Patient Satisfaction in the Peruvian Health Services: Validation and Application of the HEALTHQUAL Scale
Abstract
1. Introduction
1.1. Quality of the Services in Hospital Management
1.2. Public–Private Associations (PPPs) as an Organization Model in Health
1.3. The HEALTHQUAL Scale, Dimensions, and Items
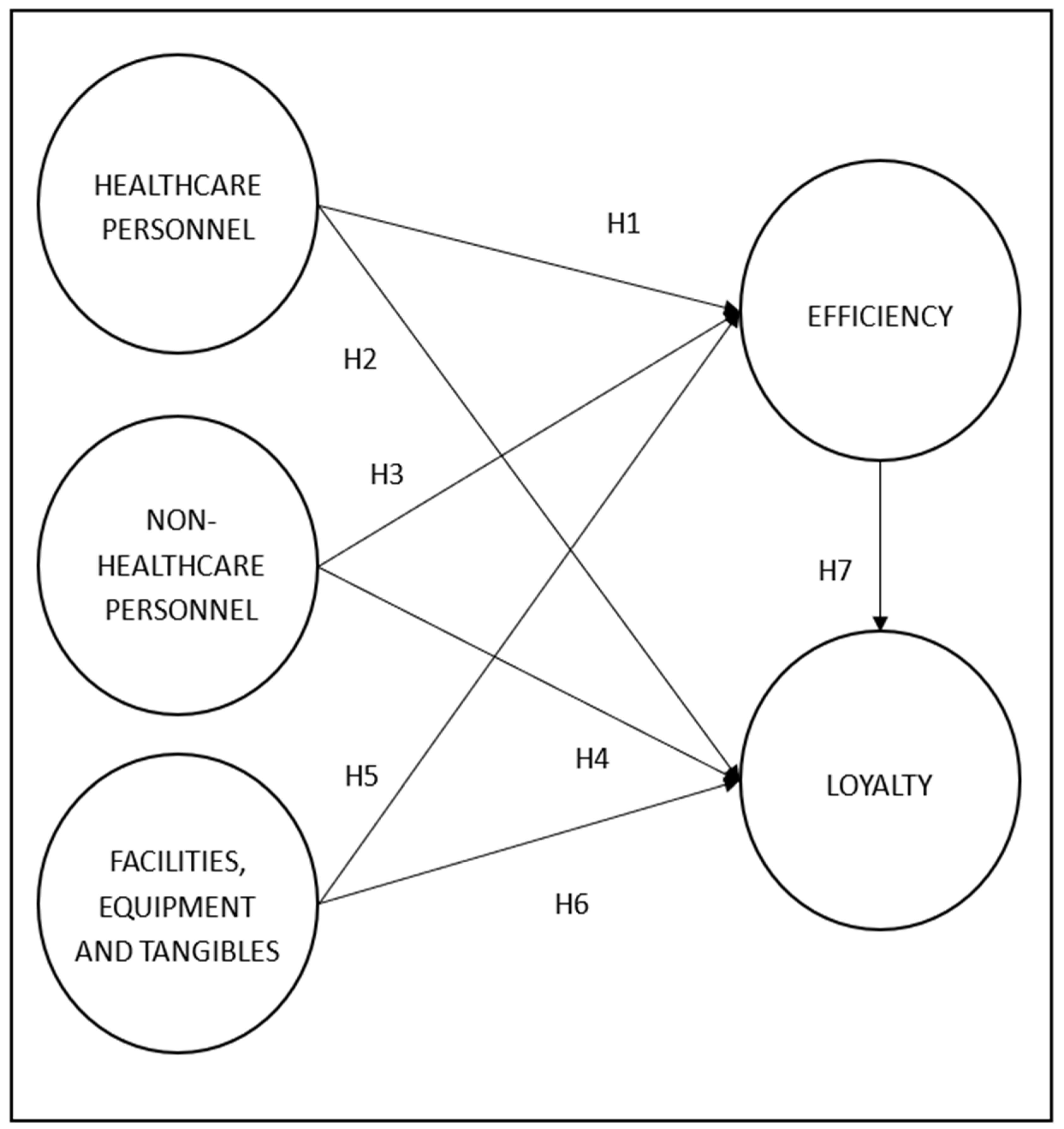
1.4. Research Model and Hypothesis
1.4.1. Healthcare Personnel Dimension (HP)
- H1: The better the performance of healthcare personnel, the greater the efficiency in healthcare; and
- H2: The better the performance of healthcare personnel, the greater loyalty of users to the healthcare service.
