Validation of Obesity Status Based on Self-Reported Data among Filipina and Indonesian Female Migrant Domestic Workers in Macao (SAR), China
Abstract
1. Introduction
- To evaluate the accuracy of BMI and BMI categories based on self-reported height and weight in these two migrant populations.
- To investigate whether ethnic differences exist between these two populations concerning the discrepancy between self-reported and objective measures.
- Identify improved overweight and obesity cut-off points for BMI derived from self-reported measures for these two populations.
2. Materials and Methods
2.1. Participants and Study Design
2.2. Measures
2.2.1. Self-Reported Height and Weight
2.2.2. Objectively Measured Height and Weight
2.2.3. Body Mass Index (BMI)
2.3. Analyses Plan
3. Results
3.1. Participant Characteristics
3.2. Difference between Self-Reported and Measured Height and Weight
3.3. Difference between Self-Reported and Measured BMI
3.4. BMI Categories
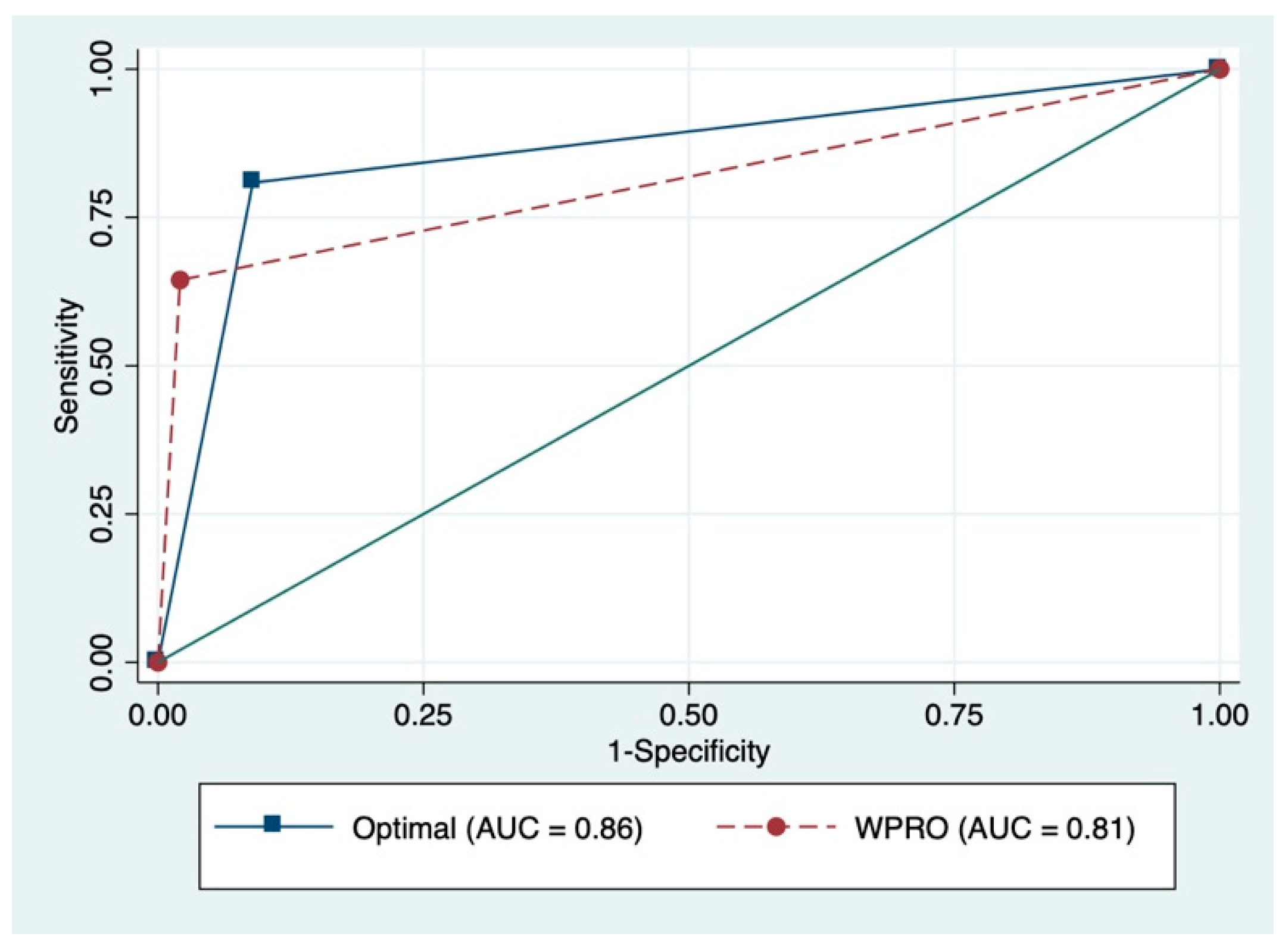
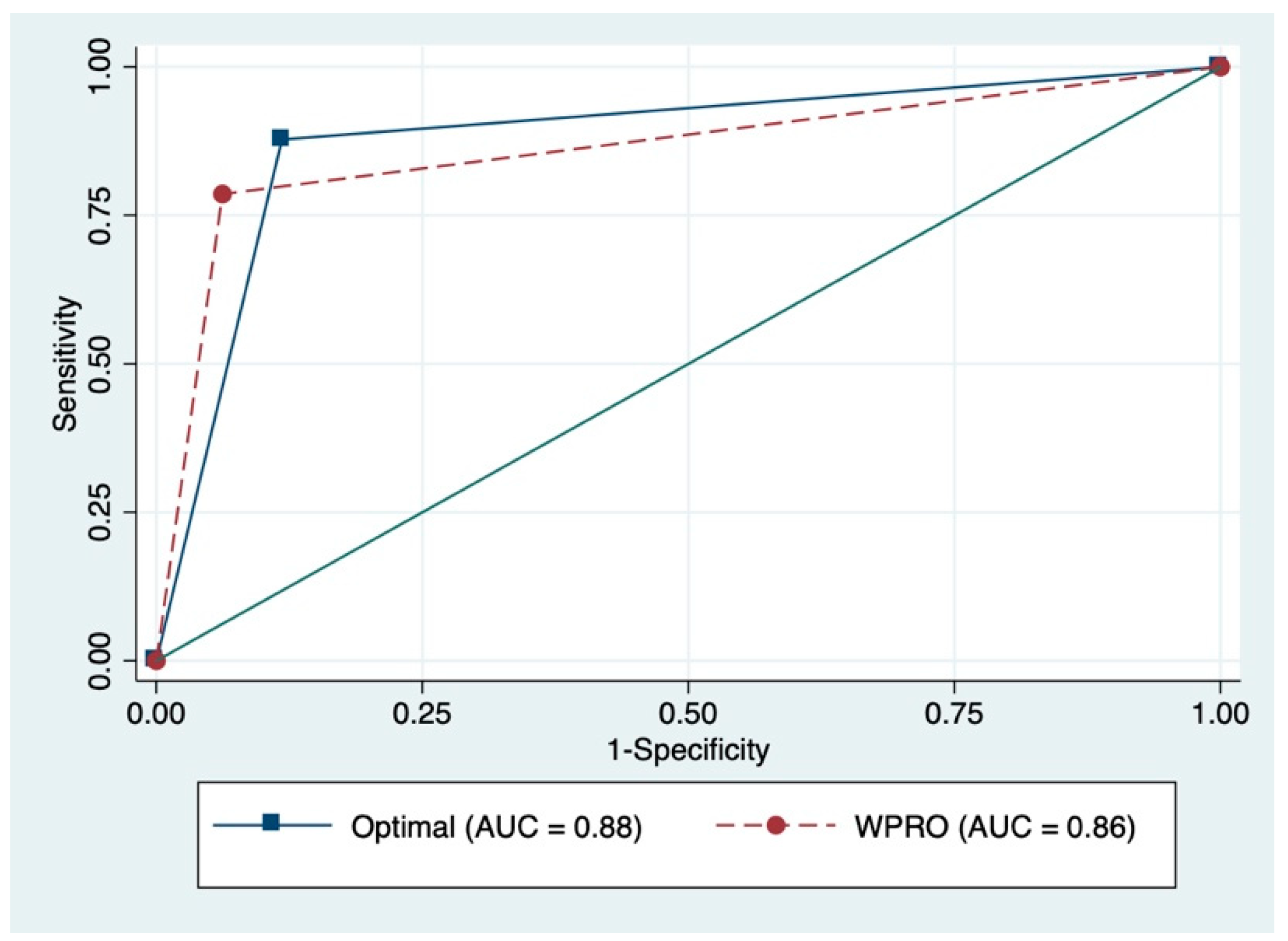
3.5. ROC Curve and Sensitivity and Specificity Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Roth, J.; Qiang, X.; Marbán, S.L.; Redelt, H.; Lowell, B.C. The Obesity Pandemic: Where Have We Been and Where Are We Going? Obes. Res. 2004, 12, 88S–101S. [Google Scholar] [CrossRef] [PubMed]
