Physiological Response of Quality Cardiopulmonary Resuscitation, Crossover Trial on Mannequin in Extreme Temperature Conditions
Abstract
1. Introduction
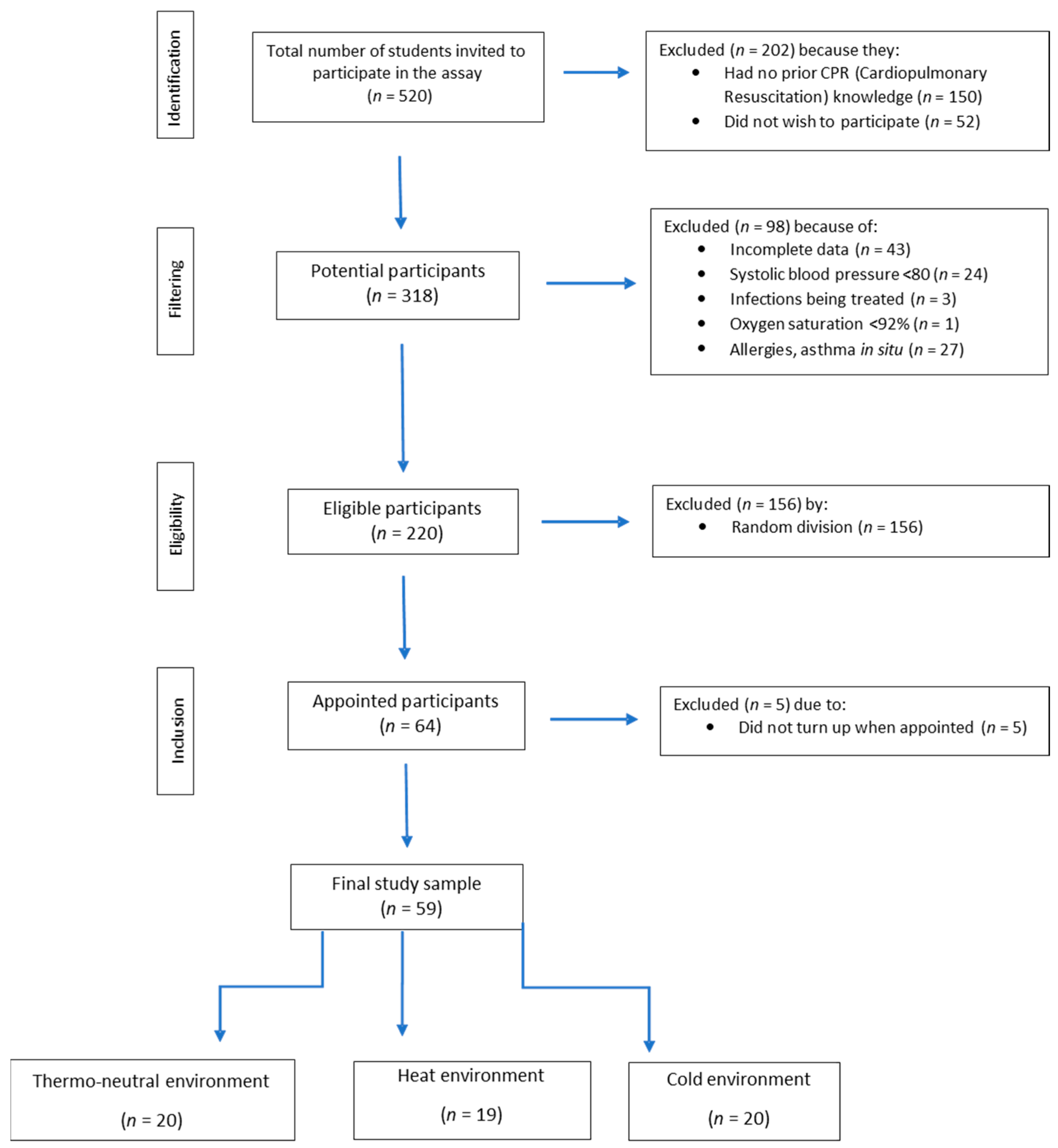
2. Materials and Methods
2.1. Study Design
2.2. Population
2.3. Study Protocol
2.4. Data Analysis
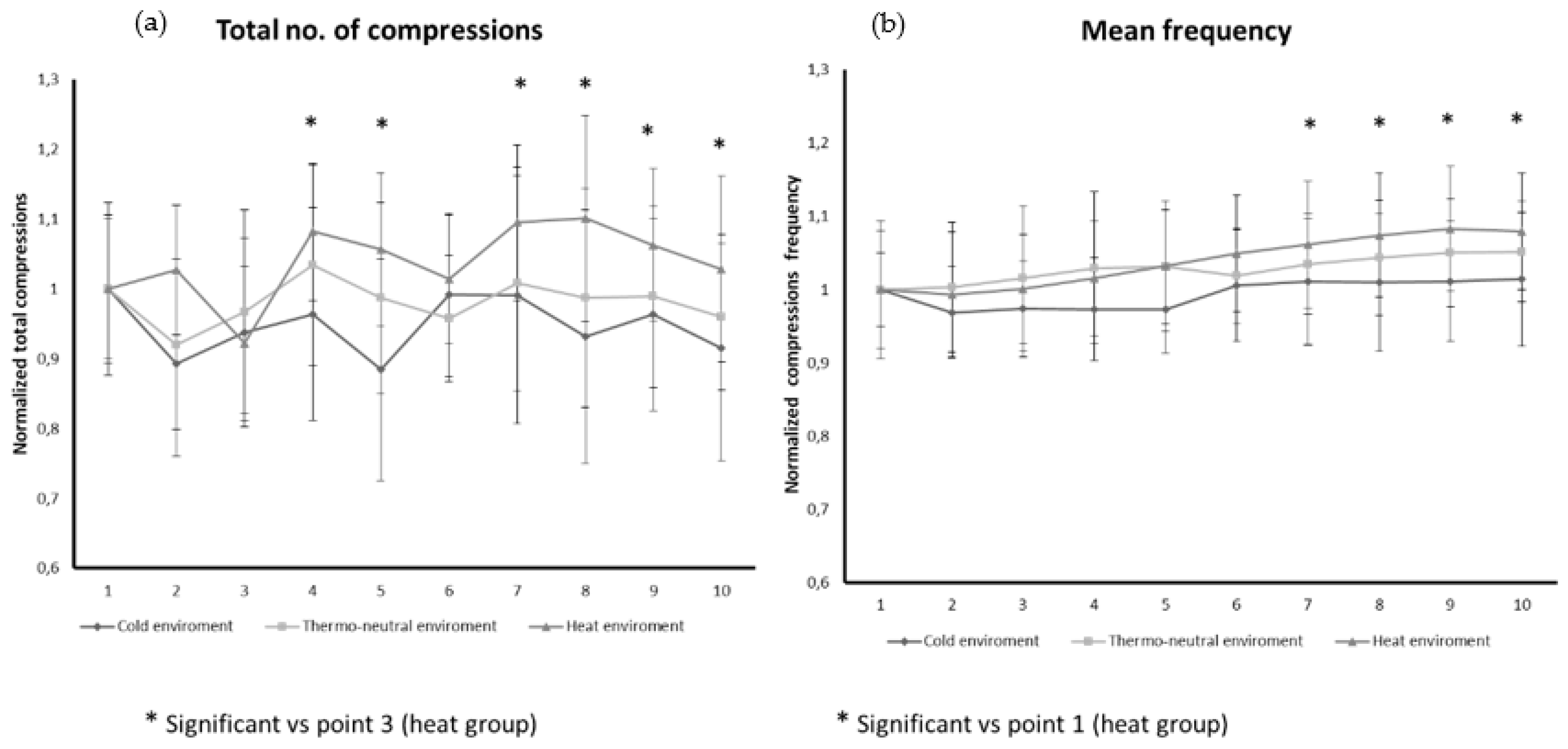
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rosell-Ortiz, F.; Escalada-Roig, X.; Fernández del Valle, P.; Sánchez-Santos, L.; Navalpotro-Pascual, J.M.; Echarri-Sucunza, A.; Adsuar-Quesada, J.M.; Ceniceros-Rozalén, I.; Ruiz-Azpiazu, J.I.; Ibarguren-Olalde, K.; et al. Out-of hospital cardiac arrest (OHCA) attended by mobile emergency teams with a physician on board. Results of the Spanish OHCA Registry (OSHCAR). Resuscitation 2017, 113, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Thorsten Gräsner, J.; Lefering, R.; Koster, R.W.; Masterson, S.; Böttiger, B.W.; Herlitz, J.; Wnent, J.; Tjelmeland, I.B.M.; Rosell Ortiz, F.; Maurer, H.; et al. EuReCa ONE—27 Nations, ONE Europe, ONE Registry. A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation 2016, 105, 188–195. [Google Scholar] [PubMed]
- Requena-Morales, R.; Palazón-Bru, A.; Rizo-Baeza, M.M.; Adsuar-Quesada, J.M.; Gil-Guillén, V.F.; Cortés-Castell, E. Mortality after out-of-hospital cardiac arrest in a Spanish Region. PLoS ONE 2017, 12, e0175818. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, C.; Booth, S.; Ji, C.; Brace-McDonnell, S.J.; Whittington, A.; Mapstone, J.; Cooke, M.W.; Deakin, C.D.; Gale, C.P.; Fothergill, R.; et al. Epidemiology and outcomes from out-of-hospital cardiac arrests in England. Resuscitation 2017, 110, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Yamanaka, S.; Young Huh, J.; Nishiyama, K.; Hayashi, H. The optimal number of personnel for good quality of chest compressions: A prospective randomized parallel manikin trial. PLoS ONE 2017, 12, e0189412. [Google Scholar] [CrossRef]
