Characteristics of Type-2 Diabetics Who are Prone to High-Cost Medical Care Expenses by Bayesian Network
Abstract
1. Introduction
2. Methods
2.1. Data Sources
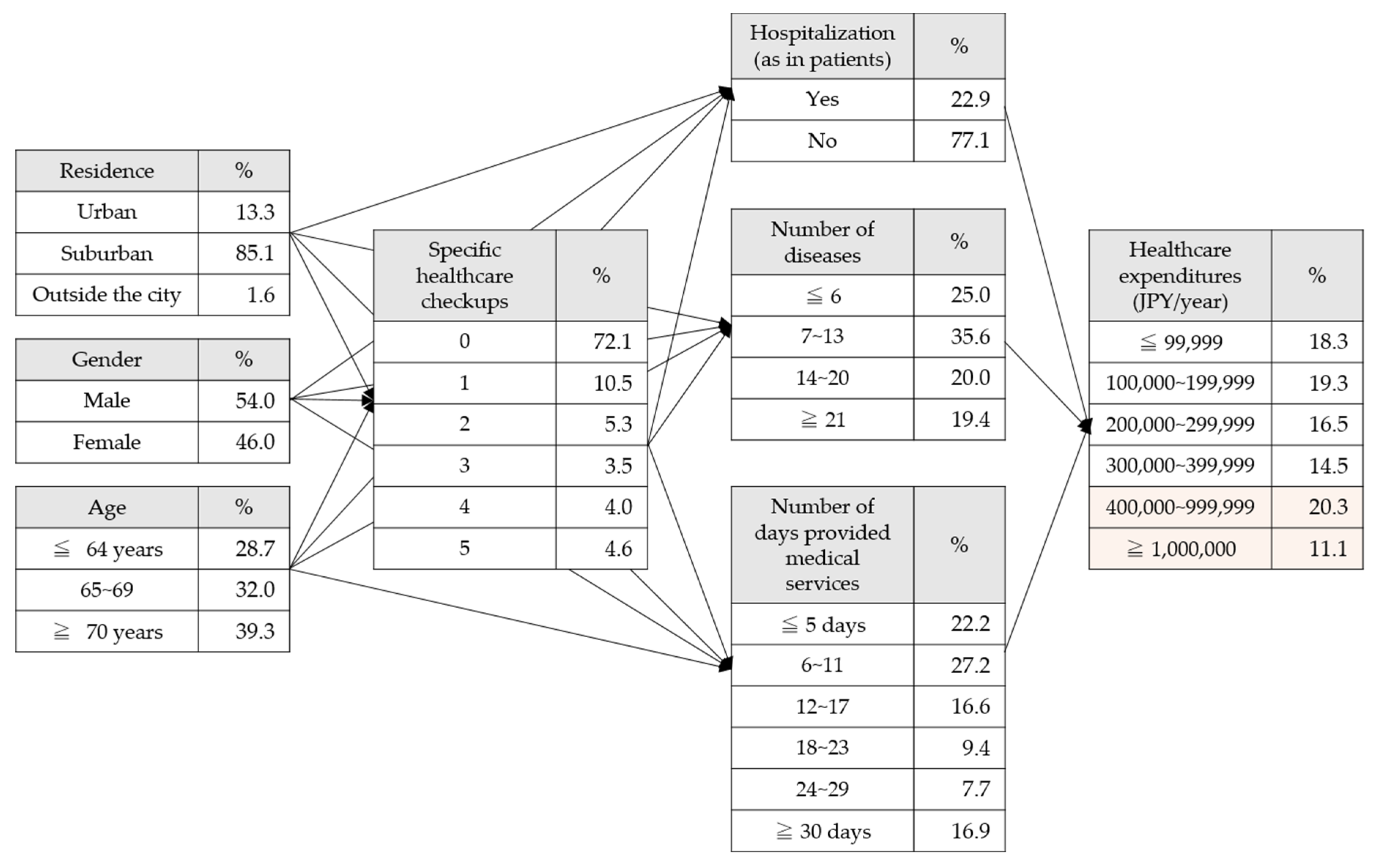
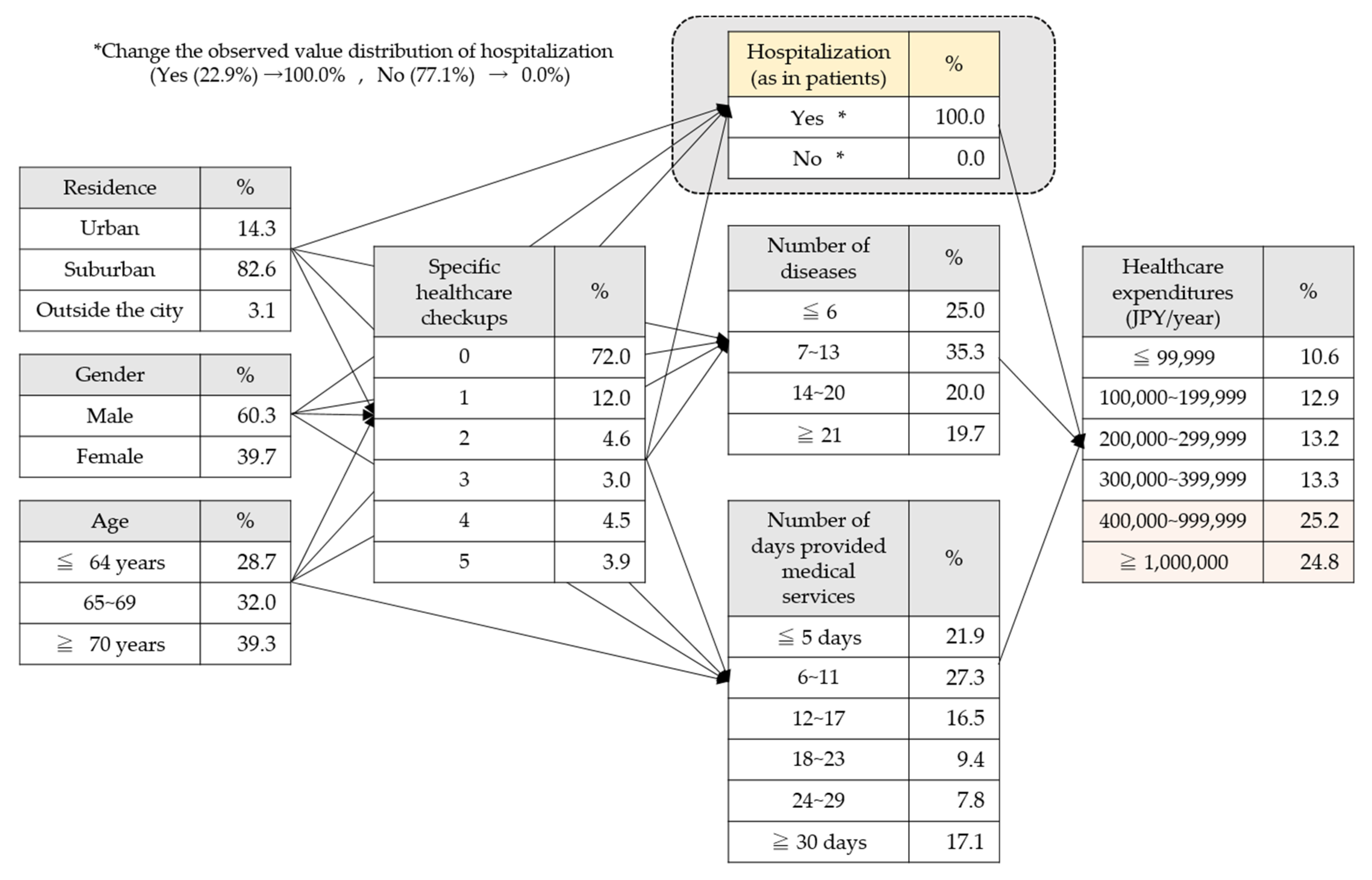
2.2. Data Analysis
- (1)
- Decision to undergo specific health checkups varies depending on age, gender, and area of residence;
- (2)
- Disease detection, hospital visits, and hospitalization changes based on specific health checkups;
- (3)
- Healthcare expenditure varies depending on the degree of the disease.