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.L.; Gortmaker, S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- World Health Organization. Obesity and Overweight Fact Sheet. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 13 July 2020).
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef]
- Pi-Sunyer, X. The medical risks of obesity. Postgrad. Med. 2009, 121, 21–33. [Google Scholar] [CrossRef]
- Lavie, C.J.; Milani, R.V.; Ventura, H.O. Obesity and Cardiovascular Disease. J. Am. Coll. Cardiol. 2009, 53, 1925–1932. [Google Scholar] [CrossRef]
- Dixon, J. The effect of obesity on health outcomes. Mol. Cell. Endocrinol. 2010, 316, 104–108. [Google Scholar] [CrossRef]
- The GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef]
- Fernandez, R.S.; Miranda, C.; Everett, B. Prevalence of obesity among migrant Asian Indians: A systematic review and meta-analysis. Int. J. Evid. Based Healthc. 2011, 9, 420–428. [Google Scholar] [CrossRef]
- Delavari, M.; Sønderlund, A.L.; Swinburn, B.; Mellor, D.; Renzaho, A. Acculturation and obesity among migrant populations in high income countries—A systematic review. BMC Public Health 2013, 13, 458. [Google Scholar] [CrossRef]
- Murphy, M.; Robertson, W.; Oyebode, O. Obesity in International Migrant Populations. Curr. Obes. Rep. 2017, 6, 314–323. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.R.; Ghimire, S.; Joshi, C.; Gyawali, B.; Shrestha, A.; Neupane, D.; Sharma, S.R.; Pokharel, Y.; Virani, S.S. Cardio-metabolic disease risk factors among South Asian labour migrants to the Middle East: A scoping review and policy analysis. Glob. Health 2019, 15, 33. [Google Scholar] [CrossRef]
- Patel, J.; Vyas, A.; Cruickshank, J.; Prabhakaran, D.; Hughes, E.; Reddy, K.S.; Mackness, M.; Bhatnagar, D.; Durrington, P. Impact of migration on coronary heart disease risk factors: Comparison of Gujaratis in Britain and their contemporaries in villages of origin in India. Atherosclerosis 2006, 185, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Fernando, E.; Razak, F.; Lear, S.A.; Anand, S.S. Cardiovascular Disease in South Asian Migrants. Can. J. Cardiol. 2015, 31, 1139–1150. [Google Scholar] [CrossRef] [PubMed]
- Martin, P.; Abella, M.; Kuptsch, C. Managing Labor Migration in the Twenty-First Century; Yale University Press: New Haven, CT, USA, 2006. [Google Scholar]
- International Labour Organization (ILO). International Migration in ASEAN at a Glance. Available online: https://www.ilo.org/asia/publications/WCMS_412975/lang--en/index.htm (accessed on 13 July 2020).
