Improving Breastfeeding by Empowering Mothers in Vietnam: A Randomised Controlled Trial of a Mobile App
Abstract
1. Introduction
1.1. The Benefits of Breastfeeding and the Current Rates of Breastfeeding in Vietnam
1.2. Barriers to Breastfeeding Practices in Vietnam
1.3. Community-Based Interventions to Improved Breastfeeding Outcomes
2. Methods
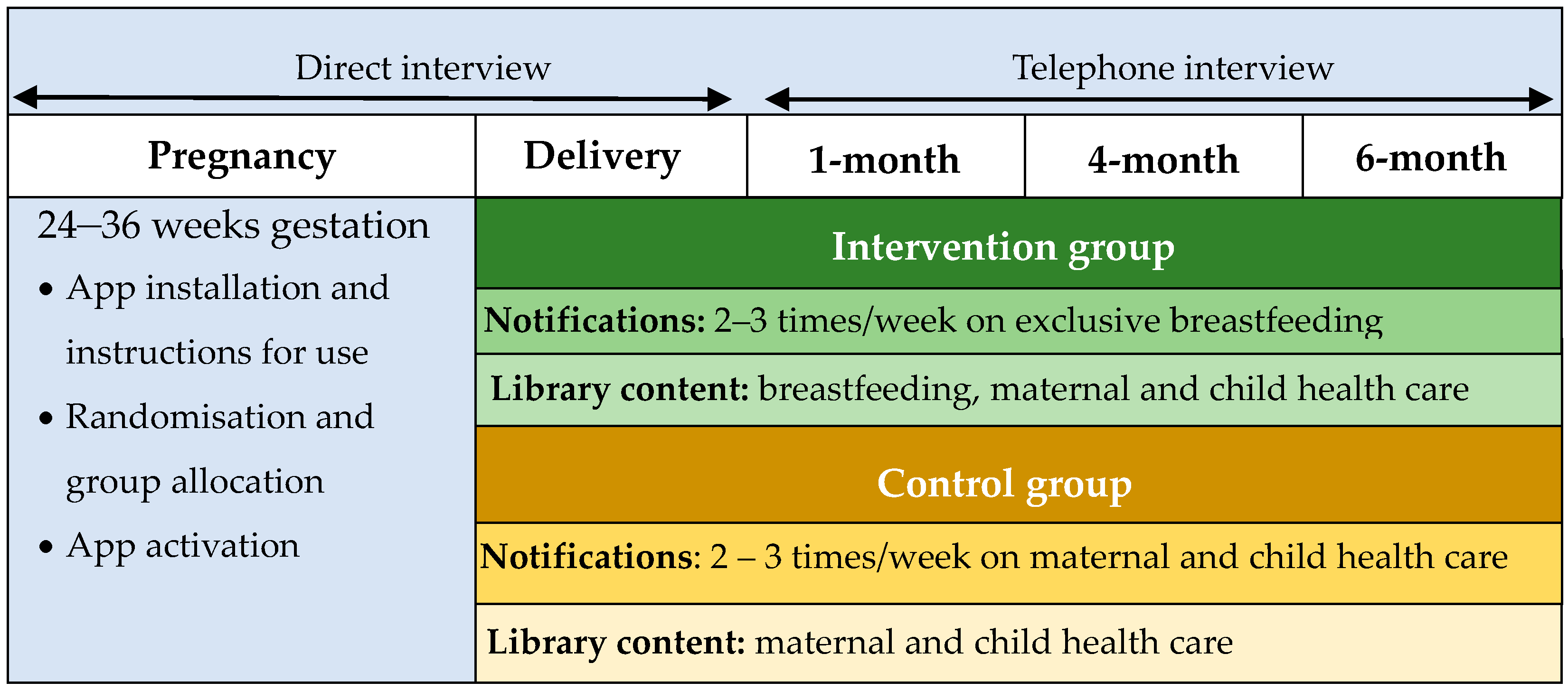
2.1. Trial Design
2.2. Participants
- attending antenatal clinics at 24–36 weeks of gestation;
- own a smartphone with at least:
- iOS version 11 (announced from 2017, support for iPhones from 2015)
- Android 5 (released from 2014);
- carrying a singleton foetus.
- being referred from other hospitals for high-risk pregnancy treatments;
- receiving advice from doctors against breastfeeding because of her health condition (e.g., positive T-cell lymphotropic virus, untreated brucellosis, varicella, H1N1 influenza) [111];
- where an infant is born with a birth weight of less than 2500, or is admitted to neonatal intensive care unit, the mother will continue receiving information from the app, but will be excluded from the analysis;
2.3. Intervention
- establish beliefs on the benefits of exclusive breastfeeding until 6 months;
- enhance the perception of sufficient breastmilk, for both vaginal delivery and caesarean section mothers;
- plan/commit to breastfeeding exclusively from birth;
- benefits and feasibility of early initiation of breastfeeding;
- overcome difficulties of breastfeeding; able to breastfeed without pain/problems;
- encourage mothers to seek advice and maintain communication with health professionals;
- involve husbands and grandmothers in preparation for exclusive breastfeeding;
- ask friends and relatives not to bring gifts of infant formula to the hospital or to the home.
2.4. Outcomes
- early initiation of breastfeeding: Proportion of infants at the first month of age who were put to the breast within one hour of birth;
- exclusive breastfeeding: Proportion of infants at 1, 4, 6 months of age who were fed by breast milk only during the previous day, and from birth;
- predominant breastfeeding: Proportion of infants at 1, 4, 6 months of age who received breast milk as the predominant source of nourishment during the previous day, and from birth;
- any breastfeeding: Proportion of infants at 1, 4, 6 months of age who were ever breastfed;
- duration of exclusive breastfeeding: The age in weeks when infants received only breast milk from birth;
- introduction of complementary and solid foods: Proportion of infants at 1, 4, 6 months of age who received solid, semi-solid, or soft foods.