2.3. Ethical Considerations
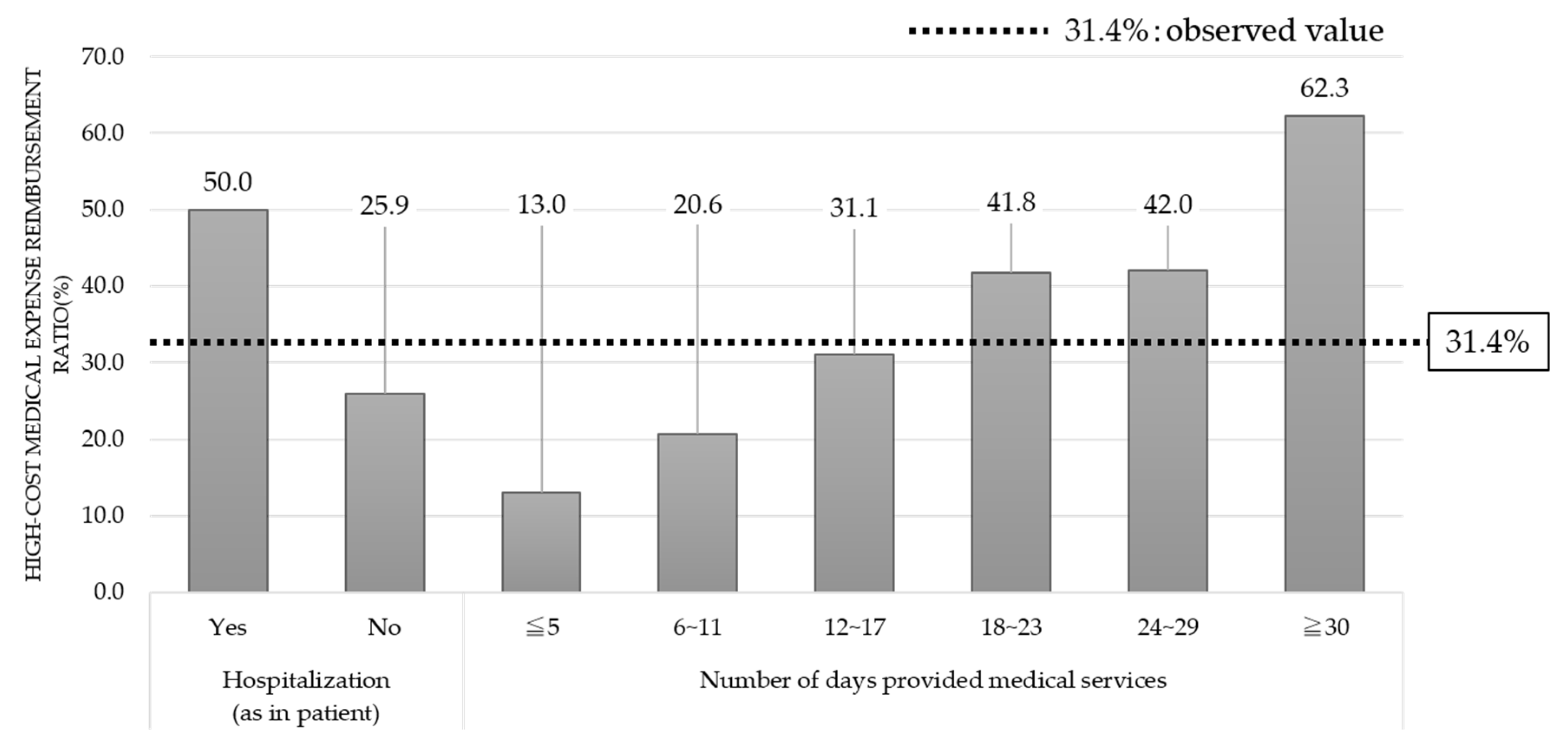
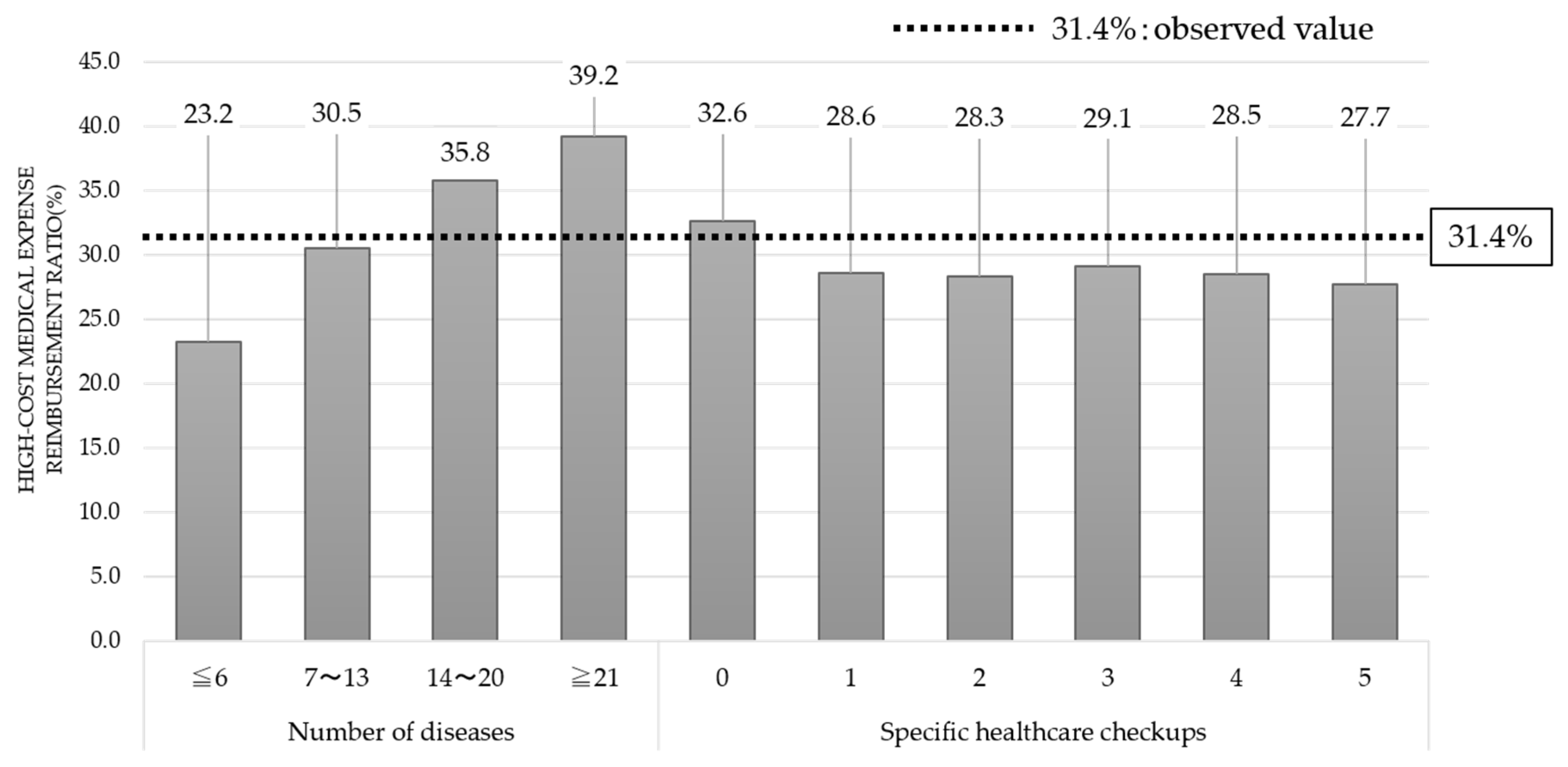
3. Results
4. Discussion
4.1. Presence or Absence of Hospitalization
4.2. Number of Days Provided Medical Services
4.3. Number of Diseases Listed on Medical Insurance Receipts
4.4. Number of Specific Healthcare Checkups
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ogurtsova, K.; Da Rocha Fernandes, J.D.; Huang, Y.; Linnenkamp, U.; Guariguata, L.; Cho, N.H.; Cavan, D.; Shaw, J.E.; Makaroff, L.E. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res. Clin. Pract. 2017, 128, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Da Rocha Fernandes, J.; Ogurtsova, K.; Linnenkamp, U.; Guariguata, L.; Seuring, T.; Zhang, P.; Cavan, D.; Makaroff, L.E. IDF Diabetes Atlas estimates of 2014 global health expenditures on diabetes. Diabetes Res. Clin. Pract. 2016, 117, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Leung, M.Y.M.; Pollack, L.M.; Colditz, G.A.; Chang, S.H. Life years lost and lifetime health care expenditures associated with diabetes in the US, National Health Interview Survey, 1997–2000. Diabetes Care 2015, 38, 460–468. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare. Overview of 2016 National Healthcare Expenditure; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2018. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/k-iryohi/16/index.html (accessed on 1 April 2020).
- OECD. OECD Health Statistics 2019; OECD: Paris, France, 2019; Available online: http://www.oecd.org/els/health-systems/health-data.htm (accessed on 1 April 2020).
- The Japanese Society for Dialysis Therapy. Current Status of Chronic Dialysis Therapy in Japan; The Japanese Society for Dialysis Therapy: Tokyo, Japan, 2017; Available online: https://docs.jsdt.or.jp/overview/index2017.html (accessed on 1 April 2020).