- Kleinman, M.E.; Goldberger, Z.D.; Rea, T.; Swor, R.A.; Bobrow, B.J.; Brennan, E.E.; Terry, M.; Hemphill, R.; Gazmuri, R.J.; Hazinski, M.F.; et al. 2017 American Heart Association Focused Update on Adult Basic Life Support and Cardiopulmonary Resuscitation Quality. Circulation 2018, 137, e7–e13. [Google Scholar] [CrossRef]
- Shin, J.; Hwang, S.Y.; Lee, H.J.; Park, C.J.; Kim, Y.J.; Son, Y.J.; Seo, J.S.; Kim, J.J.; Lee, J.E.; Lee, I.M.; et al. Comparison of CPR quality and rescuer fatigue between standard 30:2 CPR and chest compression-only CPR: A randomized crossover manikin trial. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 59. [Google Scholar] [CrossRef]
- Kwak, S.J.; Kim, Y.M.; Baek, H.J.; Hong Kim, S.; Woo Yim, H. Chest compression quality, exercise intensity, and energy expenditure during cardiopulmonary resuscitation using compression-to-ventilation ratios of 15:1 or 30:2 or chest compression only: A randomized, crossover manikin study. Clin. Exp. Emerg. Med. 2016, 3, 148–157. [Google Scholar] [CrossRef]
- Hong, J.Y.; Oh, J.H. Variations in chest compression time, ventilation time and rescuers’ heart rate during conventional cardiopulmonary resuscitation in trained male rescuers. Clin. Exp. Emerg. Med. 2019, 6, 31–35. [Google Scholar] [CrossRef]
- Abelairas-Gómez, C.; Rey, E.; González-Salvado, V.; Mecías-Calvo, M.; Rodríguez-Ruiz, E.; Rodríguez-Núñez, A. Acute muscle fatigue and CPR quality assisted by visual feedback devices: A randomized crossover simulation trial. PLoS ONE 2018, 13, e0203576. [Google Scholar] [CrossRef]
- Li, E.; Cheung, P.Y.; O’Reilly, M.; Schmölzer, G.M. Rescuer fatigue during simulated neonatal cardiopulmonary resuscitation. J. Perinatol. 2015, 35, 142–145. [Google Scholar] [CrossRef] [PubMed]
- Ogata, H.; Fujimaru, I.; Kondo, T. Degree of exercise intensity during continuous chest compression in upper-body-trained individuals. J. Physiol. Anthropol. 2015, 34, 43. [Google Scholar] [CrossRef]
