Characterization of Clostridium Perfringens Isolates Collected from Three Agricultural Biogas Plants over a One-Year Period
Abstract
1. Introduction
2. Materials and Methods
2.1. Biogas Plants and Sample Collection
2.2. Isolation of C. perfringens
2.3. DNA Extraction
2.4. Determination of the Toxin Genotype and Search for Antibiotic Resistance Genes
2.5. Testing Antimicrobial Susceptibility
2.6. Statistical Analysis
3. Results
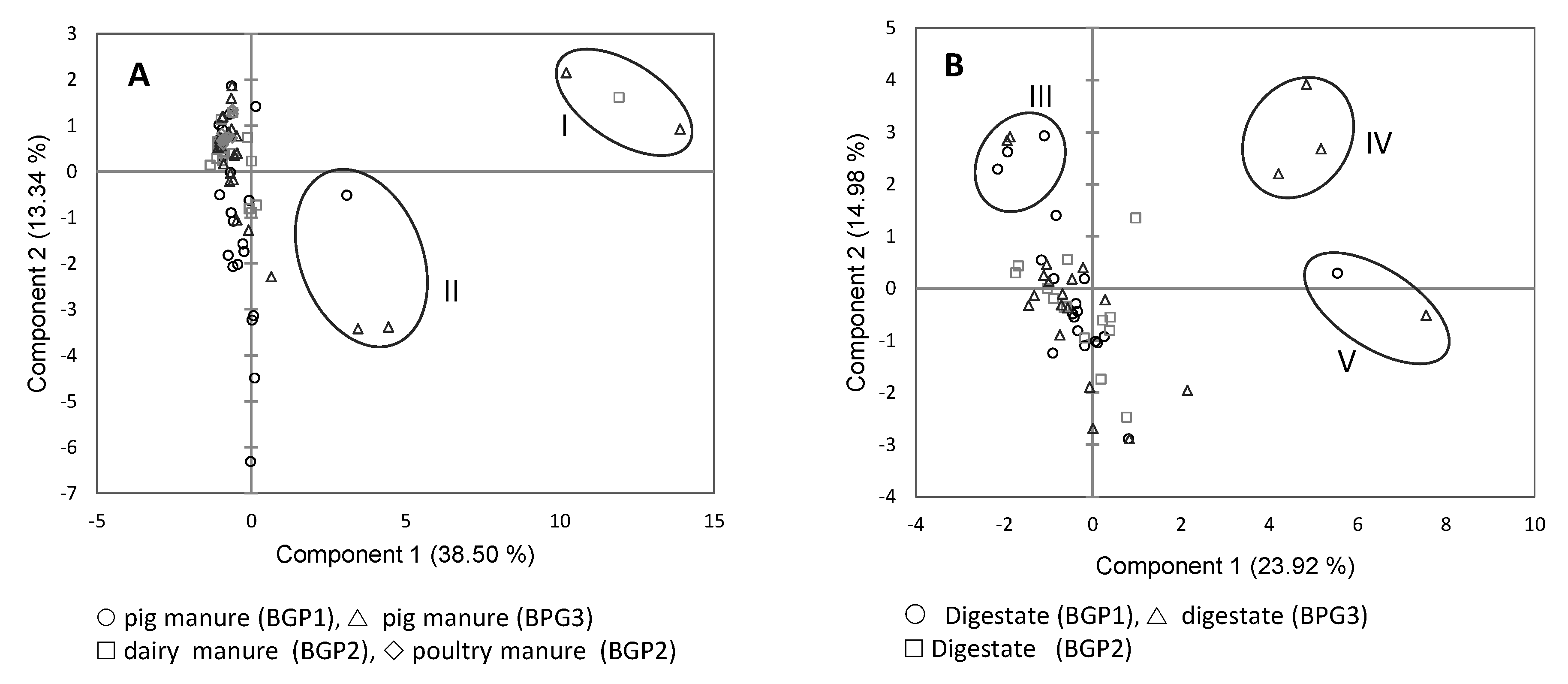
3.1. Toxinotyping of C. perfringens Isolates
3.2. Tetracycline and Erythromycin Resistance Genes of C. perfringens Isolates
3.3. Antimicrobial Susceptibility of C. perfringens Isolates
4. Discussion
4.1. Toxinotyping of C. perfringens Isolates
4.2. Tetracycline and Erythromycin Resistance Genes of C. perfringens Isolates
4.3. Antimicrobial Susceptibility of C. perfringens Isolates
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Annual Statistical Report; European Biogas Association: Gent, Belgium, 2019.
