Nutritional Status Measurement Instruments for Diabetes: A Systematic Psychometric Review
Abstract
1. Introduction
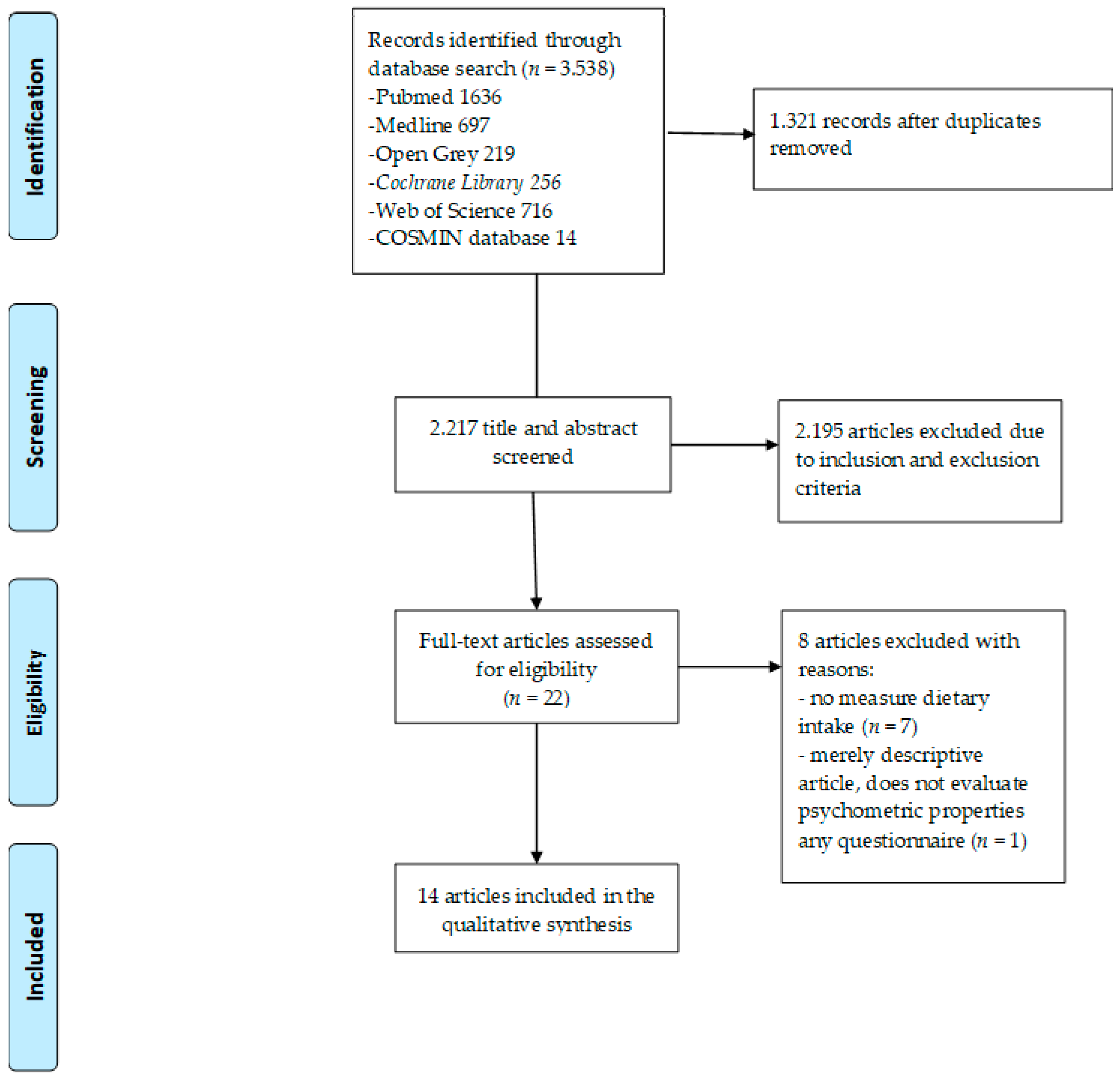
2. Materials and Methods
2.1. Design
2.2. Databases and Search Strategy
2.3. Inclusion/Exclusion Criteria
2.4. Assessment of Methodological Quality
2.5. Data Extraction
2.6. Synthesis of Data
3. Results
3.1. Psychometric Properties
3.1.1. Diabetes Knowledge and Behaviour Questionnaire (DKB)
3.1.2. Food Frequency Questionnaire (FFQ)
3.1.3. Perceived Dietary Adherence Questionnaire (PDAQ)
3.1.4. UK Diabetes and Diet Questionnaire (UKDDQ)
3.1.5. Self-Developed Dietary Knowledge Questionnaire (DKQ)
3.1.6. Diabetes Mellitus Knowledge Questionnaire (DMK)
3.1.7. Motiv.Diaf-DM2 Questionnaire (MDDM2)
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Castro-Rodríguez, M.; Carnicero, J.A.; García-García, F.J.; Walter, S.; E Morley, J.; Rodríguez-Artalejo, F.; Sinclair, A.; Rodriguez-Manas, L. Frailty as a Major Factor in the Increased Risk of Death and Disability in Older People With Diabetes. J. Am. Med. Dir. Assoc. 2016, 17, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, P.; Salpea, P.; Karuranga, S.; Petersohn, I.; Malanda, B.; Gregg, E.W.; Unwin, N.; Wild, S.H.; Williams, R. Mortality attributable to diabetes in 20–79 years old adults, 2019 estimates: Results from the International Diabetes Federation Diabetes Atlas, 9th ed. Diabetes Res. Clin. Pr. 2020, 162. [Google Scholar] [CrossRef]
- Sun, Y.; You, W.; Almeida, F.A.; Estabrooks, P.A.; Davy, B.M. The Effectiveness and Cost of Lifestyle Interventions Including Nutrition Education for Diabetes Prevention: A Systematic Review and Meta-Analysis. J. Acad. Nutr. Diet. 2017, 117, 404–421. [Google Scholar] [CrossRef] [PubMed]
- Wylie-Rosett, J.; Herman, W.H.; Goldberg, R.B. Lifestyle intervention to prevent diabetes: intensive AND cost effective. Curr. Opin. Lipidol. 2006, 17, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Patel, Y.R.; Gadiraju, T.V.; Gaziano, J.M.; Djoussé, L. Adherence to healthy lifestyle factors and risk of death in men with diabetes mellitus: The Physicians’ Health Study. Clin. Nutr. 2018, 37, 139–143. [Google Scholar] [CrossRef]
- Williams, J.L.S.; Walker, R.J.; Smalls, B.L.; A Campbell, J.; Egede, L.E. Effective interventions to improve medication adherence in Type 2 diabetes: a systematic review. Diabetes Manag. 2014, 4, 29–48. [Google Scholar] [CrossRef]
- Vasilevskis, E.E. The Challenges of Diabetes Medication Management at Hospital Discharge in Older Adults. JAMA Netw. Open 2020, 3, e201500. [Google Scholar] [CrossRef]
- Deng, A.; Pattanaik, S.; Bhattacharya, A.; Yin, J.; Ross, L.; Liu, C.; Zhang, J. Fish consumption is associated with a decreased risk of death among adults with diabetes: 18-year follow-up of a national cohort. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 1012–1020. [Google Scholar] [CrossRef]
- Bonaccio, M.; Di Castelnuovo, A.; Costanzo, S.; Persichillo, M.; De Curtis, A.; Donati, M.; De Gaetano, G.; Iacoviello, L.; on Behalf of the MOLI-SANI Study Investigators. Adherence to the traditional Mediterranean diet and mortality in subjects with diabetes. Prospective results from the MOLI-SANI study. Eur. J. Prev. Cardiol. 2015, 23, 400–407. [Google Scholar] [CrossRef]
- Jalilian, H.; Pezeshki, M.Z.; Janati, A.; Najafipour, F.; Sarbakhsh, P.; Zarnaq, R.K.; Zarnagh, R.K. Readiness for weight change and its association with diet knowledge and skills, diet decision making and diet and exercise barriers in patients with type 2 diabetes. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2889–2895. [Google Scholar] [CrossRef]
