Sex-Specific Energy Intakes and Physical Activity Levels According to the Presence of Metabolic Syndrome in Korean Elderly People: Korean National Health and Nutrition Examination Survey 2016–2018
Abstract
1. Introduction
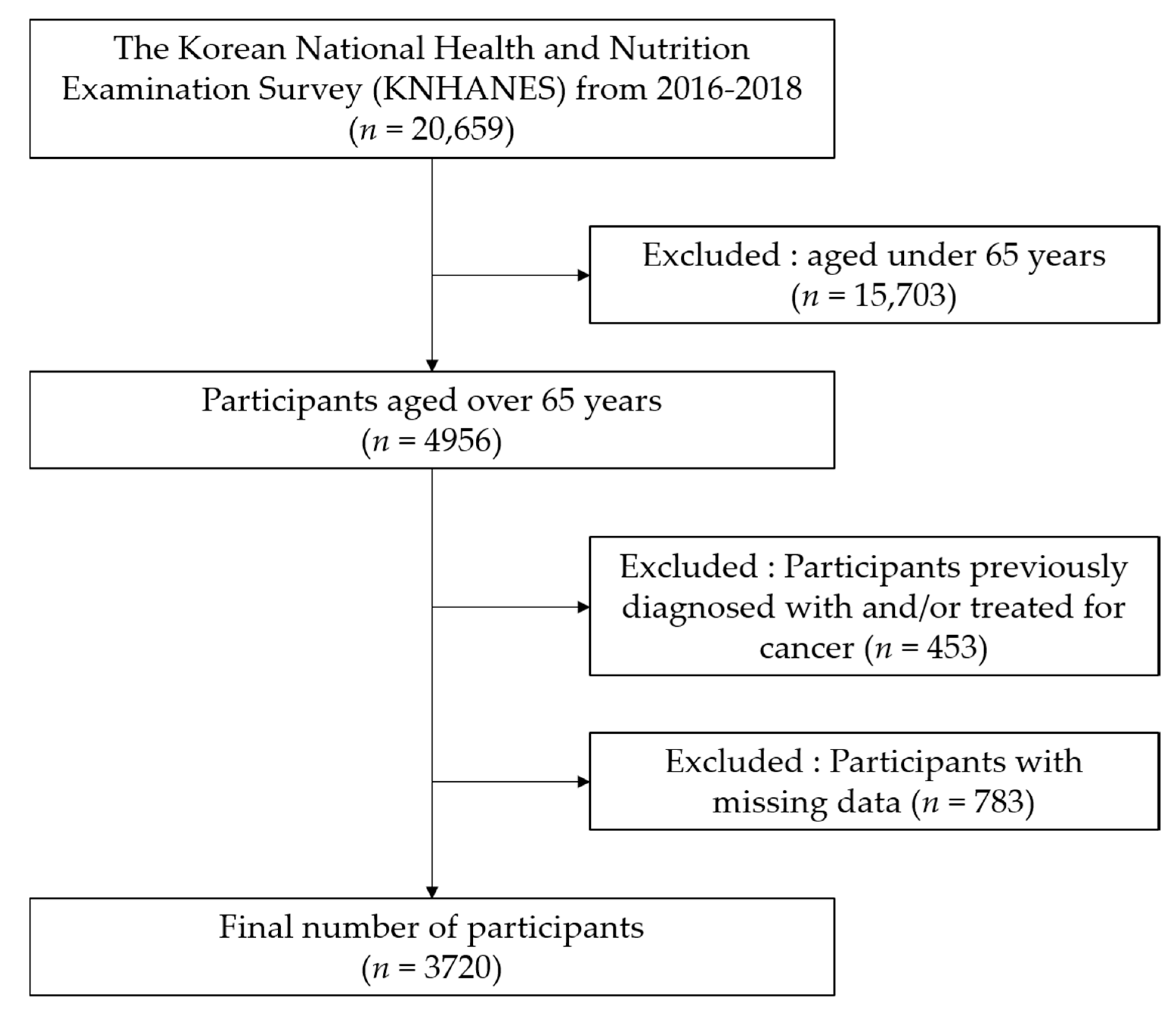
2. Materials and Methods
2.1. Sample and Design
2.2. Measures
2.3. Metabolic Syndrome
2.4. Physical Activity
- Vigorous intensity activity: occupational (MET) = 8.0 × vigorous intensity physical activity (day/week) × 1-day vigorous intensity physical activity (minutes/day)
- Moderate intensity activity: occupational (MET) = 4.0 × moderate intensity physical activity (day/week) × 1-day moderate intensity physical activity (minutes/day)
- Vigorous intensity activity: recreational (MET) = 8.0 × vigorous intensity physical activity (day/week) × 1-day vigorous intensity physical activity (minutes/day)
- Moderate intensity activity: recreational (MET) = 4.0 × moderate intensity physical activity (day/week) × 1-day moderate intensity physical activity (minutes/day)
- Place movement (MET) = 4.0 × place movement physical activity (day/week) × 1-day place movement physical activity
- Total Physical Activity (MET) = vigorous intensity activity: occupational + moderate intensity activity: occupational + vigorous intensity activity: recreational + moderate intensity activity: recreational + place movement.
