Correlation between COVID-19 Morbidity and Mortality Rates in Japan and Local Population Density, Temperature, and Absolute Humidity
Abstract
1. Introduction
2. Material and Methods
2.1. Data Source
2.2. Statistical Analysis
3. Results
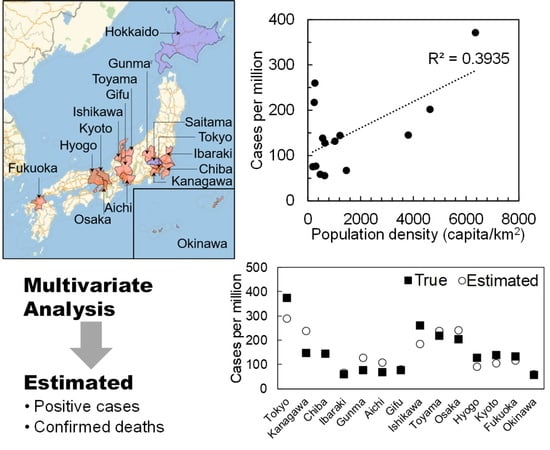
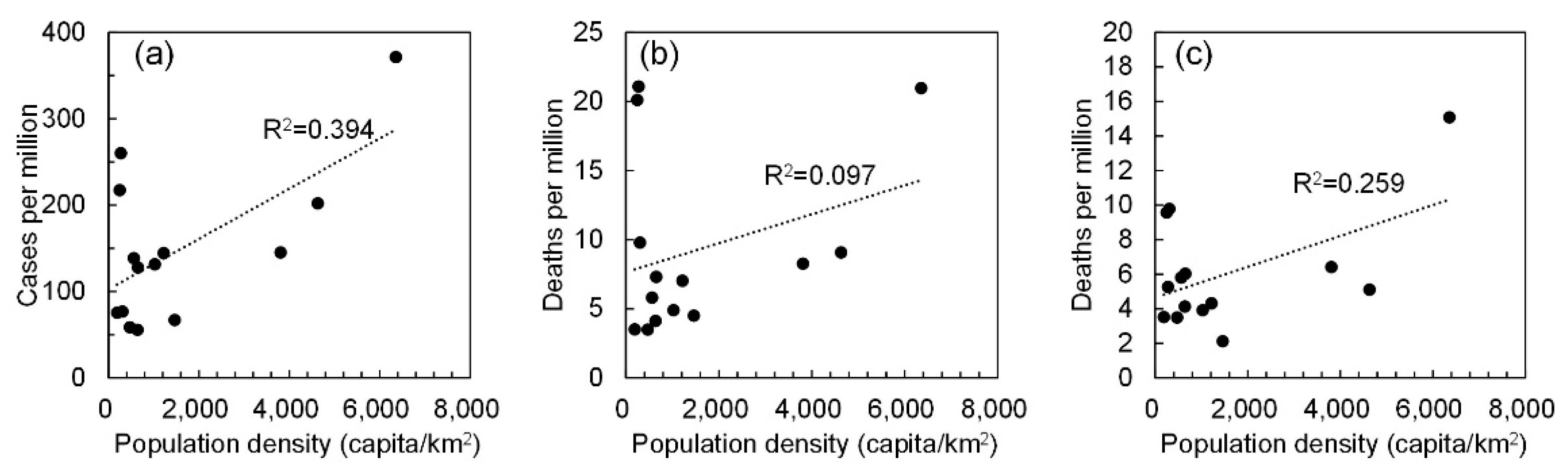
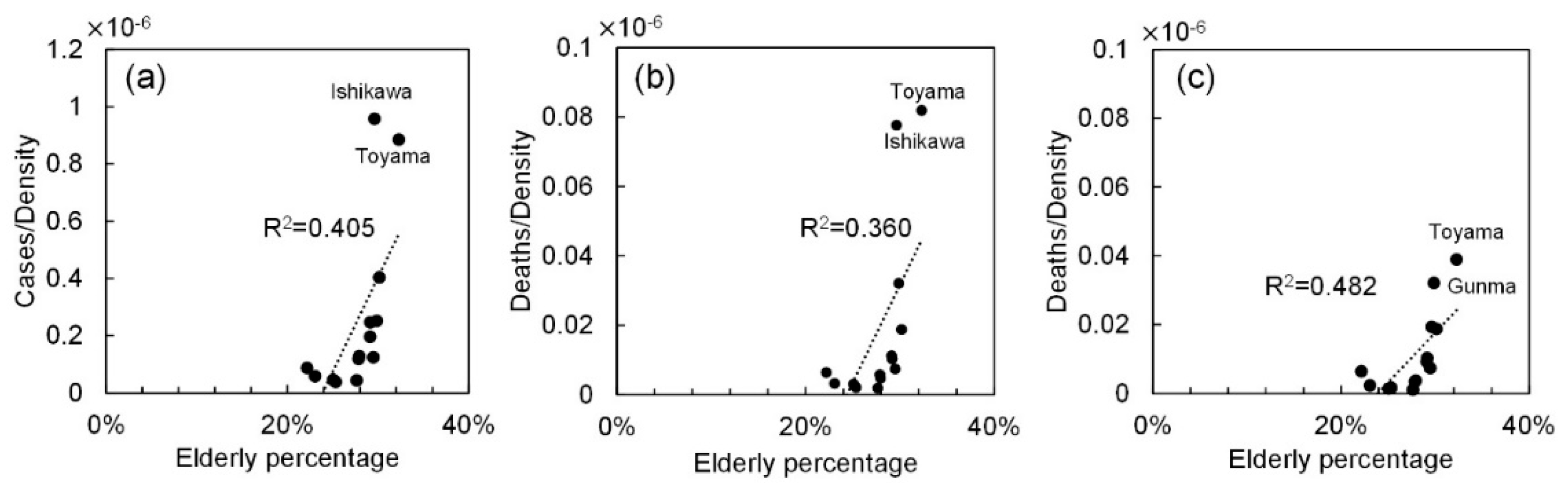
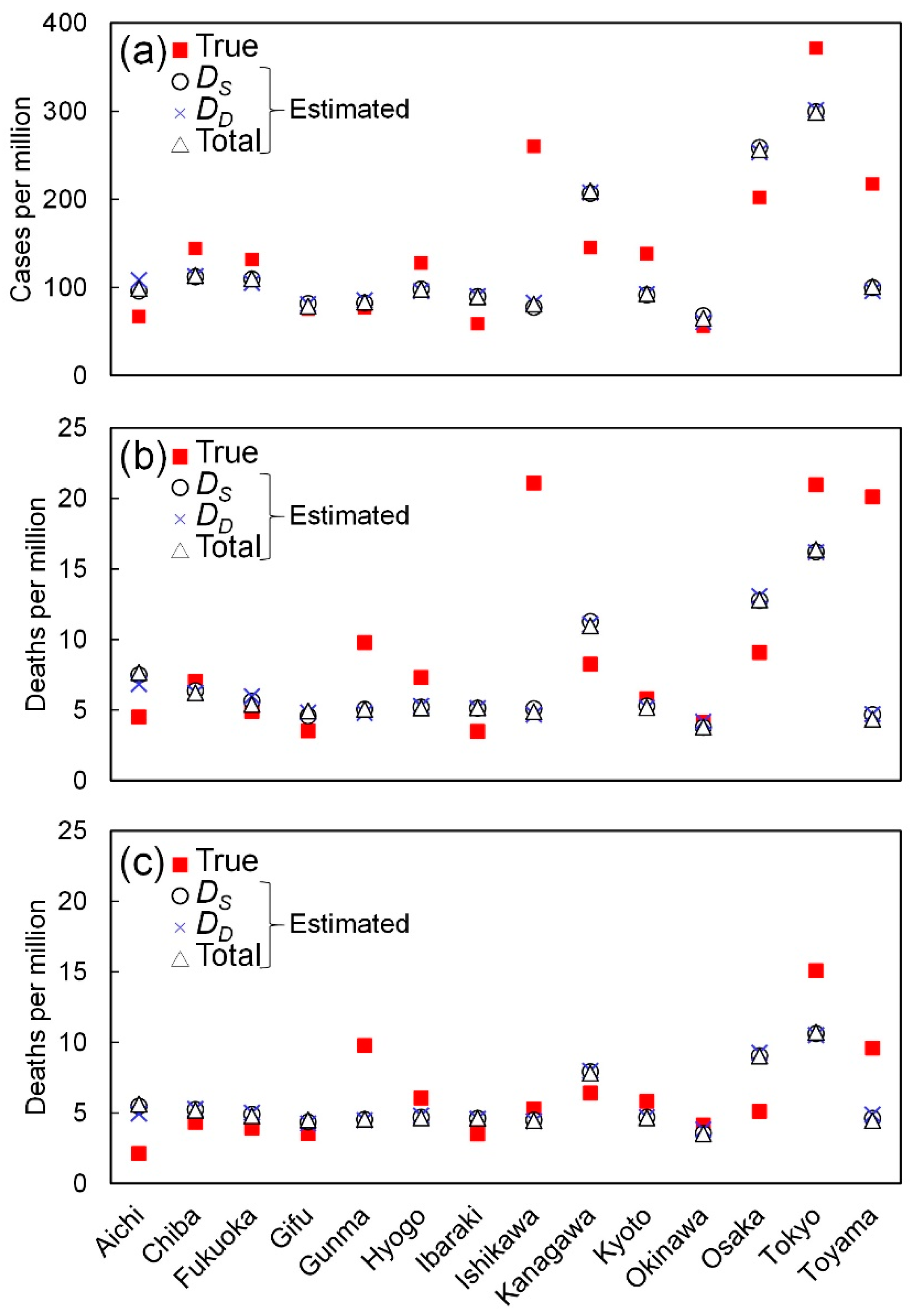
3.1. Effect of Population Density and Elderly Population
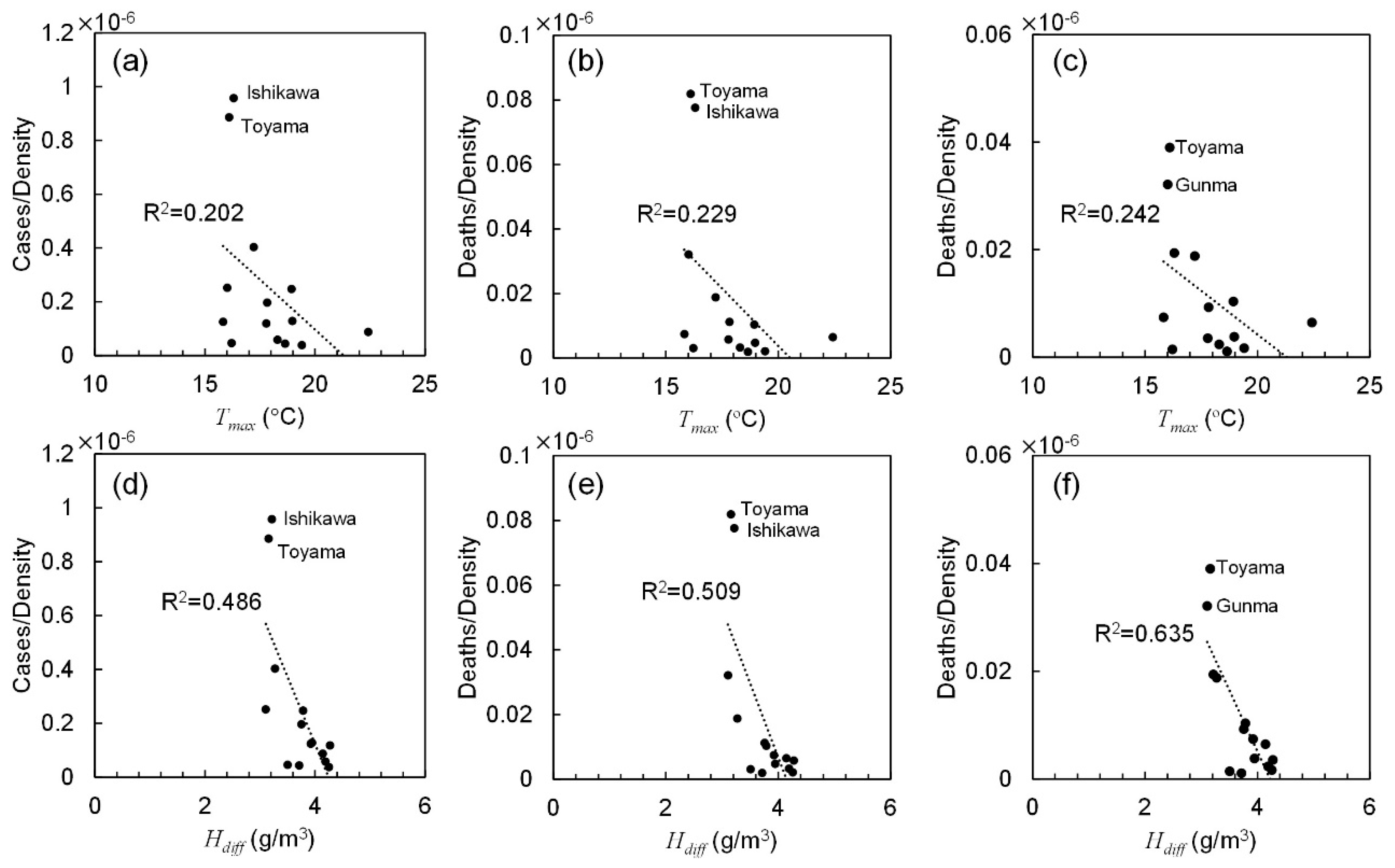
3.2. Effect of Ambient Conditions
3.3. Multivariate Linear Regression
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Jama 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report 72; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Roser, M.; Ritchie, H.; Ortiz-Ospina, E.; Hasell, J. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/coronavirus#coronavirus-country-profiles (accessed on 29 June 2020).
- Ai, T.; Yang, Z.; Hou, H.; Zhan, C.; Chen, C.; Lv, W.; Tao, Q.; Sun, Z.; Xia, L. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology 2020, 296, E32–E40. [Google Scholar] [CrossRef] [PubMed]
- Repici, A.; Maselli, R.; Colombo, M.; Gabbiadini, R.; Spadaccini, M.; Anderloni, A.; Carrara, S.; Fugazza, A.; Di Leo, M.; Galtieri, P.A. Coronavirus (COVID-19) outbreak: What the department of endoscopy should know. Gastrointest. Endosc. 2020, 92, 192–197. [Google Scholar] [CrossRef]
- CDC. Coronavirus Disease 2019 (COVID-19): How COVID-19 Spreads. Available online: https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html (accessed on 25 July 2020).
- Bahl, P.; Doolan, C.; de Silva, C.; Chughtai, A.A.; Bourouiba, L.; MacIntyre, C.R. Airborne or droplet precautions for health workers treating COVID-19? J. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Ma, Y.; Zhao, Y.; Liu, J.; He, X.; Wang, B.; Fu, S.; Yan, J.; Niu, J.; Zhou, J.; Luo, B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020, 724, 138226. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Tang, K.; Feng, K.; Lv, W. High temperature and high humidity reduce the transmission of COVID-19. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3551767 (accessed on 29 July 2020).