- Sami, W.; Alabdulwahhab, K.M.; Ab Hamid, M.R.; Alasbali, T.A.; Al Alwadani, F.; Ahmad, M.S. Dietary Knowledge among Adults with Type 2 Diabetes—Kingdom of Saudi Arabia. Int. J. Environ. Res. Public Health 2020, 17, 858. [Google Scholar] [CrossRef] [PubMed]
- García-Molina, L.; Lewis-Mikhael, A.-M.; Riquelme-Gallego, B.; Cano-Ibañez, N.; Oliveras-López, M.J.; Bueno-Cavanillas, A. Improving type 2 diabetes mellitus glycaemic control through lifestyle modification implementing diet intervention: a systematic review and meta-analysis. Eur. J. Nutr. 2019, 59, 1313–1328. [Google Scholar] [CrossRef] [PubMed]
- Mozaffari, H.; Daneshzad, E.; Azadbakht, L. Dietary carbohydrate intake and risk of bone fracture: a systematic review and meta-analysis of observational studies. Public Health 2020, 181, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Monforte, M.; Flores-Mateo, G.; Barrio, F.; Costa, B.; Sánchez, E. Metabolic syndrome and dietary patterns: a systematic review and meta-analysis of observational studies—reply. Eur. J. Nutr. 2019, 58, 3383–3386. [Google Scholar] [CrossRef]
- Knüppel, S.; Norman, K.; Boeing, H. Is a Single 24-hour Dietary Recall per Person Sufficient to Estimate the Population Distribution of Usual Dietary Intake? J. Nutr. 2019, 149, 1491–1492. [Google Scholar] [CrossRef]
- Freedman, L.S.; Midthune, D.; Arab, L.; Prentice, R.L.; Subar, A.F.; Willett, W.; Neuhouser, M.L.; Tinker, L.F.; Kipnis, V. Combining a Food Frequency Questionnaire With 24-Hour Recalls to Increase the Precision of Estimation of Usual Dietary Intakes—Evidence From the Validation Studies Pooling Project. Am. J. Epidemiol. 2018, 187, 2227–2232. [Google Scholar] [CrossRef]
- Delichatsios, H.K.; Hunt, M.K.; Lobb, R.; Emmons, K.; Gillman, M.W. EatSmart: Efficacy of a multifaceted preventive nutrition intervention in clinical practice. Prev. Med. 2001, 33, 91–98. [Google Scholar] [CrossRef]
- Patton, S.R.; Dolan, L.M.; Powers, S.W. Parent Report of Mealtime Behaviors in Young Children with Type 1 Diabetes Mellitus: Implications for better assessment of dietary adherence problems in the clinic. J. Dev. Behav. Pediatr. 2006, 27, 202–208. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; De Vet, H.C. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual. Life Res. 2010, 19, 539–549. [Google Scholar] [CrossRef]
- Terwee, C.B.; Mokkink, L.B.; Knol, D.L.; Ostelo, R.W.J.G.; Bouter, L.M.; De Vet, H.C.W. Rating the methodological quality in systematic reviews of studies on measurement properties: A scoring system for the COSMIN checklist. Qual. Life Res. 2011, 21, 651–657. [Google Scholar] [CrossRef]
- Prinsen, C.; Mokkink, L.B.; Bouter, L.M.; Alonso, J.; Patrick, D.L.; De Vet, H.C.; Terwee, C.B. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual. Life Res. 2018, 27, 1147–1157. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.; Oxman, A.D.; E Vist, G.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed]
- Han, C.Y.; Zheng, X.; Lee, L.F.; Chan, C.G.; Lee, Y.Q.; Zailani, N.A.; Ng, K.; Bhaskaran, K. Development of a diabetes-related nutrition knowledge questionnaire for individuals with type 2 diabetes mellitus in Singapore. Nutr. Diet. 2019, 76, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Quick, V.; Lipsky, L.M.; Nansel, T.R. Psychometric properties and factor structure of the adapted Self-Regulation Questionnaire assessing autonomous and controlled motivation for healthful eating among youth with type 1 diabetes and their parents. Child: Care, Health Dev. 2018, 44, 651–658. [Google Scholar] [CrossRef]
