Implications of Professional Occupation Related to Obesity in Patients Undergoing Bariatric Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Clinical Assesment and Data Collection
2.3. Surgical Procedure
2.4. Ethical Considerations
2.5. Statistical Analysis
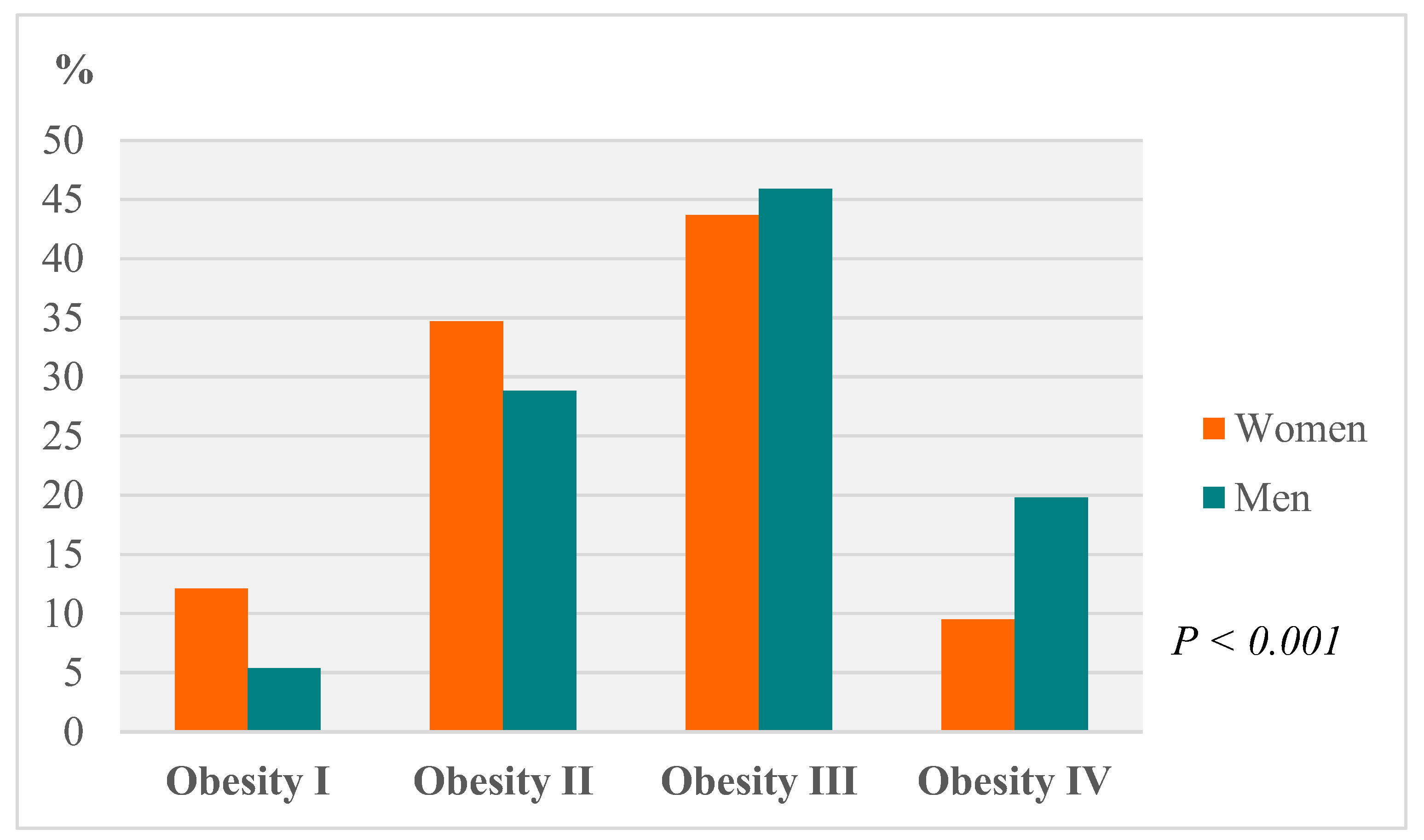
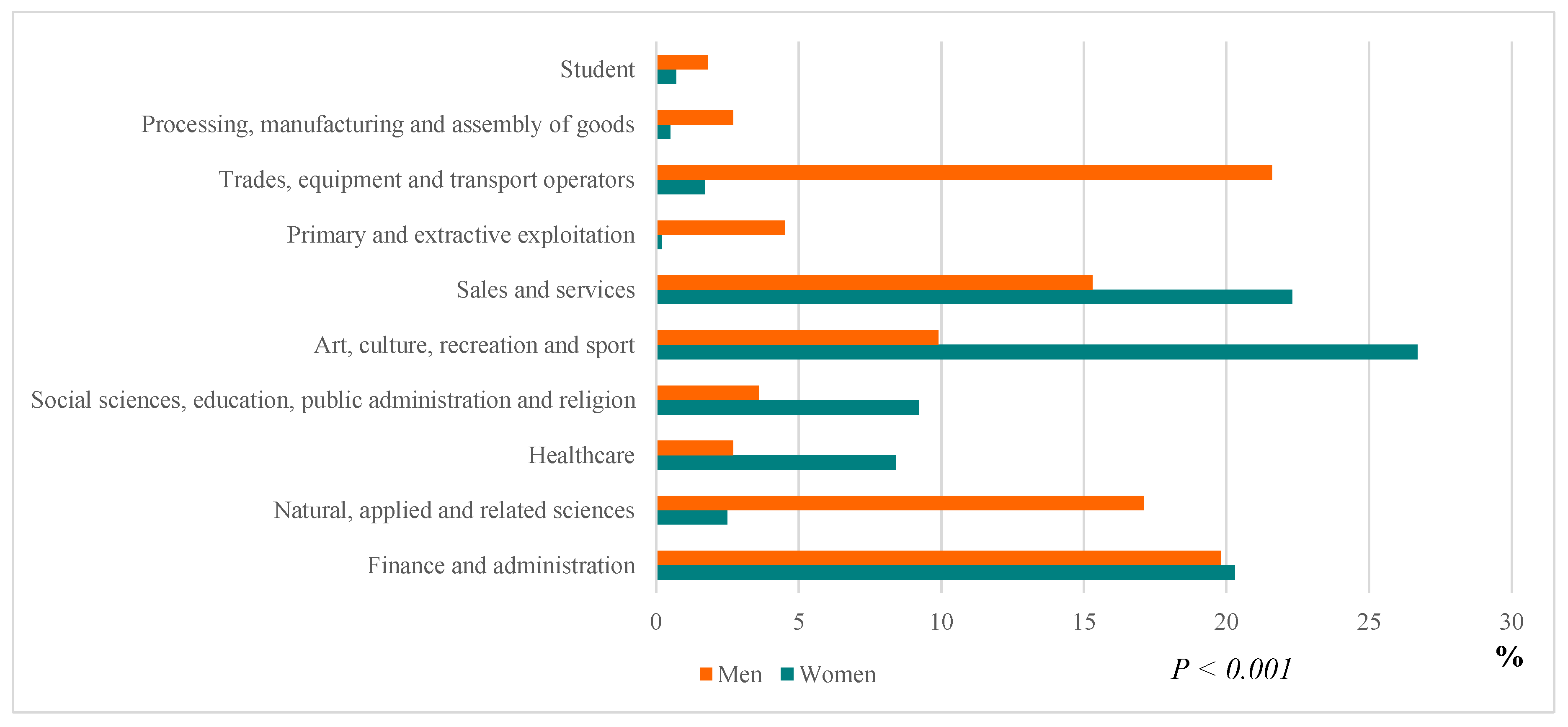
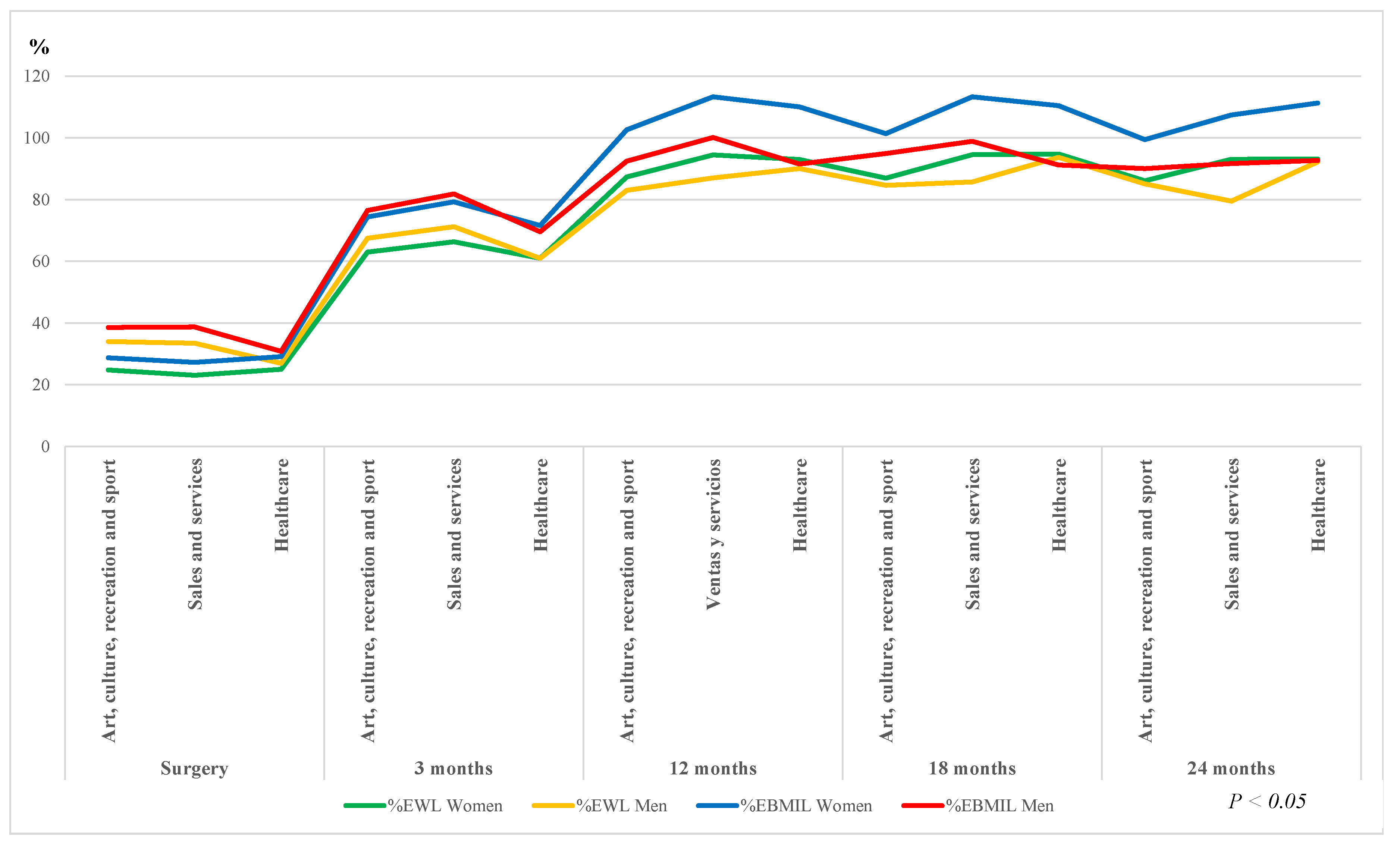
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Organización Mundial de la Salud (OMS) Obesidad y Sobrepeso. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 20 May 2020).