2.5. Energy Intake and Intake Ratio
2.6. Statistical Analysis
3. Results
3.1. Differences in Physical Activity Levels According to the Presence or Absence of Metabolic Syndrome and According to Sex
3.2. Difference in Energy Intakes According to the Presence or Absence of Metabolic Syndrome and According to Sex
3.3. Odds Ratios (95% CI) for MetS and MetS Components According to Physical Activity Levels
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lunenfeld, B.; Stratton, P. The clinical consequences of an ageing world and preventive strategies. Best Pract. Res. Clin. Obstet. Gynaecol. 2013, 27, 643–659. [Google Scholar] [CrossRef]
- Jung, W.S.; Kim, Y.Y.; Park, H.Y. Circuit training improvements in Korean women with sarcopenia. Percept. Mot. Skills 2019, 126, 828–842. [Google Scholar] [CrossRef] [PubMed]
- Potes, Y.; Perez-Martinez, Z.; Bermejo-Millo, J.C.; Rubio-Gonzalez, A.; Fernandez-Fernandez, M.; Bermudez, M.; Arche, J.M.; Solano, J.J.; Boga, J.A.; Olivan, M.; et al. Overweight in the elderly induces a switch in energy metabolism that undermines muscle integrity. Aging Dis. 2019, 10, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; von Haehling, S.; Anker, S.D.; Vellas, B. From sarcopenia to frailty: A road less traveled. J. Cachexia Sarcopenia 2014, 5, 5–8. [Google Scholar] [CrossRef]
- Falahi, E.; Khalkhali Rad, A.H.; Roosta, S. What is the best biomarker for metabolic syndrome diagnosis? Diabetes Metab. Syndr. 2015, 9, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.H.; Kang, D.R.; Jang, J.Y.; Shin, J.H.; Kim, J.Y.; Choi, S.; Cho, E.J.; Park, J.S.; Sohn, I.S.; Jo, S.H.; et al. Metabolic syndrome epidemic among Korean adults: Korean survey of cardiometabolic syndrome (2018). Atherosclerosis 2018, 277, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.Y.; Yun, J.M. Analysis of the association between health-related and work-related factors among workers and metabolic syndrome using data from the Korean national health and nutrition examination Survey (2016). Nutr. Res. Pract. 2019, 13, 444–451. [Google Scholar] [CrossRef]
- Jun, S.H.; Shin, W.K. Association of soybean food intake and cardiometabolic syndrome in Korean women: Korea national health and nutrition examination survey (2007 to 2011). Diabetes Metab. 2020, 44, 143–157. [Google Scholar] [CrossRef]
- Kim, J.H.; Ha, J.I.; Park, J.M.; Lee, J.S.; Ahn, A.L.; Oh, E.J.; Choi, J.K.; Kweon, H.J.; Cho, D.Y. Association of high-risk drinking with metabolic syndrome and its components in elderly Korean men: The Korean national health and nutrition examination survey 2010–2012. Korean J. Fam. Med. 2018, 39, 233–238. [Google Scholar] [CrossRef]
- Dulloo, A.G.; Jacquet, J.; Solinas, G.; Montani, J.P.; Schutz, Y. Body composition phenotypes in pathways to obesity and the metabolic syndrome. Int. J. Obes. (2005) 2010, 34, S4–S17. [Google Scholar] [CrossRef]
- Bankoski, A.; Harris, T.B.; McClain, J.J.; Brychta, R.J.; Caserotti, P.; Chen, K.Y.; Berrigan, D.; Troiano, R.P.; Koster, A. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care 2011, 34, 497–503. [Google Scholar] [CrossRef]