- Johansson, A.; Aspan, A.; Bagge, E.; Båverud, V.; Engström, B.E.; Johansson, K.-E. Genetic diversity of Clostridium perfringens type A isolates from animals, food poisoning outbreaks and sludge. BMC Microbiol. 2006, 6, 47. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Brandón, M.; Juárez, M.F.-D.; Zangerle, M.; Insam, H. Effects of digestate on soil chemical and microbiological properties: A comparative study with compost and vermicompost. J. Hazard. Mater. 2016, 302, 267–274. [Google Scholar] [CrossRef]
- Lau, C.H.-F.; Li, B.; Zhang, T.; Tien, Y.-C.; Scott, A.; Murray, R.; Sabourin, L.; Lapen, D.R.; Duenk, P.; Topp, E. Impact of pre-application treatment on municipal sludge composition, soil dynamics of antibiotic resistance genes, and abundance of antibiotic-resistance genes on vegetables at harvest. Sci. Total Environ. 2017, 587, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.; Tien, Y.-C.; Drury, C.F.; Reynolds, W.D.; Topp, E. Enrichment of antibiotic resistance genes in soil receiving composts derived from swine manure, yard wastes, or food wastes, and evidence for multiyear persistence of swine Clostridium spp. Can. J. Microbiol. 2018, 64, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Leclercq, S.O.; Wang, C.; Sui, Z.; Wu, H.; Zhu, B.; Deng, Y.; Feng, J. A multiplayer game: Species of Clostridium, Acinetobacter, and Pseudomonas are responsible for the persistence of antibiotic resistance genes in manure-treated soils: Antibiotic resistance genes in manure-treated soils. Environ. Microbiol. 2016, 18, 3494–3508. [Google Scholar] [CrossRef]
- Kather, E.J.; Marks, S.L.; Foley, J.E. Determination of the prevalence of antimicrobial resistance genes in canine Clostridium perfringens isolates. Vet. Microbiol. 2006, 113, 97–101. [Google Scholar] [CrossRef]
- Soge, O.O.; Tivoli, L.D.; Meschke, J.S.; Roberts, M.C. A conjugative macrolide resistance gene mef (A), in environmental Clostridium perfringens carrying multiple macrolide and/or tetracycline resistance genes. J. Appl. Microbiol. 2009, 106, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Alegbeleye, O.O.; Sant’Ana, A.S. Manure-borne pathogens as an important source of water contamination: An update on the dynamics of pathogen survival/transport as well as practical risk mitigation strategies. Int. J. Hyg. Environ. Health 2020, 227, 113524. [Google Scholar] [CrossRef]
- Nag, R.; Auer, A.; Markey, B.K.; Whyte, P.; Nolan, S.; O’Flaherty, V.; Russell, L.; Bolton, D.; Fenton, O.; Richards, K.; et al. Anaerobic digestion of agricultural manure and biomass―Critical indicators of risk and knowledge gaps. Sci. Total Environ. 2019, 690, 460–479. [Google Scholar] [CrossRef]
- Hamza, D.; Dorgham, S.M.; Elhariri, M.; Elhelw, R.; Ismael, E. New insight of apparently healthy animals as a potential reservoir for Clostridium perfringens: A public health implication. J. Vet. Res. 2018, 62, 457–462. [Google Scholar] [CrossRef]
- Tango, C.N.; Wei, S.; Khan, I.; Hussain, M.S.; Kounkeu, P.-F.N.; Park, J.; Kim, S.; Oh, D.H. Microbiological Quality and Safety of Fresh Fruits and Vegetables at Retail Levels in Korea. J. Food Sci. 2018, 83, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Pence, M.A. Antimicrobial Resistance in Clinically Important Anaerobes. Clin. Microbiol. Newsl. 2019, 41, 1–7. [Google Scholar] [CrossRef]
- Kiu, R.; Brown, J.; Bedwell, H.; Leclaire, C.; Caim, S.; Pickard, D.; Dougan, G.; Dixon, R.A.; Hall, L.J. Genomic analysis on broiler-associated Clostridium perfringens strains and exploratory caecal microbiome investigation reveals key factors linked to poultry necrotic enteritis. Anim. Microbiome 2019, 1, 12. [Google Scholar] [CrossRef] [PubMed]
- Rood, J.I.; Adams, V.; Lacey, J.; Lyras, D.; McClane, B.A.; Melville, S.B.; Moore, R.J.; Popoff, M.R.; Sarker, M.R.; Songer, J.G.; et al. Expansion of the Clostridium perfringens toxin-based typing scheme. Anaerobe 2018, 53, 5–10. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Surveillance for Foodborne Disease Outbreaks, United States, 2017; CDC: Atlanta, GA, USA, 2019; p. 10. [Google Scholar]
- Anonymous Santé Publique France/Le point Épidémio/Surveillance des Toxi-Infections Alimentaires Collectives. Données de la Déclaration Obligatoire 2018; Santé publique: Saint-Maurice, France, 2019; p. 12.
