Indoor Air Conditions for SARS-CoV-2 Inactivation. An Enthalpy-Based Approach" International Journal of Environmental Research and Public Health 17, no. 17: 6083. https://doi.org/10.3390/ijerph17176083
APA StyleSpena, A., Palombi, L., Corcione, M., Carestia, M., & Spena, V. A. (2020). On the Optimal Indoor Air Conditions for SARS-CoV-2 Inactivation. An Enthalpy-Based Approach. International Journal of Environmental Research and Public Health, 17(17), 6083. https://doi.org/10.3390/ijerph17176083