- Martinho, K.O.; Dantas, E.H.; Longo, G.Z.; Ribeiro, A.Q.; Pereira, E.T.; Franco, F.S.; Goncalves, M.R.; de Morais, K.B.; Martins, M.V.; Danesio, J.; et al. Comparison of functional autonomy with associated sociodemographic factors, lifestyle, chronic diseases (CD) and neuropsychiatric factors in elderly patients with or without the metabolic syndrome (MS). Arch. Gerontol. Geriatr. 2013, 57, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Varghese, M.; Griffin, C.; Singer, K. The role of sex and sex hormones in regulating obesity-induced inflammation. Adv. Exp. Med. Biol. 2017, 1043, 65–86. [Google Scholar] [CrossRef] [PubMed]
- Batsis, J.A.; Villareal, D.T. Sarcopenic obesity in older adults: Aetiology, epidemiology and treatment strategies. Nat. Rev. Endocrinol. 2018, 14, 513–537. [Google Scholar] [CrossRef] [PubMed]
- Di Daniele, N.; Noce, A.; Vidiri, M.F.; Moriconi, E.; Marrone, G.; Annicchiarico-Petruzzelli, M.; D’Urso, G.; Tesauro, M.; Rovella, V.; De Lorenzo, A. Impact of mediterranean diet on metabolic syndrome, cancer and longevity. Oncotarget 2017, 8, 8947–8979. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.W. Obesity and metabolic syndrome in Korea. Diabetes Metab. J. 2011, 35, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Cho, S.I.; Park, H.S. Metabolic syndrome and cancer-related mortality among Korean men and women. Ann. Oncol. 2010, 21, 640–645. [Google Scholar] [CrossRef]
- Alvarez-Sanchez, N.; Alvarez-Rios, A.I.; Guerrero, J.M.; Garcia-Garcia, F.J.; Rodriguez-Manas, L.; Cruz-Chamorro, I.; Lardone, P.J.; Carrillo-Vico, A. Homocysteine and C-reactive protein levels are associated with frailty in older Spaniards: The Toledo Study for Healthy Aging. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2019. [Google Scholar] [CrossRef]
- Rahamon, S.K.; Fabian, U.A.; Charles-Davies, M.A.; Olaniyi, J.A.; Fasanmade, A.A.; Akinlade, K.S.; Oyewole, O.E.; Owolabi, M.O.; Adebusuyi, J.R.; Hassan, O.O.; et al. Changes in mediators of inflammation and pro-thrombosis after 12 months of dietary modification in adults with metabolic syndrome. Afr. Health Sci. 2017, 17, 453–462. [Google Scholar] [CrossRef][Green Version]
- Graziani, F.; Cialdella, P.; Liuzzo, G.; Basile, E.; Brugaletta, S.; Pedicino, D.; Leccesi, L.; Guidone, C.; Iaconelli, A.; Mingrone, G.; et al. Cardiovascular risk in obesity: Different activation of inflammation and immune system between obese and morbidly obese subjects. Eur. J. Intern. Med. 2011, 22, 418–423. [Google Scholar] [CrossRef]
- Seravalle, G.; Grassi, G. Sympathetic nervous system, hypertension, obesity and metabolic syndrome. High Blood Press. Cardiovasc. Prev. 2016, 23, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Corlier, F.; Hafzalla, G.; Faskowitz, J.; Kuller, L.H.; Becker, J.T.; Lopez, O.L.; Thompson, P.M.; Braskie, M.N. Systemic inflammation as a predictor of brain aging: Contributions of physical activity, metabolic risk, and genetic risk. NeuroImage 2018, 172, 118–129. [Google Scholar] [CrossRef]
- Hwang, H.; Jung, W.-S.; Kim, J.; Park, H.-Y.; Lim, K. Comparison of association between physical activity and resting metabolic rate in young and middle-aged Korean adults. J. Exerc. Nutr. Biochem. 2019, 23, 16. [Google Scholar] [CrossRef]
- Leslie, W.; Hankey, C. Aging, Nutritional Status and Health. Health 2015, 3, 648–658. [Google Scholar] [CrossRef] [PubMed]
- Remond, D.; Shahar, D.R.; Gille, D.; Pinto, P.; Kachal, J.; Peyron, M.A.; Dos Santos, C.N.; Walther, B.; Bordoni, A.; Dupont, D.; et al. Understanding the gastrointestinal tract of the elderly to develop dietary solutions that prevent malnutrition. Oncotarget 2015, 6, 13858–13898. [Google Scholar] [CrossRef] [PubMed]
