Dietary Practices and Adolescent Obesity in Secondary School Learners at Disadvantaged Schools in South Africa: Urban–Rural and Gender Differences
Abstract
1. Introduction
2. Materials and Methods
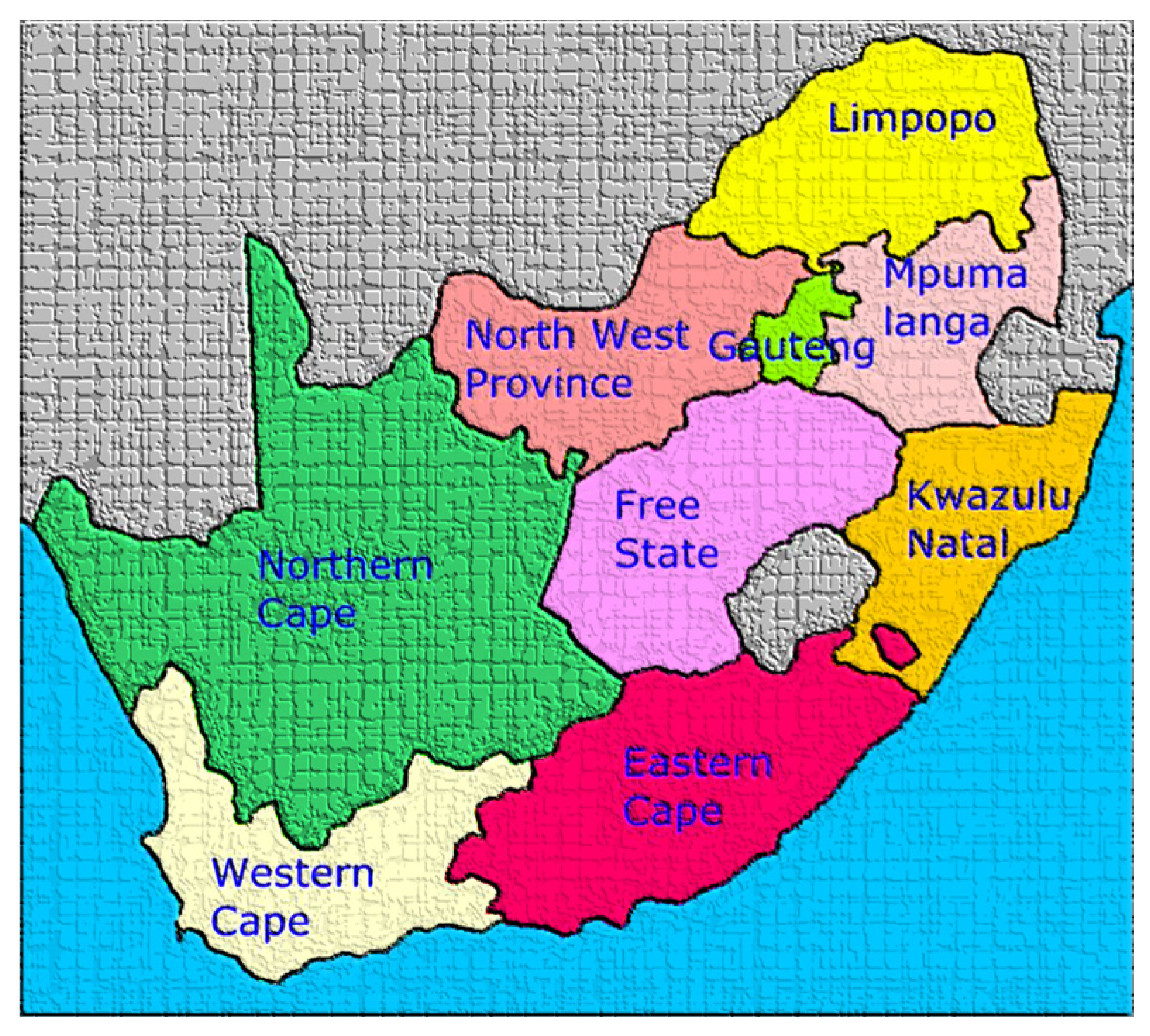
2.1. Setting and Sample
2.2. Selection and Training of Research Assistants
2.3. Measurements
2.3.1. Demographic Data on Learners
2.3.2. Food Frequency Questionnaire
2.3.3. Anthropometry
2.4. Pilot Study
2.5. Data Analyses
2.6. Ethics
3. Results
3.1. Demographic Data
3.2. Anthropometry
3.3. Usual Weekly Eating Pattern Described by the Learners
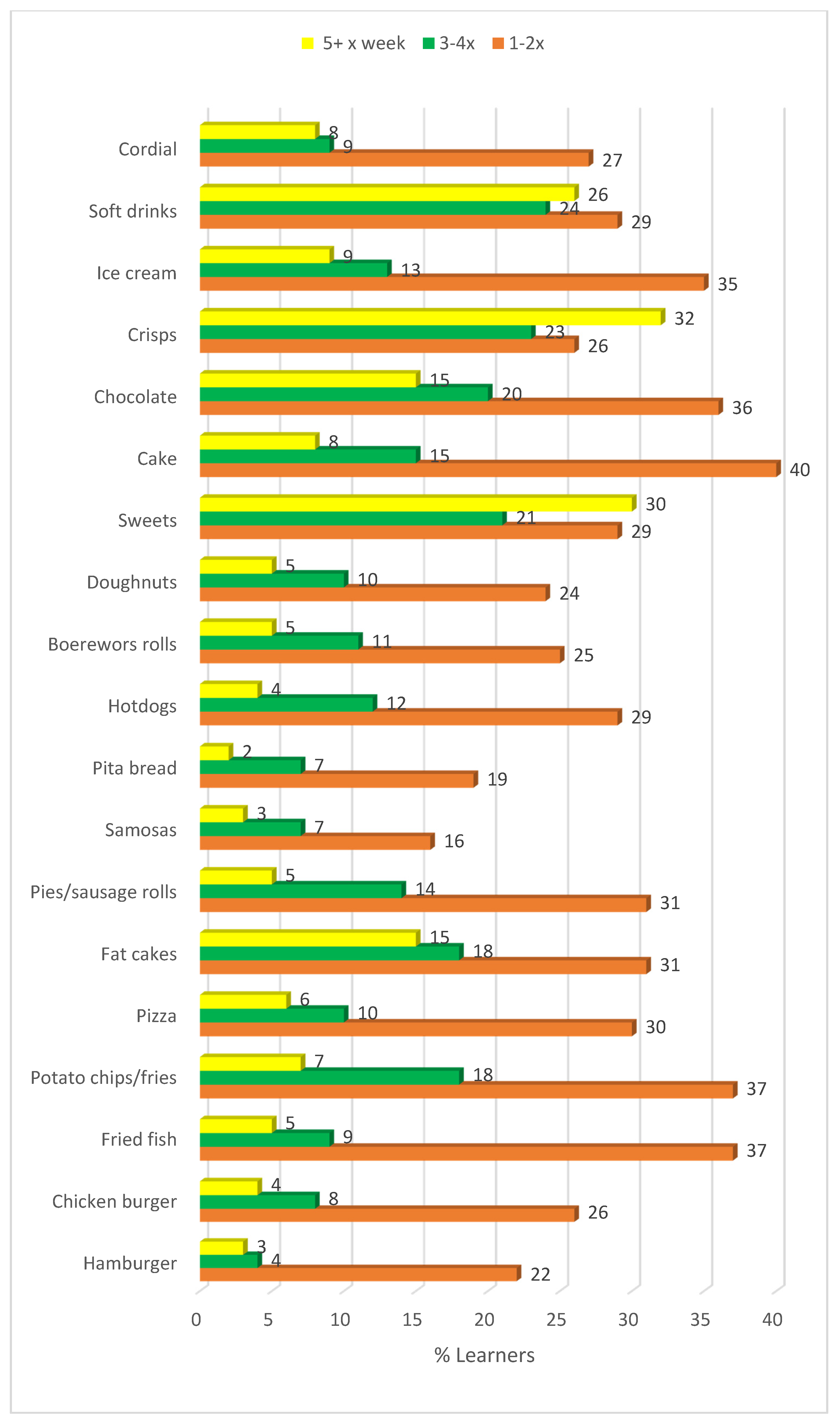
3.4. Frequency of Takeaway Food Consumed by Learners in the Past Week
3.5. Snacking Habits While Watching Television
3.6. Sources of Nutrition Information
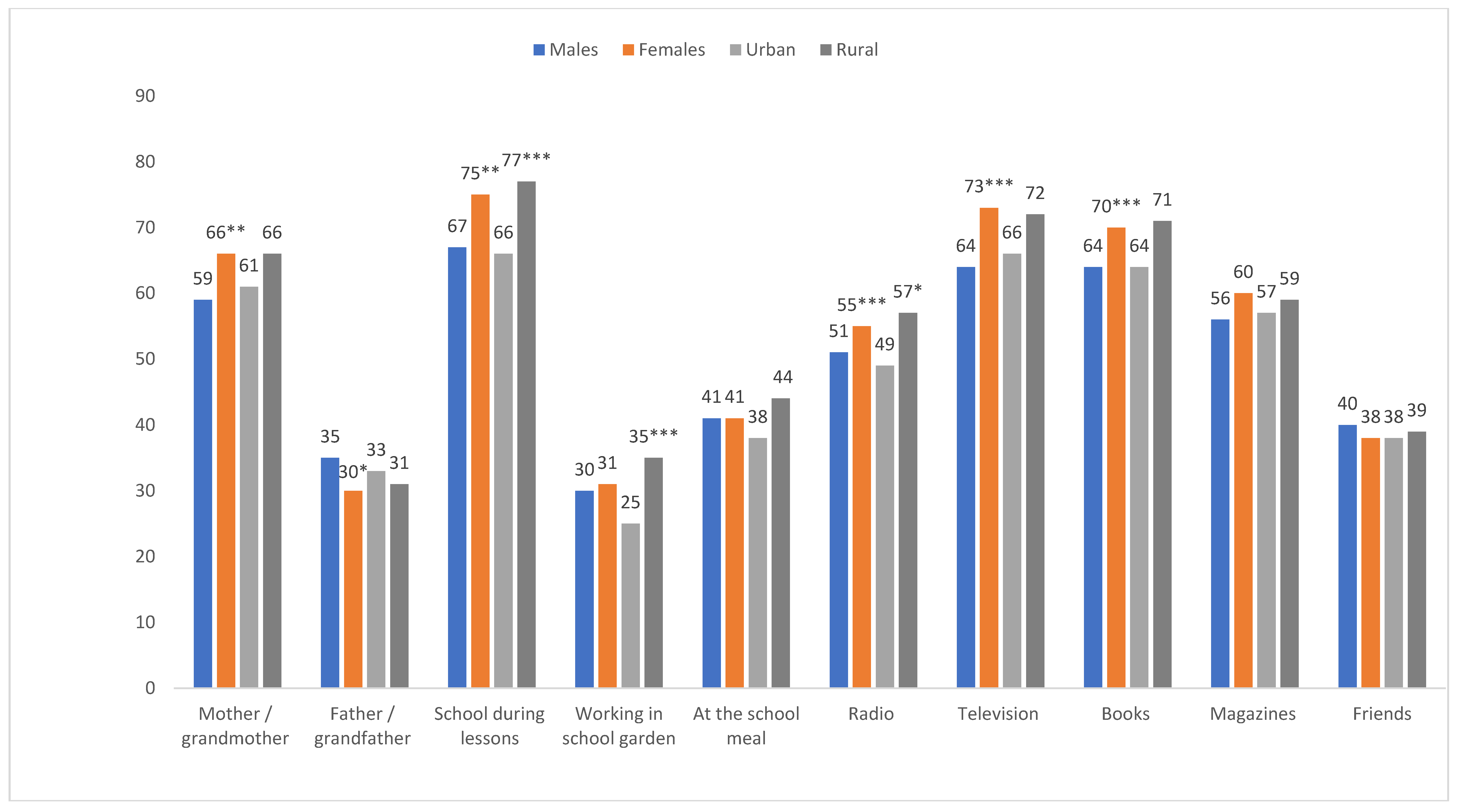
3.7. Variables Associated with Weight Status
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nittari, G.; Scuri, S.; Petrelli, F.; Pirillo, I.; Di Luca, N.M.; Grappasonni, I. Fighting obesity in children from European World Health Organization member states. Epidemiological data, medical-social aspects, and prevention programs. La Clin. Ter. 2019, 170, e223–e230. [Google Scholar]
- Sanyaolu, A.; Okorie, C.; Qi, X.; Locke, J.; Rehman, S. Childhood and Adolescent Obesity in the United States: A Public Health Concern. Glob. Pediatr. Health 2019, 6. [Google Scholar] [CrossRef]
- Choukem, S.-P.; Tochie, J.N.; Sibetcheu, A.T.; Nansseu, J.R.; Hamilton-Shield, J.P. Overweight/obesity and associated cardiovascular risk factors in sub-Saharan African children and adolescents: A scoping review. Int. J. Pediatr. Endocrinol. 2020, 2020, 1–13. [Google Scholar] [CrossRef]