- Rogers, N.T.; Power, C.; Pinto Pereira, S.M. Birthweight, lifetime obesity and physical functioning in mid-adulthood: A nationwide birth cohort study. Int. J. Epidemiol. 2019, 73. [Google Scholar] [CrossRef]
- Dhingra, R.; Vasan, R.S. Age As a Risk Factor. Med. Clin. N. Am. 2012, 96, 87–91. [Google Scholar] [CrossRef]
- Preibisch, K.; Hennebry, J. Temporary migration, chronic effects: The health of international migrant workers in Canada. Can. Med Assoc. J. 2011, 183, 1033–1038. [Google Scholar] [CrossRef]
- Lecerof, S.S.; Westerling, R.; Moghaddassi, M.; Östergren, P.-O. Health information for migrants: The role of educational level in prevention of overweight. Scand. J. Public Health 2011, 39, 172–178. [Google Scholar] [CrossRef]
- Dijkshoorn, H.; Nierkens, V.; Nicolaou, M. Risk groups for overweight and obesity among Turkish and Moroccan migrants in The Netherlands. Public Health 2008, 122, 625–630. [Google Scholar] [CrossRef]
- WHO Consultation on Obesity. Obesity: Preventing and Managing the Global Epidemic; Report of a WHO Consultation on Obesity, Geneva, 3–5 June 1997; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Wang, J.; Thornton, J.C.; Russell, M.; Burastero, S.; Heymsfield, S.; Pierson, R.N. Asians have lower body mass index (BMI) but higher percent body fat than do whites: Comparisons of anthropometric measurements. Am. J. Clin. Nutr. 1994, 60, 23–28. [Google Scholar] [CrossRef]
- World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; Health Communications Australia: Sydney, Australia, 2000. [Google Scholar]
- Wen, C.P.; Cheng, T.Y.D.; Tsai, S.P.; Chan, H.T.; Hsu, H.L.; Hsu, C.C.; Eriksen, M.P. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. 2008, 12, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Van den Brandt, P.A.; Dirx, M.J.; Ronckers, C.M.; Hoogen, P.V.D.; Goldbohm, R.A. Height, weight, weight change, and postmenopausal breast cancer risk: The Netherlands Cohort Study. Cancer Causes Control 1997, 8, 39–47. [Google Scholar] [CrossRef]
- Sleigh, A.; Seubsman, S.-A.; Bain, C. Cohort Profile: The Thai Cohort of 87 134 Open University students. Int. J. Epidemiol. 2007, 37, 266–272. [Google Scholar] [CrossRef]
- Sandler, D.P.; Hodgson, M.E.; Deming-Halverson, S.L.; Juras, P.S.; D’Aloisio, A.A.; Suarez, L.M.; Kleeberger, C.A.; Shore, D.L.; DeRoo, L.A.; Taylor, J.A.; et al. The Sister Study Cohort: Baseline Methods and Participant Characteristics. Environ. Health Perspect. 2017, 125, 127003. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Larco, R.M.; Ruiz-Alejos, A.; Bernabe-Ortiz, A.; Gilman, R.H.; Smeeth, L.; Miranda, J.J. Cohort Profile: The PERU MIGRANT Study-A prospective cohort study of rural dwellers, urban dwellers and rural-to-urban migrants in Peru. Int. J. Epidemiol. 2017, 46, 1752. [Google Scholar] [CrossRef] [PubMed]
- Gorber, S.C.; Tremblay, M.; Moher, D.; Gorber, S.C. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: A systematic review. Obes. Rev. 2007, 8, 307–326. [Google Scholar] [CrossRef]
- Stommel, M.; Schoenborn, C.A. Accuracy and usefulness of BMI measures based on self-reported weight and height: Findings from the NHANES & NHIS 2001–2006. BMC Public Health 2009, 9, 421. [Google Scholar] [CrossRef]
