Maternal and Child Survival in Haor Region in Bangladesh. An Analysis of Fathers’ Capabilities to Save the Future
Abstract
:1. Introduction
2. Materials and Methods
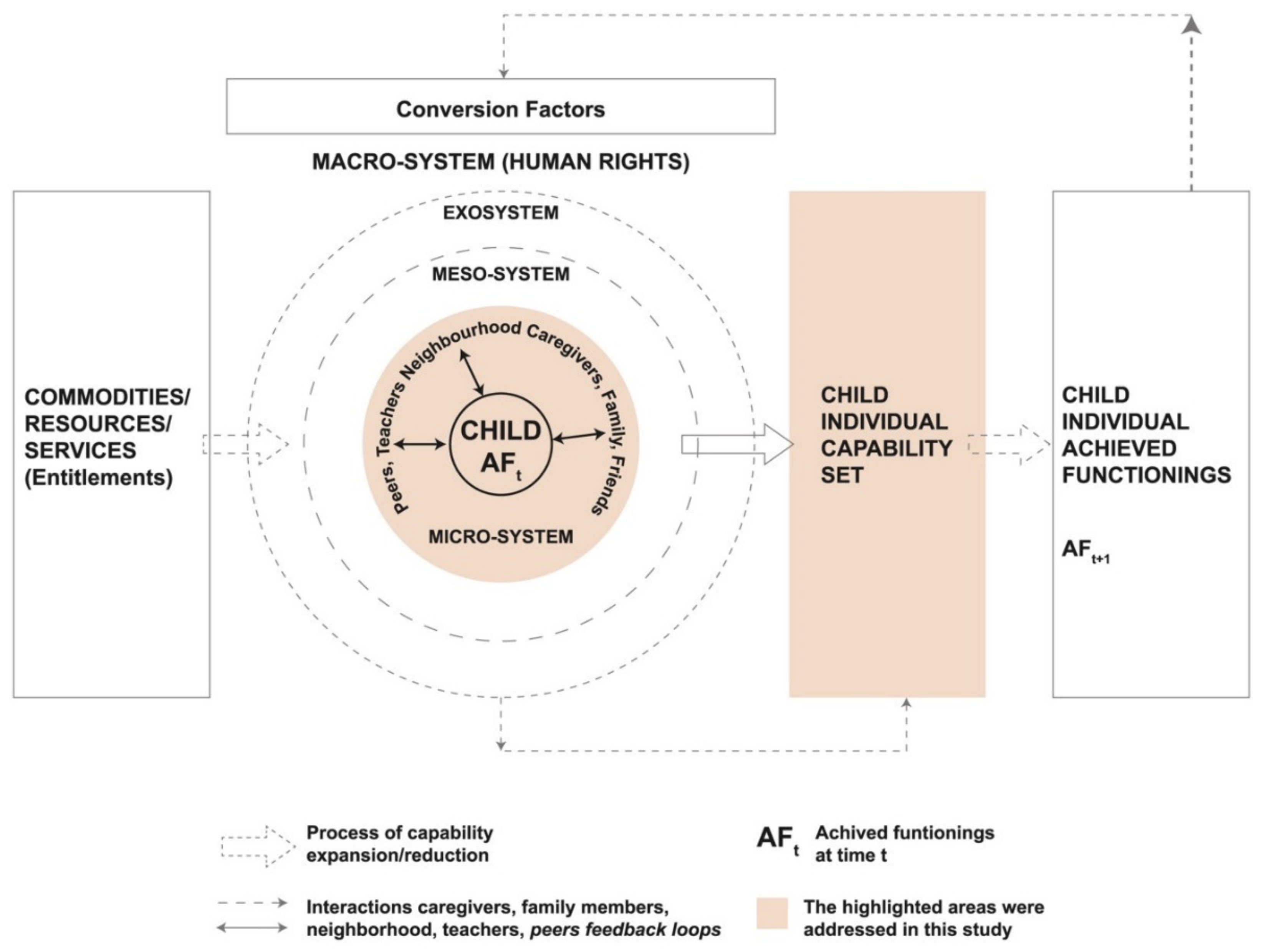
2.1. Conceptual Model
2.2. Study Area, Population, and NGO Involvement
2.3. Study Design and Participants’ Recruitment
2.4. Data Collection, Coding, and Analysis
2.5. Ethical Issues
3. Results
3.1. Participants in the Study
3.2. A Capability Analysis of “Saving the Future” in Haor
3.2.1. Being Able to Save the Lives of Mothers
“This is our main problem, particularly when there are women (pregnant women), you know! Danger comes once, it is called kaal bipod. During this danger time, we don’t get any shelter, we fall in huge trouble.”FGD, Fathers, Perua, Derai, 2nd round.