2.5. Sample Size
3. Randomisation and Masking
3.1. Randomisation Procedure
3.2. Sequence Generation
3.3. Allocation Concealment Mechanism
3.4. Implementation
3.5. Analytical Methods
3.6. Ethical Issues
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Victora, C.G.; Bahl, R.; Barros, A.J.D.; Franca, G.V.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef]
- Kramer, M.S.; Kakuma, R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst. Rev. 2012, 8, 1–95. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, J.O.; Garnett, T.; Rollins, N.C.; Roos, E. The carbon footprint of breastmilk substitutes in comparison with breastfeeding. J. Clean. Prod. 2019, 222, 436–445. [Google Scholar] [CrossRef] [PubMed]
- Breastfeeding and the Sustainable Development Goals. Available online: https://worldbreastfeedingweek.org/2016/pdf/BreastfeedingandSDGsMessaging%20WBW2016%20Shared.pdf (accessed on 5 June 2020).
- WHO; UNICEF; USAID; AED; UCDAVIS; IFPRI. Indicators for Assessing Infant and Young Child Feeding Practices: Part 1-Definition: Conclusions of a Consensus Meeting Held 6–8 November 2007 in Washington D.C; WHO: Geneva, Switizerland, 2008; Volume 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/43895/9789241596664_eng.pdf;jsessionid=4DA1CF38AE72F60974EFE8C41A64C9F2?sequence=1 (accessed on 4 May 2020).
- Infant and Young Child Feeding. Available online: https://www.who.int/en/news-room/fact-sheets/detail/infant-and-young-child-feeding (accessed on 4 May 2020).
- WHO; UNICEF. Capture the Moment–Early Initiation of Breastfeeding: The Best Start for Every Newborn; UNICEF: New York, NY, USA, 2018.
- The United Nations Children’s Fund. Breastfeeding: A Mother’s Gift, for Every Child Page 5. Prepared by UNICEF’s Nutrition Section, Programme Division, Data and Analytics Section, Division of Data, Research and Policy, and Division of Communication; UNICEF: New York, NY, USA, 2018.
- Binns, C.; Low, W.Y. Progress in Global Health. Asia Pac. J. Public Health 2012, 24, 541–542. [Google Scholar] [CrossRef]
- World Health Organization Collaborative Group. Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: A pooled analysis. WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality. Lancet 2000, 355, 451–455. [Google Scholar]
- Lee, M.K.; Binns, C. Breastfeeding and the Risk of Infant Illness in Asia: A Review. Int. J. Env. Res. Public Health 2019, 17, 186. [Google Scholar] [CrossRef]
- Binns, C.W.; Lee, M.K. Exclusive breastfeeding for six months: The WHO six months recommendation in the Asia Pacific Region. Asia Pac. J. Clin. Nutr. 2014, 23, 344–350. [Google Scholar]
- Suzuki, K. The developing world of DOHaD. J. Dev. Orig. Health Dis. 2018, 9, 266–269. [Google Scholar] [CrossRef]
- Stiemsma, L.T.; Michels, K.B. The Role of the Microbiome in the Developmental Origins of Health and Disease. Pediatrics 2018, 141, e20172437. [Google Scholar] [CrossRef]
- Beghetti, I.; Biagi, E.; Martini, S.; Brigidi, P.; Corvaglia, L.; Aceti, A. Human Milk’s Hidden Gift: Implications of the Milk Microbiome for Preterm Infants’ Health. Nutrients 2019, 11, 2944. [Google Scholar] [CrossRef]
- Scott, J.A.; Ng, S.Y.; Cobiac, L. The relationship between breastfeeding and weight status in a national sample of Australian children and adolescents. BMC Public Health 2012, 12, 107. [Google Scholar] [CrossRef]
- Ip, S.; Chung, M.; Raman, G.; Chew, P.; Magula, N.; DeVine, D.; Trikalinos, T.; Lau, J. Breastfeeding and maternal and infant health outcomes in developed countries. Evid. Rep. Technol. Assess 2007, 153, 1–186. [Google Scholar]
- U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Support Breastfeeding; Department of Health and Human Services Office of the Surgeon General: Washington, DC, USA, 2011; pp. 1–57.
- Binns, C.; Lee, M.; Low, W.Y. The Long-Term Public Health Benefits of Breastfeeding. Asia Pac. J. Public Health 2016, 28, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Horta, B.L.; Loret de Mola, C.; Victora, C.G. Breastfeeding and intelligence: A systematic review and meta-analysis. Acta. Paediatr. 2015, 104, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Zielinska, M.A.; Hamulka, J. Protective Effect of Breastfeeding on the Adverse Health Effects Induced by Air Pollution: Current Evidence and Possible Mechanisms. Int. J. Env. Res. Public Health 2019, 16, 4181. [Google Scholar] [CrossRef]
- Yusuff, A.S.; Tang, L.; Binns, C.W.; Lee, A.H. Breastfeeding and Postnatal Depression: A Prospective Cohort Study in Sabah, Malaysia. J. Hum. Lact. 2016, 32, 277–281. [Google Scholar] [CrossRef]
- Yusuff, A.S.; Tang, L.; Binns, C.W.; Lee, A.H. Prevalence and risk factors for postnatal depression in Sabah, Malaysia: A cohort study. Women Birth 2015, 28, 25–29. [Google Scholar] [CrossRef]
- Del Ciampo, L.A.; Del Ciampo, I.R.L. Breastfeeding and the Benefits of Lactation for Women’s Health. Rev. Bras. De. Ginecol. E. Obstet. 2018, 40, 354–359. [Google Scholar] [CrossRef]
- National Health Medical Research Council. Infant Feeding Guidelines: Information for Health Workers; National Health and Medical Research Council: Canberra, Australia, 2012.