- Obesidad Mundial. Federación Mundial de Obesidad. Available online: https://www.worldobesity.org/about/about-obesity (accessed on 20 May 2020).
- Organización Mundial de la Salud (OMS) OMS. Control de la Epidemia Mundial de Obesidad. Available online: https://www.who.int/nutrition/topics/obesity/en/ (accessed on 27 May 2020).
- Finkelstein, E.A.; Trogdon, J.G.; Cohen, J.W.; Dietz, W. Annual Medical Spending Attributable To Obesity: Payer-And Service-Specific Estimates. Health Aff. (Millwood) 2009, 28, w822–w831. [Google Scholar] [CrossRef] [PubMed]
- Buchwald, H.; Avidor, Y.; Braunwald, E.; Jensen, M.D.; Pories, W.; Fahrbach, K.; Schoelles, K. Bariatric surgery: A systematic review and meta-analysis. JAMA 2004, 292, 1724–1737. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Janssen, I. The Economic Costs Associated With Physical Inactivity and Obesity in Canada: An Update. Can. J. Appl. Physiol. 2004, 29, 90–115. [Google Scholar] [CrossRef] [PubMed]
- Akil, L.; Ahmad, H.A. Effects of socioeconomic factors on obesity rates in four southern states and Colorado. Ethn. Dis. 2011, 21, 58–62. [Google Scholar] [PubMed]
- Jusot, F.; Khlat, M.; Rochereau, T.; Serme, C. Job loss from poor health, smoking and obesity: A national prospective survey in France. J. Epidemiol. Community Health 2008, 62, 332–337. [Google Scholar] [CrossRef] [PubMed]
- Mummery, W.K.; Schofield, G.M.; Steele, R.; Eakin, E.G.; Brown, W.J. Occupational sitting time and overweight and obesity in australian workers. Am. J. Prev. Med. 2005, 29, 91–97. [Google Scholar] [CrossRef]
- Kudel, I.; Huang, J.C.; Ganguly, R. Impact of Obesity on Work Productivity in Different US Occupations: Analysis of the National Health and Wellness Survey 2014 to 2015. J. Occup. Environ. Med. 2018, 60, 6–11. [Google Scholar] [CrossRef]
- Yarborough, C.M., III; Brethauer, S.; Burton, W.N.; Fabius, R.J.; Hymel, P.; Kothari, S.; Kushner, R.F.; Morton, J.M.; Mueller, K.; Pronk, N.P.; et al. Obesity in the Workplace: Impact, Outcomes, and Recommendations. J. Occup. Environ. Med. 2018, 60, 97–107. [Google Scholar] [CrossRef]
- Guh, D.P.; Zhang, W.; Bansback, N.; Amarsi, Z.; Birmingham, C.L.; Anis, A. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health 2009, 9, 88. [Google Scholar] [CrossRef]
- Golzarand, M.; Toolabi, K.; Farid, R. The bariatric surgery and weight losing: A meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults. Surg. Endosc. 2017, 31, 4331–4345. [Google Scholar] [CrossRef]
- Sampalis, J.S.; Liberman, M.; Auger, S.; Christou, N.V. The impact of weight reduction surgery on health-care costs in morbidly obese patients. Obes. Surg. 2004, 14, 939–947. [Google Scholar] [CrossRef] [PubMed]