- Samuel-Hodge, C.; DeVellis, R.F.; Ammerman, A.; Keyserling, T.C.; Elasy, T.A. Reliability and Validity of a Measure of Perceived Diabetes and Dietary Competence in African American Women With Type 2 Diabetes. Diabetes Educ. 2002, 28, 979–988. [Google Scholar] [CrossRef]
- Eslami, A.A.; Rohani, H.; Ghaderi, A.; Bidkhori, M.; Raei, M. Development and psychometric evaluation of a health action process approach inventory for healthful diet among Type 2 diabetes patients. Int. J. Prev. Med. 2016, 7, 69. [Google Scholar] [CrossRef]
- Anastasiou, C.A.; Feel4Diabetes-Study Group; Fappa, E.; Zachari, K.; Mavrogianni, C.; Van Stappen, V.; Kivelä, J.; Virtanen, E.; González-Gil, E.M.; Flores-Barrantes, P.; et al. Development and reliability of questionnaires for the assessment of diet and physical activity behaviors in a multi-country sample in Europe the Feel4Diabetes Study. BMC Endocr. Disord. 2020, 20, 1–7. [Google Scholar] [CrossRef]
- Brito-Brito, P.R.; Martín-García, Á.; Quintana, C.O.; Paloma-Castro, O.; Romero-Sánchez, J.M. Development and Content Validation of a NOC-Based Instrument for Measuring Dietary Knowledge in Patients with Diabetes: CoNOCidiet-Diabetes. Int. J. Nurs. Knowl. 2019, 31, 59–73. [Google Scholar] [CrossRef]
- Stetson, B.A.; Schlundt, D.; Rothschild, C.; Floyd, J.E.; Rogers, W.; Mokshagundam, S.P. Development and validation of The Personal Diabetes Questionnaire (PDQ): A measure of diabetes self-care behaviors, perceptions and barriers. Diabetes Res. Clin. Pr. 2011, 91, 321–332. [Google Scholar] [CrossRef]
- Simmons, D.; Mandell, C.; Fleming, C.; Gatland, B.; Leakehe, L. Evaluation of a diabetes knowledge and behaviour (DKB) questionnaire. Asia Pac. J. Clin. Nutr. 1994, 3, 193–200. [Google Scholar]
- Huang, M.-C.; Lin, K.-D.; Chen, H.-J.; Wu, Y.-J.; Chang, C.-I.; Shin, S.-J.; Hung, H.-C.; Lee, C.-H.; Huang, Y.-F.; Hsu, C.-C. Validity of a Short Food Frequency Questionnaire Assessing Macronutrient and Fiber Intakes in Patients of Han Chinese Descent with Type 2 Diabetes. Int. J. Environ. Res. Public Health 2018, 15, 1142. [Google Scholar] [CrossRef] [PubMed]
- Sarmento, R.A.; Antonio, J.P.; Riboldi, B.P.; Montenegro, K.R.; Friedman, R.; De Azevedo, M.J.; De Almeida, J.C. Reproducibility and validity of a quantitative FFQ designed for patients with type 2 diabetes mellitus from southern Brazil. Public Health Nutr. 2013, 17, 2237–2245. [Google Scholar] [CrossRef] [PubMed]
- Coulibaly, A.; O’Brien, H.T.; Galibois, I. Validation of an FFQ to assess dietary protein intake in type 2 diabetic subjects attending primary health-care services in Mali. Public Health Nutr. 2009, 12, 644–650. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Farukuoye, M.; Strassburger, K.; Kacerovsky-Bielesz, G.; Giani, G.; Roden, M. Validity and reproducibility of an interviewer-administered food frequency questionnaire in Austrian adults at risk of or with overt diabetes mellitus. Nutr. Res. 2014, 34, 410–419. [Google Scholar] [CrossRef]
- Hong, S.; Choi, Y.; Lee, H.-J.; Kim, S.H.; Oe, Y.; Lee, S.Y.; Nam, M.; Kim, Y.S. Development and Validation of a Semi-Quantitative Food Frequency Questionnaire to Assess Diets of Korean Type 2 Diabetic Patients. Korean Diabetes J. 2010, 34, 32–39. [Google Scholar] [CrossRef]
- Liese, A.D.; Crandell, J.L.; Tooze, J.A.; Fangman, M.T.; Couch, S.C.; Merchant, A.T.; Bell, R.A.; Mayer-Davis, E.J. Relative validity and reliability of an FFQ in youth with type 1 diabetes. Public Health Nutr. 2014, 18, 428–437. [Google Scholar] [CrossRef]
- Luévano-Contreras, C.; Durkin, T.; Pauls, M.; Chapman-Novakofski, K. Development, relative validity, and reliability of a food frequency questionnaire for a case-control study on dietary advanced glycation end products and diabetes complications. Int. J. Food Sci. Nutr. 2013, 64, 1030–1035. [Google Scholar] [CrossRef]