- de Toro-Martin, J.; Arsenault, B.J.; Despres, J.P.; Vohl, M.C. Precision Nutrition: A Review of Personalized Nutritional Approaches for the Prevention and Management of Metabolic Syndrome. Nutrients 2017, 9, 913. [Google Scholar] [CrossRef] [PubMed]
- Freire, R.D.; Cardoso, M.A.; Gimeno, S.G.; Ferreira, S.R. Dietary fat is associated with metabolic syndrome in Japanese Brazilians. Diabetes Care 2005, 28, 1779–1785. [Google Scholar] [CrossRef]
- Kim, S.A.; Shin, S.; Ha, K.; Hwang, Y.; Park, Y.H.; Kang, M.S.; Joung, H. Effect of a balanced Korean diet on metabolic risk factors among overweight/obese Korean adults: A randomized controlled trial. Eur. J. Nutr. 2020. [Google Scholar] [CrossRef]
- Keller, H.H. Nutrition and health-related quality of life in frail older adults. J. Nutr. Health Aging 2004, 8, 245–252. [Google Scholar]
- National Cholesterol Education Program (NCEP); Expert Panel on Detection, Evaluation; Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final report. Circulation 2002, 106, 3143. [Google Scholar] [CrossRef]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. Diagnosis and management of the metabolic syndrome: An American heart association/national heart, lung, and blood institute scientific statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.H.; Lee, W.Y.; Kim, S.S.; Kang, J.H.; Kang, J.H.; Kim, K.K.; Kim, B.Y.; Kim, Y.H.; Kim, W.J.; Kim, E.M.; et al. 2018 Korean society for the study of obesity guideline for the management of obesity in Korea. J. Obes. Metab. Syndr. 2019, 28, 40–45. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Tuberculosis Report 2013; World Health Organization: Geneze, Switzerland, 2013. [Google Scholar]
- Lim, S.; Shin, H.; Song, J.H.; Kwak, S.H.; Kang, S.M.; Won Yoon, J.; Choi, S.H.; Cho, S.I.; Park, K.S.; Lee, H.K.; et al. Increasing prevalence of metabolic syndrome in Korea: The Korean national health and nutrition examination survey for 1998–2007. Diabetes Care 2011, 34, 1323–1328. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.T.; Jeong, B.Y.; Oh, J.K. The prevalence trend of metabolic syndrome and its components and risk factors in Korean adults: Results from the Korean national health and nutrition examination survey 2008–2013. BMC Public Health 2017, 17, 71. [Google Scholar] [CrossRef]
- Rosique-Esteban, N.; Babio, N.; Díaz-López, A.; Romaguera, D.; Alfredo Martínez, J.; Sanchez, V.M.; Schröder, H.; Estruch, R.; Vidal, J.; Buil-Cosiales, P.; et al. Leisure-time physical activity at moderate and high intensity is associated with parameters of body composition, muscle strength and sarcopenia in aged adults with obesity and metabolic syndrome from the PREDIMED-Plus study. Clin. Nutr. 2019, 38, 1324–1331. [Google Scholar] [CrossRef]
- Chung, P.K.; Zhao, Y.; Liu, J.D.; Quach, B. A canonical correlation analysis on the relationship between functional fitness and health-related quality of life in older adults. Arch. Gerontol. Geriatr. 2017, 68, 44–48. [Google Scholar] [CrossRef]
- Kim, S.W.; Jung, W.S.; Park, W. Twelve weeks of combined resistance and aerobic exercise improves cardiometabolic biomarkers and enhances red blood cell hemorheological function in obese older men: A randomized controlled trial. Int. J. Environ. Res. Public Health 2019, 16, 5020. [Google Scholar] [CrossRef]