- Unar-Munguia, M.; Stern, D.; Colchero, M.A.; de Cosio, T.G. The burden of suboptimal breastfeeding in Mexico: Maternal health outcomes and costs. Matern. Child Nutr. 2019, 15, e12661. [Google Scholar] [CrossRef]
- Li, D.P.; Du, C.; Zhang, Z.M.; Li, G.X.; Yu, Z.F.; Wang, X.; Li, P.F.; Cheng, C.; Liu, Y.P.; Zhao, Y.S. Breastfeeding and ovarian cancer risk: A systematic review and meta-analysis of 40 epidemiological studies. Asian Pac. J. Cancer Prev. 2014, 15, 4829–4837. [Google Scholar] [CrossRef]
- World Cancer Research Fund International/American Instritute for Cancer Research. Continuous Update Project Report: Diet, Nutrition, Physcial Activity and Breast Cancer. Available online: https://www.wcrf.org/sites/default/files/Breast-Cancer-2017-Report.pdf (accessed on 4 June 2020).
- Su, D.; Pasalich, M.; Lee, A.H.; Binns, C.W. Ovarian cancer risk is reduced by prolonged lactation: A case-control study in southern China. Am. J. Clin. Nutr. 2013, 97, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Collaboration for Breast Cancer. Breast cancer and breastfeeding: Collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease. Lancet 2002, 360, 187–195. [Google Scholar] [CrossRef]
- Sharma, A.J.; Dee, D.L.; Harden, S.M. Adherence to breastfeeding guidelines and maternal weight 6 years after delivery. Pediatrics 2014, 134 (Suppl. 1), S42–S49. [Google Scholar] [CrossRef]
- Park, S.; Choi, N.K. Breastfeeding and Maternal Hypertension. Am. J. Hypertens. 2018, 31, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Feng, L.J.; Xu, Q.L.; Hu, Z.F.; Pan, H.Y. Lactation and progression to type 2 diabetes in patients with gestational diabetes mellitus: A systematic review and meta-analysis of cohort studies. J. Diabetes Investig. 2018, 9, 1360–1369. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Norat, T.; Romundstad, P.; Vatten, L.J. Breastfeeding and the maternal risk of type 2 diabetes: A systematic review and dose-response meta-analysis of cohort studies. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 107–115. [Google Scholar] [CrossRef]
- Jager, S.; Jacobs, S.; Kroger, J.; Fritsche, A.; Schienkiewitz, A.; Rubin, D.; Boeing, H.; Schulze, M.B. Breast-feeding and maternal risk of type 2 diabetes: A prospective study and meta-analysis. Diabetologia 2014, 57, 1355–1365. [Google Scholar] [CrossRef]
- Ley, S.H.; Chavarro, J.E.; Li, M.; Bao, W.; Hinkle, S.N.; Wander, P.L.; Rich-Edwards, J.; Olsen, S.; Vaag, A.; Damm, P.; et al. Lactation Duration and Long-term Risk for Incident Type 2 Diabetes in Women With a History of Gestational Diabetes Mellitus. Diabetes Care 2020, 43, 793–798. [Google Scholar] [CrossRef]
- Nguyen, C.L.; Pham, N.M.; Binns, C.W.; Duong, D.V.; Lee, A.H. Prevalence of Gestational Diabetes Mellitus in Eastern and Southeastern Asia: A Systematic Review and Meta-Analysis. J. Diabetes Res. 2018, 2018, 6536974. [Google Scholar] [CrossRef]
- Nguyen, B.; Jin, K.; Ding, D. Breastfeeding and maternal cardiovascular risk factors and outcomes: A systematic review. PLoS ONE 2017, 12, e0187923. [Google Scholar] [CrossRef]
- Schwarz, E.B. Invited Commentary: Breastfeeding and Maternal Cardiovascular Health--Weighing the Evidence. Am. J. Epidemiol. 2015, 181, 940–943. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, E.B.; Ray, R.M.; Stuebe, A.M.; Allison, M.A.; Ness, R.B.; Freiberg, M.S.; Cauley, J.A. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet. Gynecol. 2009, 113, 974–982. [Google Scholar] [CrossRef]
- Merritt, M.A.; Riboli, E.; Murphy, N.; Kadi, M.; Tjonneland, A.; Olsen, A.; Overvad, K.; Dossus, L.; Dartois, L.; Clavel-Chapelon, F.; et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition; A cohort study. BMC Med. 2015, 13, 252. [Google Scholar] [CrossRef] [PubMed]
- The United Nations Children’s Fund UNICEF Global database on Infant and Young Child Feeding. Available online: https://data.unicef.org/topic/nutrition/infant-and-young-child-feeding/ (accessed on 16 May 2020).
- The United Nations Children’s Fund. State of the World’s Children 2019 Page 219; Comunications Division UNICEF: New York, NY, USA, 2019.