1.4.2. Nonhealthcare Personnel Dimension (NHP)
- H3: The better the performance of nonhealthcare personnel, the greater the efficiency in healthcare; and
- H4: The better the performance of nonhealthcare personnel, the greater loyalty of the user to the healthcare services.
1.4.3. Facilities, Equipment, and Tangible Dimension (FET)
- H5: The better the conditions of the facilities, equipment, and tangibles, the greater the efficiency in healthcare; and
- H6: The better the conditions of the facilities, equipment, and tangibles, the greater the loyalty of the user to the healthcare service.
1.4.4. Relationship Between Efficiency (EFI) and Loyalty (L)
- H7: The greater the efficiency of the healthcare service provided, the greater the patient’s loyalty to that healthcare service.
- H1: Healthcare personnel positively impact efficiency;
- H2: Healthcare personnel positively impact loyalty;
- H3: Nonhealthcare personnel positively impact efficiency;
- H4: Nonhealthcare personnel positively impact loyalty;
- H5: Facilities, equipment, and tangibles positively impact efficiency;
- H6: Facilities, equipment and tangibles positively impact loyalty; and
- H7: Efficiency positively impacts loyalty.
2. Materials and Methods
2.1. Measurement Instrument
2.2. Variables
2.3. Application of the Questionnaire
2.4. Data Processing and Analysis
3. Results
3.1. Global Model
3.2. Measurement Model
3.3. Structural Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Forrellat-Barrios, M. Calidad en los servicios de salud: Un reto ineludible. Rev. Cuba. Hematol. Inmunol. Hemoter. 2014, 30, 179–183. Available online: http://scielo.sld.cu/pdf/hih/v30n2/hih11214 (accessed on 10 July 2020).
- Perera, R.; Dowell, T.; Crampton, P.; Kearns, R. Panning for gold: An evidence-based tool for assessment of performance indicators in primary health care. Health Policy 2007, 80, 314–327. [Google Scholar] [CrossRef] [PubMed]
- Barreiro, L. Orientación al cliente. In Estrategia Organizacional; Editorial Félix Varela: La Habana, Cuba, 2010; Chapter 1; p. 544. [Google Scholar]
- Díaz, Y. Procedimiento Para la Evaluación de la Calidad de Servicio Percibida por Los Clientes de Empresas Cubanas de Servicios. Validación a Las Instituciones Bancarias. Ph.D. Dissertation, Universidad Central Marta Abreu de Las Villas, Santa Clara, Cuba, 2010. [Google Scholar]
- Pérez, A. La Gestión del Sistema de Calidad Basado en Valores en los Servicios Hoteleros. Ph.D. Dissertation, Universidad de Camagüey, Camagüey, Cuba, 2013. [Google Scholar]
- Ipinza Riveros, M. Calidad y Atención Integral de Salud: Dos conceptos inseparables. Cuadernos Médico Sociales 2007, 47, 5–17. Available online: https://es.slideshare.net/alexmanolo/calidad-y-atencion-integral-de-salud (accessed on 10 July 2020).