- Park, E.; Kim, J. Gender- and age-specific prevalence of metabolic syndrome among Korean adults: Analysis of the fifth Korean national health and nutrition examination survey. J. Cardiovasc. Nurs. 2015, 30, 256–266. [Google Scholar] [CrossRef]
- Park, S.H.; Lee, K.S.; Park, H.Y. Dietary carbohydrate intake is associated with cardiovascular disease risk in Korean: Analysis of the third Korea national health and nutrition examination survey (KNHANES III). Int. J. Cardiol. 2010, 139, 234–240. [Google Scholar] [CrossRef]
- Amagasa, S.; Fukushima, N.; Kikuchi, H.; Takamiya, T.; Oka, K.; Inoue, S. Light and sporadic physical activity overlooked by current guidelines makes older women more active than older men. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 59. [Google Scholar] [CrossRef]
- Davis, M.G.; Fox, K.R. Physical activity patterns assessed by accelerometry in older people. Clin. Exp. Ophthalmol. 2007, 100, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Laaksonen, D.E.; Lakka, H.M.; Salonen, J.T.; Niskanen, L.K.; Rauramaa, R.; Lakka, T.A. Low levels of leisure-time physical activity and cardiorespiratory fitness predict development of the metabolic syndrome. Diabetes Care 2002, 25, 1612–1618. [Google Scholar] [CrossRef] [PubMed]
- Zbronska, I.; Medrela-Kuder, E. The level of physical activity in elderly persons with overweight and obesity. Rocz. Państw. Zakł. Hig. 2018, 69, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Pedišić, Ž.; Greblo, Z.; Phongsavan, P.; Milton, K.; Bauman, A.E. Are total, intensity- and domain-specific physical activity levels associated with life satisfaction among university students? PLoS ONE 2015, 10, e0118137. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, Y.; Won, C.W.; Lee, K.E.; Chon, D. Nutritional status and frailty in community-dwelling older Korean adults: The korean frailty and aging cohort study. J. Nutr. Health Aging 2018, 22, 774–778. [Google Scholar] [CrossRef]
- Pae, M.; Meydani, S.N.; Wu, D. The role of nutrition in enhancing immunity in aging. Aging Dis. 2012, 3, 91–129. [Google Scholar]
- Engelheart, S.; Brummer, R. Assessment of nutritional status in the elderly: A proposed function-driven model. Food Nutr. Res. 2018, 62. [Google Scholar] [CrossRef]
- Bong, Y.; Song, W. The effects of elastic band exercises and nutritional education on frailty, strength, and nutritional intake in elderly women. J. Exerc. Nutr. Biochem. 2020, 24, 37–45. [Google Scholar] [CrossRef]
- Yang, E.-J.; Bang, H.-M. Nutritional status and health risks of low income elderly women in Gwangju area. J. Nutr. Health 2008, 41, 65–76. [Google Scholar]
- Jung, H.J.; Song, W.O.; Paik, H.-Y.; Joung, H. Dietary characteristics of macronutrient intake and the status of metabolic syndrome among Koreans. Korean J. Nutr. 2011, 44, 119–130. [Google Scholar] [CrossRef]
- Irz, X.; Fratiglioni, L.; Kuosmanen, N.; Mazzocchi, M.; Modugno, L.; Nocella, G.; Shakersain, B.; Traill, W.B.; Xu, W.; Zanello, G. Sociodemographic determinants of diet quality of the EU elderly: A comparative analysis in four countries. Public Health Nutr. 2014, 17, 1177–1189. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Barrés, S.; Martin, N.; Canela, T.; García-Barco, M.; Basora, J.; Arija, V.; Project ATDOM-NUT Group. Dietary intake in the dependent elderly: Evaluation of the risk of nutritional deficit. J. Hum. Nutr. Diet. 2016, 29, 174–184. [Google Scholar] [CrossRef]
