Study Protocol for an Online Questionnaire Survey on Symptoms/Signs, Protective Measures, Level of Awareness and Perception Regarding COVID-19 Outbreak among Dentists. A Global Survey
Abstract
1. Introduction
- What is the prevalence of the symptoms/signs reported by dentists worldwide presumably referable to the COVID-19?
- What is the level of preparedness regarding protective measures and PPE to reduce the risk of viral transmission?
- What is the level of awareness and risk perception of dentists regarding COVID-19?
2. Methods
2.1. Study Design
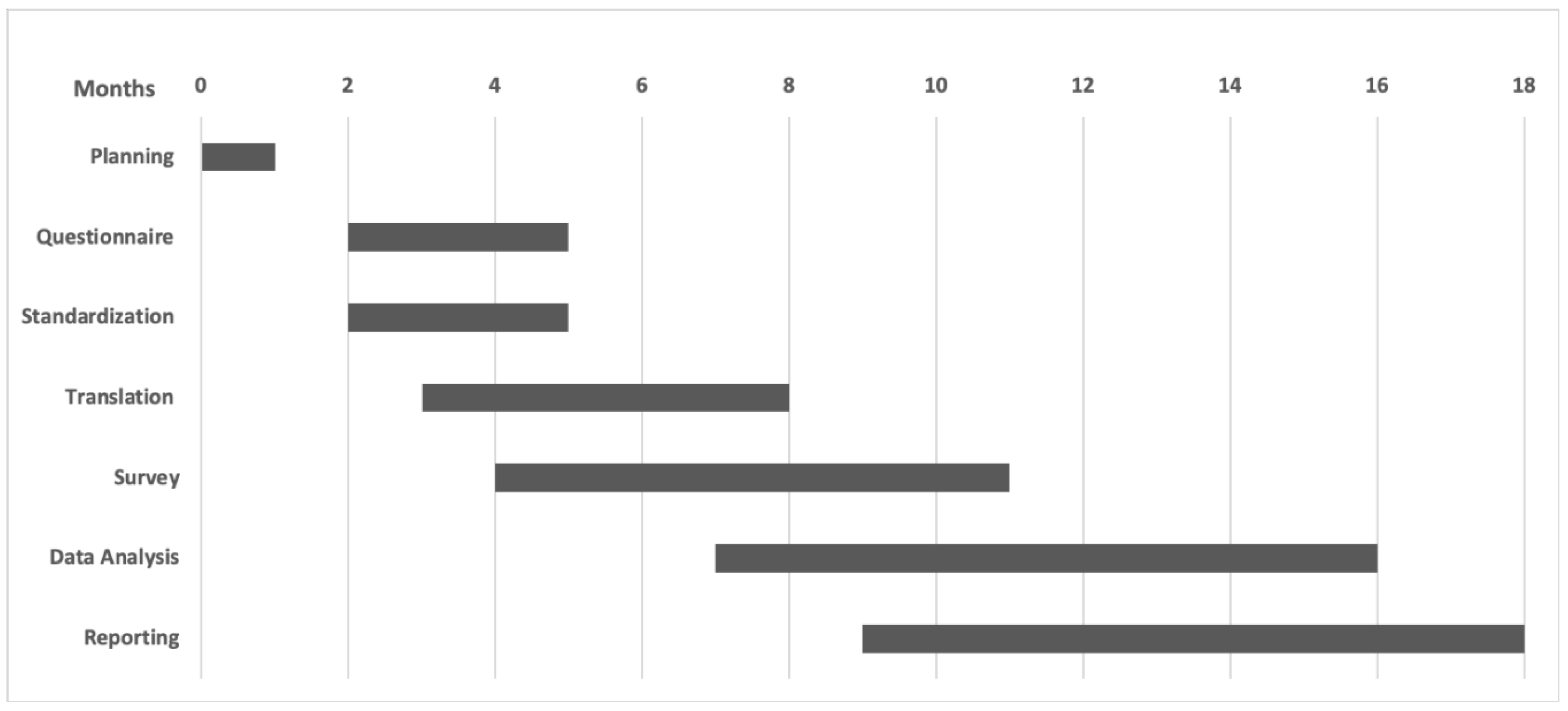
2.2. Time Period
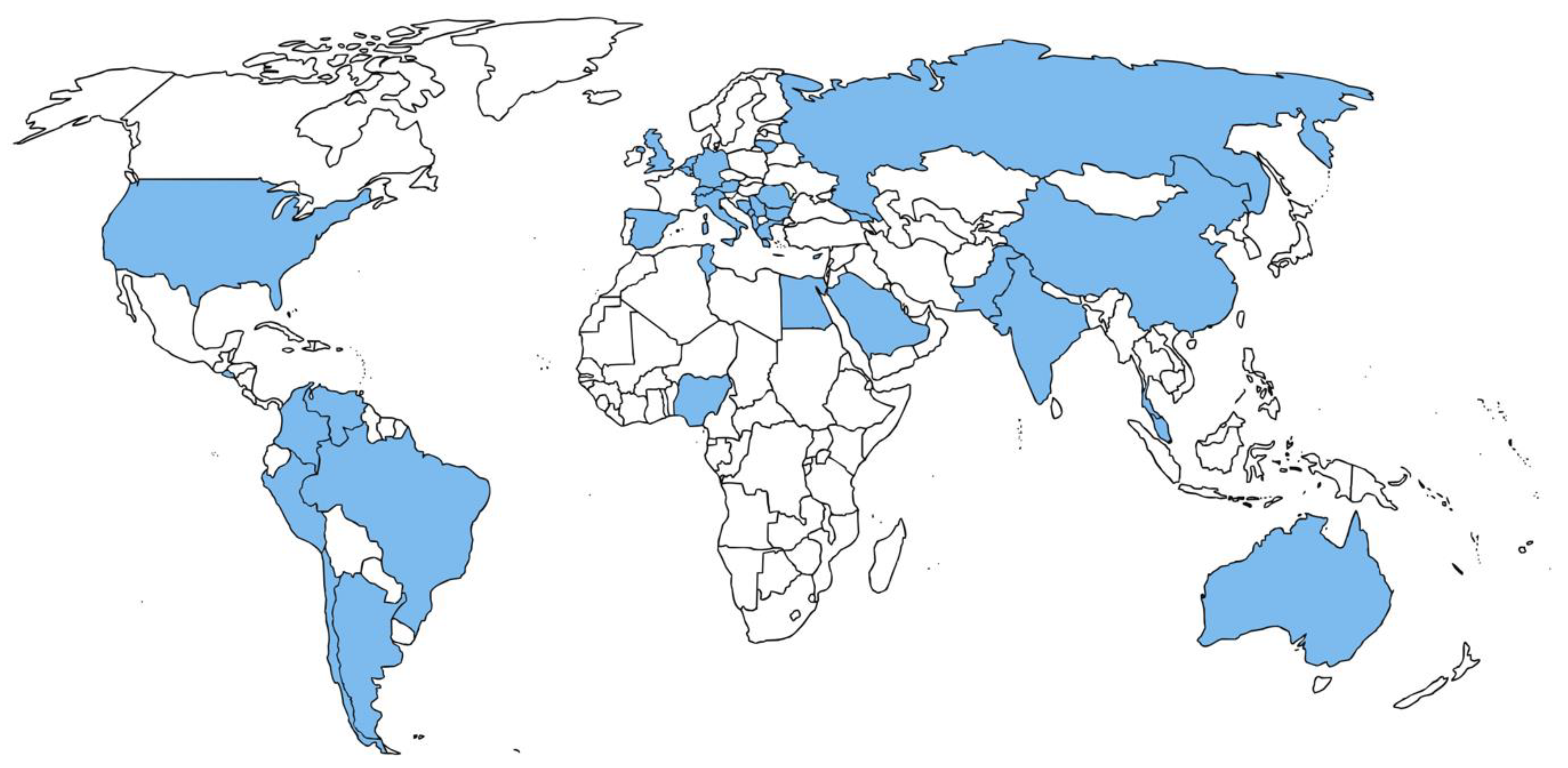
2.3. Study Settings
2.4. Study Population
2.5. Sample Size Calculation
2.6. Development and Refinement of the Questionnaire
- Stage I (Questionnaire translation and testing):
- Stage II (Pilot test and semantic adjustment of questionnaire)
2.7. Coordination and Survey Participation Sites
- Obtaining local audits, or research ethics approval (IRB/HREC approval).
- Identifying dentists who will be invited to participate in the survey.
- Deciding on which platform the survey will run in their country, how to reach the dentists, and when to run the survey. The platform for the survey will be set to avoid duplicated answers. The duration of the survey in each country will be for, at least, seven days.
- Accuracy and any misconduct related to their research project.