- Rodríguez, A. Creando una cultura de la calidad hospitalaria. Medwave 2013, 13, e5810. [Google Scholar] [CrossRef]
- Donabedian, A.; Gómez, O. Garantía y Monitoría de la Calidad de Atención Médica: Un Texto Introductorio; Instituto Nacional de Salud Pública: Cuernavaca, México, 1990. [Google Scholar]
- Miranda, F.J.; Chamorro, A.; Murillo, L.R.; Vega, J. Primary health care services quality in Spain. Int. J. Qual. Serv. Scienc. 2012, 4, 387–398. [Google Scholar] [CrossRef]
- Tsu-Ming, Y. Determining medical service improvement priority by integrating the refined Kano model, Quality function deployment and Fuzzy integrals. Afr. J. Bus. Manag. 2010, 4, 2534–2545. Available online: http://www.academicjournals.org/AJBM (accessed on 10 July 2020).
- De Man, S.; Gemmel, P.; Vlerick, P. Patients’ and personnel’s perceptions of service quality and patient satisfaction in nuclear medicine. Eur. J. Nucl. Med. 2002, 29, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Freudenberg, L.S.; Beyer, T.; Bockisch, A. Improving perceptions of the quality of service in nuclear medicine. Eur. J. Nucl. Med. 2003, 30, 472. [Google Scholar] [CrossRef] [PubMed]
- Linder-Pelz, S. Toward a theory of patient satisfaction. Soc. Sci. Med. 1982, 16, 577–582. [Google Scholar] [CrossRef]
- Naidu, A. Factors affecting patient satisfaction and healthcare quality. Int. J. Health Care Qual. Assur. 2009, 22, 366–381. [Google Scholar] [CrossRef]
- Tucker, J.; Adams, S. Incorporating patients’ assessments of satisfaction and quality: An integrative model of patients’ evaluations of their care. Manag. Serv. Qual. An Int. J. 2001, 11, 272–287. [Google Scholar] [CrossRef]
- Zeithaml, V.; Berry, L.; Parasuraman, A. The behavioral consequences of service quality. J. Mark. 1996, 60, 31–46. [Google Scholar] [CrossRef]
- Zeithaml, V.A. Consumer perceptions of price, quality, and value: A means-end model and synthesis of evidence. J. Mark. 1988, 52, 2–22. Available online: https://www.jstor.org/stable/1251446 (accessed on 10 July 2020). [CrossRef]
- Zaibaf, M.; Taherikia, F.; Fakharian, M. Effect of perceived service quality on customer satisfaction in hospitality industry: Gronroos’ service quality model development. J. Hosp. Mark. Manag. 2013, 22, 409–504. [Google Scholar] [CrossRef]
- Miranda-Veloso, C.; Paula-Montes, A. Validation of a measurement scale of service quality, image, customer satisfaction and loyalty in traditional trade. Tour. Manag. Stud. 2019, 15, 27–35. [Google Scholar] [CrossRef]
- World Bank. Best Practices in Public-Private Partnerships Financing in Latin America: The Role of Innovative Approach; World Bank: Washington, DC, USA, 2012; Available online: https://www.gihub.org/resources/publications/best-practices-in-public-private-partnerships-financing-in-latin-america-the-role-of-innovative-approaches-subsidies/ (accessed on 10 July 2020).
- Banco Mundial. Guía de Referencia de Asociaciones Público Privadas Versión 2.0. Washington: Publicaciones del Banco Mundial; The World Bank Group: Washington, DC, USA, 2014; Available online: https://consultations.worldbank.org/sites/default/files/materials/consultation-template/public-private-partnerships-reference-guideopenconsultationtemplate/materials/pppreferenceguidev02sp (accessed on 10 July 2020).
- OECD. Public-Private Partnerships: In Pursuit of Risk Sharing and Value for Money; OECD Publishing: Paris, France, 2008. [Google Scholar] [CrossRef]
- Stemmer, E. Contractual Structures and Risk allocation and Mitigation in the Context of Public Private Partnerships in the Health Sector; World Bank: Washington, DC, USA, 2008; Available online: http://documents.worldbank.org/curated/en/976241468339052434/Contractual-structures-and-risk-allocation-and-mitigation-in-the-context-of-public-private-partnerships-in-the-health-sector (accessed on 10 July 2020).