- Tosepu, R.; Gunawan, J.; Effendy, D.S.; Lestari, H.; Bahar, H.; Asfian, P. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020, 725, 138436. [Google Scholar] [CrossRef]
- Ogen, Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to the coronavirus (COVID-19) fatality rate. Sci. Total Environ. 2020, 726, 138605. [Google Scholar] [CrossRef]
- Xie, J.; Zhu, Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020, 724, 138201. [Google Scholar] [CrossRef]
- Liu, J.; Zhou, J.; Yao, J.; Zhang, X.; Li, L.; Xu, X.; He, X.; Wang, B.; Fu, S.; Niu, T. Impact of meteorological factors on the COVID-19 transmission: A multi-city study in China. Sci. Total Environ. 2020, 726, 138513. [Google Scholar] [CrossRef]
- Tomar, A.; Gupta, N. Prediction for the spread of COVID-19 in India and effectiveness of preventive measures. Sci. Total Environ. 2020, 728, 138762. [Google Scholar] [CrossRef]
- Yao, Y.; Pan, J.; Liu, Z.; Meng, X.; Wang, W.; Kan, H.; Wang, W. No Association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020, 55, 2000517. [Google Scholar] [CrossRef]
- Briz-Redón, Á.; Serrano-Aroca, Á. A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci. Total Environ. 2020, 728, 138811. [Google Scholar] [CrossRef] [PubMed]
- Pirouz, B.; Shaffiee Haghshenas, S.; Pirouz, B.; Shaffiee Haghshenas, S.; Piro, P. Development of an assessment method for investigating the impact of climate and urban parameters in confirmed cases of covid-19: A new challenge in sustainable development. Int. J. Environ. Res. Public Health 2020, 17, 2801. [Google Scholar] [CrossRef] [PubMed]
- Shaffiee Haghshenas, S.; Pirouz, B.; Shaffiee Haghshenas, S.; Pirouz, B.; Piro, P.; Na, K.-S.; Cho, S.-E.; Geem, Z.W. Prioritizing and Analyzing the Role of Climate and Urban Parameters in the Confirmed Cases of COVID-19 Based on Artificial Intelligence Applications. Int. J. Environ. Res. Public Health 2020, 17, 3730. [Google Scholar] [CrossRef]
- Menebo, M.M. Temperature and precipitation associate with Covid-19 new daily cases: A correlation study between weather and Covid-19 pandemic in Oslo, Norway. Sci. Total Environ. 2020, 737, 139659. [Google Scholar] [CrossRef] [PubMed]
- Auler, A.; Cássaro, F.; da Silva, V.; Pires, L. Evidence that high temperatures and intermediate relative humidity might favor the spread of COVID-19 in tropical climate: A case study for the most affected Brazilian cities. Sci. Total Environ. 2020, 737, 139090. [Google Scholar] [CrossRef]
- Prata, D.N.; Rodrigues, W.; Bermejo, P.H. Temperature significantly changes COVID-19 transmission in (sub) tropical cities of Brazil. Sci. Total Environ. 2020, 729, 138862. [Google Scholar] [CrossRef]
- Park, J.E.; Son, W.S.; Ryu, Y.; Choi, S.B.; Kwon, O.; Ahn, I. Effects of temperature, humidity, and diurnal temperature range on influenza incidence in a temperate region. Influ. Other Respir. Viruses 2020, 14, 11–18. [Google Scholar] [CrossRef]
- Shimmei, K.; Nakamura, T.; Ng, C.F.S.; Hashizume, M.; Murakami, Y.; Maruyama, A.; Misaki, T.; Okabe, N.; Nishiwaki, Y. Association Between Seasonal Influenza and Absolute Humidity: Time-Series Analysis with Daily Surveillance Data in Japan. Sci. Rep. 2020, 10, 1–7. [Google Scholar] [CrossRef]
- Wu, Y.; Jing, W.; Liu, J.; Ma, Q.; Yuan, J.; Wang, Y.; Du, M.; Liu, M. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020, 729, 139051. [Google Scholar] [CrossRef]
- Huang, Z.; Huang, J.; Gu, Q.; Du, P.; Liang, H.; Dong, Q. Optimal temperature zone for the dispersal of COVID-19. Sci. Total Environ. 2020, 736, 139487. [Google Scholar] [CrossRef] [PubMed]
- Oliveiros, B.; Caramelo, L.; Ferreira, N.C.; Caramelo, F. Role of temperature and humidity in the modulation of the doubling time of COVID-19 cases. MedRxiv 2020. [Google Scholar] [CrossRef]
- Hu, H.; Nigmatulina, K.; Eckhoff, P. The scaling of contact rates with population density for the infectious disease models. Math. Biosci. 2013, 244, 125–134. [Google Scholar] [CrossRef]
- e-Stat. Statistics of Japan. Available online: https://www.e-stat.go.jp/en/ (accessed on 2 July 2020).
- Rashed, E.A.; Kodera, S.; Gomez-Tames, J.; Hirata, A. Influence of absolute humidity, temperature and population density on COVID-19 spread and decay durations: Multi-prefecture study in Japan. Int. J. Environ. Res. Public Health 2020, 17, 5354. [Google Scholar] [CrossRef]
- Statistics Bureau of Japan. Population Estimates. Available online: https://www.stat.go.jp/index.html (accessed on 2 June 2020).
- Toyo Keizai Online. Coronavirus Disease (COVID-19) Situation Report in Japan. Available online: https://toyokeizai.net/sp/visual/tko/covid19/en.html (accessed on 31 May 2020).