3.2.2. Being Able to Save the Lives of Children
“See, before marriage people dream of having a beautiful wife, then after getting married people dream of having babies. (Someone starts laughing) … No do not laugh! Why do you laugh? When we talk about the important aspects of marriage you laugh! See these children are our future. Now to get this future, if the future along with the person through whom the future is delivered, die, it takes us through the saddest experience of life. The saddest thing more than anything!”FGD, Fathers, Golbogi, Baniachang, 1st round
3.2.3. Endowments Underlying the Capability “to Save the Future”
3.3. Conversion Factors: Barriers and Facilitators of Father’s Capability “to Save the Future”
3.3.1. Lack of Communication About a Mother’s Health
“…She had an infection on one side of the bottom of her belly but she did not tell anyone about it. She didn’t tell anyone! Four months passed and when she was in her tenth month of pregnancy, the condition deteriorated and she was totally infected. …they admitted her to the government hospital at Banglabazar. The doctor didn’t give her any medicine. He said: ‘it is delivery pain; both baby and mother could die if they would be given any medicine’. That woman’s condition got worse but the doctor didn’t want to take any risk. They returned home, and went to another doctor. They bought medicine for the fever. After having that medicine, the baby probably died. It was stuck inside the mother’s womb! … Then they took out the baby through caesarean section, but both the mother and the baby died.”FGD, Mothers, Basakarach, Derai, 1st round
3.3.2. Inadequate Advice by Local Doctors
“She got water throughout the body. The body was swelled by water. The husband didn’t treat her. He said if I treat her for the body water the baby will die. Because the doctor said not to treat her for this, it may kill the baby. That’s why he didn’t do it. Then she had caesarean delivery, after 3 days my sister died.”FGD, Mothers, Sarail, Baniachang, 1st round
3.3.3. Fear of Having a Hospitalized Delivery
“We first try at home, all observe, the patient herself observes. In our area home delivery is better. For example, here the women need to do heavy work. If they go for caesarean they won’t be able to do such heavy works. We all want to have normal delivery at home.”FGD, Mothers, Chandipur, Baniachang, 1st Round
3.3.4. Reliance on God’s Mercy
“I didn’t take her for any checkup. One advised me to do ultrasonography, but I didn’t do because I have the confidence. Good or bad will be justified by God, what’s happening in our mind all are known by God”IDI, Father, Talibpur, Baniachang, 1st round
3.3.5. Poor Transportation Due to Flooding or Receding Water
“It was during the wet season, there was a high wave with storm, during that storm the baby’s mother had delivery pain and I was not getting a boat. There were huge waves in the river, I could not manage any boat. Thus, a day went by; in the end, I couldn’t reach the hospital.”FGD, Fathers, Rafinagar, Derai, 2nd round
“The vehicle is not available nearby the door; in other areas, the vehicles are available nearby the door. The reason is, there is no road. First a boat is required, then a vehicle is hired… You need to take this route (to reach the road where the vehicle becomes available) at least. You see, even if it is dry, there is no tempo (local motor vehicle with three wheels) available. A honda is available, but you can’t take her with a honda. Then she is to be taken by placing her on a hammock.”FGD, Mothers, Dalarkandi, Ashtagram, 2nd round
“…Now if half of us stay inside our homes we will remain well but if we move through the street, you know, … it is very difficult. The bumping of the vehicle makes the condition serious). If your disease is 50%, it will increase by 25% more. The condition gets worse…”FGD, Fathers, Golbogi, Baniachang, 1st round
“The baby was okay after the delivery. At the fifth day, it had pneumonia. After searching rigorously, they got a boat and took the baby. Next, they got a van, then they were required to move to a motor vehicle, but they didn’t get it. Then finally they got the vehicle but they were late. They got it around at 1–2 pm. Then they took the baby to the hospital. There the baby didn’t get the treatment. The patient was seriously ill. Now at the last minute, they took the patient to Habiganj. From there they had to take the baby to the doctor’s house but in the meantime the baby died, finally they couldn’t reach the doctor with their baby.”FGD, Mothers, Sarail, Baniachang, 1st round
3.4. Gender Issues and Mothers’ Autonomy
“Suppose we know how to go to another village, how to go to Mordanpur, Muradpur, but not all know how to reach there, particularly the women don’t know how to reach the place. There is one (health care centre) in Auladpur, and the other in Mordanpur. We need to walk to bring the doctors from there”FGD, Fathers, Makhonia, Baniachang, 1st round
“…to carry someone by hammock requires four people. Four people are not always available. If there would be a vehicle and a driver, the women could take the patient (to the hospital)”FGD, Mothers, Dalarkandi, Ashtagram, 2nd round
“…if the mother could do other work, could earn, then she would be able to spend it for health care, she could follow a doctor’s instructions, thus she could keep herself healthy”FGD, Fathers, Dhalbazar, Derai, 2nd round
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- National Institute of Population Research and Training (NIPORT); Mitra and Associates; ICF International. Bangladesh Demographic and Health Survey 2014; NIPORT: Dhaka, Bangladesh; Mitra and Associates: Dhaka, Bangladesh; ICF International: Dhaka, Bangladesh, 2016.