- Torres De Mastle, C.; Encinas, J.; Farquharson, E.; Yescombe, E.R. How to Engage with the Private Sector in Public-Private Partnerships in Emerging Markets; World Bank Group: Washington, DC, USA, 2011; Available online: http://documents.worldbank.org/curated/en/995241468337913618/How-to-engage-with-the-private-sector-in-public-private-partnerships-in-emerging-markets (accessed on 10 July 2020).
- Rebollo, A. La Experiencia Española en APPs: Hospitales, Infraestructura Social y Otros Equipamientos de uso Público y Municipal, PIAPPEM; Banco Interamericano de Desarrollo (BID): Washington, DC, USA, 2009; Available online: https://publications.iadb.org/publications/spanish/document/La-experiencia-española-en-concesiones-y-APPs-Hospitales-infraestructura-social-y-otros-equipamientos-de-uso-público-y-muncipal (accessed on 10 July 2020).
- Alonso, P.; Pinto, D.M.; Astorga, I.; Freddie, J. Menos Cuentos, Más Evidencia. Asociaciones Público-Privadas en el Sector de la Salud en América Latina. Nota Técnica n° IDB-TN-882; Banco Interamericano de Desarrollo: Washington, DC, USA, 2015; Available online: http://repositorio.minedu.gob.pe/bitstream/handle/123456789/4254/Menos%20cuentos%2c%20más%20evidencia.%20Asociaciones%20público-privadas%20en%20la%20literatura%20cientifica.pdf?sequence=1&isAllowed=y (accessed on 10 July 2020).
- Millan, G. Asociaciones Público-Privadas Para el Desarrollo de Infraestructura y la Provisión de Servicios Públicos. Experiencia del Reino Unido; Banco Interamericano de Desarrollo: Washington, DC, USA, 2009; Available online: https://publications.iadb.org/publications/spanish/document/Asociaciones-público---privadas-para-el-desarrollo-de-infraestructura-y-la-provisión-de-servicios-públicos-Experiencia-del-Reino-Unido (accessed on 10 July 2020).
- Quaid, R.M.; Scherrer, W. Public Private Partnership in the European Union: Experiences in the UK, Germany and Austria. Uprava, Letnik VI, 2008. Available online: https://www.napier.ac.uk/~/media/worktribe/output-234356/scherrer (accessed on 10 July 2020).
- Lee, D. HEALTHQUAL: A multi-item scale for assessing healthcare service quality. Serv. Bus. 2017, 11, 491–516. [Google Scholar] [CrossRef]
- Lam, S.K. SERVQUAL: A tool for measuring patient’s opinions of hospital service quality in Hong Kong. Total Qual. Manag. 2001, 8, 145–152. [Google Scholar] [CrossRef]
- Sofaer, S.; Firminger, K. Patient perceptions of the quality of health services. Annu. Rev. Public Health 2005, 26, 513–559. Available online: https://www.annualreviews.org/doi/pdf/10.1146/annurev.publhealth.25.050503.153958 (accessed on 10 July 2020). [CrossRef]
- Crow, R.; Gage, H.; Hampson, S.; Hart, J.; Kimber, A.; Storey, L. The measurement of satisfaction with healthcare: Implications for practice from a systematic review of the literature. Health Technol. Assess. 2002, 6, 1–244. [Google Scholar] [CrossRef]
- Myers, B. A Guide to Medical Care Administration: Concepts and Principles; American Public Health Association: Washington, DC, USA, 1969. [Google Scholar]
- Donabedian, A. The Definition of Quality and Approaches to Its Assessment; Health Administration Press: Chicago, IL, USA, 1980. [Google Scholar]
- Vuori, H. Quality Assurance of Health Services: Concepts and Methodology; Regional Office for Europe, World Health Organization: Copenhagen, Denmark, 1982. Available online: https://trove.nla.gov.au/version/26291550 (accessed on 10 July 2020).