- Freedman, J.C.; Theoret, J.R.; Wisniewski, J.A.; Uzal, F.A.; Rood, J.I.; McClane, B.A. Clostridium perfringens type A–E toxin plasmids. Res. Microbiol. 2015, 166, 264–279. [Google Scholar] [CrossRef]
- Uzal, F.A.; Navarro, M.A.; Li, J.; Freedman, J.C.; Shrestha, A.; McClane, B.A. Comparative pathogenesis of enteric clostridial infections in humans and animals. Anaerobe 2018, 53, 11–20. [Google Scholar] [CrossRef]
- Fisher, D.J.; Miyamoto, K.; Harrison, B.; Akimoto, S.; Sarker, M.R.; McClane, B.A. Association of beta2 toxin production with Clostridium perfringens type A human gastrointestinal disease isolates carrying a plasmid enterotoxin gene: cpb2/cpe -positive C. perfringens disease isolates. Mol. Microbiol. 2005, 56, 747–762. [Google Scholar] [CrossRef]
- Rood, J.I.; Buddle, J.R.; Wales, A.J.; Sidhu, R. The occurrence of antibiotic resistance in Clostridium perfringens from pigs. Aust. Vet. J. 1985, 62, 276–279. [Google Scholar] [CrossRef]
- Slavić, Đ.; Boerlin, P.; Fabri, M.; Klotins, K.C.; Zoethout, J.K.; Weir, P.E.; Bateman, D. Antimicrobial susceptibility of Clostridium perfringens isolates of bovine, chicken, porcine, and turkey origin from Ontario. Can. J. Vet. Res. 2011, 75, 89–97. [Google Scholar]
- Adams, V.; Han, X.; Lyras, D.; Rood, J.I. Antibiotic resistance plasmids and mobile genetic elements of Clostridium perfringens. Plasmid 2018, 99, 32–39. [Google Scholar] [CrossRef]
- Johansson, A.; Greko, C.; Engström, B.E.; Karlsson, M. Antimicrobial susceptibility of Swedish, Norwegian and Danish Clostridium perfringens from poultry, and distribution of tetracycline resistance genes. Vet. Microbiol. 2004, 99, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Park, M.; Rafii, F. The prevalence of plasmid-coded cpe enterotoxin, β2 toxin, tpeL toxin, and tetracycline resistance in Clostridium perfringens strains isolated from different sources. Anaerobe 2019, 56, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Berryman, D.I.; Lyristis, M.; Rood, J.I. Cloning and sequence analysis of ermQ, the predominant macrolide-lincosamide-streptogramin B resistance gene in Clostridium perfringens. Antimicrob. Agents Chemother. 1994, 38, 1041–1046. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, Y.; Yamamoto, K.; Tamura, Y.; Takahashi, T. Tetracycline-resistance genes of Clostridium perfringens, Clostridium septicum, and Clostridium sordellii isolated from cattle affected with malignant edema. Vet. Microbiol. 2001, 83, 61–69. [Google Scholar] [CrossRef]
- Park, M.; Rooney, A.P.; Hecht, D.W.; Li, J.; McClane, B.A.; Nayak, R.; Paine, D.D.; Rafii, F. Phenotypic and genotypic characterization of tetracycline and minocycline resistance in Clostridium perfringens. Arch. Microbiol. 2010, 192, 803–810. [Google Scholar] [CrossRef]
- Salvarani, F.M.; Silva, R.O.S.; Pires, P.S.; Cruz Júnior, E.C.D.C.; Albefaro, I.S.; Guedes, R.M.D.C.; Lobato, F.C.F. Antimicrobial susceptibility of Clostridium perfringens isolated from piglets with or without diarrhea in Brazil. Braz. J. Microbiol. 2012, 43, 1030–1033. [Google Scholar] [CrossRef]