- Rosell-Ortiz, F.; Escalada-Roig, F.; Navalpotro Pascual, J.M.; Iglesias Vazquez, J.A.; Echarri Sucunza, A.; Cordero Torres, J.A.; Cobos, E.; Martínez del Valle, M.; Ceniceros Rozalen, I.; Martín Sánchez, E.; et al. Out-of-Hospital Spanish Cardiac Arrest Registry (OHSCAR). Results of the first year. Resucitation 2015, 96, 100. [Google Scholar] [CrossRef]
- Martín-Rodríguez, F.; Fernández-Pérez, C.; Castro-Villamor, M.A.; Martín-Conty, J.L.; Arnillas-Gómez, P.; Casado-Vicente, V. Does level D personal protective equipment guard against hazardous biologic agents during cardiopulmonary resuscitation? Emergencias 2018, 30, 119–122. [Google Scholar]
- Martín-Rodríguez, F.; Martín Conty, J.L.; Casado Vicente, V.; Arnillas Gómez, P.; Mohedano-Moriano, A.; Castro Villamor, M.A. Does Gender Influence Physiological Tolerance in Resuscitators When Using Personal Protection Equipment against Biological Hazards? Emerg. Med. Int. 2018, 2018, 5890535. [Google Scholar] [CrossRef] [PubMed]
- Barcala-Furelos, R.; Abelairas-Gomez, C.; Romo-Perez, V.; Palacios-Aguilar, J. Effect of physical fatigue on the quality CPR: A water rescue study of lifeguards: Physical fatigue and quality CPR in a water rescue. Am. J. Emerg. Med. 2013, 31, 473–477. [Google Scholar] [CrossRef]
- Sato, T.; Takazawa, T.; Inoue, M.; Tada, Y.; Suto, T.; Tobe, M.; Saito, S. Cardiorespiratory dynamics of rescuers during cardiopulmonary resuscitation in a hypoxic environment. Am. J. Emerg. Med. 2018, 36, 1561–1564. [Google Scholar] [CrossRef]
- Chen, J.; Lu, K.Z.; Yi, B.; Chen, Y. Chest Compression with Personal Protective Equipment During Cardiopulmonary Resuscitation: A Randomized Crossover Simulation Study. Medicine 2016, 95, e3262. [Google Scholar] [CrossRef]
- Martin-Conty, J.L.; Martin-Rodríguez, F.; Criado-Álvarez, J.J.; Romo Barrientos, C.; Maestre-Miquel, C.; Viñuela, A.; Polonio-López, B.; Durantez-Fernández, C.; Marcos-Tejedor, F.; Mohedano-Moriano, A. Do Rescuers’ Physiological Responses and Anxiety Influence Quality Resuscitation under Extreme Temperatures? Int. J. Environ. Res. Public Health 2020, 17, E4241. [Google Scholar] [CrossRef]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-Predicted Maximal Heart Rate Revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef]