- Chiolero, A.; Peytremann-Bridevaux, I.; Paccaud, F. Associations between obesity and health conditions may be overestimated if self-reported body mass index is used. Obes. Rev. 2007, 8, 373–374. [Google Scholar] [CrossRef]
- Keith, S.W.; Fontaine, K.R.; Pajewski, N.M.; Mehta, T.; Allison, D.B. Use of self-reported height and weight biases the body mass index–mortality association. Int. J. Obes. 2010, 35, 401–408. [Google Scholar] [CrossRef]
- Larson, M.R. Social desirability and self-reported weight and height. Int. J. Obes. 2000, 24, 663–665. [Google Scholar] [CrossRef]
- Gattario, K.H.; Frisén, A. Body dissatisfaction across cultures: Findings and research problems. Eur. Eat. Disord. Rev. 2010, 18, 133–146. [Google Scholar] [CrossRef]
- Swami, V.; Frederick, D.A.; Aavik, T.; Alcalay, L.; Allik, J.; Anderson, D.; Andrianto, S.; Arora, A.; Brännström, Å.; Cunningham, J.; et al. The Attractive Female Body Weight and Female Body Dissatisfaction in 26 Countries Across 10 World Regions: Results of the International Body Project I. Pers. Soc. Psychol. Bull. 2010, 36, 309–325. [Google Scholar] [CrossRef]
- Duncan, D.T.; Wolin, K.; Scharoun-Lee, M.; Ding, E.L.; Warner, E.T.; Bennett, G.G. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 20. [Google Scholar] [CrossRef]
- Bhanji, S.; Khuwaja, A.K.; Siddiqui, F.; Azam, S.I.; Kazmi, K.A. Underestimation of weight and its associated factors among overweight and obese adults in Pakistan: A cross sectional study. BMC Public Health 2011, 11, 363. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.-I.; Lee, S.-Y.D. Health literacy as the missing link in the provision of immigrant health care: A qualitative study of Southeast Asian immigrant women in Taiwan. Int. J. Nurs. Stud. 2016, 54, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Chang, W.; Zhou, H.; Hu, H.; Liang, W. Factors associated with health-seeking behavior among migrant workers in Beijing, China. BMC Health Serv. Res. 2010, 10, 69. [Google Scholar] [CrossRef]
- De Mola, C.L.; Pillay, T.D.; Diez-Canseco, F.; Gilman, R.H.; Smeeth, L.; Miranda, J.J. Body Mass Index and Self-Perception of Overweight and Obesity in Rural, Urban and Rural-to-Urban Migrants: PERU MIGRANT Study. PLoS ONE 2012, 7, e50252. [Google Scholar] [CrossRef]
- Hall, B.J.; Garabiles, M.R.; Latkin, C.A. Work life, relationship, and policy determinants of health and well-being among Filipino domestic Workers in China: A qualitative study. BMC Public Health 2019, 19, 229. [Google Scholar] [CrossRef] [PubMed]
- DSAL. Number of Non-Resident Workers by Industry and Country/Region of Issuance of Identification Document; Labour Affairs Bureau, Goverment of the Macao Special Administrative Region: Macao, China, 2018.
- Wells, J.K.; Marphatia, A.A.; Cole, T.J.; McCoy, D. Associations of economic and gender inequality with global obesity prevalence: Understanding the female excess. Soc. Sci. Med. 2012, 75, 482–490. [Google Scholar] [CrossRef]
- World Health Organization. Diabetes Country Profiles, 2016. Available online: https://www.who.int/diabetes/country-profiles/en/ (accessed on 13 July 2020).