- Duong, D.V.; Binns, C.W.; Lee, A.H. Breast-feeding initiation and exclusive breast-feeding in rural Vietnam. Public Health Nutr. 2004, 7, 795–799. [Google Scholar] [CrossRef] [PubMed]
- Duong, D.V.; Lee, A.H.; Binns, C.W. Determinants of breast-feeding within the first 6 months post-partum in rural Vietnam. J. Paediatr. Child Health 2005, 41, 338–343. [Google Scholar] [CrossRef]
- Bui, Q.T.-T.; Lee, H.-Y.; Le, A.T.-K.; Van Dung, D.; Vu, L.T.-H. Trends and determinants for early initiation of and exclusive breastfeeding under six months in Vietnam: Results from the Multiple Indicator Cluster Surveys, 2000–2011. Glob. Health Action 2016, 9, 29433. [Google Scholar] [CrossRef]
- Le, Q.-N.T.; Phung, K.-L.; Nguyen, V.-T.T.; Anders, K.L.; Nguyen, M.-N.; Hoang, D.-T.T.; Bui, T.-T.T.; Nguyen, V.-C.V.; Thwaites, G.E.; Simmons, C.; et al. Factors associated with a low prevalence of exclusive breastfeeding during hospital stay in urban and semi-rural areas of southern Vietnam. Int. Breastfeed. J. 2018, 13, 46. [Google Scholar] [CrossRef]
- Nguyen, P.; Binns, C.W.; Ha, A.V.V.; Chu, T.K.; Nguyen, L.C.; Duong, D.V.; Do, D.V.; Lee, A.H. Prelacteal and early formula feeding increase risk of infant hospitalisation: A prospective cohort study. Arch. Dis. Child. 2020, 105, 122–126. [Google Scholar] [CrossRef]
- Walters, D.; Horton, S.; Siregar, A.Y.M.; Pitriyan, P.; Hajeebhoy, N.; Mathisen, R.; Phan, L.T.H.; Rudert, C. The cost of not breastfeeding in Southeast Asia. Health Policy Plan. 2016, 31, 1107–1116. [Google Scholar] [CrossRef]
- Cai, X.; Wardlaw, T.; Brown, D.W. Global trends in exclusive breastfeeding. Int. Breastfeed J. 2012, 7, 12. [Google Scholar] [CrossRef]
- Thu, H.N.; Eriksson, B.; Khanh, T.T.; Petzold, M.; Bondjers, G.; Kim, C.N.; Thanh, L.N.; Ascher, H. Breastfeeding practices in urban and rural Vietnam. BMC Public Health 2012, 12, 964. [Google Scholar] [CrossRef] [PubMed]
- Hector, D.; King, L.; Webb, K.; Heywood, P. Factors affecting breastfeeding practices: Applying a conceptual framework. NSW Public Health Bull. 2005, 16, 52–55. [Google Scholar]
- Vinje, K.H.; Phan, L.T.H.; Nguyen, T.T.; Henjum, S.; Ribe, L.O.; Mathisen, R. Media audit reveals inappropriate promotion of products under the scope of the International Code of Marketing of Breast-milk Substitutes in South-East Asia. Public Health Nutr. 2017, 20, 1333–1342. [Google Scholar] [CrossRef] [PubMed]
- Robinson, H.; Buccini, G.; Curry, L.; Perez-Escamilla, R. The World Health Organization Code and exclusive breastfeeding in China, India, and Vietnam. Matern. Child. Nutr. 2018, 15, e12685. [Google Scholar] [CrossRef]
- The World Breastfeeding Trends Initiative. The World Breastfeeding Trends Initiative Vietnam Assessment Report 2015; International Baby Food Action Network (IBFAN): Delhi, India, 2015. [Google Scholar]
- Durako, S.J.; Thompson, M.; Diallo, M. Country Assessments of Breast-milk Substitutes (BMS) Companies’ Compliance with the International Code of Marketing of Breast-milk Substitutes. Final Vietnam Report; Westat: Rockville, MD, USA, 2016. [Google Scholar]
- Tuan, N.T.; Nguyen, P.H.; Hajeebhoy, N.; Frongillo, E.A. Gaps between breastfeeding awareness and practices in Vietnamese mothers result from inadequate support in health facilities and social norms. J. Nutr. 2014, 144, 1811–1817. [Google Scholar] [CrossRef][Green Version]
- Vietnam Ministry of Health; Vietnam Ministry of Labor—Invalids and Social Affairs. Annual Activities Report 2018; Vietnam Ministry of Health; Vietnam Ministry of Labor—Invalids and Social Affairs: Hanoi, Vietnam, 2019.
- Nguyen, P.H.; Keithly, S.C.; Nguyen, N.T.; Nguyen, T.T.; Tran, L.M.; Hajeebhoy, N. Prelacteal feeding practices in Vietnam: Challenges and associated factors. BMC Public Health 2013, 13, 932. [Google Scholar] [CrossRef]
- Giang, H.T.N.; Ulrich, S.; Tran, H.T.; Bechtold-Dalla Pozza, S. Monitoring and interventions are needed to reduce the very high Caesarean section rates in Vietnam. Acta. Paediatr. 2018, 107, 2109–2114. [Google Scholar] [CrossRef]
- Nguyen, P.T.H.; Binns, C.W.; Ha, A.V.V.; Nguyen, C.L.; Chu, T.K.; Duong, D.V.; Do, D.V.; Lee, A.H. Caesarean delivery associated with adverse breastfeeding practices: A prospective cohort study. J. Obstet. Gynaecol. 2019, 40, 644–648. [Google Scholar] [CrossRef]
- Nguyen, P.H.; Menon, P.; Ruel, M.; Hajeebhoy, N. A situational review of infant and young child feeding practices and interventions in Viet Nam. Asia Pac. J. Clin. Nutr. 2011, 20, 359–374. [Google Scholar]
- Ramoo, S.; Trinh, T.A.; Hirst, J.E.; Jeffery, H.E. Breastfeeding practices in a hospital-based study of Vietnamese women. Breastfeed. Med. 2014, 9, 479–485. [Google Scholar] [CrossRef]
- Lundberg, P.C.; Ngoc Thu, T.T. Breast-feeding attitudes and practices among Vietnamese mothers in Ho Chi Minh City. Midwifery 2012, 28, 252–257. [Google Scholar] [CrossRef]
- Almroth, S.; Arts, M.; Quang, N.D.; Hoa, P.T.; Williams, C. Exclusive breastfeeding in Vietnam: An attainable goal. Acta. Paediatr. 2008, 97, 1066–1069. [Google Scholar] [CrossRef] [PubMed]