- Simera, I.; Moher, D.; Hoey, J.; Schulz, K.F.; Altman, D.G. A catalogue of reporting guidelines for health research. Eur. J. Clin. Invest. 2010, 40, 35–53. [Google Scholar] [CrossRef] [PubMed]
- Mora Rodríguez, R.; Aguado Jiménez, R. Influencia del calor ambiental en un test incremental de umbral de AL. Arch. Med. Deporte Confed. Iberoam. Med. Deporte 2002, 19, 181–186. [Google Scholar]
- Brooks, G.A. Anaerobic threshold: Review of the concept and directions for future research. Med. Sci. Sports Exerc. 1985, 17, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Ochoa, F.J.; Ramalle-Gómara, E.; Lisa, V.; Saralegui, I. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation 1998, 37, 149–152. [Google Scholar] [CrossRef]
- Ashton, A.; McCluskey, A.; Gwinnutt, C.L.; Keenan, A.M. Effect of rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation 2002, 55, 151–155. [Google Scholar] [CrossRef]
- Petrofsky, J.S. The influence of recruitment order and temperature on muscle contraction with special reference to motor unit fatigue. Eur. J. Appl. Physiol. Occup. Physiol. 1981, 47, 17–25. [Google Scholar] [CrossRef]
- Barcala-Furelos, R.; Fernández-Méndez, M.; Cano-Noguera, F.; Otero-Agra, M.; Morán-Navarro, R.; Martínez-Isasi, S. Measuring the physiological impact of extreme heat on lifeguards during cardiopulmonary resuscitation. Randomized simulation study. Am. J. Emerg. Med. 2020, in press. [Google Scholar] [CrossRef]

| Variable | Thermo-Neutral Environment | Heat Environment | Cold Environment | p-Value ** |
|---|---|---|---|---|
| Number (n (%)) | 20 (33.9%) | 19 (32.2%) | 20 (33.9%) | |
| Age * | 20.85 ± 2.94 | 22.95 ± 2.65 | 20.40 ± 2.14 | 0.08 |
| Gender | 0.806 | |||