- Petersen, K.S.; Smith, J.M.; Clifton, P.M.; Keogh, J.B. Dietary intake in adults with type 1 and type 2 diabetes: validation of the Dietary Questionnaire for Epidemiological Studies version 2 FFQ against a 3-d weighed food record and 24-h urinalysis. Br. J. Nutr. 2015, 114, 2056–2063. [Google Scholar] [CrossRef]
- Riley, M.D.; Blizzard, L. Comparative Validity of a Food Frequency Questionnaire for Adults with IDDM. Diabetes Care 1995, 18, 1249–1254. [Google Scholar] [CrossRef]
- Sami, W.; Ansari, T.; Butt, N.S.; Ab Hamid, M.R. Psychometric evaluation of dietary habits questionnaire for type 2 diabetes mellitus. J. Physics: Conf. Ser. 2017, 890, 12151. [Google Scholar] [CrossRef]
- Asaad, G.; Sadegian, M.; Lau, R.; Xu, Y.; Soria-Contreras, D.C.; Bell, R.; Chan, C.B. The Reliability and Validity of the Perceived Dietary Adherence Questionnaire for People with Type 2 Diabetes. Nutrition 2015, 7, 5484–5496. [Google Scholar] [CrossRef] [PubMed]
- England, C.Y.; Thompson, J.L.; Jago, R.; Cooper, A.; Andrews, R. Development of a brief, reliable and valid diet assessment tool for impaired glucose tolerance and diabetes: the UK Diabetes and Diet Questionnaire. Public Health Nutr. 2016, 20, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Payo, R.M.; Méndez, X.G.; Cano, C.P.; Álvarez, J.S. Development and validation of a questionnaire for assessing the characteristics of diet and physical activity in patients with type 2 diabetes. Psicothema 2018, 30, 116–122. [Google Scholar]
- Donini, L.M.; Savina, C.; Rosano, A.; Cannella, C. Systematic review of nutritional status evaluation and screening tools in the elderly. J. Nutr. Health Aging 2007, 11, 421. [Google Scholar] [PubMed]
- Bell, L.K.; Golley, R.K.; Magarey, A. Short Tools to Assess Young Children’s Dietary Intake: A Systematic Review Focusing on Application to Dietary Index Research. J. Obes. 2013, 2013, 1–17. [Google Scholar] [CrossRef]
| 1 (“Diabetes mellitus” [MeSH] OR “diabetes” [All Fields]) |
| 2 (“nutritional status”[MeSH] OR “nutrition”[All Fields] OR “nutrition status”[All Fields] OR “eating” [MeSH] OR “food intake” [All Fields] OR “food frequency” [All Fields]) |
| 3 (“Instrument”[tiab] OR “instruments”[tiab] OR “measure” [tiab] OR “measures” [tiab] OR “questionnaire”[tiab] OR “questionnaires”[tiab] OR “scale”[tiab] OR “scales”[tiab] OR “tool”[tiab] OR “tools”[tiab] OR “survey” [tiab] OR “test” [tiab]) |
| 4 (“Instrumentation”[sh] OR “methods”[sh] OR “Validation Studies”[pt] OR “Comparative Study”[pt] OR “psychometrics”[MeSH] OR psychometr*[tiab] OR clinimetr*[tw] OR clinometr*[tw] OR “outcome assessment (health care)”[MeSH] OR “outcome assessment”[tiab] OR “outcome measure*”[tw] OR “observer variation”[MeSH] OR “observer variation”[tiab] OR “Health Status Indicators”[Mesh] OR “reproducibility of results”[MeSH] OR “reproducib*”[tiab] OR “discriminant analysis”[MeSH] OR “reliab*”[tiab] OR “unreliab*”[tiab] OR “valid*”[tiab] OR “coefficient”[tiab] OR “homogeneity”[tiab] OR “homogeneous”[tiab] OR ““internal consistency””[tiab] OR (“cronbach*”[tiab] AND (“alpha”[tiab] OR “alphas”[tiab])) OR (item[tiab] AND (correlation*[tiab] OR selection*[tiab] OR reduction*[tiab])) OR “agreement”[tiab] OR “precision”[tiab] OR “imprecision”[tiab] OR “precise values”[tiab] OR “test-retest”[tiab] OR(“test”[tiab] AND “retest”[tiab]) OR(“reliab*” [tiab] AND (“test”[tiab] OR “retest”[tiab])) OR“stability”[tiab] OR “interrater”[tiab] OR “inter-rater”[tiab] OR “intrarater”[tiab] OR “intra-rater”[tiab] OR “intertester”[tiab] OR “inter-tester”[tiab] OR “intratester”[tiab] OR “intra-tester”[tiab] OR “interobserver”[tiab] OR “inter-observer”[tiab] OR “intraobserver”[tiab] OR “intraobserver”[tiab] OR “intertechnician”[tiab] OR “inter-technician”[tiab] OR “intratechnician”[tiab] OR “intra-technician”[tiab] OR “interexaminer”[tiab] OR “inter-examiner”[tiab] OR “intraexaminer”[tiab] OR “intra-examiner”[tiab] OR “interassay”[tiab] OR “inter-assay”[tiab] OR “intraassay”[tiab] OR “intra-assay”[tiab] OR “interindividual”[tiab] OR “inter-individual”[tiab] OR “intraindividual”[tiab] OR “intra-individual”[tiab] OR “interparticipant”[tiab] OR “inter-participant”[tiab] OR “intraparticipant”[tiab] OR “intra-participant”[tiab] OR “kappa”[tiab] OR “kappa’s”[tiab] OR “kappas”[tiab] OR “repeatab*”[tiab] OR ((“replicab*”[tiab] OR “repeated”[tiab]) AND (“measure”[tiab] OR “measures”[tiab] OR “findings”[tiab] OR “result”[tiab] OR “results”[tiab] OR “test”[tiab] OR “tests”[tiab])) OR “generaliza*”[tiab] OR “generalisa*”[tiab] OR “concordance”[tiab] OR (“intraclass”[tiab] AND “correlation*”[tiab]) OR “discriminative”[tiab] OR “known group”[tiab] OR “factor analysis”[tiab] OR “factor analyses”[tiab] OR “dimension*”[tiab] OR “subscale*”[tiab] OR (“multitrait”[tiab] AND “scaling”[tiab] AND (“analysis”[tiab] OR “analyses”[tiab])) OR “item discriminant”[tiab] OR “interscale correlation*”[tiab] OR error[tiab] OR errors[tiab] OR “individual variability”[tiab] OR (“variability”[tiab] AND (“analysis”[tiab] OR “values”[tiab])) OR (“uncertainty”[tiab] AND (“measurement”[tiab] OR “measuring”[tiab])) OR “standard error of measurement”[tiab] OR “sensitiv*”[tiab] OR “responsive*”[tiab] OR ((“minimal”[tiab] OR “minimally”[tiab] OR “clinical”[tiab] OR “clinically”[tiab]) AND (“important”[tiab] OR “significant”[tiab] OR “detectable”[tiab]) AND (“change”[tiab] OR “difference”[tiab])) OR (“small*”[tiab] AND (“real”[tiab] OR “detectable”[tiab]) AND (“change”[tiab] OR “difference”[tiab])) OR “meaningful change” [tiab] OR “ceiling effect”[tiab] OR “floor effect”[tiab] OR “Item response model”[tiab] OR “IRT”[tiab] OR “Rasch”[tiab] OR “Differential item functioning”[tiab] OR DIF[tiab] OR “computer adaptive testing”[tiab] OR “item bank”[tiab] OR “cross-cultural equivalence”[tiab]) |
| 5 #1 AND #2 AND #3 AND #4 |
| 6 “Protocol”[Publication Type] OR “addresses”[Publication Type] OR “biography”[Publication Type] OR “case reports”[Publication Type] OR “comment”[Publication Type] OR “editorial”[Publication Type] OR “congresses” [Publication Type] OR “consensus development conference”[Publication Type] OR “consensus development conference”[Publication Type] OR “practice guideline”[Publication Type]) OR “suffering from”[tiab] OR “animals”[MeSH] |
| 7 #5 NOT #6 |
| 8 FILTER: Language (English and Spanish) |
| 9 FILTER: Species (Humans) |
| Study (Author and Year) | Population/Type of Mellitus Diabetes | Setting | Instrument Description | Measurement Properties | COSMIN Score | Measurement Values |
|---|---|---|---|---|---|---|
| Diabetes Knowledge and Behaviour Questionnaire (DKB) | ||||||
| Simmons et al., (1994) | 397 adults with type 2 diabetes | New Zealand: Patients were recruited from the community | DKB includes five open-ended questions, a four-point and five-point Likert scale, and 47 closed questions. The questions are grouped into 10 stems with 3–6 true/false answers. For its definitive application, the incorrect answer is assigned a negative score of −1, the correct answer is a score of +1 and “does not know” is scored with 0. | 1-Internal consistency 2-Hypotheses testing 3-Responsiveness | 1-Inadequate 2-Doubtful 3-Doubtful | α: 0.59–0.90 #total calories (r = 0.48–0.64) # calories due to fat (r = 0.41–0.65) Negative correlations with the frequency of fruit consumption (r = (−0.25)–(−0.33)) |