- Will, J.C.; Galuska, D.A.; Ford, E.S.; Mokdad, A.; Calle, E.E. Cigarette smoking and diabetes mellitus: Evidence of positive association from a large prospective cohort study. Int. J. Epidemiol. 2001, 3, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, T.; Fujiwara, T.; Ohba, H.; Suzuki, T.; Ogasawara, K. Forecasting the regional distribution and sufficiency of physicians in Japan with a coupled system dynamics—Geographic information system model. Hum. Resour. Health 2017, 12–15, 64. [Google Scholar] [CrossRef] [PubMed]
- Pearl, J.; Mackenzie, D. The Book of Why: The New Science of Cause and Effect; Penguin Books: London, UK, 2018; pp. 347–369. [Google Scholar]
- Murakami, T.; Suyama, A.; Orihira, R. Consumer behavior modeling using bayesian networks. In Proceedings of the The 18th Annual Conference of the Japanese Society for Artificial Intelligence, Kanazawa, Japan, 2–4 June 2004; Volume 3F3-01, p. 18. [Google Scholar] [CrossRef]
- Miyauchi, Y.; Nishimura, H. Construction of Bayesian Network Corresponding to the Framework of the Specific Health Checkup. Trans. Jpn. Soc. Kansei Eng. 2013, 12, 455–463. [Google Scholar] [CrossRef]
- Suzuki, T.; Shimoda, T.; Takahashi, N.; Tsutsumi, K.; Samukawa, M.; Yoshimura, S.; Ogasawara, K. Factors Affecting Bone Mineral Density Among Snowy Region Residents in Japan: Analysis Using Multiple Linear Regression and Bayesian Network Model. Interact. J. Med. Res. 2018, 7, e10. [Google Scholar] [CrossRef] [PubMed]
- Velikova, M.; Terwisscha, J.; Lucas, P.J.F.; Spaandermanc, M. Exploiting causal functional relationships in Bayesian network modelling for personalised healthcare. Int. J. Approx. Reason. 2014, 55, 59–73. [Google Scholar] [CrossRef]