- Voidarou, C.; Bezirtzoglou, E.; Alexopoulos, A.; Plessas, S.; Stefanis, C.; Papadopoulos, I.; Vavias, S.; Stavropoulou, E.; Fotou, K.; Tzora, A.; et al. Occurrence of Clostridium perfringensfrom different cultivated soils. Anaerobe 2011, 17, 320–324. [Google Scholar] [CrossRef]
- Lloret, E.; Salar, M.J.; Blaya, J.; Pascual, J.A. Two-stage mesophilic anaerobic–thermophilic digestion for sludge sanitation to obtain advanced treated sludge. Chem. Eng. J. 2013, 230, 59–63. [Google Scholar] [CrossRef]
- Le Maréchal, C.; Druilhe, C.; Repérant, E.; Boscher, E.; Rouxel, S.; Le Roux, S.; Poëzévara, T.; Ziebal, C.; Houdayer, C.; Nagard, B.; et al. Evaluation of the occurrence of sporulating and non-sporulating pathogenic bacteria in manure and in digestate of five agricultural biogas plants. Microbiology 2019, 8. [Google Scholar] [CrossRef]
- Anonymous ISO 7937: 2005-02: Microbiology of Food and Animal Feeding Stuffs―Horizontal Method for the Enumeration of Clostridium perfringens―Colony-Count Technique; International Standard Organization: Geneva, Switzerland, 2005.
- Keyburn, A.L.; Boyce, J.D.; Vaz, P.; Bannam, T.L.; Ford, M.E.; Parker, D.; Di Rubbo, A.; Rood, J.I.; Moore, R.J. NetB. a New Toxin That Is Associated with Avian Necrotic Enteritis Caused by Clostridium perfringens. PLoS Pathog. 2008, 4, e26. [Google Scholar] [CrossRef]
- Baums, C.G.; Schotte, U.; Amtsberg, G.; Goethe, R. Diagnostic multiplex PCR for toxin genotyping of Clostridium perfringens isolates. Vet. Microbiol. 2004, 100, 11–16. [Google Scholar] [CrossRef]
- Gu, Z.; Eils, R.; Schlesner, M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics 2016, 32, 2847–2849. [Google Scholar] [CrossRef] [PubMed]
- Orzi, V.; Scaglia, B.; Lonati, S.; Riva, C.; Boccasile, G.; Alborali, G.L.; Adani, F. The role of biological processes in reducing both odor impact and pathogen content during mesophilic anaerobic digestion. Sci. Total Environ. 2015, 526, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Ngamwongsatit, B.; Tanomsridachchai, W.; Suthienkul, O.; Urairong, S.; Navasakuljinda, W.; Janvilisri, T. Multidrug resistance in Clostridium perfringens isolated from diarrheal neonatal piglets in Thailand. Anaerobe 2016, 38, 88–93. [Google Scholar] [CrossRef]
- Fohler, S.; Klein, G.; Hoedemaker, M.; Scheu, T.; Seyboldt, C.; Campe, A.; Jensen, K.C.; Abdulmawjood, A. Diversity of Clostridium perfringens toxin-genotypes from dairy farms. BMC Microbiol. 2016, 16. [Google Scholar] [CrossRef]
- Zhang, T.; Zhang, W.; Ai, D.; Zhang, R.; Lu, Q.; Luo, Q.; Shao, H. Prevalence and characterization of Clostridium perfringens in broiler chickens and retail chicken meat in central China. Anaerobe 2018, 54, 100–103. [Google Scholar] [CrossRef]
- Freedman, J.; Shrestha, A.; McClane, B. Clostridium perfringens Enterotoxin: Action, Genetics, and Translational Applications. Toxins 2016, 8, 73. [Google Scholar] [CrossRef]
- Hashimoto, A.; Tsuchioka, H.; Higashi, K.; Ota, N.; Harada, H. Distribution of Enterotoxin Gene-positive Clostridium perfringens Spores among Human and Livestock Samples and its Potential as a Human Fecal Source Tracking Indicator. J. Water Environ. Technol. 2016, 14, 447–454. [Google Scholar] [CrossRef]