- Bowers, M.; Swan, J.; Koehler, W. What attributes determine quality and satisfaction with healthcare delivery? Healthc. Manag. Rev. 1994, 19, 49–55. [Google Scholar] [CrossRef]
- Lee, D.; Kim, K.K. Assessing healthcare service quality: A comparative study of patient treatment types. Intern. J. Qual. Innovat. 2017, 3, 1–15. Available online: http://hdl.handle.net/10419/176484 (accessed on 10 July 2020). [CrossRef]
- Messarina, P. Calidad de atención del personal de salud y satisfacción del paciente en el servicio de resonancia magnética del Hospital de Alta Complejidad Trujillo. UCV Sci. 2016, 8, 119–123. Available online: http://revistas.ucv.edu.pe/index.php/UCV-SCIENTIA/article/view/1030/806 (accessed on 10 July 2020).
- Vega, E.N.M. La Gestión Administrativa y Calidad del Servicio en el Personal de la Comunidad Local de Administración de Salud (CLAS) Aguamiro—Yurimaguas—2017. Master’s Tesis, Universidad César Vallejo, Trujillo, Peru, 2017. Available online: http://repositorio.ucv.edu.pe/bitstream/handle/UCV/12765/montoya_ve.pdf?sequence=1&isAllowed=y (accessed on 10 July 2020).
- González, S.C. Manual de Mantenimiento de los Servicios de Salud: Instalaciones y Bienes de equipo; Serie HSP-UNI Manuales Operativos Paltex; Organización Mundial de la salud Organización Panamericana de la Salud: Washington, DC, USA, 1996; Volume II, Available online: https://apps.who.int/medicinedocs/documents/s17391es/s17391es (accessed on 10 July 2020).
- García-Cornejo, B. Análisis de eficiencia del sector hospitalario: Una revisión de métodos. Cuadernos de Estudios Empresariales 1997, 7, 151–176. Available online: https://www.researchgate.net/publication/27581587_Analisis_de_eficiencia_del_sector_hospitalario_una_revision_de_metodos (accessed on 10 July 2020).
- Puig-Junoy, J.; Dalmau, E. Qué Sabemos Acerca de la Eficiencia de las Organizaciones Sanitarias en España; Una revisión de la literatura económica; XX Jornadas de Economía de la Salud Asociación de Economía de la Salud (AES): Barcelona, Spain, 2000; Available online: https://jaumepuigjunoy.cat/wp-content/uploads/2017/11/AesXX (accessed on 10 July 2020).
- Mittal, V.; Kamakura, W.A. Satisfaction, repurchase intent, and repurchase behavior: Investigating the moderating effect of customer characteristics. J. Mark. Res. 2001, 38, 131–142. Available online: http://www.jstor.org/stable/1558577 (accessed on 10 July 2020). [CrossRef]
- Miranda, F.J.; Chamorro, A.; Murillo, L.R.; Vega, J. Assessing primary healthcare services quality in Spain: Managers vs. patients’ perceptions. Serv. Ind. J. 2010, 30, 2137–2149. [Google Scholar] [CrossRef]
- Chahal, H.; Kumari, N. Development of multidimensional scale for healthcare service quality (HCSQ) in Indian context. J. Indian Bus. Res. 2010, 2, 230–255. [Google Scholar] [CrossRef]
- Kondasani, R.K.R.; Panda, R.K. Customer perceived service quality, satisfaction and loyalty in Indian private healthcare. Int. J. Health Care Qual. Assur. 2005, 28, 452–467. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, D.; Kang, C.Y. The impact of high-performance work systems in the health-care industry: Employee reactions, service quality, customer satisfaction, and customer loyalty. Serv. Ind. J. 2012, 32, 17–36. [Google Scholar] [CrossRef]
- Salanova, M.; Agut, S.; Peiró, J.M. Linking organizational resources and work engagement to employee performance and customer loyalty: The mediation of service climate. J. Appl. Psychol. 2005, 90, 1217–1227. [Google Scholar] [CrossRef]
- Wold, H. Partial least squares. In Encyclopedia of Statistical Sciences; Kotz, S., Johnson, N.L., Eds.; Wiley: Hoboken, NJ, USA, 1985; Volume 6, pp. 581–591. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Fit indices in covariance structure modeling: Sensitivity to under parameterized model misspecification. Psychol. Methods 1998, 3, 424–453. [Google Scholar] [CrossRef]
- Carmines, E.G.; Zeller, R.A. Reliability and Validity Assessment. N. 07-017, Sage University Paper Series on Quantitative Applications in the Social Sciences; Sage: Beverly Hills, CA, USA, 1979; Available online: https://assets.thalia.media/doc/5d/fc/5dfc98a3-7c74-4fa7-a5b5-2133b883553a (accessed on 10 July 2020).