| Food Frequency Questionnaire (FFQ) | ||||||
| Riley et al., (1995) | 84 patients with type 1 diabetes | Australia: Patients were randomly selected from a population-based insulin-treated diabetes register. | The questionnaire typically includes questions on 80 to 120 food and beverage items. In this article, the final version of the FFQ consists of 153 food items. | 1-Criterion validity 2-Responsiveness | 1-Inadequate 2-Inadequate | # 2-day weighed dietary (r = 0.38–0.60) # true usual dietary intake (r = 0.60) |
| Coulibaly et al., (2008) | 57 patients with type 2 diabetes | Mali: Primary health-care services. | In this article, the final version of the FFQ consists of 53 food items. | 1-Content validity 2-Hypotheses testing 3-Responsiveness | 1-Inadequate 2- Inadequate 3-Doubtful | # 48 h recall (r = 0.63) |
| Hong et al., (2010) | 85 patients with type 2 diabetes | Korea: Patients were recruited from Korean National Diabetes Program (KNDP) | In this article, the final version of the FFQ consists of 85 food items. | 1-Criterion validity 2-Responsiveness | 1-Inadequate 2-Inadequate |
# energy (r = 0.74) # iron (r = 0.27) The Kappa values for energy, carbohydrate, protein, fat and calcium were 0.54, 0.37, 0.36, 0.46, and 0.19, respectively |
| Aguiar et al., (2013) | 88 patients with type 2 diabetes | South of Brazil: Hospital de Clínicas de Porto Alegre. Out-patients | In this article, the final version of the FFQ consists of 98 food items. | 1-Criterion validity 2-Responsiveness | 1-Inadequate 2-Doubtful | # WDR for most nutrients |
| Luevano-Contreras et al., (2013) | 30 patients with type 2 diabetes | USA: University of Illinois | In this article, the final version of the FFQ consists of 90 food items. | 1-Reliability 2-Criterion validity 3-Responsiveness | 1-Inadequate 2-Inadequate 3-Inadequate | ICC = 0.98 # FR time 1 (r = 0.68) # FR time 2 (r = 0.80) |
| Farukuoye et al., (2014) | 27 nondiabetic relatives of patients with DM2, 66 patients with diabetes (32 patients with DM2 and 34 with DM1 diabetes) and 30 nondiabetic healthy individuals | Vienna: Diabetes Outpatient Service of the 1st Medical Department of Hanusch Hospital, Teaching Hospital of Medical University of Vienna, and from a local Physiotherapy Service. | In this article, the final version of the FFQ consists of 107 food items. | 1-Criterion validity2-Responsiveness | 1-Inadequate 2-Inadequate | # 7DR (r = 0.23–0.72) |
| Liese et al., (2014) | 172 patients with type 1 diabetes | USA: University of North Carolina Nutrition Obesity Research Center. | In this article, the final version of the FFQ consists of 85 food items. | 1-Reliability 2-Hypotheses testing 3-Responsiveness | 1-Inadequate 2-Doubtful 3-Doubtful | ICC both FFQ,(r = 0.24–0.71) # between the items of FFQ (r = 0.38–0.41) |
| Petersen et al., (2015) | 67 patients with type 1 and 2 diabetes | Australia. Patients were recruited from the community | In this article, the final version of the FFQ consists of 74 food items. | 1-Criterion validity 2-Responsiveness | 1-Inadequate 2-Inadequate | # WFR # Food intake |
| Sami et al., (2017) | 132 patients with type 2 diabetes | Saudi Arabia | In this article, the final version of the FFQ consists of 99 food items. | 1-Content Validity 2-Structural Validity 3-Internal Consistency 4-Hypotheses testing 5-Responsiveness | 1-Doubtful 2-Doubtful 3-Doubtful 4-Inadequate 5-Inadequate | EFA resulted in five-factor solution with eigenvalues greater than 1. α = 0.782–0.908 # 24-HDRs (r = 0.58–0.66) |