- Serrano-Sánchez, J.A.; Fernández-Rodríguez, M.J.; Sanchis-Moysi, J.; Rodríguez-Pérez, M.D.C.; Marcelino-Rodríguez, I.; Cabrera de León, A. Domain and intensity of physical activity are associated with metabolic syndrome: A population-based study. PLoS ONE 2019, 14, e0219798. [Google Scholar]
- Kim, Y.J.; Hwang, J.-Y.; Kim, H.; Park, S.; Kwon, O. Diet quality, physical activity, and their association with metabolic syndrome in Korean adults. Nutrition 2019, 59, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Jung, W.-S.; Hwang, H.; Kim, J.; Park, H.-Y.; Lim, K. Effect of interval exercise versus continuous exercise on excess post-exercise oxygen consumption during energy-homogenized exercise on a cycle ergometer. J. Exerc. Nutr. Biochem. 2019, 23, 45. [Google Scholar] [CrossRef]
| Variables | Total (n = 3720) | Male (n = 1586) | Female (n = 2134) | |||
|---|---|---|---|---|---|---|
| Non-MetS (n = 2347) | MetS (n = 1373) | Non-MetS (n = 1018) | MetS (n = 586) | Non-MetS (n = 1248) | MetS (n = 886) | |
| Age (years) | 72.8 ± 0.1 | 73.0 ± 0.1 | 72.7 ± 0.2 | 72.4 ± 0.2 | 72.8 ± 0.2 | 73.3 ± 0.2 |
| Height (cm) | 158.2 ± 0.2 | 157.0 ± 0.2 | 165.3 ± 0.2 | 165.9 ± 0.2 | 151.7 ± 0.2 | 151.9 ± 0.2 |
| Body weight (kg) | 57.7 ± 0.2 | 63.4 ± 0.2 | 62.4 ± 0.3 | 69.8 ± 0.4 | 53.4 ± 0.2 | 59.7 ± 0.3 |
| BMI (kg/m2) | 23.0 ± 0.1 | 25.7 ± 0.1 | 22.8 ± 0.1 | 25.3 ± 0.1 | 23.2 ± 0.1 | 25.9 ± 0.1 |
| Alcohol | 75.3 | 70.5 | 90.5 | 90.6 | 61.7 | 59.4 |
| Smoking | 39.3 | 32.3 | 77.1 | 80.5 | 5.7 | 5.5 |
| Waist circumference (cm) | 81.7 ± 0.2 | 89.7 ± 0.2 | 83.7 ± 0.3 | 92.0 ± 0.3 | 80.0 ± 0.2 | 88.4 ± 0.2 |
| TG (mg/dL) | 102.6 ± 1.0 | 173.2 ± 2.5 | 103.1 ± 1.6 | 183.3 ± 3.8 | 102.1 ± 1.2 | 167.3 ± 3.2 |
| HDL-C (mg/dL) | 52.1 ± 0.3 | 42.8 ± 0.2 | 49.3 ± 0.4 | 40.4 ± 0.4 | 54.6 ± 0.4 | 44.1 ± 0.3 |
| SBP (mmHg) | 125.5 ± 0.4 | 132.4 ± 0.4 | 123.8 ± 0.5 | 130.2 ± 0.7 | 127.0 ± 0.5 | 133.6 ± 0.5 |
| DBP (mmHg) | 71.7 ± 0.2 | 73.0 ± 0.3 | 71.6 ± 0.3 | 72.4 ± 0.4 | 71.7 ± 0.3 | 73.4 ± 0.3 |
| Fasting glucose (mg/dL) | 100.3 ± 0.4 | 118.5 ± 0.8 | 102.6 ± 0.7 | 122.9 ± 1.5 | 98.2 ± 0.5 | 116.0 ± 0.9 |
| Mets (%) | 63.1 | 36.9 | 69.2 | 30.8 | 58.5 | 41.5 |
| Occupational activity: vigorous | 20.2 ± 7.6 | 35.6 ± 16.2 | 32.0 ± 13.9 | 71.1 ± 37.6 | 9.4 ± 7.0 | 15.2 ± 13.4 |
| Occupational activity: moderate | 55.0 ± 12.2 | 49.3 ± 10.6 | 55.3 ± 14.8 | 46.8 ± 14.4 | 54.62 ± 19.1 | 50.7 ± 14.6 |
| Place movement | 399.3 ± 15.3 | 322.4 ± 14.0 | 424.9 ± 24.4 | 362.9 ± 26.0 | 375.9 ± 18.9 | 299.2 ± 16.3 |
| Recreational activity: vigorous | 30.4 ± 7.2 | 26.2 ± 6.2 | 54.2 ± 14.5 | 57.0 ± 14.2 | 8.7 ± 3.4 | 8.5 ± 5.4 |
| Recreational activity: moderate | 108.2 ± 8.7 | 73.0 ± 7.1 | 148.0 ± 15.0 | 139.3 ± 16.9 | 71.7 ± 9.3 | 34.8 ± 5.3 |
| Total physical activity | 613.1 ± 25.3 | 506.4 ± 29.3 | 714.3 ± 40.5 | 677.1 ± 60.1 | 520.3 ± 30.9 | 408.3 ± 30.3 |
| Total energy intake (kcal) | 1677.3 ± 15.4 | 1572.1 ± 16.2 | 1898.2 ± 21.8 | 1891.9 ± 28.6 | 1475.1 ± 19.8 | 1388.3 ± 17.2 |
| Carbohydrate intake (kcal) | 1175.9 ± 10.9 | 1114.9 ± 10.9 | 1285.7 ± 14.8 | 1275.0 ± 18.3 | 1075.3 ± 15.3 | 1022.8 ± 12.8 |