- Reddy, S.P.; Resnicow, K.; James, S.; Funani, I.N.; Kambaran, N.S.; Omardien, R.G.; Masuka, P.; Sewpaul, R.; Vaughan, R.D.; Mbewu, A. Rapid Increases in Overweight and Obesity Among South African Adolescents: Comparison of Data From the South African National Youth Risk Behaviour Survey in 2002 and 2008. Am. J. Public Health 2012, 102, 262–268. [Google Scholar] [CrossRef]
- Shisana, O.; Labadarios, D.; Rehle, T.; Simbayi, L.; Zuma, K.; Dhansay, A.; Reddy, P.; Parker, W.; Hoosain, E.; Naidoo, P.; et al. South African National Health and Nutrition Examination Survey (SANHANES-1); HSRC Press: Cape Town, South Africa, 2014. [Google Scholar]
- Wrottesley, S.V.; Pedro, T.M.; Fall, C.H.; Norris, S. A review of adolescent nutrition in South Africa: Transforming adolescent lives through nutrition initiative. S. Afr. J. Clin. Nutr. 2019, 1–39. [Google Scholar] [CrossRef]
- Briefel, R.R.; Johnson, C.L. Secular trends in dietary intake in the United States. Annu. Rev. Nutr. 2004, 24, 401–431. [Google Scholar] [CrossRef]
- Hobbs, M.; Pearson, N.; Foster, P.J.; Biddle, S. Sedentary behaviour and diet across the lifespan: An updated systematic review. Br. J. Sports Med. 2014, 49, 1179–1188. [Google Scholar] [CrossRef]
- Pearson, N.; Biddle, S. Sedentary Behavior and Dietary Intake in Children, Adolescents, and Adults. Am. J. Prev. Med. 2011, 41, 178–188. [Google Scholar] [CrossRef]
- Poskitt, E.M.E. Countries in transition: Underweight to obesity non-stop? Ann. Trop. Paediatr. 2009, 29, 1–11. [Google Scholar] [CrossRef]
- Gorely, T.; Marshall, S.J.; Biddle, S. Couch kids: Correlates of television viewing among youth. Int. J. Behav. Med. 2004, 11, 152–163. [Google Scholar] [CrossRef]