| Meng-Chuan et al., (2018) | 126 patients with type 2 diabetes | Taiwan: Kaohsiung Medical University Hospital | In this article, the final version of the FFQ consists of 45 food items. | 1-Criterion validity 2-Responsiveness | 1-Inadequate 2-Inadequate | # protein (r = 0.65) #fat (r = 0.58) #carbohydrate (r = 0.64) #fiber (r = 0.66) |
| Perceived Dietary Adherence Questionnaire (PDAQ) | ||||||
| Asaad et al., (2015) | 73 patients with type 2 diabetes | Canada: Patients were recruited from the community | Nine-item questionnaires with scores ranging from lowest 0 to highest 7 based on a seven-point Likert scale. Higher scores reflect higher adherence except for items 4 and 9, which reflect unhealthy choices (foods high in sugar or fat). | 1-Content validity 2-Internal consistency 3-Reliability 4-Hypotheses testing 5-Responsiveness | 1-Doubtful 2-Inadequate 3-Inadequate 4-Doubtful 5-Doubtful | α = 0.78 ICC = 0.78 # 24-HDR (r = 0.11–0.46) |
| UK Diabetes and Diet Questionnaire (UKDDQ) | ||||||
| England et al., (2016) | 177 patients with type 2 diabetes | United Kingdom (Southwest England): Patients were recruited into STAMP-2: Sedentary time and metabolic health in people with (or at risk of) type 2 diabetes | The UK Diabetes and Diet Questionnaire (UKDDQ) consists of 25 items; of those 25 items, 20 contribute to the overall score. Each of the 20 items has six categories for the participant to choose from, which corresponds to the frequency of consumption of the participant for that particular item, the score for each item ranges from 0–5 (with 0 being healthier and 5 less healthy). | 1-Content validity 2-Reliability 3-Hypotheses testing4-Responsiveness | 1-Inadequate 2-Doubtful 3-Doubtful 4-Inadequate | ICC = 0.90 Total scores from the UKDDQ and food diaries compared well ICC = 0.54. |
| The self-developed Dietary Knowledge Questionnaire (DKQ/DK) | ||||||
| Sami et al., (2017) | 132 patients with type 2 diabetes | Saudi Arabia | The self-prepared dietary knowledge questionnaire (DKQ) used in this research consists of 20 multiple-choice questions (MCQ). The answers are coded as 1 = correct and 0 = incorrect, and I don’t know. The score ranges from 0 to 20; a higher DK level is indicated by a higher score. | 1-Content Validity 2-Structural Validity 3-Internal Consistency 4-Hypotheses testing 5-Responsiveness | 1-Doubtful 2-Doubtful 3-Doubtful 4-Inadequate 5- Inadequate | EFA resulted in five-factor solution with eigenvalues greater than 1 α = 0.869 # between items (r = 0.364–0.588) |
| Diabetes Mellitus Knowledge Questionnaire (DMK) | ||||||
| Sami et al., (2017) | 132 patients with type 2 diabetes | Saudi Arabia | The new version of DMK questionnaire used in this research comprised 30 questions. Responses are coded as 1 = yes and 0 = no, and I don’t know. | 1-Content Validity 2-Structural Validity 3-Internal Consistency 4-Hypotheses testing 5-Responsiveness | 1-Doubtful 2-Doubtful 3-Doubtful 4-Inadequate 5-Inadequate | EFA resulted in five-factor solution with eigenvalues greater than 1 α = 0.891 # between items (r = 0.358–0.529) |
| Motiv.Diaf-DM2 Questionnaire (MDDM2) | ||||||
| Martín Payo et al., (2018) | 206 patients with type 2 diabetes | Spain: Primary care services | Motivate. Diaf-DM2 is made up of three blocks including sociodemographic variables, type of motivation of the patients performing physical activity and resilience. This questionnaire consists of four items in Likert format on a scale of 1 (It does not describe me at all) to 5 (It describes me very well). | 1-Content validity 2-Structural validity 3-Internal consistency 4-Reliability 5-Hypotheses testing 6-Responsiveness | 1-Inadequate 2-Inadequate 3-Inadequate 4-Inadequate 5-Doubtful 6-Doubtful | EFA resulted in two-dimensional instrument. A = 0.756–0.821 # between factors (r = 0.604–0.638) |