- UNICEF; WHO; World Bank Group; United Nations. Levels and Trends in Child Mortality 2019: Estimates Developed by the United Nations Inter-Agency Group for Child Mortality Estimation; UNICEF: New York, NY, USA, 2019. [Google Scholar]
- National Institute of Population and Training (NIPORT); International Center for Diaarroeal Disease Research Bangladesh (icddr, b); MEASURE Evaluation. Bangladesh Maternal Mortality and Health Care Survey 2016; Final Report; NIPORT (National Institute of Population Research and Training): Dhaka, Bangladesh; International Centre for Diarrhoeal Disease Research (icddr,b): Dhaka, Bangladesh; MEASURE Evaluation: Chapel Hill, NC, USA, 2019.
- National Institute of Population Research and Training (NIPORT); Associates for Community and Population Research (ACPR); ICG. Bangladesh Health Facility Survey 2017; NIPORT: Dhaka, Bangladesh; ACPR: Dhaka, Bangladesh; ICF: Dhaka, Bangladesh, 2018.
- National Institute of Population Research and Training (NIPORT); Associates for Community and Population Research (ACPR); ICF International. Bangladesh Health Facility Survey 2014; NIPORT (National Institute of Population Research and Training): Dhaka, Bangladesh; M&A (Mitra and Associates): Dhaka, Bangladesh; ICF International: Dhaka, Bangladesh, 2017.
- National Institute of Population Research and Training (NIPORT); MEASURE Evaluation; UNC-CH; USA International Center for Diaarroeal Disease Research Bangladesh (icddr, b). Bangladesh Maternal Mortality and Health Care Survey 2010; NIPORT (National Institute of Population Research and Training): Dhaka, Bangladesh; International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b): Dhaka, Bangladesh; MEASURE Evaluation: Dhaka, Bangladesh, 2012.
- Mosley, W.H.; Chen, L.C. An analytical framework for the study of child survival in developing countries. Popul. Dev. Rev. 1984, 10, 25. [Google Scholar] [CrossRef] [Green Version]
- Thaddeus, S.; Maine, D. Too far to walk: Maternal mortality in context. Soc. Sci. Med. 1994, 38, 1091–1110. [Google Scholar] [CrossRef]
- Sen, A. Development as capability expansion. In Readings in Human Development; Fukuda-Parr, S., Shiva Kumar, A.K., Eds.; Oxford University Press: New Delhi, India; New York, NY, USA, 2003. [Google Scholar]
- Sen, A. Human rights and capabilities. J. Hum. Dev. 2005, 6, 151–166. [Google Scholar] [CrossRef]
- Nussbaum, M.C. Women’s capabilities and social justice. J. Hum. Dev. 2000, 1, 219–247. [Google Scholar] [CrossRef]
- Yousefzadeh, S.; Biggeri, M.; Arciprete, C.; Haisma, H. A capability approach to child growth. Child Indic. Res. 2019, 12, 711–731. [Google Scholar] [CrossRef] [Green Version]
- Haisma, H.; Yousefzadeh, S.; van Hensbroek, P.B. Towards a capability approach to child growth: A theoretical framework. Matern. Child Nutr. 2018, 14, e12534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Statistic and Information Division (SID), Bangladesh Bureau of Statistics (BBS), Ministry of Planning. Bangladesh Statistics 2017; Bangladesh Bureau of Statistics (BBS), Ministry of Planning, Government of the People’s Republic of Bangladesh: Dhaka, Bangladesh, 2018. Available online: http://bbs.portal.gov.bd/sites/default/files/files/bbs.portal.gov.bd/page/a1d32f13_8553_44f1_92e6_8ff80a4ff82e/Bangladesh%20%20Statistics-2017 (accessed on 27 July 2020).
- Statistic and Information Division (SID), Bangladesh Bureau of Statistics (BBS), Ministry of Planning. Report on Labour Force Survey 2010; Bangladesh Bureau of Statistics, Government of the People’s Republic of Bangladesh: Dhaka, Bangladesh, 2011. Available online: http://www.mccibd.org/images/uploadimg/statistics/Labour%20Force%20Survey%202010.pdf (accessed on 20 June 2019).