- Vayr, F.; Charras, L.; Savall, F.; Soulat, J.M.; Ritz, P.; Herin, F. The Impact of Bariatric Surgery on Employment: A Systematic Review. Bariatr. Surg. Pr. Patient Care 2018, 13, 54–63. [Google Scholar] [CrossRef]
- Hawkins, S.C.; Osborne, A.; Finlay, I.G.; Alagaratnam, S.; Edmond, J.R.; Welbourn, R. Paid work increases and state benefit claims decrease after bariatric surgery. Obes. Surg. 2007, 17, 434–437. [Google Scholar] [CrossRef] [PubMed]
- Welbourn, R.; Hollyman, M.; Kinsman, R.; Dixon, J.; Liem, R.; Ottosson, J.; Ramos, A.; Våge, V.; Al-Sabah, S.; Brown, W.; et al. Bariatric Surgery Worldwide: Baseline Demographic Description and One-Year Outcomes from the Fourth IFSO Global Registry Report 2018. Obes. Surg. 2019, 29, 782–795. [Google Scholar] [CrossRef]
- Carbajo, M.A.; Luque-de-León, E.; Jiménez, J.M.; Ortiz-de-Solórzano, J.; Pérez-Miranda, M.; Castro-Alija, M.J. Laparoscopic One-Anastomosis Gastric Bypass: Technique, Results, and Long-Term Follow-Up in 1200 Patients. Obes. Surg. 2017, 27, 1153–1167. [Google Scholar] [CrossRef]
- Sharples, A.J.; Cheruvu, C.V. Systematic Review and Meta-Analysis of Occupational Outcomes after Bariatric Surgery. Obes. Surg. 2017, 27, 774–781. [Google Scholar] [CrossRef]
- Dixon, J.B.; Zimmet, P.; Alberti, K.G.; Rubino, F. Bariatric surgery: An IDF statement for obese Type 2 diabetes. Surg. Obes. Relat. Dis. 2011, 7, 433–447. [Google Scholar] [CrossRef]
- International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO). Available online: https://www.ifso.com/about-ifso/ (accessed on 29 May 2020).
- Clasificación Nacional de Ocupaciones, C.N.O. Una herramienta para gestión de empleo y formación. Available online: https://www.oei.es/historico/oeivirt/fp/cuad2a03.htm (accessed on 29 May 2020).
- Magouliotis, D.E.; Tasiopoulou, V.S.; Tzovaras, G. One anastomosis gastric bypass versus Roux-en-Y gastric bypass for morbid obesity: A meta-analysis. Clin. Obes. 2018, 8, 159–169. [Google Scholar] [CrossRef]
- Carbajo, M.A.; Luque-de-León, E. Mini-gastric bypass/one-anastomosis gastric bypass—Standardizing the name. Obes. Surg. 2015, 25, 858–859. [Google Scholar] [CrossRef]
- Ruiz-Tovar, J.; Carbajo, M.A.; Jiménez, J.M.; Luque-de-Leon, E.; Ortiz-De-Solorzano, J.; Castro, M.J. Are There Ideal Small Bowel Limb Lengths for One-Anastomosis Gastric Bypass (OAGB) to Obtain Optimal Weight Loss and Remission of Comorbidities with Minimal Nutritional Deficiencies? World J. Surg. 2020, 44, 855–862. [Google Scholar] [CrossRef]
- Clasificación del Sobrepeso y la Obesidad Según el IMC. Sociedad Española para el Estudio de la Obesidad. Available online: https://www.seedo.es/index.php/pacientes/calculo-imc (accessed on 29 May 2020).