| Instrument | Article | Content Validity | Structural Validity | Internal Consistency | Reliability | Criterion Validity | Hypotheses Testing | Responsiveness | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | Q | M | Q | M | Q | M | Q | M | Q | M | Q | M | Q | ||
| DKB | Simmons et al., (1994) | I | − | D | ? | D | ? | ||||||||
| FFQ | Riley et al., (1995) | I | − | I | + | ||||||||||
| Coulibaly et al., (2008) | I | ? | I | ? | D | ? | |||||||||
| Hong et al., (2010) | I | − | I | + | |||||||||||
| Aguiar et al., (2013) | I | − | D | + | |||||||||||
| Luevano-Contreras et al., (2013) | I | + | I | − | I | + | |||||||||
| Farukuoye et al., (2014) | I | − | I | + | |||||||||||
| Liese et al., (2014) | I | − | D | ? | D | ? | |||||||||
| Petersen et al., (2015) | I | + | I | + | |||||||||||
| Sami et al., (2017) | D | − | D | ? | D | + | I | + | I | + | |||||
| Meng-Chuan et al., (2018) | I | − | I | + | |||||||||||
| PDAQ | Asaad et al., (2015) | D | − | I | + | I | + | D | ? | D | ? | ||||
| UKDDQ | England et al., (2016) | I | + − | D | + | D | ? | I | ? | ||||||
| DKQ/(DK) | Sami et al., (2017) | D | − | D | ? | D | + | I | + | I | + | ||||
| DMK | Sami et al., (2017) | D | − | D | ? | D | + | I | + | I | + | ||||
| MDDM2 | Martín Payo et al., (2018) | I | ? | I | − | I | + | I | − | D | ? | D | ? | ||
| Instrument | Content Validity | Structural Validity | Internal Consistency | Reliability | Criterion Validity | Hypotheses Testing | Responsiveness | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | Q | QE | M | Q | QE | M | Q | QE | M | Q | QE | M | Q | QE | M | Q | QE | M | Q | QE | |
| DKB | I | − | VL | D | ? | L | D | ? | L | ||||||||||||
| FFQ | I | − | VL | D | ? | VL | D | + | L | I | − | VL | I | − | L | I | ? | L | I | ? | L |
| PDAQ | D | − | L | I | + | VL | I | + | VL | D | ? | L | D | ? | L | ||||||
| UKDDQ | I | + − | VL | D | + | L | D | ? | L | I | ? | VL | |||||||||
| DKQ/DK | D | − | L | D | ? | L | D | + | L | I | + | VL | I | + | VL | ||||||
| DMK | D | − | L | D | ? | L | D | + | L | I | + | VL | I | + | VL | ||||||
| MDDM2 | I | ? | VL | I | − | VL | I | + | VL | I | − | VL | D | ? | L | D | ? | L | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montagut-Martínez, P.; Pérez-Cruzado, D.; García-Arenas, J.J. Nutritional Status Measurement Instruments for Diabetes: A Systematic Psychometric Review. Int. J. Environ. Res. Public Health 2020, 17, 5719. https://doi.org/10.3390/ijerph17165719
Montagut-Martínez P, Pérez-Cruzado D, García-Arenas JJ. Nutritional Status Measurement Instruments for Diabetes: A Systematic Psychometric Review. International Journal of Environmental Research and Public Health. 2020; 17(16):5719. https://doi.org/10.3390/ijerph17165719
Chicago/Turabian StyleMontagut-Martínez, Pedro, David Pérez-Cruzado, and José Joaquín García-Arenas. 2020. "Nutritional Status Measurement Instruments for Diabetes: A Systematic Psychometric Review" International Journal of Environmental Research and Public Health 17, no. 16: 5719. https://doi.org/10.3390/ijerph17165719
APA StyleMontagut-Martínez, P., Pérez-Cruzado, D., & García-Arenas, J. J. (2020). Nutritional Status Measurement Instruments for Diabetes: A Systematic Psychometric Review. International Journal of Environmental Research and Public Health, 17(16), 5719. https://doi.org/10.3390/ijerph17165719