- Ministry of Health Labour and Welfare. About Coronavirus Disease 2019 (COVID-19). Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/newpage_00032.html (accessed on 26 May 2020).
- Japan Meteorological Agency Weather/Earthquake. Available online: https://www.jma.go.jp/jma/indexe.html (accessed on 29 May 2020).
- Rencher, A.C. Methods of Multivariate Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2003; Volume 492. [Google Scholar]
- Metz, J.A.; Finn, A. Influenza and humidity–Why a bit more damp may be good for you! J. Infect. 2015, 71, S54–S58. [Google Scholar] [CrossRef]
- Alin, A. Multicollinearity. Wiley Interdiscip. Rev. Comput. Stat. 2010, 2, 370–374. [Google Scholar] [CrossRef]
- Daley, D.J.; Gani, J. Epidemic Modelling: An Introduction; Cambridge University Press: Cambridge, UK, 2001; Volume 15. [Google Scholar]
- Singh, R.; Adhikari, R. Age-structured impact of social distancing on the COVID-19 epidemic in India. Available online: https://arxiv.org/abs/2003.12055 (accessed on 29 July 2020).
- Ministry of Health Labour and Welfare. Pandemic Influenza and Avian Influenza. Available online: https://www.mhlw.go.jp/english/topics/influenza/ (accessed on 4 July 2020).

| Prefectures | Population (×1000) | Density (capita/km2) | Total Cases | Confirmed Deaths | Confirmed Deaths (Ex.) † | Cases/1M | Elderly (>65 years) (%) |
|---|---|---|---|---|---|---|---|
| Aichi | 7552 | 1460.0 | 507 | 34 | 16 | 67.1 | 25.1 |
| Chiba | 6259 | 1217.4 | 904 | 44 | 27 | 144.4 | 27.8 |
| Fukuoka | 5104 | 1024.8 | 672 | 25 | 20 | 131.7 | 27.9 |
| Gifu | 1987 | 187.3 | 150 | 7 | 7 | 75.5 | 30.1 |
| Gunma | 1942 | 304.6 | 149 | 19 | 19 | 76.7 | 29.9 |
| Hyogo | 5466 | 650.4 | 699 | 40 | 33 | 127.9 | 29.1 |
| Ibaraki | 2860 | 470.4 | 168 | 10 | 10 | 58.7 | 29.5 |
| Ishikawa | 1138 | 271.7 | 296 | 24 | 6 | 260.1 | 29.6 |
| Kanagawa | 9198 | 3807.5 | 1336 | 76 | 59 | 145.2 | 25.3 |
| Kyoto | 2583 | 560.1 | 358 | 15 | 15 | 138.6 | 29.2 |
| Okinawa | 1453 | 637.5 | 81 | 6 | 6 | 55.7 | 22.2 |
| Osaka | 8809 | 4631.0 | 1781 | 80 | 45 | 202.2 | 27.6 |
| Tokyo | 13,921 | 6354.8 | 5170 | 292 | 210 | 371.4 | 23.1 |
| Toyama | 1044 | 245.6 | 227 | 21 | 10 | 217.4 | 32.3 |
| Prefectures | Spread Stage | Decay Stage | ||
|---|---|---|---|---|
| TSS | TSE | TDS | TDE | |
| Aichi | 22-February | 30-March | 1-April | 27-April |
| Chiba | 19-March | 2-April | 13-April | 5-May |
| Fukuoka | 22-March | 1-April | 9-April | 27-April |
| Gifu | 25-March | 4-April | 6-April | 17-April |
| Gunma | 25-March | 5-April | 9-April | 22-April |
| Hyogo | 19-March | 4-April | 7-April | 4-May |
| Ibaraki | 16-March | 28-March | 8-April | 23-April |
| Ishikawa | 24-March | 3-April | 8-April | 8-May |
| Kanagawa | 19-March | 3-April | 11-April | 19-May |
| Kyoto | 16-March | 2-April | 5-April | 9-May |
| Okinawa | 28-March | 3-April | 10-April | 25-April |
| Osaka | 18-March | 6-April | 13-April | 6-May |
| Tokyo | 17-March | 3-April | 10-April | 7-May |
| Toyama | 1-April | 13-April | 18-April | 30-April |