- Henseler, J.; Hubona, G.; Ray, P. Using PLS path modeling in new technology research: Updated guidelines. Ind. Manag. Data Syst. 2016, 116, 2–20. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in Variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Hair, F., Jr.; Sarstedt, M.; Hopkins, L.; Kuppelwieser, G.V. Partial least squares structural equation modeling (PLS-SEM): An emerging tool in business research. Eur. Bus. Rev. 2014, 26, 106–121. [Google Scholar] [CrossRef]
- Jiménez-Paneque, R.E. Indicadores de calidad y eficiencia de los servicios hospitalarios: Una mirada actual. Rev. Cuba. Salud Pública 2004, 30, 1. Available online: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-34662004000100004 (accessed on 10 July 2020).
- Alborta, G.; Stevenson, C.; Triana, S. Asociaciones Público-privadas Para la Prestación de Servicios. In Una Visión Hacia el Futuro. Documento de Discusión # IDB-DP-195; Banco Interamericano de Desarrollo: Washington, DC, USA, 2011; Available online: http://www.ampres.com.mx/assets/idbdp195-asociaciones-publico-privada-s-para-la-prestación-de-servicios (accessed on 10 July 2020).
- Bravo-Orellana, S. Asociaciones Público Privadas en el sector salud. Círculo Derecho Administrativo 2013, 13, 123–140. Available online: http://revistas.pucp.edu.pe/index.php/derechoadministrativo/article/view/13472/14099 (accessed on 10 July 2020).
- Redacción, G. IBT Health recibe la certificación de calidad ISO 9001-2015 en tres servicios. Diario Gestión, 7 August 2017. Available online: https://gestion.pe/economia/empresas/ibt-health-recibe-certificacion-calidad-iso-9001-2015-tres-servicios-141094-noticia/ (accessed on 10 July 2020).
- Rodríguez-Abad, J. Asociaciones público-privadas (APP): ¿Cómo pueden mejorar la calidad de los servicios de salud? Conexión ESAN, 2 November 2018. Available online: https://www.esan.edu.pe/conexion/actualidad/2018/11/02/asociaciones-publico-privadas-app-como-pueden-mejorar-la-calidad-de-los-servicios-de-salud/ (accessed on 10 July 2020).
- Seclén, J.; Darras, C. Satisfacción de los usuarios de los servicios de salud: Factores sociodemográficos y de accesibilidad asociados. Perú, 2000. Anales de la Facultad de Medicina 2005, 66, 127–141. Available online: https://pdfs.semanticscholar.org/4aad/5ce750343536c59ae9bf1a3fef119b89c286.pdf?_ga=2.72550355.150962373.1582721298-1919672084.1505835431 (accessed on 10 July 2020). [CrossRef]
- Sifuentes, A. Uso Exploratorio del SERVQUAL en la Evaluación de la Calidad del Servicio de Pediatría del Hospital Nacional Cayetano Heredia. Master’s Tesis, Universidad Peruana Cayetano Heredia, Lima, Perú, 2000. Available online: http://repositorio.upch.edu.pe/bitstream/handle/upch/7700/Calidad_QuirozOrtiz_Fabiola.pdf?sequence=1&isAllowed=y (accessed on 10 July 2020).