- Proper, K.I.; Hildebrandt, V.H. Overweight and obesity among Dutch workers: Differences between occupational groups and sectors. Int. Arch. Occup. Environ. Health 2010, 83, 61–68. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Barclay, K.S.; Forwell, S. Occupational Performance Issues of Adults Seeking Bariatric Surgery for Obesity. Am. J. Occup. Ther. 2018, 72, 7205195030p1–7205195030p10. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, M.; Nautiyal, H.K.; Mathur, W.; Kosta, S. OAGB vs BGBP: A retrospective comparative study of a cohort of patients who had bariatric surgery in 2012 at one centre by a single surgeon. Clin. Obes. 2019, 9, e12308. [Google Scholar] [CrossRef] [PubMed]
- Hutter, M.M.; Schirmer, B.D.; Jones, D.B.; Ko, C.Y.; Cohen, M.E.; Merkow, R.P.; Nguyen, N.T. First Report from the American College of Surgeons Bariatric Surgery Center Network: Laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann. Surg. 2011, 254, 410–422. [Google Scholar] [CrossRef] [PubMed]
- Wagner, A.J.; Fabry, J.M.; Thirlby, R.C. Return to Work After Gastric Bypass in Medicaid-Funded Morbidly Obese Patients. Arch. Surg. 2007, 142, 935. [Google Scholar] [CrossRef] [PubMed]
| % of Men (n) | % of Men (n) | Total % (n) | |
|---|---|---|---|
| High blood pressure | 24.4% (95) | 56.8% (63) * | 31.5% (158) |
| Oral anti-hypertensive drugs treatment | 16.2% (63) | 36.9% (41) * | 20.8% (104) |
| Diabetes Mellitus | 13.1% (51) | 18% (20) | 14.2% (71) |
| Treatment with oral anti-diabetics | 6.2% (24) | 7.2% (8) | 6.4% (32) |
| Insulin treatment | 1% (4) | 3.6% (4) | 1.6% (8) |
| Obstructive sleep apnea syndrome | 77.7% (303) | 86.5% (96) * | 79.6% (399) |
| Respiratory failure | 93.6% (365) | 98.2% (109) * | 94.6% (474) |
| Arthropathy | 84.6% (330) | 78.4% (87) | 83.2% (417) |
| Varicose veins | 35.6% (139) * | 21.6% (24) | 32.5% (163) |
| Dyslipemia | 56.9% (222) | 64.9% (72) | 58.7% (294) |
| Hepatic steatosis | 67.7% (264) | 82% (91) * | 70.9% (355) |
| Gastroesophageal reflux | 35.4% (138) | 37.8% (42) | 35.9% (180) |
| Hiatal hernia | 46.7% (182) | 56.8% (63) * | 48.9% (245) |
| Cholelithiasis | 13.1% (51) | 8.1% (9) | 12% (60) |
| Thyroid disease | 9.7% (38) * | 3.6% (4) | 8.4% (42) |
| Anxiety | 1.8% (7) | - | 1.4% (7) |
| Depression | 46.7% (182) * | 18.9% (21) | 40.5% (203) |
| Psychiatric treatment | 23.8% (93) * | 9.9% (11) | 20.8% (104) |
| Preoperative | 3 Months | 12 Months | 18 Months | 24 Months | ||
|---|---|---|---|---|---|---|
| Finance and administration | Weight | 110.6 ± 20 | 78.3 ± 12.6 * | 68.4 ± 13.1 * | 66.2 ± 14.1 * | 68.2 ± 15.1 * |