- Yadav, J.P.; Das, S.C.; Dhaka, P.; Vijay, D.; Kumar, M.; Mukhopadhyay, A.K.; Chowdhury, G.; Chauhan, P.; Singh, R.; Dhama, K.; et al. Molecular characterization and antimicrobial resistance profile of Clostridium perfringens type A isolates from humans, animals, fish and their environment. Anaerobe 2017, 47, 120–124. [Google Scholar] [CrossRef]
- Yang, W.-Y.; Chou, C.-H.; Wang, C. Characterization of toxin genes and quantitative analysis of netB in necrotic enteritis (NE)-producing and non-NE-producing Clostridium perfringens isolated from chickens. Anaerobe 2018, 54, 115–120. [Google Scholar] [CrossRef]
- Chan, G.; Farzan, A.; Soltes, G.; Nicholson, V.M.; Pei, Y.; Friendship, R.; Prescott, J.F. The epidemiology of Clostridium perfringens type A on Ontario swine farms, with special reference to cpb2-positive isolates. BMC Vet. Res. 2012, 8, 156. [Google Scholar] [CrossRef] [PubMed]
- Martel, A.; Devriese, L.; Cauwerts, K.; De Gussem, K.; Decostere, A.; Haesebrouck, F. Susceptibility of Clostridium perfringens strains from broiler chickens to antibiotics and anticoccidials. Avian Pathol. 2004, 33, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Gholamiandehkordi, A.; Eeckhaut, V.; Lanckriet, A.; Timbermont, L.; Bjerrum, L.; Ducatelle, R.; Haesebrouck, F.; Van Immerseel, F. Antimicrobial resistance in Clostridium perfringens isolates from broilers in Belgium. Vet. Res. Commun. 2009, 33, 1031–1037. [Google Scholar] [CrossRef]
- Villarino, N.; Brown, S.A.; Martín-Jiménez, T. The role of the macrolide tulathromycin in veterinary medicine. Vet. J. 2013, 198, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Llanco, L.; Nakano, V.; Ajp, F.; Mj, A.-C. Toxinotyping and antimicrobial susceptibility of Clostridium perfringens isolated from broiler chickens with necrotic enteritis. Int. J. Micr. Res. 2012, 4, 290–294. [Google Scholar] [CrossRef]
- Oliveira Júnior, C.A.D.; Silva, R.O.S.; Diniz, A.N.; Pires, P.S.; Salvarani, F.M.; Assis, R.A.D.; Lobato, F.C.F. Antimicrobial susceptibility of Clostridium perfringens isolated from domestic and wild animal species in Brazil. Sem. Ci. Agr. 2016, 37, 257. [Google Scholar] [CrossRef]
- Tien, Y.-C.; Li, B.; Zhang, T.; Scott, A.; Murray, R.; Sabourin, L.; Marti, R.; Topp, E. Impact of dairy manure pre-application treatment on manure composition, soil dynamics of antibiotic resistance genes, and abundance of antibiotic-resistance genes on vegetables at harvest. Sci. Total Environ. 2017, 581, 32–39. [Google Scholar] [CrossRef]
- Sahlström, L.; Bagge, E.; Emmoth, E.; Holmqvist, A.; Danielsson-Tham, M.-L.; Albihn, A. A laboratory study of survival of selected microorganisms after heat treatment of biowaste used in biogas plants. Bioresour. Technol. 2008, 99, 7859–7865. [Google Scholar] [CrossRef]
- Carrère, H.; Antonopoulou, G.; Affes, R.; Passos, F.; Battimelli, A.; Lyberatos, G.; Ferrer, I. Review of feedstock pretreatment strategies for improved anaerobic digestion: From lab-scale research to full-scale application. Bioresour. Technol. 2016, 199, 386–397. [Google Scholar] [CrossRef]