- Supporting translation of the questionnaire (both forward and reverse translations) into the local language and conducting the pilot test and semantic adjustment of the questionnaire.
- Following all steps of the local survey.
- Verifying that the data are accurately collected and organized, before sending them to the central management team (University of Bern).
- Writing a report about the country-based local data.
2.8. Data Management
2.9. Ethical Approval
2.10. Confidentiality and Data Retention
3. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention (CDC): Healthcare Personnel Preparedness Checklist for 2019-nCoV. Available online: https://www.cdc.gov/coronavirus/2019-ncov/downloads/hcp-preparedness-checklist.pdf (accessed on 4 June 2020).
- World Health Organization (WHO): Coronavirus Disease (COVID-2019) Advice for the Public. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 22 July 2020).
- Chen, X.; Ran, L.; Liu, Q.; Hu, Q.; Du, X.; Tan, X. Hand Hygiene, Mask-Wearing Behaviors and Its Associated Factors during the COVID-19 Epidemic: A Cross-Sectional Study among Primary School Students in Wuhan, China. Int. J. Environ. Res. Public Health 2020, 17, 2893. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Available online: https://www.ecdc.europa.eu/en/cases-2019-ncov-eueea (accessed on 22 July 2020).
- Hodge, J.G., Jr. Emergency Legal Preparedness: COVID-19. Available online: https://www.networkforphl.org/resources/emergency-legal-preparedness-covid19/ (accessed on 18 June 2020).