| BMI | 40.8 ± 5.7 | 29 ± 3.8 * | 25 ± 3.5 * | 24.2 ± 3.3 * | 25 ± 3.7 * | |
| % EWL | 24.9 ± 9.5 | 66.8 ± 13.8 * | 90.2 ± 19 * | 93.3 ± 17.9 * | 89.3 ± 19.2 * | |
| % EBMIL | 28.7 ± 11 | 79.9 ± 21.4 * | 106 ± 29.8 * | 111.3 ± 27.4 * | 107.4 ± 30 * | |
| Natural, applied and related sciences | Weight | 126.9 ± 29 | 86.1 ± 15.6 * | 78.4 ± 15.3 * | 82.7 ± 13.5 * | 84.8 ± 7.6 * |
| BMI | 43.3 ± 8.2 | 29.5 ± 4.9 * | 26.2 ± 3.7 * | 26.7 ± 2.7 * | 27.1 ± 1.9 * | |
| % EWL | 30.6 ± 11.1 | 69.7 ± 14.8 * | 84.9 ± 14 * | 82.2 ± 11.2 * | 80.6 ± 4.8 * | |
| % EBMIL | 37.1 ± 14 | 82.6 ± 16.2 * | 98.1 ± 19.3 * | 92.1 ± 12 * | 91.7 ± 8.4 * | |
| Healthcare | Weight | 114.3 ± 21.6 | 81.9 ± 14.1 * | 66.4 ± 11.9 * | 70.1 ± 6.9 * | 66.6 ± 9 * |
| BMI | 41.9 ± 6.3 | 29.9 ± 3.5 * | 24.1 ± 3.5 * | 23.9 ± 2.3 * | 23.5 ± 3.2 * | |
| % EWL | 25.1 ± 7.3 | 61 ± 13.3 * | 92.9 ± 13.9 * | 94.8 ± 9.8 * | 93.1 ± 16.6 * | |
| % EBMIL | 29.3 ± 8.3 | 71.3 ± 16.1 * | 110.1 ± 18.4 * | 110.4 ± 15.4 * | 111.3 ± 20.3 * | |
| Social sciences, education, public administration and religion | Weight | 114.3 ± 22.2 | 82.8 ± 17.6 * | 66.7 ± 11.7* | 67.6 ± 15.3 * | 72.9 ± 18.2 * |
| BMI | 42.2 ± 6.1 | 30.4 ± 4.8 * | 24.6 ± 3.5 * | 25.6 ± 4.7 * | 25 ± 5.3 * | |
| % EWL | 2.8 ± 9 | 62.2 ± 14.5 * | 90 ± 16 * | 87.4 ± 21.9 * | 96.2 ± 20.6 * | |
| % EBMIL | 26.6 ± 9.9 | 73.1 ± 20.2 * | 107 ± 21.7 * | 104.3 ± 25.2 * | 118.2 ± 20.9 * | |
| Art, culture, recreation and sport | Weight | 112.1 ± 19.8 | 79.5 ± 14.2 * | 67.1 ± 15.3 * | 66.2 ± 13.5 * | 65.4 ± 10.1 * |
| BMI | 43 ± 6.7 | 30.7 ± 5.1 * | 26.11 ± 5.4 * | 25.6 ± 3.9 * | 25.7 ± 3.2 * | |
| % EWL | 25.6 ± 9.3 | 63.4 ± 15.7 * | 87 ± 18.2 * | 86.8 ± 16.1 * | 86.1 ± 14.2 * | |
| % EBMIL | 29.7 ± 10.8 | 74.6 ± 22.7 * | 101.9 ± 23.4 * | 100.9 ± 21.7 * | 99.4 ± 20.1 * | |
| Sales and services | Weight | 111.6 ± 19.7 | 78.1 ± 13.1 * | 65.4 ± 10.4 * | 66.3 ± 10 * | 64.8 ± 9.1 * |
| BMI | 41.5 ± 6.2 | 29.2 ± 4.6 * | 24.3 ± 2.9 * | 24.3 ± 2.5 * | 24.6 ± 2.7 * | |
| % EWL | 24.8 ± 9.9 | 67 ± 15.9 * | 93 ± 15.2 * | 92.2 ± 13.8 * | 90.5 ± 13.7 * | |
| % EBMIL | 29.1 ± 11.4 | 79.7 ± 22.6 * | 110.7 ± 24.7 * | 109.6 ± 24.3 * | 104.5 ± 17.9 * | |
| Primary and extractive exploitation | Weight | 129.7 ± 37.7 | 79.2 ± 7.7 * | 65 ± 1.4 * | 72.5 ± 7.7 * | 69.8 ± 7 * |
| BMI | 44.8 ± 13.1 | 27.5 ± 3.2 * | 25.4 ± 2.3 * | 25.8 ± 2.4 * | 25.2 ± 1.8 * | |
| % EWL | 30.6 ± 4.4 | 74.1 ± 14.5 * | 82.6 ± 17.6 * | 78.5 ± 15.5 * | 84 ± 13* | |