| Protein intake (kcal) | 252.3 ± 4.3 | 227.7 ± 4.7 | 287.4 ± 6.4 | 288.7 ± 9.2 | 220.1 ± 5.5 | 192.6 ± 4.9 |
| Fat intake (kcal) | 225.7 ± 2.6 | 207.5 ± 2.7 | 260.3 ± 4.0 | 255.2 ± 5.0 | 194.0 ± 3.0 | 180.1 ± 2.8 |
| Carbohydrate intake (%) | 71.3 ± 0.3 | 72.6 ± 0.3 | 68.9 ± 0.4 | 69.2 ± 0.5 | 73.5 ± 0.3 | 74.5 ± 0.3 |
| Protein intake (%) | 13.4 ± 0.1 | 13.1 ± 0.1 | 13.6 ± 0.1 | 13.3 ± 0.1 | 13.1 ± 0.1 | 12.9 ± 0.1 |
| Fat intake (%) | 14.4 ± 0.2 | 13.7 ± 0.2 | 14.6 ± 0.2 | 14.4 ± 0.3 | 14.2 ± 0.2 | 13.2 ± 0.2 |
| Physical Activity (MET × min/Week) | Group | Total | Male | Female | p-Value | ANOVA | |||
|---|---|---|---|---|---|---|---|---|---|
| F-Value | p-Value (η2) | Power | |||||||
| Occupational vigorous | Non-MetS | 20.2 ± 7.6 | 32.0 ± 13.9 | 9.4 ± 7.0 | 0.148 | S | 5.118 | 0.024 (0.001) | 0.619 |
| MetS | 35.6 ± 16.2 | 71.1 ± 37.6 | 15.2 ± 13.4 | 0.162 | M | 1.678 | 0.195 (0.000) | 0.254 | |
| p-value | 0.364 | 0.329 | 0.704 | S × M | 0.926 | 0.336 (0.000) | 0.161 | ||
| Occupational moderate | Non-MetS | 55.0 ± 12.2 | 55.3 ± 14.8 | 54.62 ± 19.06 | 0.977 | S | 0.009 | 0.925 (0.000) | 0.051 |
| MetS | 49.3 ± 10.6 | 46.8 ± 14.4 | 50.69 ± 14.56 | 0.861 | M | 0.136 | 0.713 (0.000) | 0.066 | |
| p-value | 0.731 | 0.697 | 0.869 | S × M | 0.018 | 0.893 (0.000) | 0.052 | ||
| Place movement | Non-MetS | 399.3 ± 15.3 | 424.9 ± 24.4 | 375.9 ± 18.9 | 0.112 | S | 6.889 | 0.009 (0.002) | 0.747 |
| MetS | 322.4 ± 14.0 | 362.9 ± 26.0 | 299.2 ± 16.3 | 0.038 * | M | 10.439 | 0.001 (0.003) | 0.898 | |
| p-value | < 0.001 *** | 0.082 | 0.002 ** | S × M | 0.116 | 0.733 (0.000) | 0.063 | ||
| Recreational vigorous | Non-MetS | 30.4 ± 7.2 | 54.2 ± 14.5 | 8.7 ± 3.4 | 0.002 ** | S | 22.790 | 0.000 (0.006) | 0.998 |
| MetS | 26.2 ± 6.2 | 57.0 ± 14.2 | 8.5 ± 5.4 | <0.001 *** | M | 0.018 | 0.894 (0.000) | 0.052 | |
| p-value | 0.661 | 0.894 | 0.974 | S × M | 0.024 | 0.877 (0.000) | 0.053 | ||
| Recreational moderate | Non-MetS | 108.2 ± 8.7 | 148.0 ± 15.0 | 71.7 ± 9.3 | <0.001 *** | S | 59.790 | 0.000 (0.016) | 10.000 |
| MetS | 73.0 ± 7.1 | 139.3 ± 16.9 | 34.8 ± 5.3 | <0.001 *** | M | 3.811 | 0.051 (0.001) | 0.497 | |
| p-value | 0.002 ** | 0.706 | 0.001 ** | S × M | 1.458 | 0.227 (0.000) | 0.227 | ||
| Total physical activity | Non-MetS | 613.1 ± 25.3 | 714.3 ± 40.5 | 520.3 ± 30.9 | <0.001 *** | S | 34.916 | 0.000 (0.009) | 10.000 |
| MetS | 506.4 ± 29.3 | 677.1 ± 60.1 | 408.3 ± 30.3 | <0.001 *** | M | 3.634 | 0.057 (0.001) | 0.478 | |
| p-value | 0.006 ** | 0.593 | 0.010 * | S × M | 0.911 | 0.340 (0.000) | 0.159 | ||
| Variables | Group | Total | Male | Female | p-Value | ANOVA | |||
|---|---|---|---|---|---|---|---|---|---|
| F-Value | p-Value (η2) | Power | |||||||
| Total energyintake (kcal) | Non-MetS | 1677.3 ± 15.4 | 1898.2 ± 21.8 | 1475.1 ± 19.8 | <0.001 *** | S | 460.451 | 0.000 (0.110) | 1.000 |
| MetS | 1572.1 ± 16.2 | 1891.9 ± 28.6 | 1388.3 ± 17.2 | <0.001 *** | M | 4.652 | 0.031 (0.001) | 0.578 | |
| p-value | <0.001 *** | 0.859 | 0.001 ** | S × M | 3.479 | 0.062 (0.001) | 0.462 | ||
| Carbohydrate intake (kcal) | Non-MetS | 1175.9 ± 10.9 | 1285.7 ± 14.8 | 1075.3 ± 15.3 | <0.001 *** | S | 224.853 | 0.000 (0.057) | 1.000 |
| MetS | 1114.9 ± 10.9 | 1275.0 ± 18.3 | 1022.8 ± 12.8 | <0.001 *** | M | 4.188 | 0.041 (0.001) | 0.534 | |
| p-value | <0.001 *** | 0.650 | 0.008 ** | S × M | 1.832 | 0.176 (0.000) | 0.272 | ||