- Joseph, J.; Liamputtong, P.; Brodribb, W. From Liminality to Vitality: Infant Feeding Beliefs Among Refugee Mothers From Vietnam and Myanmar. Qual. Health Res. 2019, 30, 1171–1182. [Google Scholar] [CrossRef] [PubMed]
- Inoue, M.; Binns, C.W. Introducing solid foods to infants in the Asia Pacific region. Nutrients 2014, 6, 276–288. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.A.; Binns, C.W.; Graham, K.I.; Oddy, W.H. Predictors of the early introduction of solid foods in infants: Results of a cohort study. BMC Pediatr. 2009, 9, 60. [Google Scholar] [CrossRef]
- Lundberg, P.C.; Trieu Thi Ngoc, T. Vietnamese women’s cultural beliefs and practices related to the postpartum period. Midwifery 2011, 27, 731–736. [Google Scholar] [CrossRef] [PubMed]
- Ngo, L.T.H.; Chou, H.F.; Gau, M.L.; Liu, C.Y. Breastfeeding self-efficacy and related factors in postpartum Vietnamese women. Midwifery 2019, 70, 84–91. [Google Scholar] [CrossRef]
- Nguyen, P.T.K.; Tran, H.T.; Thai, T.T.T.; Foster, K.; Roberts, C.L.; Marais, B.J. Factors associated with breastfeeding intent among mothers of newborn babies in Da Nang, Viet Nam. Int. Breastfeed. J. 2018, 13, 2. [Google Scholar] [CrossRef]
- Duong, D.V.; Binns, C.W.; Lee, A.H. Introduction of complementary food to infants within the first six months postpartum in rural Vietnam. Acta. Paediatr. 2005, 94, 1714–1720. [Google Scholar] [CrossRef]
- Murray, L.; Tran, T.; Thang, V.V.; Cass, L.; Fisher, J. How do caregivers understand and respond to unsettled infant behaviour in Vietnam? A qualitative study. Child Care Health Dev. 2018, 44, 62–70. [Google Scholar] [CrossRef]
- Menon, P.; Nguyen, P.H.; Saha, K.K.; Khaled, A.; Kennedy, A.; Tran, L.M.; Sanghvi, T.; Hajeebhoy, N.; Baker, J.; Alayon, S. Impacts on breastfeeding practices of at-scale strategies that combine intensive interpersonal counseling, mass media, and community mobilization: Results of cluster-randomized program evaluations in Bangladesh and Viet Nam. PLoS Med. 2016, 13, e1002159. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, P.H.; Kim, S.S.; Nguyen, T.T.; Hajeebhoy, N.; Tran, L.M.; Alayon, S.; Ruel, M.T.; Rawat, R.; Frongillo, E.A.; Menon, P. Exposure to mass media and interpersonal counseling has additive effects on exclusive breastfeeding and its psychosocial determinants among Vietnamese mothers. Matern. Child Nutr. 2016, 12, 713–725. [Google Scholar] [CrossRef] [PubMed]
- Bich, T.H.; Long, T.K.; Hoa, D.P. Community-based father education intervention on breastfeeding practice-Results of a quasi-experimental study. Matern. Child Nutr. 2019, 15 (Suppl. 1), e12705. [Google Scholar] [CrossRef]
- Bich, T.H.; Hoa, D.T.; Ha, N.T.; le Vui, T.; Nghia, D.T.; Malqvist, M. Father’s involvement and its effect on early breastfeeding practices in Viet Nam. Matern. Child Nutr. 2016, 12, 768–777. [Google Scholar] [CrossRef] [PubMed]
- Bich, T.H.; Hoa, D.T.; Malqvist, M. Fathers as supporters for improved exclusive breastfeeding in Viet Nam. Matern. Child Health J. 2014, 18, 1444–1453. [Google Scholar] [CrossRef] [PubMed]
- Aiga, H.; Nguyen, V.D.; Nguyen, C.D.; Nguyen, T.T.; Nguyen, L.T. Knowledge, attitude and practices: Assessing maternal and child health care handbook intervention in Vietnam. BMC Public Health 2016, 16, 129. [Google Scholar] [CrossRef]
- Executive, Board. mHealth: Use of Appropriate Digital Technologies for Public Health: Report by the Director-General; World Health Organization: Geneva, Switzerland, 2017.
- McFadden, A.; Gavine, A.; Renfrew, M.J.; Wade, A.; Buchanan, P.; Taylor, J.L.; Veitch, E.; Rennie, A.M.; Crowther, S.A.; Neiman, S.; et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst. Rev. 2017, 5, CD001141. [Google Scholar] [CrossRef]
- Skouteris, H.; Bailey, C.; Nagle, C.; Hauck, Y.; Bruce, L.; Morris, H. Interventions Designed to Promote Exclusive Breastfeeding in High-Income Countries: A Systematic Review Update. Breastfeed. Med. 2017, 12, 604–614. [Google Scholar] [CrossRef]
- Chen, H.; Chai, Y.; Dong, L.; Niu, W.; Zhang, P. Effectiveness and Appropriateness of mHealth Interventions for Maternal and Child Health: Systematic Review. JMIR Mhealth Uhealth 2018, 6, e7. [Google Scholar] [CrossRef]
- Lau, Y.; Htun, T.P.; Tam, W.S.; Klainin-Yobas, P. Efficacy of e-technologies in improving breastfeeding outcomes among perinatal women: A meta-analysis. Matern. Child Nutr. 2016, 12, 381–401. [Google Scholar] [CrossRef]
- Lee, S.H.; Nurmatov, U.B.; Nwaru, B.I.; Mukherjee, M.; Grant, L.; Pagliari, C. Effectiveness of mHealth interventions for maternal, newborn and child health in low- and middle-income countries: Systematic review and meta-analysis. J. Glob. Health 2016, 6, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Efrat, M.W.; Esparza, S.; Mendelson, S.G.; Lane, C.J. The effect of lactation educators implementing a telephone-based intervention among low-income Hispanics: A randomised trial. Health Educ. J. 2015, 74, 424–441. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.; Zhu, Y.; Zhang, Z.; Wan, H. Effectiveness of a theory-based breastfeeding promotion intervention on exclusive breastfeeding in China: A randomised controlled trial. Midwifery 2016, 42, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Li, M.; Wen, L.M.; Hu, Q.; Yang, D.; He, G.; Baur, L.A.; Dibley, M.J.; Qian, X. Effect of short message service on infant feeding practice: Findings from a community-based study in Shanghai, China. JAMA Pediatr. 2014, 168, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Giglia, R.; Cox, K.; Zhao, Y.; Binns, C.W. Exclusive breastfeeding increased by an internet intervention. Breastfeed. Med. 2015, 10, 20–25. [Google Scholar] [CrossRef]