- Heckathorn, D.D. Respondent-Driven Sampling: A New Approach to the Study of Hidden Populations. Soc. Probl. 1997, 44, 174–199. [Google Scholar] [CrossRef]
- Heckathorn, U.D.; Semaan, S.; Broadhead, R.S.; Hughes, J.J. Extensions of Respondent-Driven Sampling: A New Approach to the Study of Injection Drug Users Aged 18–25. AIDS Behav. 2002, 6, 55–67. [Google Scholar] [CrossRef]
- Cogill, B. Anthropometric Indicators Measurement Guide. Available online: http://www.ergo-eg.com/uploads/books/anthro_1.pdf (accessed on 13 July 2020).
- Mony, P.K.; Swaminathan, S.; Gajendran, J.K.; Vaz, M. Quality assurance for accuracy of anthropometric measurements in clinical and epidemiological studies [Errare humanum est = to err is human]. Indian J. Community Med. 2016, 41, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Wada, K.; Tamakoshi, K.; Tsunekawa, T.; Otsuka, R.; Zhang, H.; Murata, C.; Nagasawa, N.; Matsushita, K.; Sugiura, K.; Yatsuya, H.; et al. Validity of self-reported height and weight in a Japanese workplace population. Int. J. Obes. 2005, 29, 1093–1099. [Google Scholar] [CrossRef] [PubMed]
- Wen, M.; Kowaleski-Jones, L. Sex and ethnic differences in validity of self-reported adult height, weight and body mass index. Ethn. Dis. 2012, 22, 72–78. [Google Scholar] [PubMed]
- Nakamura, K.; Hoshino, Y.; Kodama, K.; Yamamoto, M. Reliability of self-reported body height and weight of adult japanese women. J. Biosoc. Sci. 1999, 31, 555–558. [Google Scholar] [CrossRef]
- Lim, L.L.; Seubsman, S.-A.; Sleigh, A.C. Validity of self-reported weight, height, and body mass index among university students in Thailand: Implications for population studies of obesity in developing countries. Popul. Health Metr. 2009, 7, 15. [Google Scholar] [CrossRef]
- Bolton-Smith, C.; Woodward, M.; Tunstall-Pedoe, H.; Morrison, C. Accuracy of the estimated prevalence of obesity from self reported height and weight in an adult Scottish population. J. Epidemiol. Community Health 2000, 54, 143–148. [Google Scholar] [CrossRef]
- Krul, A.J.; Daanen, H.A.M.; Choi, H. Self-reported and measured weight, height and body mass index (BMI) in Italy, the Netherlands and North America. Eur. J. Public Health 2010, 21, 414–419. [Google Scholar] [CrossRef]
- Nawaz, H.; Chan, W.; Abdulrahman, M.; Larson, D.; Katz, D.L. Self-reported weight and height: Implications for obesity research. Am. J. Prev. Med. 2001, 20, 294–298. [Google Scholar] [CrossRef]
- Akhtar-Danesh, N.; Dehghan, M.; Merchant, A.T.; Rainey, J.A. Validity of self-reported height and weight for measuring prevalence of obesity. Open Med. 2008, 2, e83–e88. [Google Scholar]
- Hayes, A.J.; Kortt, M.A.; Clarke, P.M.; Brandrup, J.D. Estimating equations to correct self-reported height and weight: Implications for prevalence of overweight and obesity in Australia. Aust. N. Z. J. Public Health 2008, 32, 542–545. [Google Scholar] [CrossRef] [PubMed]
- Nyholm, M.; Gullberg, B.; Merlo, J.; Råstam, L.; Lindblad, U.; Lundqvist-Persson, C. The Validity of Obesity Based on Self-reported Weight and Height: Implications for Population Studies. Obesity 2007, 15, 197. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Filipina (n = 1388) | Indonesian (n = 369) | ||