- Coon, K.A.; Tucker, K.L. Television and children’s consumption patterns. A review of the literature. Minerva Pediatr. 2002, 54, 423–436. [Google Scholar] [PubMed]
- Williamson, V.G.; Dilip, A.; Dillard, J.R.; Morgan-Daniel, J.; Lee, A.M.; Cardel, M.I. The Influence of Socioeconomic Status on Snacking and Weight among Adolescents: A Scoping Review. Nutrients 2020, 12, 167. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, L.D.; Zuelch, M.L.; Dimitratos, S.; Scherr, R.E. Adolescent Obesity: Diet Quality, Psychosocial Health, and Cardiometabolic Risk Factors. Nutrients 2019, 12, 43. [Google Scholar] [CrossRef]
- Funtikova, A.N.; Navarro, E.; Bawaked, R.A.; Fitó, M.; Schröder, H. Impact of diet on cardiometabolic health in children and adolescents. Nutr. J. 2015, 14, 118. [Google Scholar] [CrossRef]
- Hill, D.; Moss, R.H.; Sykes-Muskett, B.; Conner, M.; O’Connor, D. Stress and eating behaviors in children and adolescents: Systematic review and meta-analysis. Appetite 2018, 123, 14–22. [Google Scholar] [CrossRef]
- Kuźbicka, K.; Rachoń, D. Bad eating habits as the main cause of obesity among children. Pediatr. Endocrinol. Diabetes Metab. 2013, 19, 106–110. [Google Scholar]
- Rebolledo, N.; Reyes, M.; Corvalán, C.; Popkin, B.; Taillie, L.S. Dietary Intake by Food Source and Eating Location in Low- and Middle-Income Chilean Preschool Children and Adolescents from Southeast Santiago. Nutrients 2019, 11, 1695. [Google Scholar] [CrossRef]
- Popkin, B.M.; Hawkes, C. Sweetening of the global diet, particularly beverages: Patterns, trends, and policy responses. Lancet Diabetes Endocrinol. 2016, 4, 174–186. [Google Scholar] [CrossRef]
- Keding, G. Nutrition Transition in Rural Tanzania and Kenya. Hidden Hunger. 2016, 115, 68–81. [Google Scholar] [CrossRef]