| Fat intake (kcal) | Non-MetS | 252.3 ± 4.3 | 287.4 ± 6.4 | 220.1 ± 5.5 | <0.001 *** | S | 165.840 | 0.000 (0.043) | 1.000 |
| MetS | 227.7 ± 4.7 | 288.7 ± 9.2 | 192.6 ± 4.9 | <0.001 *** | M | 4.255 | 0.039 (0.001) | 0.541 | |
| p-value | <0.001 *** | 0.901 | <0.001 *** | S × M | 5.177 | 0.023 (0.001) | 0.624 | ||
| Protein intake (kcal) | Non-MetS | 225.7 ± 2.6 | 260.3 ± 4.0 | 194.0 ± 3.0 | <0.001 *** | S | 376.450 | 0.000 (0.092) | 1.000 |
| MetS | 207.5 ± 2.7 | 255.2 ± 5.0 | 180.1 ± 2.8 | <0.001 *** | M | 6.834 | 0.009 (0.002) | 0.743 | |
| p-value | <0.001 *** | 0.422 | 0.001 ** | S × M | 1.457 | 0.227 (0.000) | 0.226 | ||
| Physical Activity Level | MET min/Week (Mean ± SE) | ||||
|---|---|---|---|---|---|
| Total | n | Male | n | Female | |
| Inactive (n = 2084) | 32.2 ± 1.6 | 836 | 32.2 ± 2.5 | 1248 | 32.3 ± 2.0 |
| Somewhat active (n = 439) | 402.1 ± 3.3 | 166 | 397.9 ± 5.2 | 273 | 404.6 ± 4.2 |
| Active (n = 585) | 731.0 ± 5.6 | 251 | 735.8 ± 8.8 | 334 | 727.5 ± 7.1 |
| Very active (n = 612) | 2333.2 ± 82.4 | 333 | 2499.1 ± 114.1 | 279 | 2135.2 ± 118.1 |
| Physical Activity Group | MetS | High Waist Circumference | High Triglycerides | Low HDL-C | High Blood Pressure | High Glucose |
|---|---|---|---|---|---|---|
| Inactive (n = 2084) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Somewhat active (n = 439) | 1.03 (0.83–1.29) | 0.91 (0.74–1.14) | 0.96 (0.77–1.21) | 0.88 (0.72–1.08) | 1.08 (0.87–1.33) | 0.99 (0.80–1.23) |
| Active (n = 585) | 0.81 (0.66–0.98) * | 0.80 (0.66–0.96) * | 0.96 (0.79–1.18) | 0.86 (0.72–1.04) | 0.88 (0.73–1.06) | 0.86 (0.72–1.04) |
| Very active (n = 612) | 0.72 (0.59–0.88) ** | 0.77 (0.64–0.93) ** | 0.79 (0.65–0.97) * | 0.64 (0.53–0.77) *** | 0.82 (0.69–0.99) * | 0.85 (0.71–1.02) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, W.-S.; Park, H.-Y.; Kim, S.-W.; Lim, K. Sex-Specific Energy Intakes and Physical Activity Levels According to the Presence of Metabolic Syndrome in Korean Elderly People: Korean National Health and Nutrition Examination Survey 2016–2018. Int. J. Environ. Res. Public Health 2020, 17, 5416. https://doi.org/10.3390/ijerph17155416
Jung W-S, Park H-Y, Kim S-W, Lim K. Sex-Specific Energy Intakes and Physical Activity Levels According to the Presence of Metabolic Syndrome in Korean Elderly People: Korean National Health and Nutrition Examination Survey 2016–2018. International Journal of Environmental Research and Public Health. 2020; 17(15):5416. https://doi.org/10.3390/ijerph17155416
Chicago/Turabian StyleJung, Won-Sang, Hun-Young Park, Sung-Woo Kim, and Kiwon Lim. 2020. "Sex-Specific Energy Intakes and Physical Activity Levels According to the Presence of Metabolic Syndrome in Korean Elderly People: Korean National Health and Nutrition Examination Survey 2016–2018" International Journal of Environmental Research and Public Health 17, no. 15: 5416. https://doi.org/10.3390/ijerph17155416
APA StyleJung, W.-S., Park, H.-Y., Kim, S.-W., & Lim, K. (2020). Sex-Specific Energy Intakes and Physical Activity Levels According to the Presence of Metabolic Syndrome in Korean Elderly People: Korean National Health and Nutrition Examination Survey 2016–2018. International Journal of Environmental Research and Public Health, 17(15), 5416. https://doi.org/10.3390/ijerph17155416