|---|---|---|---|---|
| N | % | N | % | |
| Age | ||||
| 18–24 | 28 | 2.0 | 8 | 2.2 |
| 25–34 | 298 | 21.5 | 118 | 32.4 |
| 35–44 | 555 | 40.0 | 172 | 47.3 |
| 45–54 | 414 | 29.8 | 61 | 16.8 |
| 55–64 | 90 | 6.5 | 4 | 1.1 |
| 65–74 | 3 | 0.2 | 1 | 0.3 |
| Marital Status | ||||
| Single, never married | 353 | 25.4 | 72 | 19.6 |
| Married | 617 | 44.5 | 140 | 38.0 |
| Partnered, but not married | 99 | 7.1 | 16 | 4.4 |
| Separated | 216 | 15.6 | 27 | 7.3 |
| Legally separated | 9 | 0.7 | 46 | 12.5 |
| Widowed | 94 | 6.8 | 67 | 18.2 |
| BMI categories (self-reported) | ||||
| Underweight | 77 | 5.8 | 25 | 7.0 |
| Normal | 696 | 52.5 | 168 | 47.1 |
| Overweight | 258 | 19.5 | 65 | 18.2 |
| Obese I | 256 | 19.3 | 72 | 20.2 |
| Obese II | 38 | 2.9 | 27 | 7.6 |
| BMI categories (measured) | ||||
| Underweight | 23 | 1.7 | 14 | 3.8 |
| Normal | 468 | 34.3 | 150 | 41.1 |
| Overweight | 341 | 25.0 | 70 | 19.2 |
| Obese I | 455 | 33.4 | 100 | 27.4 |
| Obese II | 76 | 5.6 | 31 | 8.5 |
| Self-Reported BMI (kg/m2) | ||||||
|---|---|---|---|---|---|---|
| Measured BMI (kg/m2) | Underweight | Normal | Overweight | Obese Stage I | Obese Stage II | Kappa |
| Filipina (n = 1388) | ||||||
| Underweight | 18 | 4 | 0 | 0 | 0 | 0.4 p < 0.001 |
| Normal | 49 | 400 | 8 | 2 | 0 | |
| Overweight | 6 | 222 | 94 | 10 | 0 | |
| Obese stage I | 1 | 69 | 149 | 213 | 6 | |
| Obese stage II | 0 | 1 | 7 | 31 | 32 | |
| Indonesian (n = 369) | ||||||
| Underweight | 7 | 6 | 1 | 0 | 0 | 0.5 p < 0.001 |
| Normal | 16 | 122 | 4 | 5 | 0 | |
| Overweight | 2 | 31 | 28 | 7 | 1 | |
| Obese stage I | 0 | 8 | 32 | 53 | 4 | |
| Obese stage II | 0 | 1 | 0 | 7 | 22 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, L.; Chen, W.; Renzaho, A.M.N.; Hall, B.J. Validation of Obesity Status Based on Self-Reported Data among Filipina and Indonesian Female Migrant Domestic Workers in Macao (SAR), China. Int. J. Environ. Res. Public Health 2020, 17, 5927. https://doi.org/10.3390/ijerph17165927
Huang L, Chen W, Renzaho AMN, Hall BJ. Validation of Obesity Status Based on Self-Reported Data among Filipina and Indonesian Female Migrant Domestic Workers in Macao (SAR), China. International Journal of Environmental Research and Public Health. 2020; 17(16):5927. https://doi.org/10.3390/ijerph17165927
Chicago/Turabian StyleHuang, Lei, Wen Chen, Andre M. N. Renzaho, and Brian J. Hall. 2020. "Validation of Obesity Status Based on Self-Reported Data among Filipina and Indonesian Female Migrant Domestic Workers in Macao (SAR), China" International Journal of Environmental Research and Public Health 17, no. 16: 5927. https://doi.org/10.3390/ijerph17165927
APA StyleHuang, L., Chen, W., Renzaho, A. M. N., & Hall, B. J. (2020). Validation of Obesity Status Based on Self-Reported Data among Filipina and Indonesian Female Migrant Domestic Workers in Macao (SAR), China. International Journal of Environmental Research and Public Health, 17(16), 5927. https://doi.org/10.3390/ijerph17165927