- Stats South Africa. Mid-Year Population Estimates Report P0302; Statistics South Africa: Pretoria, South Africa, 2017.
- Nana, A.; Zema, T. Dietary practices and associated factors during pregnancy in north-western Ethiopia. BMC Pregnancy Childbirth 2018, 18, 183. [Google Scholar] [CrossRef]
- Audain, K.A.; Veldman, F.J.; Kassier, S.M. A comparative analysis of nutritional status in adolescents from an urban versus a peri-urban school in Kwazulu-Natal, South Africa. Cent. Afr. J. Public Health 2015, 1, 25. [Google Scholar]
- Marfell-Jones, M.; Olds, T.; Stew, A.; Carter, L. International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: Underdale, Australia, 2006. [Google Scholar]
- WHO. Obesity: Preventing and Managing the Global Epidemic (Report of a World Health Organization Consultation). Available online: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ (accessed on 6 March 2019).
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef] [PubMed]
- WHO. Health for the World Adolescents. Recognizing Adolescents. Available online: https://apps.who.int/adolescent/second-decade/section2/page1/recognizing-adolescence.html#:~:text=The%20World%20Health%20Organization%20(WHO,the%20age%20of%2018%20years (accessed on 21 July 2020).
- Kruger, H.S.; Wissing, M.P.; Towers, W.; Doak, C.M. Sex Differences Independent of Other Psycho-sociodemographic Factors as a Predictor of Body Mass Index in Black South African Adults. J. Health Popul. Nutr. 2012, 30, 56–65. [Google Scholar] [CrossRef]
- Department of Health & South African Medical Research Council (MRC). South Africa Demographic and Health Survey: 2016; Department of Health & South African Medical Research Council (MRC): Pretoria, South Africa, 2017.