- Cabello, E.; Chirinos, J. Validación y aplicabilidad de encuestas SERVQUAL modificadas para medir la satisfacción de usuarios externos en servicios de salud. Rev. Med. Hered. 2012, 23, 88–95. Available online: http://www.scielo.org.pe/pdf/rmh/v23n2/v23n2ao2 (accessed on 10 July 2020). [CrossRef]
| Age | Hospital 1 1 | Hospital 2 2 | Total | ||
|---|---|---|---|---|---|
| Male | Female | Male | Female | ||
| 18–34 | 16 | 16 | 17 | 18 | 67 |
| 35–54 | 25 | 24 | 25 | 27 | 101 |
| 55–74 | 16 | 18 | 12 | 14 | 60 |
| +75 | 6 | 7 | 5 | 4 | 22 |
| Total | 128 | 122 | 250 | ||
| Indicator | |
|---|---|
| SRMR 1 | |
| Saturated Model | 0.0643 |
| Estimated Model | 0.0643 |
| Construct/Indicator | Factor Loadings | Composite Reliability | AVE 1 | ρA 2 | |
|---|---|---|---|---|---|
| Healthcare Personnel (HP) | 0.952 | 0.667 | 0.947 | ||
| HP1 | The professionalism of the healthcare personnel is very high | 0.7574 *** | |||
| HP2 | The kindness and courtesy of the healthcare personnel is very high | 0.7497 *** | |||
| HP3 | Confidence in the healthcare personnel is very high | 0.8000 *** | |||
| HP 4 | The healthcare personnel provide a highly personalized service | 0.7828 *** | |||
| HP5 | Communication with the healthcare personnel is very good | 0.8387 *** | |||
| HP6 | Individualized care of the healthcare personnel to the problems of the patient is very good | 0.8623 *** | |||
| HP7 | The interest of the healthcare personnel in attending to the patient’s problems is very high | 0.8733 *** | |||
| HP8 | The concern of the healthcare personnel to understand the problems of the patient is very high | 0.8514 *** | |||
| HP9 | The prestige of the medical staff is very good | 0.8554 *** | |||
| HP10 | Doctors explain in detail the diagnoses and treatment of a disease | 0.7858 *** | |||
| Nonhealthcare personnel (NHP) | 0.957 | 0.848 | 0.941 | ||
| NHP1 | The professionalism of the non-healthcare personnel is very high | 0.9034 *** | |||
| NHP2 | The kindness and courtesy of the nonhealthcare personnel is very good | 0.9250 *** | |||
| NHP3 | Individualized care of the nonhealthcare personnel to the problems of the patient is very good | 0.9335 *** | |||
| NHP4 | The interest of the nonhealthcare personnel in attending to the patient’s problems is very high | 0.9221 *** | |||
| Facilities, equipment, and tangibles (FET) | 0.894 | 0.585 | 0.865 | ||
| FET1 | The cleanliness of the facilities is very high | 0.6434 *** | |||
| FET2 | The equipment of the healthcare center is very good | 0.7434 *** | |||
| FET3 | The accessibility of the healthcare center is very good | 0.8034 *** | |||
| FET4 | The appearance and presence of the healthcare personnel is very good | 0.8435 *** | |||
| FET5 | The appearance and presence of the non-healthcare personnel is very good | 0.8051 *** | |||
| FET6 | There is clear signage for each department in the hospital | 0.7335 *** | |||
| Efficiency (EFI) | 0.919 | 0.507 | 0.906 | ||