| % EBMIL | 35.7 ± 4.1 | 86.3 ± 18.2 * | 94.4 ± 14.8 * | 93.8 ± 18.3 * | 97.5 ± 12.9 * | |
| Trades, equipment and transport operators | Weight | 125.7 ± 19.7 | 84.4 ± 11.4 * | 76.3 ± 13.2 * | 78.3 ± 10.9 * | 81.2 ± 8.5 * |
| BMI | 42.3 ± 5.9 | 28.4 ± 3.9 * | 25.3 ± 3.3 * | 26.4 ± 3.8 * | 25.8 ± 3.4 * | |
| % EWL | 30.6 ± 9.9 | 70.5 ± 15.3 * | 86 ± 14.8 * | 79.1 ± 17.3 * | 79.9 ± 15.2 * | |
| % EBMIL | 35.9 ± 12 | 83.5 ± 21 * | 101.2 ± 19.1 * | 94.5 ± 23.7 * | 97.2 ± 19.9 * | |
| Processing, manufacturing and assembly of goods | Weight | 124.1 ± 21.9 | 85.6 ± 9.9 * | 71.6 ± 9.7 * | 72.4 ± 13.8 * | 70.5 ± 8.1 * |
| BMI | 38.7 ± 4.8 | 27.9 ± 2 * | 23.2 ± 0.9 * | 23.6 ± 1.7 * | 22.5 ± 1.4 * | |
| % EWL | 30.8 ± 7.6 | 67.5 ± 8.8 * | 95.2 ± 4.2 * | 94.4 ± 7.7 * | 99.2 ± 8.3 * | |
| % EBMIL | 37 ± 7.4 | 81.3 ± 14.1 * | 114.3 ± 9.2 * | 110.2 ± 11.8 * | 129.3 ± 13.2 | |
| Student | Weight | 136.1 ± 24.3 | 89.6 ± 11.1 * | 74.4 ± 9.9 * | 75.1 ± 12.5 * | 74.3 ± 11.9 * |
| BMI | 46.9 ± 6.7 | 31 ± 3.1 * | 25.7 ± 1.8 * | 25.8 ± 2.1 * | 25.5 ± 1.9 * | |
| % EWL | 28.8 ± 5.5 | 64,9 ± 8.4 * | 87.4 ± 5.5 * | 86.9 ± 6 * | 87.9 ± 5.5 * | |
| % EBMIL | 32.3 ± 5.6 | 73 ± 9.5 * | 98.5 ± 8.8 * | 97.9 ± 9.3 * | 99.1 ± 8.8 * |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiménez, J.-M.; García, S.; Carbajo, M.-Á.; López, M.; Cao, M.-J.; Ruiz-Tovar, J.; Castro, M.-J. Implications of Professional Occupation Related to Obesity in Patients Undergoing Bariatric Surgery. Int. J. Environ. Res. Public Health 2020, 17, 5557. https://doi.org/10.3390/ijerph17155557
Jiménez J-M, García S, Carbajo M-Á, López M, Cao M-J, Ruiz-Tovar J, Castro M-J. Implications of Professional Occupation Related to Obesity in Patients Undergoing Bariatric Surgery. International Journal of Environmental Research and Public Health. 2020; 17(15):5557. https://doi.org/10.3390/ijerph17155557
Chicago/Turabian StyleJiménez, José-María, Sara García, Miguel-Ángel Carbajo, María López, María-José Cao, Jaime Ruiz-Tovar, and María-José Castro. 2020. "Implications of Professional Occupation Related to Obesity in Patients Undergoing Bariatric Surgery" International Journal of Environmental Research and Public Health 17, no. 15: 5557. https://doi.org/10.3390/ijerph17155557
APA StyleJiménez, J.-M., García, S., Carbajo, M.-Á., López, M., Cao, M.-J., Ruiz-Tovar, J., & Castro, M.-J. (2020). Implications of Professional Occupation Related to Obesity in Patients Undergoing Bariatric Surgery. International Journal of Environmental Research and Public Health, 17(15), 5557. https://doi.org/10.3390/ijerph17155557