| Spread Duration (DS) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Prefectures | Tave | Tmax | Tmin | Tdiff | Have | Hmax | Hmin | Hdiff | Vair | DL |
| Aichi | 10.1 | 14.8 | 6.0 | 8.8 | 5.9 | 7.9 | 4.4 | 3.5 | 3.3 | 5.3 |
| Chiba | 12.4 | 16.1 | 8.1 | 8.1 | 6.6 | 9.5 | 4.6 | 4.9 | 4.5 | 4.5 |
| Fukuoka | 14.2 | 17.5 | 11.3 | 6.2 | 8.8 | 11.0 | 6.9 | 4.1 | 3.1 | 3.5 |
| Gifu | 12.0 | 16.4 | 7.7 | 8.7 | 6.7 | 8.4 | 4.9 | 3.5 | 2.7 | 4.2 |
| Gunma | 10.6 | 15.3 | 5.4 | 9.9 | 5.7 | 7.5 | 4.6 | 3.0 | 2.6 | 4.4 |
| Hyogo | 12.7 | 16.4 | 9.1 | 7.3 | 7.2 | 9.6 | 5.3 | 4.2 | 3.7 | 5.1 |
| Ibaraki | 10.3 | 17.1 | 3.4 | 13.7 | 5.7 | 8.5 | 3.7 | 4.8 | 2.7 | 7.0 |
| Ishikawa | 9.9 | 14.7 | 5.7 | 9.0 | 5.9 | 7.2 | 4.1 | 3.1 | 4.6 | 4.4 |
| Kanagawa | 12.4 | 16.7 | 8.0 | 8.7 | 6.8 | 9.7 | 4.7 | 5.0 | 4.4 | 4.6 |
| Kyoto | 11.5 | 16.6 | 6.8 | 9.8 | 6.4 | 8.6 | 4.7 | 3.9 | 2.4 | 4.6 |
| Okinawa | 21.3 | 24.0 | 18.8 | 5.1 | 14.7 | 17.4 | 12.4 | 5.0 | 4.3 | 1.9 |
| Osaka | 12.7 | 17.0 | 8.9 | 8.1 | 6.7 | 8.9 | 5.1 | 3.9 | 2.6 | 5.1 |
| Tokyo | 11.7 | 16.7 | 6.7 | 10.0 | 6.4 | 9.3 | 4.5 | 4.8 | 3.3 | 5.4 |
| Toyama | 9.7 | 14.6 | 5.2 | 9.4 | 6.3 | 7.7 | 4.7 | 3.0 | 3.2 | 4.4 |
| Decay Duration (DD) | ||||||||||
| Tave | Tmax | Tmin | Tdiff | Have | Hmax | Hmin | Hdiff | Vair | DL | |
| Aichi | 13.0 | 18.3 | 8.6 | 9.7 | 6.5 | 8.4 | 4.9 | 3.5 | 3.9 | 6.1 |
| Chiba | 15.1 | 19.1 | 11.2 | 7.8 | 8.4 | 10.3 | 6.4 | 3.9 | 4.4 | 4.6 |
| Fukuoka | 14.0 | 17.5 | 10.9 | 6.6 | 7.3 | 9.4 | 5.7 | 3.7 | 3.6 | 4.7 |
| Gifu | 12.6 | 18.2 | 7.7 | 10.6 | 5.1 | 6.6 | 3.6 | 3.0 | 3.5 | 6.5 |
| Gunma | 11.5 | 16.3 | 7.2 | 9.1 | 6.3 | 8.4 | 4.9 | 3.4 | 3.2 | 5.2 |
| Hyogo | 15.5 | 19.0 | 12.4 | 6.6 | 8.1 | 9.5 | 6.0 | 3.5 | 4.0 | 5.3 |
| Ibaraki | 10.8 | 15.6 | 6.4 | 9.1 | 6.5 | 8.2 | 4.9 | 3.3 | 3.5 | 4.7 |
| Ishikawa | 13.1 | 17.3 | 9.2 | 8.1 | 7.0 | 8.7 | 5.4 | 3.3 | 4.4 | 4.5 |
| Kanagawa | 16.6 | 20.7 | 13.0 | 7.7 | 9.8 | 11.7 | 7.7 | 4.0 | 3.9 | 4.9 |
| Kyoto | 14.7 | 20.1 | 10.0 | 10.1 | 7.1 | 9.0 | 5.3 | 3.7 | 2.5 | 5.0 |
| Okinawa | 19.8 | 22.1 | 17.6 | 4.5 | 11.8 | 14.1 | 10.0 | 4.0 | 5.0 | 3.2 |
| Osaka | 16.2 | 20.6 | 12.3 | 8.3 | 8.1 | 10.2 | 6.3 | 3.9 | 2.7 | 5.3 |
| Tokyo | 14.4 | 19.2 | 9.9 | 9.3 | 8.6 | 10.7 | 6.7 | 3.9 | 3.2 | 5.0 |
| Toyama | 12.1 | 17.6 | 7.7 | 9.9 | 7.5 | 9.1 | 5.8 | 3.3 | 3.7 | 3.9 |
| All Duration, from TSS to TDE | ||||||||||
| Tave | Tmax | Tmin | Tdiff | Have | Hmax | Hmin | Hdiff | Vair | DL | |
| Aichi | 11.3 | 16.2 | 7.1 | 6.2 | 8.2 | 4.6 | 3.5 | 11.3 | 3.5 | 5.5 |
| Chiba | 13.8 | 17.8 | 9.6 | 7.3 | 9.7 | 5.4 | 4.3 | 13.8 | 4.3 | 4.9 |
| Fukuoka | 14.9 | 19.0 | 11.4 | 8.6 | 10.8 | 6.8 | 3.9 | 14.9 | 3.3 | 5.5 |
| Gifu | 12.2 | 17.2 | 7.7 | 5.8 | 7.4 | 4.2 | 3.3 | 12.2 | 3.2 | 5.5 |
| Gunma | 11.1 | 16.0 | 6.2 | 5.9 | 7.7 | 4.6 | 3.1 | 11.1 | 2.9 | 5.2 |
| Hyogo | 14.2 | 17.8 | 10.9 | 7.5 | 9.3 | 5.5 | 3.8 | 14.2 | 3.8 | 5.6 |
| Ibaraki | 10.4 | 15.8 | 4.8 | 6.2 | 8.3 | 4.4 | 3.9 | 10.4 | 2.9 | 5.5 |
| Ishikawa | 12.1 | 16.3 | 8.0 | 6.6 | 8.1 | 4.9 | 3.2 | 12.1 | 4.2 | 4.7 |
| Kanagawa | 15.1 | 19.4 | 11.2 | 8.6 | 10.8 | 6.6 | 4.3 | 15.1 | 4.0 | 5.0 |
| Kyoto | 13.6 | 18.9 | 8.8 | 6.8 | 8.8 | 5.0 | 3.8 | 13.6 | 2.4 | 4.9 |