- Bangladesh Haor and Wetland Development Board, Ministry of Water Resources, Government of the People’s Republic of Bangladesh. Master Plan of Haor Area; Main Report, Volume II; Bangladesh Haor and Wetland Development Board (BHWDB), Ministry of Water Resources (MWR), Government Republic of Bangladesh (GoB): Dhaka, Bangladesh; Centre for Environmental and Geographic Information Services: Dhaka, Bangladesh, 2012. Available online: https://dbhwd.portal.gov.bd/sites/default/files/files/dbhwd.portal.gov.bd/publications/298d5166_988c_4589_96cb_36e143deba4f/Haor%20Master%20Plan%20Volume%202.pdf (accessed on 27 July 2020).
- Haque, M.R.; Dash, S.K.; Chowdhury, M.A.B. Maternal health care seeking behavior: The case of Haor (wetland) in Bangladesh. BMC Public Health 2016, 1, 592. [Google Scholar] [CrossRef] [Green Version]
- Rahman, A.E.; Perkins, J.; Islam, S.; Siddique, A.B.; Moinuddin, M.; Anwar, M.R.; Mazumder, T.; Ansar, A.; Rahman, M.M.; Raihana, S.; et al. Knowledge and involvement of husbands in maternal and newborn health in rural Bangladesh. BMC Pregnancy Childbirth 2018, 18, 247. [Google Scholar] [CrossRef] [Green Version]
- Story, W.T.; Burgard, S.A.; Lori, J.R.; Taleb, F.; Ali, N.A.; Hoque, D.E. Husbands’ involvement in delivery care utilization in rural Bangladesh: A qualitative study. BMC Pregnancy Childbirth 2012, 12, 28. [Google Scholar] [CrossRef] [Green Version]
- Khanam, M.; Jafrin, N. Determinants of maternal care utilization in a rural area of Bangladesh: A case Study of Udaypur Village of Bagerhat District. Glob. J. Int. Res. 2017, 17. [Google Scholar]
- Jammeh, A.; Sundby, J.; Vangen, S. Barriers to emergency obstetric care services in perinatal deaths in rural Gambia: A qualitative in-depth interview study. ISRN Obstet. Gynecol. 2011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewis, S.; Lee, A.; Simkhada, P. The role of husbands in maternal health and safe childbirth in rural Nepal: A qualitative study. BMC Pregnancy Childbirth 2015, 15, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, M.W. ‘Because he loves me’: Husbands’ involvement in maternal health in Guatemala. Cult. Health Sex. 2002, 4, 259–279. [Google Scholar] [CrossRef]
- Chakraborty, B.; Yousefzadeh, S.; Darak, S.; Haisma, H. “We struggle with the earth everyday”: Parents’ perspectives on the capabilities for healthy child growth in haor region of Bangladesh. BMC Public Health 2020, 20, 1–40. [Google Scholar] [CrossRef] [Green Version]
- Mchome, Z.; Bailey, A.; Darak, S.; Haisma, H. “A child may be tall but stunted.” Meanings attached to childhood height in Tanzania. Matern. Child. Nutr. 2019, 15, e12769. [Google Scholar] [CrossRef] [PubMed]
- Sen, A. Development as Freedom; Oxford University Press: Oxford, UK, 2004; p. 394. [Google Scholar]
- Statistics and Informatics Division, Bangaldesh Bureau of Statistics, Ministry of Planning. Population and Housing Census—2011; Bangladesh Bureau of Statistics (BBS), Ministry of Planning, Government of the People’s Republic of Bangladesh: Dhaka, Bangladesh, 2014. Available online: http://203.112.218.65:8008/WebTestApplication/userfiles/Image/National%20Reports/Union%20Statistics.pdf (accessed on 27 July 2020).
- Hennink, M.; Hutter, I.; Bailey, A. Qualittaive Research Methods; Sage Publications Ltd.: London, UK, 2011. [Google Scholar]
- Biggeri, M.; Libanora, R.; Mariani, S.; Menchini, L. Children conceptualizing their capabilities: Results of a survey conducted during the first children’s world congress on child labour. J. Hum. Dev. 2006, 7, 59–83. [Google Scholar] [CrossRef]
- Biggeri, M.; Mehrotra, S. Child poverty. In Children and the Capability Approach; Biggeri, M., Ballet, J., Commi, F., Eds.; Palgrave Macmillan: London, UK, 2011; pp. 46–75. [Google Scholar]
- Millionnaya, Z. Mother and Baby Clip arts, Stock Vector and Royalty Free Mother and Baby Illustrations. Available online: https://www.123rf.com/photo_37616422_stock-vector-mother-and-baby-stylized-vector-symbol.html. (accessed on 28 July 2020).