- Charmaine, S.N.; Matthias, P.H.S.T.; Yu, K.; Joyce, Y.L. Direct medical cost of type 2 diabetes in Singapore. PLoS ONE 2015, 10, e0122795. [Google Scholar] [CrossRef]
- Maeda, Y. International Comparison of Medical Data—OECD Health Statistics 2016; Report No: 407; Medical Association Research Institute: Tokyo, Japan, 2018. [Google Scholar]
- Samnaliev, M.; Noh, H.L.; Sonneville, K.R.; Austin, S.B. The economic burden of eating disorders and related mental health comorbidities: An exploratory analysis using the US Medical Expenditures Panel Survey. Prev. Med. Rep. 2015, 2, 32–34. [Google Scholar] [CrossRef]
- Rudisill, C.; Charlton, J.; Booth, H.P.; Gulliford, M.C. Are healthcare costs from obesity associated with body mass index, comorbidity or depression? Cohort study using electronic health records. Clin. Obes. 2016, 6, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Wacker, M.E.; Jörres, R.A.; Schulz, H.; Heinrich, J.; Karrasch, S.; Karch, A.; Koch, A.; Peters, A.; Leidl, R.; Vogelmeier, C.; et al. Direct and indirect costs of COPD and its comorbidities: Results from the German COSYCONET study. Respir. Med. 2016, 111, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Akena, D.; Kadama, P.; Ashaba, S.; Akello, C.; Kwesiga, B.; Rejani, L.; Okello, J.; Mwesiga, E.K.; Obuku, E.A. The association between depression, quality of life, and the health care expenditure of patients with diabetes mellitus in Uganda. J. Affect. Disord. 2015, 174, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, K. The relationship between undergoing a basic health checkup based on the health and medical services law for the aged and medical expenditure covered under the national health insurance in Japan. Jpn. J. Hyg. 2002, 56, 673–681. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Seuring, T.; Archangelidi, O.; Suhrcke, M. The economic costs of type 2 diabetes: A global systematic review. Pharmacoeconomics 2015, 33, 811–831. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sase, Y.; Kumagai, D.; Suzuki, T.; Yamashina, H.; Tani, Y.; Fujiwara, K.; Tanikawa, T.; Enomoto, H.; Aoyama, T.; Nagai, W.; et al. Characteristics of Type-2 Diabetics Who are Prone to High-Cost Medical Care Expenses by Bayesian Network. Int. J. Environ. Res. Public Health 2020, 17, 5271. https://doi.org/10.3390/ijerph17155271
Sase Y, Kumagai D, Suzuki T, Yamashina H, Tani Y, Fujiwara K, Tanikawa T, Enomoto H, Aoyama T, Nagai W, et al. Characteristics of Type-2 Diabetics Who are Prone to High-Cost Medical Care Expenses by Bayesian Network. International Journal of Environmental Research and Public Health. 2020; 17(15):5271. https://doi.org/10.3390/ijerph17155271
Chicago/Turabian StyleSase, Yuji, Daiki Kumagai, Teppei Suzuki, Hiroko Yamashina, Yuji Tani, Kensuke Fujiwara, Takumi Tanikawa, Hisashi Enomoto, Takeshi Aoyama, Wataru Nagai, and et al. 2020. "Characteristics of Type-2 Diabetics Who are Prone to High-Cost Medical Care Expenses by Bayesian Network" International Journal of Environmental Research and Public Health 17, no. 15: 5271. https://doi.org/10.3390/ijerph17155271
APA StyleSase, Y., Kumagai, D., Suzuki, T., Yamashina, H., Tani, Y., Fujiwara, K., Tanikawa, T., Enomoto, H., Aoyama, T., Nagai, W., & Ogasawara, K. (2020). Characteristics of Type-2 Diabetics Who are Prone to High-Cost Medical Care Expenses by Bayesian Network. International Journal of Environmental Research and Public Health, 17(15), 5271. https://doi.org/10.3390/ijerph17155271