| Okinawa | 20.1 | 22.4 | 17.9 | 12.5 | 14.8 | 10.6 | 4.1 | 20.1 | 4.6 | 2.5 |
| Osaka | 14.3 | 18.6 | 10.4 | 7.2 | 9.3 | 5.6 | 3.7 | 14.3 | 2.6 | 5.4 |
| Tokyo | 13.3 | 18.3 | 8.5 | 7.6 | 9.9 | 5.7 | 4.2 | 13.3 | 3.2 | 5.3 |
| Toyama | 10.9 | 16.1 | 6.2 | 6.8 | 8.4 | 5.2 | 3.2 | 10.9 | 3.4 | 4.3 |
| (i) | (ii) | (iii) | (iv) | (v) | (vi) | ||
|---|---|---|---|---|---|---|---|
| Population density | 0.393 | 0.097 | 0.259 | — | — | — | |
| Elderly density | 0.363 | 0.078 | 0.210 | 0.225 | 0.185 | 0.295 | |
| Elderly percentage | 0.009 | 0.014 | 0.007 | 0.405 | 0.360 | 0.482 | |
| Tave | DS | 0.073 | 0.143 | 0.041 | 0.151 | 0.157 | 0.122 |
| DD | 0.000 | 0.035 | 0.011 | 0.164 | 0.173 | 0.274 | |
| Total | 0.009 | 0.075 | 0.020 | 0.158 | 0.173 | 0.216 | |
| Tmax | DS | 0.089 | 0.161 | 0.035 | 0.175 | 0.181 | 0.130 |
| DD | 0.008 | 0.019 | 0.001 | 0.143 | 0.166 | 0.229 | |
| Total | 0.003 | 0.081 | 0.006 | 0.202 | 0.229 | 0.242 | |
| Tmin | DS | 0.053 | 0.114 | 0.054 | 0.105 | 0.116 | 0.112 |
| DD | 0.001 | 0.041 | 0.019 | 0.147 | 0.147 | 0.246 | |
| Total | 0.013 | 0.069 | 0.034 | 0.122 | 0.134 | 0.192 | |
| Tdiff | DS | 0.007 | 0.027 | 0.047 | 0.015 | 0.021 | 0.043 |
| DD | 0.026 | 0.042 | 0.048 | 0.071 | 0.055 | 0.128 | |
| Total | 0.026 | 0.042 | 0.078 | 0.036 | 0.036 | 0.101 | |
| Have | DS | 0.076 | 0.091 | 0.043 | 0.055 | 0.055 | 0.048 |
| DD | 0.017 | 0.002 | 0.019 | 0.099 | 0.061 | 0.142 | |
| Total | 0.006 | 0.026 | 0.004 | 0.095 | 0.080 | 0.127 | |
| Hmax | DS | 0.069 | 0.123 | 0.032 | 0.152 | 0.149 | 0.131 |
| DD | 0.016 | 0.001 | 0.019 | 0.127 | 0.081 | 0.160 | |
| Total | 0.005 | 0.038 | 0.003 | 0.160 | 0.138 | 0.191 | |
| Hmin | DS | 0.086 | 0.084 | 0.036 | 0.044 | 0.039 | 0.025 |
| DD | 0.011 | 0.002 | 0.016 | 0.089 | 0.051 | 0.117 | |
| Total | 0.011 | 0.024 | 0.004 | 0.079 | 0.060 | 0.089 | |
| Hdiff | DS | 0.001 | 0.107 | 0.002 | 0.463 | 0.488 | 0.546 |
| DD | 0.052 | 0.001 | 0.031 | 0.347 | 0.277 | 0.384 | |
| Total | 0.006 | 0.074 | 0.000 | 0.485 | 0.509 | 0.635 | |
| Vair | DS | 0.034 | 0.058 | 0.007 | 0.020 | 0.022 | 0.044 |
| DD | 0.035 | 0.000 | 0.091 | 0.023 | 0.027 | 0.003 | |
| Total | 0.001 | 0.008 | 0.032 | 0.015 | 0.017 | 0.015 | |
| DL | DS | 0.023 | 0.007 | 0.012 | 0.012 | 0.010 | 0.014 |
| DD | 0.021 | 0.077 | 0.025 | 0.045 | 0.086 | 0.018 | |
| Total | 0.008 | 0.007 | 0.000 | 0.035 | 0.053 | 0.029 | |
| Parameters | Cases/Density | Deaths/Density | Deaths/Density (Ex.) | ||||
|---|---|---|---|---|---|---|---|
| p | p-value | p | p-value | p | p-value | ||
| Elderly percentage | 0.864 | <0.0001 | 0.824 | <0.001 | 0.842 | <0.001 | |
| Tave | −0.456 | 0.101 | −0.489 | 0.076 | −0.456 | 0.101 | 0.101 |
| −0.565 | <0.05 | −0.539 | <0.05 | −0.543 | <0.05 | <0.005 | |
| −0.503 | 0.067 | −0.543 | <0.05 | −0.508 | 0.064 | 0.064 | |
| Tmax | −0.526 | 0.050 | −0.551 | <0.05 | −0.471 | 0.089 | 0.089 |
| −0.631 | <0.05 | −0.574 | <0.05 | −0.560 | <0.05 | <0.005 | |
| Total | −0.475 | 0.086 | −0.535 | <0.05 | −0.473 | 0.088 | |
| Tmin | DS | −0.385 | 0.175 | −0.446 | 0.110 | −0.442 | 0.114 |