- Flax, V.L.; Negerie, M.; Ibrahim, A.U.; Leatherman, S.; Daza, E.J.; Bentley, M.E. Integrating group counseling, cell phone messaging, and participant-generated songs and dramas into a microcredit program increases Nigerian women’s adherence to international breastfeeding recommendations. J. Nutr. 2014, 144, 1120–1124. [Google Scholar] [CrossRef]
- White, B.K.; Martin, A.; White, J.A.; Burns, S.K.; Maycock, B.R.; Giglia, R.C.; Scott, J.A. Theory-Based Design and Development of a Socially Connected, Gamified Mobile App for Men About Breastfeeding (Milk Man). JMIR Mhealth Uhealth 2016, 4, e81. [Google Scholar] [CrossRef]
- Wang, C.J.; Chaovalit, P.; Pongnumkul, S. A Breastfeed-Promoting Mobile App Intervention: Usability and Usefulness Study. JMIR Mhealth Uhealth 2018, 6, e27. [Google Scholar] [CrossRef]
- Taki, S.; Campbell, K.J.; Russell, C.G.; Elliott, R.; Laws, R.; Denney-Wilson, E. Infant Feeding Websites and Apps: A Systematic Assessment of Quality and Content. Interact. J. Med. Res. 2015, 4, e18. [Google Scholar] [CrossRef]
- McKay, F.H.; Cheng, C.; Wright, A.; Shill, J.; Stephens, H.; Uccellini, M. Evaluating mobile phone applications for health behaviour change: A systematic review. J. Telemed. Telecare 2016, 24, 22–30. [Google Scholar] [CrossRef]
- Wheaton, N.; Lenehan, J.; Amir, L.H. Evaluation of a Breastfeeding App in Rural Australia: Prospective Cohort Study. J. Hum. Lact. 2018, 34, 711–720. [Google Scholar] [CrossRef]
- Laws, R.A.; Denney-Wilson, E.A.; Taki, S.; Russell, C.G.; Zheng, M.; Litterbach, E.K.; Ong, K.L.; Lymer, S.J.; Elliott, R.; Campbell, K.J. Key Lessons and Impact of the Growing Healthy mHealth Program on Milk Feeding, Timing of Introduction of Solids, and Infant Growth: Quasi-Experimental Study. JMIR Mhealth Uhealth 2018, 6, e78. [Google Scholar] [CrossRef] [PubMed]
- Maycock, B.R.; Scott, J.A.; Hauck, Y.L.; Burns, S.K.; Robinson, S.; Giglia, R.; Jorgensen, A.; White, B.; Harries, A.; Dhaliwal, S.; et al. A study to prolong breastfeeding duration: Design and rationale of the Parent Infant Feeding Initiative (PIFI) randomised controlled trial. BMC Pregnancy Childbirth 2015, 15, 159. [Google Scholar] [CrossRef] [PubMed]
- Maycock, B.; Binns, C.W.; Dhaliwal, S.; Tohotoa, J.; Hauck, Y.; Burns, S.; Howat, P. Education and support for fathers improves breastfeeding rates: A randomized controlled trial. J. Hum. Lact 2013, 29, 484–490. [Google Scholar] [CrossRef] [PubMed]
- White, B.K.; Giglia, R.C.; Scott, J.A.; Burns, S.K. How New and Expecting Fathers Engage With an App-Based Online Forum: Qualitative Analysis. JMIR Mhealth Uhealth 2018, 6, e144. [Google Scholar] [CrossRef] [PubMed]
- Friedman, L.B.; Silva, M.; Smith, K. A Focus Group Study Observing Maternal Intention to Use a WIC Education App. Am. J. Health Behav. 2018, 42, 110–123. [Google Scholar] [CrossRef]
- Demirci, J.; Caplan, E.; Murray, N.; Cohen, S. “I Just Want to Do Everything Right:” Primiparous Women’s Accounts of Early Breastfeeding via an App-Based Diary. J. Pediatr. Health Care 2018, 32, 163–172. [Google Scholar] [CrossRef]
- Demirci, J.R.; Bogen, D.L. Feasibility and acceptability of a mobile app in an ecological momentary assessment of early breastfeeding. Matern. Child Nutr. 2017, 13, e12342. [Google Scholar] [CrossRef]
- Coughlin, S.S. The need for research-tested smartphone applications for promoting breastfeeding. mHealth 2016, 2, 18. [Google Scholar] [CrossRef]
- White, B.K.; Burns, S.K.; Giglia, R.C.; Scott, J.A. Designing evaluation plans for health promotion mHealth interventions: A case study of the Milk Man mobile app. Health Promot. J. Austr. 2016, 27, 198–203. [Google Scholar] [CrossRef]
- National Institute of Nutrition Mặt trời bé thơ (The little sun). Available online: http://mattroibetho.vn/vi/mat-troi-be-tho.nl47.bic (accessed on 7 May 2020).
- Zhang, M.W.; Tran, B.X.; Le, H.T.; Nguyen, H.D.; Nguyen, C.T.; Tran, T.D.; Latkin, C.A.; Ho, R.C. Perceptions of Health-Related Information on Facebook: Cross-Sectional Study Among Vietnamese Youths. Interact. J. Med. Res. 2017, 6, e16. [Google Scholar] [CrossRef]
- Grant, S.; Mayo-Wilson, E.; Montgomery, P.; Macdonald, G.; Michie, S.; Hopewell, S.; Moher, D. CONSORT-SPI 2018 Explanation and Elaboration: Guidance for reporting social and psychological intervention trials. Trials 2018, 19, 406. [Google Scholar] [CrossRef]
- Vietnam General Statistics Office. The 1/4/2017 Time-Point Population Change and Family Planning Survey; Vietnam General Statistics Office: Hanoi, Vietnam, 2018.