- Volgenant, C.M.C.; de Soet, J.J. Cross-transmission in the Dental Office: Does This Make You Ill? Curr. Oral Health Rep. 2018, 5, 221–228. [Google Scholar] [CrossRef]
- Szymańska, J. Dental bioaerosol as an occupational hazard in a dentist’s workplace. Ann. Agric. Environ. Med. 2007, 14, 203–207. [Google Scholar]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 9. [Google Scholar] [CrossRef]
- Zemouri, C.; de Soet, H.; Crielaard, W.; Laheij, A. A scoping review on bio-aerosols in healthcare and the dental environment. PLoS ONE 2017, 12, e0178007. [Google Scholar] [CrossRef] [PubMed]
- Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; Lloyd-Smith, J.O.; de Wit, E.; Munster, V.J.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar]
- Brug, J.; Aro, A.R.; Oenema, A.; de Zwart, O.; Richardus, J.H.; Bishop, G.D. SARS risk perception, knowledge, precautions, and information sources, The Netherlands. Emerg. Infect. Dis. 2004, 10, 1486–1489. [Google Scholar] [CrossRef] [PubMed]
- Stehr-Green, P.A.; Stehr-Green, J.K.; Nelson, A. Developing a questionnaire. Focus Field Epidemiol. 2003, 2, 1–6. [Google Scholar]
- Cagetti, M.G.; Cairoli, J.L.; Senna, A.; Campus, G. COVID-19 Outbreak in North Italy: An Overview on Dentistry. A Questionnaire Survey. Int. J. Environ. Res. Public Health 2020, 17, 3835. [Google Scholar] [CrossRef] [PubMed]
- Khader, Y.; Al Nsour, M.; Al-Batayneh, O.B.; Saadeh, R.; Bashier, H.; Alfaqih, M.; Al-Azzam, S. Dentists’ Awareness, Perception, and Attitude Regarding COVID-19 and Infection Control: Cross-Sectional Study Among Jordanian Dentists. JMIR Public Health Surveill. 2020, 6, e18798. [Google Scholar] [CrossRef] [PubMed]
- Spagnuolo, G.; De Vito, D.; Rengo, S.; Tatullo, M. COVID-19 Outbreak: An Overview on Dentistry. Int. J. Environ. Res. Public Health 2020, 17, 2094. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC): Guidance for Dental Settings. Interim Infection Prevention and Control Guidance for Dental Settings During the COVID-19 Response. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html (accessed on 11 June 2020).
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campus, G.; Diaz-Betancourt, M.; Cagetti, M.G.; Carvalho, J.C.; Carvalho, T.S.; Cortés-Martinicorena, J.F.; Deschner, J.; Douglas, G.V.A.; Giacaman, R.A.; Machiulskiene, V.; et al. Study Protocol for an Online Questionnaire Survey on Symptoms/Signs, Protective Measures, Level of Awareness and Perception Regarding COVID-19 Outbreak among Dentists. A Global Survey. Int. J. Environ. Res. Public Health 2020, 17, 5598. https://doi.org/10.3390/ijerph17155598
Campus G, Diaz-Betancourt M, Cagetti MG, Carvalho JC, Carvalho TS, Cortés-Martinicorena JF, Deschner J, Douglas GVA, Giacaman RA, Machiulskiene V, et al. Study Protocol for an Online Questionnaire Survey on Symptoms/Signs, Protective Measures, Level of Awareness and Perception Regarding COVID-19 Outbreak among Dentists. A Global Survey. International Journal of Environmental Research and Public Health. 2020; 17(15):5598. https://doi.org/10.3390/ijerph17155598
Chicago/Turabian StyleCampus, Guglielmo, Marcela Diaz-Betancourt, Maria Grazia Cagetti, Joana C. Carvalho, Thiago S. Carvalho, Javier F. Cortés-Martinicorena, James Deschner, Gail V. A. Douglas, Rodrigo A. Giacaman, Vita Machiulskiene, and et al. 2020. "Study Protocol for an Online Questionnaire Survey on Symptoms/Signs, Protective Measures, Level of Awareness and Perception Regarding COVID-19 Outbreak among Dentists. A Global Survey" International Journal of Environmental Research and Public Health 17, no. 15: 5598. https://doi.org/10.3390/ijerph17155598
APA StyleCampus, G., Diaz-Betancourt, M., Cagetti, M. G., Carvalho, J. C., Carvalho, T. S., Cortés-Martinicorena, J. F., Deschner, J., Douglas, G. V. A., Giacaman, R. A., Machiulskiene, V., Manton, D. J., Raggio, D. P., Ramos-Gomez, F., Sava-Rosianu, R., Morozova, N. S., Spagnuolo, G., Vukovic, A., Wolf, T. G., & on behalf of the COVIDental Collaboration Group. (2020). Study Protocol for an Online Questionnaire Survey on Symptoms/Signs, Protective Measures, Level of Awareness and Perception Regarding COVID-19 Outbreak among Dentists. A Global Survey. International Journal of Environmental Research and Public Health, 17(15), 5598. https://doi.org/10.3390/ijerph17155598