- Carrère, H.; Sialve, B.; Bernet, N. Improving pig manure conversion into biogas by thermal and thermo-chemical pretreatments. Bioresour. Technol. 2009, 100, 3690–3694. [Google Scholar] [CrossRef]
- Talukdar, P.K.; Udompijitkul, P.; Hossain, A.; Sarker, M.R. Inactivation Strategies for Clostridium perfringens Spores and Vegetative Cells. Appl. Envion. Microbiol. 2017, 83, e02731-16. [Google Scholar] [CrossRef] [PubMed]
| BGP1 | BGP2 | BGP3 | |||||
|---|---|---|---|---|---|---|---|
| Matrix | Manure | Digestate | Dairy Manure | Poultry Manure | Digestate | Manure | Digestate |
| Nb isolates | 24 | 21 | 25 | 14 | 19 | 29 | 25 |
| Gene | Primers | Sequences (5′-3′) | Amplicon Size (bp) | Reference |
|---|---|---|---|---|
| cpa | CPA5L | AGTCTACGCTTGGGATGGAA | 900 | [35] |
| CPA5R | TTTCCTGGGTTGTCCATTTC | |||
| cpb | CPBL | TCCTTTCTTGAGGGAGGATAAA | 611 | [35] |
| CPBR | TGAACCTCCTATTTTGTATCCCA | |||
| iap | CPIL | AAACGCATTAAAGCTCACACC | 293 | [35] |
| CPIR | CTGCATAACCTGGAATGGCT | |||
| etx | CPETXL | TGGGAACTTCGATACAAGCA | 396 | [35] |
| CPEXTR | TTAACTCATCTCCCATAACTGCAC | |||
| cpe | CPEL | GGGGAACCCTCAGTAGTTTCA | 506 | [35] |
| CPER | ACCAGCTGGATTTGAGTTTAATG | |||
| cpb2 | CPB2L | CAAGCAATTGGGGGAGTTTA | 200 | [35] |
| CPB2R | GCAGAATCAGGATTTTGACCA | |||
| netB | AKP78 | GCTGGTGCTGGAATAAATGC | 383 | [34] |
| AKP79 | TCGCCATTGAGTAGTTTCCC | |||
| erm(Q) | GE 350 | GAAGAGTTAAATYCACCAACTGA | 84 | This study |
| GE 352 | ACTCTCTCTAGGTATTCCCA | |||
| tetA(P) | GE 353 | TGTAGCACAGATTGTATGGGGA | 124 | This study |
| GE 355 | CCCTGCTTGTGCTCCCTTTA | |||
| tetB(P) | GE 359 | TTTTGGGCGACAGTAGGCTT | 90 | This study |
| GE 361 | TGGCAATGACCCTACTGAAACA | |||
| tet(M) | GE 362 | GCTATTGCCACAGAGAGAGAGA | 127 | This study |
| GE 364 | CGGGTCACTGTCGGAGATTT |
| Type (Gene) | BGP1 n (%) | BGP2 n (%) | BGP3 n (%) | Total n (%) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Manure n = 23 | Digestate n = 20 | Dairy Manure n = 19 | Poultry Manure n = 14 | Digestate n = 14 | Manure n = 24 | Digestate n = 24 | Manure n = 80 | Digestate n = 58 | |
| A (cpa) | 6 (26.1) | 3 (15) | 15 (78.9) | 12 (85.7) | 8 (57.1) | 6 (25) | 6 (25) | 39 (67.2) | 17(21.3) |
| A (cpa + cpb2) | 13 (56.5) | 15 (75) | 2(10.5) | 2(14.3) | 5 (35.7) | 8 (33.3) | 7 (29.2) | 25 (43.1) | 27(33.8) |
| G (netB) | 2 (8.7) | 1 (5) | 2(10.5) | - | - | 4 (16.7) | 1 (4.2) | 8 (13.8) | 2(2.5) |
| G (netB + cpb2) | 2 (8.7) | 1 (5) | - | - | 1 (7.1) | 3 (12.5) | 6 (25) | 5 (8.6) | 8(10) |
| C (cpb) | -1 | - | - | - | - | - | 1 (4.2) | - | 1 (1.3) |
| C (cpb + cpb2) | - | - | - | - | - | 1 (4.2) | 3 (12.5) | 1 (1.7) | 3(3.8) |
| D (etx) | - | - | - | - | - | 1 (4.2) | - | 1 (1.7) | - |
| D (etx + cpb2) | - | - | - | - | - | 1 (4.2) | - | 1 (1.7) | - |
| Gene | BGP1 n (%) | BGP2 n (%) | BGP3 n (%) | Total n (%) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Manure n = 23 | Digestate n = 20 | Dairy Manure n = 19 | Poultry Manure n = 14 | Digestate n = 14 | Manure n = 24 | Digestate n = 24 | Manure n = 80 | Digestate n = 58 | |