- The National Institute of Nutrition. The National Nutrition Surveillance System, Hanoi Report 2012–2014; The National Institute of Nutrition: Hanoi, Vietnam, 2014.
- The Nielsen Company. Nielsen Vietnam Smartphone Insights Report 2017; The Nielsen company: Ho Chi Minh, Vietnam, 2017. [Google Scholar]
- Johnston, M.; Landers, S.; Noble, L.; Szucs, K.; Viehmann, L. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar]
- World Health Organization. Acceptable Medical Reasons for Use of Breastmilk Substitutes; WHO: Geneva, Switzerland, 2009. Available online: https://www.who.int/nutrition/publications/infantfeeding/WHO_NMH_NHD_09.01/en/ (accessed on 29 November 2019).
- Lee, Y.; Moon, M. Utilization and Content Evaluation of Mobile Applications for Pregnancy, Birth, and Child Care. Healthc. Inform. Res. 2016, 22, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Zapata, B.C.; Fernandez-Aleman, J.L.; Idri, A.; Toval, A. Empirical studies on usability of mHealth apps: A systematic literature review. J. Med. Syst. 2015, 39, 1. [Google Scholar] [CrossRef] [PubMed]
- Denney-Wilson, E.; Laws, R.; Russell, C.G.; Ong, K.-l.; Taki, S.; Elliot, R.; Azadi, L.; Lymer, S.; Taylor, R.; Lynch, J. Preventing obesity in infants: The growing healthy feasibility trial protocol. BMJ Open 2015, 5, e009258. [Google Scholar] [CrossRef] [PubMed]
- Sanghvi, T.; Jimerson, A.; Hajeebhoy, N.; Zewale, M.; Nguyen, G.H. Tailoring Communication Strategies to Improve Infant and Young Child Feeding Practices in Different Country Settings. Food Nutr. Bull. 2013, 34 (Suppl. 2), S169–S180. [Google Scholar] [CrossRef] [PubMed]
- Dobson, R.; Whittaker, R.; Bartley, H.; Connor, A.; Chen, R.; Ross, M.; McCool, J. Development of a Culturally Tailored Text Message Maternal Health Program: TextMATCH. JMIR Mhealth Uhealth 2017, 5, e49. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- Scott, J.A.; Binns, C.W.; Graham, K.I.; Oddy, W.H. Temporal changes in the determinants of breastfeeding initiation. Birth 2006, 33, 37–45. [Google Scholar] [CrossRef]
- Scott, J.A.; Kwok, Y.Y.; Synnott, K.; Bogue, J.; Amarri, S.; Norin, E.; Gil, A.; Edwards, C.A. A comparison of maternal attitudes to breastfeeding in public and the association with breastfeeding duration in four European countries: Results of a cohort study. Birth 2015, 42, 78–85. [Google Scholar] [CrossRef]
- Binns, C.; Lee, M.K.; Kagawa, M.; Low, W.Y.; Scott, J.; Lee, A.; Zerfas, A.; Maycock, B.; Qiu, L.; Yusuff, A.; et al. Infant Feeding Guidelines for the Asia Pacific Region. Asia Pac. J. Public Health 2018, 40, 682–690. [Google Scholar] [CrossRef] [PubMed]
- Binns, C.W.; Fraser, M.L.; Lee, A.H.; Scott, J. Defining exclusive breastfeeding in Australia. J. Paediatr. Child. Health 2009, 45, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Khanal, V.; Lee, A.H.; Scott, J.A.; Karkee, R.; Binns, C.W. Implications of methodological differences in measuring the rates of exclusive breastfeeding in Nepal: Findings from literature review and cohort study. BMC Pregnancy Childbirth 2016, 16, 389. [Google Scholar] [CrossRef] [PubMed]
- ClinCalc. Kane SP Sample Size Calculator. Available online: https://clincalc.com/stats/samplesize.aspx (accessed on 16 July 2020).
- Zhong, B. How to calculate sample size in randomized controlled trial? J. Thorac. Dis. 2009, 1, 51–54. [Google Scholar] [PubMed]
- Dettori, J.R. Loss to follow-up. Evid. Cased Spine Care J. 2011, 2, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Matts, J.P.; Lachin, J.M. Properties of permuted-block randomization in clinical trials. Control. Clin. Trials. 1988, 9, 327–344. [Google Scholar] [CrossRef]
- Broglio, K. Randomization in Clinical Trials: Permuted Blocks and Stratification. JAMA 2018, 319, 2223–2224. [Google Scholar] [CrossRef]
- Alzaheb, R.A. A Review of the Factors Associated With the Timely Initiation of Breastfeeding and Exclusive Breastfeeding in the Middle East. Clin. Med. Insights Pediatr. 2017, 11, 1179556517748912. [Google Scholar] [CrossRef]
- Cohen, S.S.; Alexander, D.D.; Krebs, N.F.; Young, B.E.; Cabana, M.D.; Erdmann, P.; Hays, N.P.; Bezold, C.P.; Levin-Sparenberg, E.; Turini, M.; et al. Factors Associated with Breastfeeding Initiation and Continuation: A Meta-Analysis. J. Pediatr. 2018, 203, 190–196 e121. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Binns, C.W.; Lee, M.K. Public Health Impact of Breastfeeding. In Encyclopaedia of Global Public Health; McQueen, D., Ed.; Oxford University Press: New York, NY, USA, 2019; pp. 1–46. Available online: https://oxfordre.com/publichealth/view/10.1093/acrefore/9780190632366.001.0001/acrefore-9780190632366-e-66?rskey=R3HoVj&result=1 (accessed on 7 June 2020).