- FAVPNG.com. Drawing Father Son Child. Available online: https://favpng.com/png_view/child-drawing-father-son-child-png/SCKp8t6N (accessed on 28 July 2020).
- Chiappero-Martinetti, E.; Venkatapuram, S. The capability approach: A framework for population studies. Afr. Popul. Stud. 2014, 28, 708–720. [Google Scholar] [CrossRef]
- Human Resource Management Unit, Ministry of Health and Family Welfare, Bangladesh Secreteriat. Data Sheet 2014; Human Resource Management Unit, Ministry of Health and Family Welfare, Bangladesh Secreteriat: Dhaka, Bangladesh, 2015.
- Chandrasiri, J.; Anuranga, C.; Wickramasinghe, R.; RannanEliya, R.P. The Impact of Out-of-Pocket Expenditures on Poverty and Inequalities in Use of Maternal and Child Health Services in Bangladesh: Evidence from the Household Income and Expenditure Surveys 2000–2010 RETA–6515 Country Brief; Asian Development Bank: Manila, Philippines, 2012. Available online: https://www.adb.org/sites/default/files/publication/30152/impact-out-pocket-spending-bangladesh.pdf (accessed on 27 July 2020).
- World Health Organization; Ministry of Health and Family Welfare of Bangladesh. Success Factors for Women’s and Children’s Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Asm, A.; Hossain, M.; Rahman, F.; Halima, A.; Biswas, A. Community Delay in Decision Making and Transferring Complicated Mothers at Facilities Caused Maternal Deaths: A Qualitative Study in Rural Bangladesh. Integr. J. Glob. Health 2017, 1, 6. [Google Scholar]
- Moinuddin, M.; Christou, A.; Hoque, D.M.E.; Tahsina, T.; Salam, S.S.; Billah, S.M.; Kuppens, L.; Matin, M.Z.; Arifeen, S.E. Birth preparedness and complication readiness (BPCR) among pregnant women in hard-to-reach areas in Bangladesh. PLoS ONE 2017, 12, e0189365. [Google Scholar] [CrossRef]
- Gudeta, T.A.; Regassa, T.M. Factors Associated with birth preparedness and complication readiness among pregnant women in Bench Maji zone, Southwest Ethiopia: A community-based cross-sectional study. Ethiop. J. Health Sci. 2019, 29, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, R. Effect of women’s autonomy on maternal health service utilization in Nepal: A cross sectional study. BMC Womens Health 2016, 16, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, S.; Creanga, A.A.; Gillespie, D.G.; Tsui, A.O. Economic status, education and empowerment: Implications for maternal health service utilization in developing countries. PLoS ONE 2010, e11190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chakraborty, N.; Islam, M.A.; Chowdhury, R.I.; Bari, W.; Akhter, H.H. Determinants of the use of maternal health services in rural Bangladesh. Health Promot. Int. 2003, 18, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Fawole, O.I.; Adeoye, I.A. Women’s status within the household as a determinant of maternal health care use in Nigeria. Afr. Health Sci. 2015, 15, 217–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]


© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chakraborty, B.; Darak, S.; Haisma, H. Maternal and Child Survival in Haor Region in Bangladesh. An Analysis of Fathers’ Capabilities to Save the Future. Int. J. Environ. Res. Public Health 2020, 17, 5781. https://doi.org/10.3390/ijerph17165781
Chakraborty B, Darak S, Haisma H. Maternal and Child Survival in Haor Region in Bangladesh. An Analysis of Fathers’ Capabilities to Save the Future. International Journal of Environmental Research and Public Health. 2020; 17(16):5781. https://doi.org/10.3390/ijerph17165781
Chicago/Turabian StyleChakraborty, Barnali, Shrinivas Darak, and Hinke Haisma. 2020. "Maternal and Child Survival in Haor Region in Bangladesh. An Analysis of Fathers’ Capabilities to Save the Future" International Journal of Environmental Research and Public Health 17, no. 16: 5781. https://doi.org/10.3390/ijerph17165781
APA StyleChakraborty, B., Darak, S., & Haisma, H. (2020). Maternal and Child Survival in Haor Region in Bangladesh. An Analysis of Fathers’ Capabilities to Save the Future. International Journal of Environmental Research and Public Health, 17(16), 5781. https://doi.org/10.3390/ijerph17165781