| DD | −0.524 | 0.055 | −0.506 | 0.065 | −0.511 | 0.062 | |
| Total | −0.429 | 0.126 | −0.477 | 0.084 | −0.453 | 0.104 | |
| Tdiff | DS | 0.234 | 0.422 | 0.280 | 0.333 | 0.311 | 0.280 |
| DD | 0.317 | 0.269 | 0.273 | 0.345 | 0.289 | 0.317 | |
| Total | 0.315 | 0.273 | 0.326 | 0.255 | 0.375 | 0.187 | |
| Have | DS | −0.314 | 0.275 | −0.353 | 0.215 | −0.331 | 0.248 |
| DD | −0.560 | <0.05 | −0.465 | 0.094 | −0.469 | 0.091 | |
| Total | −0.496 | 0.071 | −0.476 | 0.085 | −0.450 | 0.107 | |
| Hmax | DS | −0.578 | <0.05 | −0.569 | <0.05 | −0.534 | <0.05 |
| DD | −0.570 | <0.05 | −0.497 | 0.070 | −0.488 | 0.076 | |
| Total | −0.601 | <0.05 | −0.579 | <0.05 | −0.542 | <0.05 | |
| Hmin | DS | −0.080 | 0.787 | −0.113 | 0.701 | −0.060 | 0.839 |
| DD | −0.532 | 0.050 | −0.439 | 0.116 | −0.444 | 0.112 | |
| Total | −0.495 | 0.072 | −0.493 | 0.073 | −0.453 | 0.104 | |
| Hdiff | DS | −0.665 | <0.01 | −0.583 | <0.05 | −0.579 | <0.05 |
| DD | −0.777 | <0.005 | −0.736 | <0.005 | −0.699 | <0.01 | |
| Total | −0.669 | <0.01 | −0.636 | <0.05 | −0.623 | <0.05 | |
| Vair | DS | −0.160 | 0.584 | −0.081 | 0.782 | −0.187 | 0.523 |
| DD | −0.024 | 0.935 | 0.077 | 0.794 | −0.029 | 0.923 | |
| Total | −0.108 | 0.714 | −0.007 | 0.982 | −0.103 | 0.725 | |
| DL | DS | −0.464 | 0.095 | −0.411 | 0.144 | −0.446 | 0.110 |
| DD | −0.169 | 0.563 | −0.222 | 0.446 | −0.231 | 0.427 | |
| Total | −0.191 | 0.513 | −0.301 | 0.296 | −0.319 | 0.267 | |
| Cases | Deaths | Deaths (Ex.) † | |||||||
|---|---|---|---|---|---|---|---|---|---|
| R2 | adj. R2 | p-Value | R2 | adj. R2 | p-Value | R2 | adj. R2 | p-Value | |
| DS | 0.777 | 0.693 | <0.01 | 0.659 | 0.532 | <0.05 | 0.384 | 0.153 | 0.251 |
| DD | 0.773 | 0.688 | <0.01 | 0.653 | 0.523 | <0.05 | 0.383 | 0.151 | 0.253 |
| Total | 0.776 | 0.692 | <0.01 | 0.662 | 0.536 | <0.05 | 0.386 | 0.155 | 0.249 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kodera, S.; Rashed, E.A.; Hirata, A. Correlation between COVID-19 Morbidity and Mortality Rates in Japan and Local Population Density, Temperature, and Absolute Humidity. Int. J. Environ. Res. Public Health 2020, 17, 5477. https://doi.org/10.3390/ijerph17155477
Kodera S, Rashed EA, Hirata A. Correlation between COVID-19 Morbidity and Mortality Rates in Japan and Local Population Density, Temperature, and Absolute Humidity. International Journal of Environmental Research and Public Health. 2020; 17(15):5477. https://doi.org/10.3390/ijerph17155477
Chicago/Turabian StyleKodera, Sachiko, Essam A. Rashed, and Akimasa Hirata. 2020. "Correlation between COVID-19 Morbidity and Mortality Rates in Japan and Local Population Density, Temperature, and Absolute Humidity" International Journal of Environmental Research and Public Health 17, no. 15: 5477. https://doi.org/10.3390/ijerph17155477
APA StyleKodera, S., Rashed, E. A., & Hirata, A. (2020). Correlation between COVID-19 Morbidity and Mortality Rates in Japan and Local Population Density, Temperature, and Absolute Humidity. International Journal of Environmental Research and Public Health, 17(15), 5477. https://doi.org/10.3390/ijerph17155477