- Binns, C.; Lee, M.K.; Low, W.Y.; Zerfas, A. The Role of Public Health Nutrition in Achieving the Sustainable Development Goals in the Asia Pacific Region. Asia Pac. J. Public Health 2017, 29, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Baker, P.; Smith, J.; Salmon, L.; Friel, S.; Kent, G.; Iellamo, A.; Dadhich, J.P.; Renfrew, M.J. Global trends and patterns of commercial milk-based formula sales: Is an unprecedented infant and young child feeding transition underway? Public Health Nutr. 2016, 19, 2540–2550. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.P. “Lost Milk?” Counting the Economic Value of Breast Milk in Gross Domestic Product. J. Hum. Lact. 2013, 29, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Kemp, S. Digital 2020: Vietnam. Available online: https://datareportal.com/reports/digital-2020-vietnam (accessed on 7 June 2020).
- Daly, L.M.; Horey, D.; Middleton, P.F.; Boyle, F.M.; Flenady, V. The Effect of Mobile App Interventions on Influencing Healthy Maternal Behavior and Improving Perinatal Health Outcomes: Systematic Review. JMIR Mhealth Uhealth 2018, 6, e10012. [Google Scholar] [CrossRef]
- Canner, P.L. Covariate adjustment of treatment effects in clinical trials. Control. Clin. Trials 1991, 12, 359–366. [Google Scholar] [CrossRef]
- Hernandez, A.V.; Steyerberg, E.W.; Habbema, J.D. Covariate adjustment in randomized controlled trials with dichotomous outcomes increases statistical power and reduces sample size requirements. J. Clin. Epidemiol. 2004, 57, 454–460. [Google Scholar] [CrossRef]
- Gamble, C.; Krishan, A.; Stocken, D.; Lewis, S.; Juszczak, E.; Dore, C.; Williamson, P.R.; Altman, D.G.; Montgomery, A.; Lim, P.; et al. Guidelines for the Content of Statistical Analysis Plans in Clinical Trials. JAMA 2017, 318, 2337–2343. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gotzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c869. [Google Scholar] [CrossRef]
- Akl, E.A.; Briel, M.; You, J.J.; Sun, X.; Johnston, B.C.; Busse, J.W.; Mulla, S.; Lamontagne, F.; Bassler, D.; Vera, C. Potential impact on estimated treatment effects of information lost to follow-up in randomised controlled trials (LOST-IT): Systematic review. BMJ 2012, 344, e2809. [Google Scholar] [CrossRef] [PubMed]
- Hellard, M.E.; Sinclair, M.I.; Forbes, A.B.; Fairley, C.K. Methods used to maintain a high level of participant involvement in a clinical trial. J. Epidemiol. Community Health 2001, 55, 348–351. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bower, P.; Brueton, V.; Gamble, C.; Treweek, S.; Smith, C.T.; Young, B.; Williamson, P. Interventions to improve recruitment and retention in clinical trials: A survey and workshop to assess current practice and future priorities. Trials 2014, 15, 399. [Google Scholar] [CrossRef] [PubMed]
- Abshire, M.; Dinglas, V.D.; Cajita, M.I.; Eakin, M.N.; Needham, D.M.; Himmelfarb, C.D. Participant retention practices in longitudinal clinical research studies with high retention rates. BMC Med. Res. Methodol. 2017, 17, 30. [Google Scholar] [CrossRef] [PubMed]
- National Research Council; Panel on Handling Missing Data in Clinical Trials; Committee on National Statistics; Division of Behavioral and Social Sciences and Education. The Prevention and Treatment of Missing Data in Clinical Trials; National Academies Press: Washington, DC, USA, 2010.
- European Medicines Agency Committee for Medicinal Products for Human Use (CHMP). Guideline on Missing Data in Confirmatory Clinical Trials EMA/CPMP/EWP/1776/99 Rev. 1; EMA: Brussels, Belgium, 2010. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doan, T.T.D.; Binns, C.; Pham, N.M.; Zhao, Y.; Dinh, T.P.H.; Bui, T.T.H.; Tran, T.C.; Nguyen, X.H.; Giglia, R.; Xu, F.; et al. Improving Breastfeeding by Empowering Mothers in Vietnam: A Randomised Controlled Trial of a Mobile App. Int. J. Environ. Res. Public Health 2020, 17, 5552. https://doi.org/10.3390/ijerph17155552
Doan TTD, Binns C, Pham NM, Zhao Y, Dinh TPH, Bui TTH, Tran TC, Nguyen XH, Giglia R, Xu F, et al. Improving Breastfeeding by Empowering Mothers in Vietnam: A Randomised Controlled Trial of a Mobile App. International Journal of Environmental Research and Public Health. 2020; 17(15):5552. https://doi.org/10.3390/ijerph17155552
Chicago/Turabian StyleDoan, Thi Thuy Duong, Colin Binns, Ngoc Minh Pham, Yun Zhao, Thi Phuong Hoa Dinh, Thi Thu Ha Bui, Trung Chuyen Tran, Xuan Hoai Nguyen, Roslyn Giglia, Fenglian Xu, and et al. 2020. "Improving Breastfeeding by Empowering Mothers in Vietnam: A Randomised Controlled Trial of a Mobile App" International Journal of Environmental Research and Public Health 17, no. 15: 5552. https://doi.org/10.3390/ijerph17155552
APA StyleDoan, T. T. D., Binns, C., Pham, N. M., Zhao, Y., Dinh, T. P. H., Bui, T. T. H., Tran, T. C., Nguyen, X. H., Giglia, R., Xu, F., & Lee, A. (2020). Improving Breastfeeding by Empowering Mothers in Vietnam: A Randomised Controlled Trial of a Mobile App. International Journal of Environmental Research and Public Health, 17(15), 5552. https://doi.org/10.3390/ijerph17155552