- Baalwa, J.; Byarugaba, B.B.; Kabagambe, E.K.; Otim, A.M. Prevalence of overweight and obesity in young adults in Uganda. Afr. Health Sci. 2010, 10, 367–373. [Google Scholar]
- Olatunbosun, S.T.; Kaufman, J.S.; Bella, A.F. Prevalence of obesity and overweight in urban adult Nigerians. Obes. Rev. 2010, 12, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Letamo, G. The prevalence of, and factors associated with, overweight and obesity in botswana. J. Biosoc. Sci. 2010, 43, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Steyn, N.P.; Nel, J.H.; Parker, W.-A.; Ayah, R.; Mbithe, D. Dietary, social, and environmental determinants of obesity in Kenyan women. Scand. J. Public Health 2010, 39, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Zagorsky, J.L. Health and wealth: The late-20th Century obesity epidemic in the US. Econ. Hum. Biol. 2005, 3, 296–313. [Google Scholar] [CrossRef]
- Case, A.; Menendez, A. Sex differences in obesity rates in poor countries: Evidence from South Africa. Econ. Hum. Boil. 2009, 7, 271–282. [Google Scholar] [CrossRef]
- Mayosi, B.; Flisher, A.J.; Lalloo, U.G.; Sitas, F.; Tollman, S.M.; Bradshaw, D. The burden of non-communicable diseases in South Africa. Lancet 2009, 374, 934–947. [Google Scholar] [CrossRef]
- Micklesfield, L.; Lambert, E.V.; Hume, D.J.; Chantler, S.; Pienaar, P.R.; Dickie, K.; Puoane, T.; Goedecke, J.H. Socio-cultural, environmental and behavioural determinants of obesity in black South African women: Review articles. Cardiovasc. J. Afr. 2013, 24, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Dake, F.A.; Tawiah, E.O.; Badasu, D.M. Sociodemographic correlates of obesity among Ghanaian women. Public Health Nutr. 2011, 14, 1285–1291. [Google Scholar] [CrossRef] [PubMed]
- Villamor, E.; Msamanga, G.; Urassa, W.; Petraro, P.; Spiegelman, D.; Hunter, D.J.; Fawzi, W.W. Trends in obesity, underweight, and wasting among women attending prenatal clinics in urban Tanzania, 1995–2004. Am. J. Clin. Nutr. 2006, 83, 1387–1394. [Google Scholar] [CrossRef] [PubMed]
- Mfenyana, K.; Griffin, M.; Yogeswaran, P.; Modell, B.; Modell, M.; Chandia, J.; Nazareth, I. Socio-economic inequalities as a predictor of health in South Africa—The Yenza cross-sectional study. S. Afr. Med. J. 2006, 96, 323–330. [Google Scholar] [PubMed]
- Costa, C.S.; Del-Ponte, B.; Assunção, M.C.F.; Santos, I.S. Consumption of ultra-processed foods and body fat during childhood and adolescence: A systematic review. Public Health Nutr. 2017, 21, 148–159. [Google Scholar] [CrossRef] [PubMed]
- Allman-Farinelli, M.; Partridge, S.R.; Roy, R. Weight-Related Dietary Behaviors in Young Adults. Curr. Obes. Rep. 2016, 5, 23–29. [Google Scholar] [CrossRef]
- Larson, N.; Story, M. A Review of Snacking Patterns among Children and Adolescents: What Are the Implications of Snacking for Weight Status? Child. Obes. 2013, 9, 104–115. [Google Scholar] [CrossRef]
- Moreno, L.A.; Rodríguez, G. Dietary risk factors for development of childhood obesity. Curr. Opin. Clin. Nutr. Metab. Care 2007, 10, 336–341. [Google Scholar] [CrossRef]
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 2020, 395, 65–74. [Google Scholar] [CrossRef]
- Sedibe, M.H.; Pisa, P.T.; Feeley, A.B.; Pedro, T.; Kahn, K.; Norris, S. Dietary Habits and Eating Practices and Their Association with Overweight and Obesity in Rural and Urban Black South African Adolescents. Nutrients 2018, 10, 145. [Google Scholar] [CrossRef]
- Mameli, C.; Mazzantini, S.; Zuccotti, G.V. Nutrition in the First 1000 Days: The Origin of Childhood Obesity. Int. J. Environ. Res. Public Health 2016, 13, 838. [Google Scholar] [CrossRef] [PubMed]
| Variables | Variable | n | % |
|---|---|---|---|
| Age (years) | 11–14 | 225 | 16.6 |
| 15–17 | 606 | 44.7 | |
| 18–26 | 526 | 38.8 | |