| Men (n (%)) | 8 (40%) | 9 (47.4%) | 10 (50%) | |
| Women (n (%)) | 12 (60%) | 10 (52.6%) | 10 (50%) | |
| Mean depth * | 4.97 ± 0.38 | 5.03 ± 0.42 | 4.97 ± 0.3 | 0.874 |
| Optimum depth of compressions * | 410 ± 200 | 445 ± 204 | 455 ± 182.2 | 0.740 |
| Mean frequency * | 114.5 ± 8.0 | 116.7 ± 7.91 | 110.4 ± 7.33 | 0.047 |
| Compressions in optimum zone * | 598.3 ± 239.4 | 464.1 ± 207.1 | 598.8 ± 172.8 | 0.070 |
| Compression fraction * | 84.8 ± 6.13 | 83.7 ± 5.82 | 86.1 ± 5.78 | 0.448 |
| Compressions in optimum depth zone and optimum frequency * | 289.5 ± 214.7 | 259.8 ± 165.6 | 319.2 ± 142.6 | 0.582 |
| Variable | Thermo-Neutral Environment | Heat Environment | Cold Environment | p-Value ** |
|---|---|---|---|---|
| HEART RATE | ||||
| Baseline * | 79.4 ± 15.4 | 78.32 ± 13.0 | 84.2 ± 14.9 | 0.467 |
| Min. 3 * | 135.6 ± 15.1 | 134.81 ± 17.2 | 135.2 ± 16.3 | 0.979 |
| Min. 6 * | 161.1 ± 26.4 | 153.9 ± 28.3 | 155.9 ± 22.0 | 0.737 |
| Min. 9 * | 158.9 ± 16.9 | 155.9 ± 21.8 | 156.8 ± 21.1 | 0.709 |
| Rest at 10 min. * | 96.1 ± 12.2 | 91.6 ± 15.3 | 99.7 ± 16.3 | 0.339 |
| LACTIC ACID | ||||
| Baseline * | 2.2 ± 1.5 | 1.9 ± 1.0 | 1.9 ± 1.2 | 0.734 |
| Min. 3 * | 3.8 ± 2.0 | 6.7 ± 5.4 | 3.0 ± 2.4 | <0.001 |
| Min. 6 * | 4.9 ± 2.8 | 6.3 ± 4.2 | 5.2 ± 4.9 | 0.356 |
| Min. 9 * | 4.1 ± 2.6 | 5.1 ± 3.3 | 5.0 ± 4.2 | 0.494 |
| Rest at 10 min. * | 3.5 ± 1.3 | 2.8 ± 1.5 | 2.8 ± 2.1 | 0.097 |
| Variable | Thermo-Neutral Environment | Heat Environment | Cold Environment | p-Value ** |
|---|---|---|---|---|
| HEART RATE > Anaerobic threshold | ||||
| Baseline * | 0 | 0 | 0 | - |
| Min. 3 * | 0 | 0 | 0 | - |
| Min. 6 * | 9 (45%) | 6 (31.6%) | 6 (30%) | 0.555 |
| Min. 9 * | 4 (20%) | 5 (26.9%) | 6 (30%) | 0.764 |
| Rest at 10 min. * | 0 | 0 | 0 | - |
| LACTIC ACID > 4 mmol/L | ||||
| Baseline * | 2 (10%) | 1 (5.3%) | 2 (10%) | 0.830 |
| Min. 3 * | 8 (40%) | 11 (57.9%) | 4 (20%) | 0.052 |
| Min. 6 * | 12 (60%) | 14 (73.7%) | 9 (45%) | 0.189 |
| Min. 9 * | 8 (40%) | 13 (68.4%) | 9 (45%) | 0.168 |