| tetA(P) | 12 (52.2) | 13 (65) | 2(10.5) | - | 2 (14.3) | 10 (41.7) | 5 (20.8) | 24 (30) | 20 (34.5) |
| tetA(P) + tetB(P) | 9 (39.2) | 6 (30) | 10 (52.6) | - | 8 (57.1) | 5 (20.8) | 10 (41.7) | 24 (30) | 24 (41.4) |
| tetA(P) + erm(Q) | 1 (4.3) | - | - | - | - | - | 1 (4.2) | 1 (1.25) | 1 (1.7) |
| tetB(P) + erm(Q) | - 1 | - | - | - | - | 1 (4.2) | - | 1 (1.25) | - |
| tetA(P) + tetB(P) + erm(Q) | 1 (4.3) | 1 (5) | - | - | - | - | 4 (16.7) | 1 (1.25) | 5 (8.6) |
| tet(M) | - | - | - | - | - | - | - | - | - |
| no ARG 2 | - | - | 7 (36.8) | 14 (100) | 4 (28.6) | 8 (33.3) | 4 (16.7) | 29 (36.3) | 8 (13.8) |
| Antimicrobial Agents | Origin of Isolates | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Manure (n = 80) | Digestate (n = 58) | ||||||||
| MIC50 | MIC90 | Min | Max | MIC50 | MIC90 | Min | Max | ||
| β-lactams | Penicillin | ≤0.125 | 1 | ≤0.125 | >8 | ≤0.125 | 0.5 | ≤0.125 | 1 |
| Ampicillin | ≤0.25 | ≤0.25 | ≤0.25 | >16 | ≤0.25 | ≤0.25 | ≤0.25 | 2 | |
| Ceftiofur | ≤0.25 | 1 | ≤0.25 | 4 | ≤0.25 | 2 | ≤0.25 | 2 | |
| Macrolides | Tartrate Tylosin | ≤0.5 | 4 | ≤0.5 | >32 | ≤0.5 | 8 | ≤0.5 | 16 |
| Tilmicosin | ≤4 | 8 | ≤4 | >64 | ≤4 | ≤4 | ≤4 | >64 | |
| Tulathromycin | 64 | >64 | 16 | >64 | 64 | >64 | 32 | >64 | |
| Lincosamides | Clindamycin | 2 | 2 | ≤0.25 | >16 | 2 | 4 | ≤0.25 | >16 |
| Fluoroquinolones | Enrofloxacin | 0.25 | >2 | 0.25 | >2 | 0.50 | >2 | ≤0.125 | >2 |
| Danofloxacin | 1 | >1 | 0.25 | >1 | 1 | >1 | 0.5 | >1 | |
| Pleuromutilins | Tiamulin | 4 | 8 | ≤0.5 | >32 | 4 | 16 | ≤0.5 | >32 |
| Phenicols | Florfenicol | 1 | 2 | 0.5 | >8 | 1 | 1 | ≤0.25 | 2 |
| Tetracyclines | Chlortetracycline | ≤0.5 | 8 | ≤0.5 | >8 | 1 | 4 | ≤0.5 | 8 |
| Oxytetracycline | 2 | >8 | ≤0.5 | >8 | 8 | >8 | ≤0.5 | >8 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Derongs, L.; Druilhe, C.; Ziebal, C.; Le Maréchal, C.; Pourcher, A.-M. Characterization of Clostridium Perfringens Isolates Collected from Three Agricultural Biogas Plants over a One-Year Period. Int. J. Environ. Res. Public Health 2020, 17, 5450. https://doi.org/10.3390/ijerph17155450
Derongs L, Druilhe C, Ziebal C, Le Maréchal C, Pourcher A-M. Characterization of Clostridium Perfringens Isolates Collected from Three Agricultural Biogas Plants over a One-Year Period. International Journal of Environmental Research and Public Health. 2020; 17(15):5450. https://doi.org/10.3390/ijerph17155450
Chicago/Turabian StyleDerongs, Lorine, Céline Druilhe, Christine Ziebal, Caroline Le Maréchal, and Anne-Marie Pourcher. 2020. "Characterization of Clostridium Perfringens Isolates Collected from Three Agricultural Biogas Plants over a One-Year Period" International Journal of Environmental Research and Public Health 17, no. 15: 5450. https://doi.org/10.3390/ijerph17155450
APA StyleDerongs, L., Druilhe, C., Ziebal, C., Le Maréchal, C., & Pourcher, A.-M. (2020). Characterization of Clostridium Perfringens Isolates Collected from Three Agricultural Biogas Plants over a One-Year Period. International Journal of Environmental Research and Public Health, 17(15), 5450. https://doi.org/10.3390/ijerph17155450