| Gender | Male | 529 | 38.9 |
| Female | 831 | 61.1 | |
| Race | Black African | 1315 | 96.8 |
| White | 7 | 0.5 | |
| Mixed ancestry | 35 | 2.6 | |
| Indian | 2 | 0.1 | |
| Geographic location | Urban | 653 | 48.0 |
| Rural | 707 | 52.0 | |
| School quintiles | 1 and 2 | 612 | 45.0 |
| 3 | 748 | 55.0 | |
| Grade | 8 | 250 | 18.6 |
| 9 | 188 | 14 | |
| 10 | 336 | 24.9 | |
| 11 | 381 | 28.3 | |
| 12 | 192 | 14.3 | |
| Mother’s highest education | None | 88 | 6.5 |
| Primary | 220 | 16.2 | |
| High school | 826 | 60.8 | |
| Tertiary | 220 | 16.2 | |
| Don’t know | 5 | 0.4 | |
| Father’s highest education | None | 150 | 11.1 |
| Primary | 211 | 15.6 | |
| High school | 692 | 51.1 | |
| Tertiary | 286 | 21.1 | |
| Don’t know | 14 | 1.0 |
| Males (%) | Females (%) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | All Males | 11–14 | 15–17 | 18–26 | p-Value | Urban | Rural | p-Value | All Females | 11–14 | 15–17 | 18–26 | p-Value | Urban | Rural | p-Value |
| n | 474 | 78 | 173 | 223 | 221 | 253 | 764 | 127 | 369 | 268 | 320 | 444 | ||||
| Mean BMI kgm2 (SD) | 20.7 &&& 0.18 | 19.3 (A) 0.25 | 20.4 (B) 0.26 | 21.4 (C) 0.21 | >0.05 | 21.0 0.24 | 20.4 0.22 | >0.05 | 23.9 0.26 | 21.7 [B] 0.46 | 23.9 [A] 0.34 | 24.9 [A] 0.33 | p < 0.05 | 24.3 0.35 | 23.6 0.34 | >0.05 |
| % Underweight | 13.3 | 10.3 | 15.6 | 12.6 | 0.124 | 13.6 | 13.0 | 0.014 * | 5.5 | 6.3 | 6.0 | 4.5 | 0.402 | 6.3 | 5.0 | 0.070 |
| % Normal weight | 76.8 | 75.6 | 76.9 | 77.1 | 72.4 | 80.6 | 58.4 | 66.1 | 58.5 | 54.5 | 52.5 | 62.6 | ||||
| % Overweight | 7.4 | 12.8 | 4.6 | 7.6 | 10.0 | 5.1 | 23.8 | 19.7 | 23.8 | 25.7 | 25.3 | 22.7 | ||||
| % Obese | 2.5 | 1.3 | 2.9 | 2.7 | 4.1 | 1.2 | 12.3 | 7.9 | 11.7 | 15.3 | 15.9 | 9.7 | ||||
| % Overweight and obese | 9.9 | 14.1 | 7.5 | 10.3 | <0.05 # | 14.0 | 6.3 | <0.001 *** | 36.1 | 27.6 | 35.5 | 41.0 | 0.053 | 41.3 | 32.4 | <0.023 $ |
| Frequency | Total (%) | Gender | Place of Residence | |||||
|---|---|---|---|---|---|---|---|---|
| n = 1336 | Male n (%) | Female n (%) | Rao–Scott Chi-sq. p-Value | Urban n (%) | Rural n (%) | Rao–Scott Chi-sq. p-Value | ||
| Number days breakfast is usually eaten on weekdays | ≤2 | 435 (32.6) | 151 (29.1) | 284 (34.8) | 0.002 ** | 241 (37.9) | 194 (27.7) | <0.001 *** |
| 3–5 | 901 (67.4) | 368 (70.9) | 533 (65.2) | 395 (62.1) | 506 (72.3) | |||
| Number of days breakfast is usually eaten on weekends | ≤1 | 369 (27.5) | 153 (29.3) | 216 (26.3) | 0.339 | 215 (33.8) | 154 (21.8) | <0.001 *** |
| 2 | 973 (72.5) | 369 (70.7) | 604 (73.7) | 422 (66.2) | 551 (78.2) | |||
| Number of meals usually eaten on weekdays | 1-2 | 530 (40.2) | 212 (41.5) | 318 (39.5) | 0.684 | 237 (37.9) | 293 (42.4) | 0.359 |
| ≥3 | 787 (59.8) | 299 (58.5) | 488 (60.5) | 389 (62.1) | 398 (57.6) | |||
| Number of meals usually eaten on weekends | 1-2 | 507 (38.1) | 212 (41.1) | 295 (36.3) | 0.189 | 239 (38.1) | 268 (38.2) | 0.992 |
| ≥3 | 822 (61.9) | 304 (58.9) | 518 (63.7) | 388 (61.9) | 434 (61.8) | |||
| Number of times snacks are usually eaten per day | ≤2 | 944 (70.1) | 397 (75.8) | 547 (66.5) | 0.008 ** | 444 (69.1) | 500 (71.0) | 0.601 |
| ≥3 | 403 (29.9) | 127 (24.2) | 276 (33.5) | 199 (30.9) | 204 (29.0) | |||
| Number of times of drinking hot drinks# per day | ≤2 | 1080 (80.2) | 416 (79.4) | 664 (80.7) | 0.701 | 489 (76.0) | 591 (83.9) | <0.001 *** |
| ≥3 | 267 (19.8) | 108 (20.6) | 159 (19.3) | 154 (24.0) | 113 (16.1) | |||
| Number of teaspoons added to hot drinks | 0–1 | 321 (24.3) | 117 (22.9) | 204 (25.2) | 0.264 | 121 (19.5) | 200 (28.7) | <0.001 *** |
| ≥2 | 999 (75.7) | 395 (77.1) | 604 (74.8) | 501 (80.5) | 298 (71.3) | |||
| Mean (CI) | Mean (CI) | Mean (CI) | p-Value | Mean (CI) | Mean (CI) | p-Value | ||
| Frequency of eating breakfast on weekdays | 3.1 (3.0–3.2) | 3.2 (3.1–3.3) | 3.0 (3.0–3.1) | 0.005 ** | 3.0 (2.8–3.1) | 3.2 (3.1–3.3) | <0.001 *** | |