| Rest at 10 min. * | 8 (40%) | 3 (15.8%) | 4 (20%) | 0.175 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martin-Conty, J.L.; Polonio-López, B.; Maestre-Miquel, C.; Mohedano-Moriano, A.; Durantez-Fernández, C.; Mordillo-Mateos, L.; Jurado-Palomo, J.; Viñuela, A.; Bernal-Jiménez, J.J.; Martin-Rodríguez, F. Physiological Response of Quality Cardiopulmonary Resuscitation, Crossover Trial on Mannequin in Extreme Temperature Conditions. Int. J. Environ. Res. Public Health 2020, 17, 5835. https://doi.org/10.3390/ijerph17165835
Martin-Conty JL, Polonio-López B, Maestre-Miquel C, Mohedano-Moriano A, Durantez-Fernández C, Mordillo-Mateos L, Jurado-Palomo J, Viñuela A, Bernal-Jiménez JJ, Martin-Rodríguez F. Physiological Response of Quality Cardiopulmonary Resuscitation, Crossover Trial on Mannequin in Extreme Temperature Conditions. International Journal of Environmental Research and Public Health. 2020; 17(16):5835. https://doi.org/10.3390/ijerph17165835
Chicago/Turabian StyleMartin-Conty, José Luis, Begoña Polonio-López, Clara Maestre-Miquel, Alicia Mohedano-Moriano, Carlos Durantez-Fernández, Laura Mordillo-Mateos, Jesús Jurado-Palomo, Antonio Viñuela, Juan José Bernal-Jiménez, and Francisco Martin-Rodríguez. 2020. "Physiological Response of Quality Cardiopulmonary Resuscitation, Crossover Trial on Mannequin in Extreme Temperature Conditions" International Journal of Environmental Research and Public Health 17, no. 16: 5835. https://doi.org/10.3390/ijerph17165835
APA StyleMartin-Conty, J. L., Polonio-López, B., Maestre-Miquel, C., Mohedano-Moriano, A., Durantez-Fernández, C., Mordillo-Mateos, L., Jurado-Palomo, J., Viñuela, A., Bernal-Jiménez, J. J., & Martin-Rodríguez, F. (2020). Physiological Response of Quality Cardiopulmonary Resuscitation, Crossover Trial on Mannequin in Extreme Temperature Conditions. International Journal of Environmental Research and Public Health, 17(16), 5835. https://doi.org/10.3390/ijerph17165835