| Frequency of taking a lunch box to school in past week | 2.1 (1.9–2.3) | 1.7(1.6–1.9) | 2.3 (2.1–2.5) | <0.001 *** | 2.2 (2.0–2.3) | 2.0 (1.7–2.3) | 0.358 | |
| Frequency of takeaways (past week) | 3.9 (3.6–4.2) | 3.7 (3.4–4.1) | 4.0 (3.7–4.4) | 0.166 | 4.0 (3.5–4.5) | 3.9 (3.4–4.3) | 0.679 | |
| Fried and fatty snacks (past week) | 3.1 (2.9–3.2) | 2.9 (2.7–3.1) | 3.2 (2.9–3.4) | 0.108 | 3.1 (2.9–3.3) | 3.1 (2.7–3.4) | 0.794 | |
| Sugary snacks (past week) | 7.2 (6.7–7.6) | 6.5(6.1–6.9) | 7.6 (6.9–8.3) | 0.007 ** | 6.9 (6.2–7.7) | 7.4 (6.7–8.2) | 0.274 | |
| Salty snacks (past week) | 1.6 (1.5–1.8) | 1.5 (1.3–1.7) | 1.7 (1.6–1.9) | 0.014 * | 1.6 (1.3–1.9) | 1.7 (1.5–1.9) | 0.631 | |
| Healthy TV snacks (past week) | 2.4 (1.9–2.8) | 2.5 (2.0–3.1) | 2.2 (1.9–2.6) | 0.045 * | 2.4 (1.4–3.4) | 2.3 (2.0–2.7) | 0.854 | |
| Unhealthy TV snacks (past week) | 8.5 (7.1–10.0) | 9.1 (7.3–10.8) | 8.1 (6.9–9.4) | 0.019 * | 8.3(4.9–11.8) | 8.7 (7.4–9.9) | 0.809 | |
| Frequency | Total n (%) | Gender | Place of Residence | |||||
|---|---|---|---|---|---|---|---|---|
| Male n (%) | Female n (%) | Rao–Scott Chi-sq. p-Value | Urban n (%) | Rural n (%) | Rao–Scott Chi-Square p-Value | |||
| Frequency of eating cooked porridge with milk for breakfast | 0–2 | 1001 (74.8) | 385 (73.9) | 616 (75.3) | 0.643 | 467 (73.7) | 534 (75.7) | 0.294 |
| 3–5 | 338 (25.2) | 136 (26.1) | 202 (24.7) | 167 (26.3) | 171 (24.3) | |||
| Frequency of eating cooked porridge without milk for breakfast | 0–2 | 1107(83.7) | 415 (80.3) | 692 (85.9) | p < 0.001 *** | 521 (84.3) | 586 (83.1) | 0.564 |
| 3–5 | 216 (16.3) | 102 (19.7) | 114 (14.1) | 97 (15.7) | 119 (16.9) | |||
| Frequency of eating instant cereal with milk for breakfast | 0–2 | 941 (71.0) | 382 (73.7) | 559 (69.3) | 0.269 | 431 (69.4) | 510 (72.4) | 0.237 |
| 3–5 | 384 (29.0) | 136 (26.3) | 248 (30.7) | 190 (30.6) | 194 (27.6) | |||
| Frequency of eating white bread with spread for breakfast | 0–2 | 942 (70.9) | 380 (73.2) | 562 (69.4) | 0.098 | 442 (70.8) | 500 (70.9) | 0.976 |
| 3–5 | 387 (29.1) | 139 (26.8) | 248 (30.6) | 182 (29.2) | 205 (29.1) | |||
| Frequency of eating white bread without spread for breakfast | 0–2 | 1100 (83.1) | 425 (82.2) | 675 (83.7) | 0.593 | 522 (84.5) | 578 (82.0) | 0.144 |
| 3–5 | 223 (16.9) | 92 (17.8) | 131 (16.3) | 96 (15.5) | 127 (18.0) | |||
| Frequency of eating brown bread with spread for breakfast | 0–2 | 893 (67.4) | 350 (67.2) | 543 (67.5) | 0.880 | 410 (66.1) | 483 (68.5) | 0.386 |
| 3–5 | 432 (32.6) | 171 (32.8) | 261 (32.5) | 210 (33.9) | 222 (31.5) | |||
| Frequency of eating brown bread without spread for breakfast | 0–2 | 1075 (81.3) | 31.6 (81.0) | 657 (81.4) | 0.859 | 510 (82.5) | 565 (80.1) | 0.106 |
| 3–5 | 248 (18.7) | 98 (19.0) | 150 (18.6) | 108 (17.5) | 140 (19.9) | |||
| Frequency of drinking milk or yoghurt for breakfast | 0–2 | 914 (68.8) | 364(70.4) | 550 (67.7) | 0.110 | 415 (66.5) | 499 (70.8) | 0.066 |
| 3–5 | 415 (31.2) | 153 (29.6) | 262 (32.3) | 209 (33.5) | 206 (29.2) | |||
| Frequency of drinking tea or coffee with milk for breakfast | 0–2 | 822 (61.7) | 310 (59.5) | 512 (63.1) | 0.090 | 413 (65.9) | 409 (58.0) | 0.003 ** |
| 3–5 | 510 (38.3) | 211 (40.5) | 299 (36.9) | 214 (34.1) | 296 (42.0) | |||
| Frequency of drinking tea or coffee without milk for breakfast | 0–2 | 996 (75.4) | 391 (75.8) | 605 (75.2) | 0.794 | 472 (76.6) | 524 (74.3) | 0.320 |
| 3–5 | 325 (24.6) | 125 (24.2) | 200 (24.8) | 144 (23.4) | 181 (25.7) | |||
| Frequency of eating fruit for breakfast | 0–2 | 712 (53.4) | 284 (54.7) | 428 (52.6) | 0.516 | 346 (55.1) | 366 (51.9) | 0.541 |
| 3–5 | 621 (46.6) | 235 (45.3) | 386 (47.4) | 282 (44.9) | 339 (48.1) | |||
| Factors | BMI Status | Bivariate Logistic Regression | ||||||
|---|---|---|---|---|---|---|---|---|
| Underweight n (%) | Normal weight n (%) | Overweight n (%) | Obese n (%) | Rao–Scott Chi-Square p-Value | Risk of Underweight OR (95% CI) | Risk of Overweight or/Obesity OR (95% CI) | Risk of Obesity OR (95% CI) | |
| Grade | n = 105 UW | n = 323 OV + O | n = 106 O | |||||
| 8 | 17 (7.6) | 165 (74.0) | 31 (13.9) | 10 (4.5) | 0.1681 | Ref | Ref | Ref |
| 9 | 17 (10.0) | 110 (64.7) | 29 (17.1) | 14 (8.2) | 1.28 (0.47–3.50) | 1.33 (0.71–2.48) | 1.68 (0.63–4.49) | |
| 10 | 34 (11.1) | 193 (63.3) | 47 (15.4) | 31 (10.2) | 1.45 (0.62–3.40) | 1.35 (0.87–2.11) | 2.13 (1.04–4.33) * | |
| 11 | 22 (6.4) | 228 (65.9) | 66 (19.1) | 30 (8.7) | 0.79 (0.29–2.14) | 1.51 (0.92–2.47) | 1.79 (0.70–4.59) | |
| 12 | 13 (7.2) | 110 (60.8) | 39 (21.5) | 19 (10.5) | 0.93 (0.46–1.91) | 1.94 (1.05–3.58) * | 2.30 (0.81–6.54) | |
| Gender | ||||||||
| Male | 63 (13.3) | 364 (76.8) | 35 (7.4) | 12 (2.5) | <0.001 *** | 2.54 (1.47–4.39) ** | 0.20 (0.13–0.31) *** | 0.18 (0.08–0.44) ** |
| Female | 42 (5.5) | 446 (58.4) | 182 (23.8) | 94 (12.3) | Ref | Ref | Ref | |
| Mother’s highest level education | ||||||||
| None | 8 (10.1) | 60 (75.9) | 8 (10.1) | 3 (3.8) | 0.655 | Ref | Ref | Ref |
| Primary | 15 (7.4) | 135 (66.2) | 38 (18.6) | 16 (7.8) | 0.79 (0.27–2.27) | 1.86 (0.92–3.76) | 1.77 (0.45–6.95) | |
| High school | 66 (8.8) | 488 (65.2) | 132 (17.6) | 63 (8.4) | 0.93 (0.45–1.94) | 1.77 (1.10–2.83) * | 1.86 (0.49–7.11) | |
| Tertiary | 16 (8.0) | 125 (62.2) | 37 (18.4) | 23 (11.4) | 0.84 (0.37–1.92) | 2.14 (1.09–4.23) * | 2.63 (0.56–12.41) | |
| Father’s highest level of education | ||||||||
| None | 15 (10.6) | 93 (66.0) | 24 (17.0) | 9 (6.4) | 0.992 | Ref | Ref | Ref |
| Primary | 14 (6.9) | 135 (66.8) | 35 (17.3) | 18 (8.9) | 0.60 (0.28–1.28) | 1.17 (0.62–2.21) | 1.50 (0.55–4.12) | |
| High school | 51 (8.3) | 401 (65.3) | 109 (17.8) | 53 (8.6) | 0.68 (0.34–1.35) | 1.07 (0.73–1.57) | 1.34 (0.46–3.90) | |
| Tertiary | 22 (8.4) | 169 (64.8) | 45 (17.2) | 25 (9.6) | 0.71 (0.39–1.30) | 1.13 (0.64–2.00) | 1.54 (0.40–5.97) | |
| School location | ||||||||
| Urban | 50 (9.2) | 328 (60.6) | 103 (19.0) | 60 (11.1) | 0.020 * | Ref | Ref | Ref |
| Rural | 55 (7.9) | 482 (69.2) | 114 (16.4) | 46 (6.6) | 1.02 (0.59–1.76) | 0.88 (0.64–1.21) | 0.69 (0.36–1.30) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okeyo, A.P.; Seekoe, E.; de Villiers, A.; Faber, M.; Nel, J.H.; Steyn, N.P. Dietary Practices and Adolescent Obesity in Secondary School Learners at Disadvantaged Schools in South Africa: Urban–Rural and Gender Differences. Int. J. Environ. Res. Public Health 2020, 17, 5864. https://doi.org/10.3390/ijerph17165864
Okeyo AP, Seekoe E, de Villiers A, Faber M, Nel JH, Steyn NP. Dietary Practices and Adolescent Obesity in Secondary School Learners at Disadvantaged Schools in South Africa: Urban–Rural and Gender Differences. International Journal of Environmental Research and Public Health. 2020; 17(16):5864. https://doi.org/10.3390/ijerph17165864
Chicago/Turabian StyleOkeyo, Alice P., Eunice Seekoe, Anniza de Villiers, Mieke Faber, Johanna H. Nel, and Nelia P. Steyn. 2020. "Dietary Practices and Adolescent Obesity in Secondary School Learners at Disadvantaged Schools in South Africa: Urban–Rural and Gender Differences" International Journal of Environmental Research and Public Health 17, no. 16: 5864. https://doi.org/10.3390/ijerph17165864
APA StyleOkeyo, A. P., Seekoe, E., de Villiers, A., Faber, M., Nel, J. H., & Steyn, N. P. (2020). Dietary Practices and Adolescent Obesity in Secondary School Learners at Disadvantaged Schools in South Africa: Urban–Rural and Gender Differences. International Journal of Environmental Research and Public Health, 17(16), 5864. https://doi.org/10.3390/ijerph17165864