| EFI1 | The hospital provides many facilities to arrange a medical appointment | 0.7402 *** | |||
| EFI2 | The level of bureaucracy is minimal (very low) | 0.7282 *** | |||
| EFI3 | The waiting time in the healthcare center before entering a medical consultation is adequate | 0.6685 *** | |||
| EFI4 | The hospital provides a very good computerized service | 0.6844 *** | |||
| EFI5 | The speed of ancillary testing is very high | 0.7036 *** | |||
| EFI6 | Complaint resolution is very fast and satisfactory | 0.7796 *** | |||
| EFI7 | The time spent focusing on the care of each patient is adequate | 0.7330 *** | |||
| EFI8 | The hours of the healthcare center are very wide and adequate | 0.6492 *** | |||
| EFI9 | Medical expenses are reasonable | 0.6465 *** | |||
| EFI10 | The existence of improvement in the medical condition as a result of the efforts and treatment by medical personnel is very high | 0.7512 *** | |||
| EFI11 | The occurrence of side effects when patients take their medicines is very low | 0.7382 *** | |||
| Loyalty (L) | 0.945 | 0.852 | 0.913 | ||
| L1 | The patient is treated again in this hospital | 0.9169 *** | |||
| L2 | The patient recommends this hospital to his friends and family | 0.9432 *** | |||
| L3 | Visiting the hospital again for its effectiveness in organization and service | 0.9081 *** | |||
| Heterotrait–Monotrait Ratio (HTMT) | |||||
|---|---|---|---|---|---|
| HP | NHP | FET | EFI | L | |
| HP | |||||
| NHP | 0.63 | ||||
| FET | 0.679 | 0.593 | |||
| EFI | 0.73 | 0.661 | 0.756 | ||
| L | 0.697 | 0.588 | 0.626 | 0.785 | |
| Fornell–Larcker Criterion | |||||
| HP | NHP | FET | EFI | L | |
| HP | 0.817 | ||||
| NHP | 0.613 | 0.921 | |||
| FET | 0.672 | 0.531 | 0.765 | ||
| EFI | 0.682 | 0.613 | 0.672 | 0.712 | |
| L | 0.65 | 0.546 | 0.566 | 0.72 | 0.923 |
| Construct | HP | NHP | FET | EFI | L |
|---|---|---|---|---|---|
| HP | 1.907 | 2.184 | |||
| NHP | 1.655 | 1.792 | |||
| FET | 1.726 | 2.02 | |||
| EFI | 2.504 | ||||
| L |
| Hypothesis | Suggested Effect | Path Coefficient | Confidence Interval 99% | Student’s t | p-Value |
|---|---|---|---|---|---|
| H1: HP -> EFI | + | 0.3331 *** | [0.2410; 0.4223] | 6.0374 | 0.0000 |
| H2: HP -> L | + | 0.2525 *** | [0.1039; 0.4118] | 2.7147 | 0.0033 |
| H3: NHP -> EFI | + | 0.2338 *** | [0.1547; 0.3252] | 4.4977 | 0.0000 |
| H4: NHP -> L | + | 0.0856 | [−0.0566; 0.2069] | 1.0763 | 0.1409 |
| H5: FET -> EFI | + | 0.3428 *** | [0.2545; 0.4314] | 6.3340 | 0.0000 |
| H6: FET -> L | + | 0.0595 | [−0.0555; 0.1763] | 0.8476 | 0.1983 |
| H7: EFI -> L | + | 0.4550 *** | [0.3345; 0.5904] | 5.9320 | 0.0000 |
| Construct | R2 | Q2 | f2 | Direct Effect | Correlation | Variance Explained |
|---|---|---|---|---|---|---|
| EFI | 0.6007 | 0.2792 | ||||
| H1: HP | 0.1457 | 0.3331 | 0.682 | 22.70% | ||
| H3: NHP | 0.0827 | 0.2338 | 0.6131 | 14.30% | ||
| H5: FET | 0.1705 | 0.3428 | 0.6715 | 23.00% | ||
| L | 0.572 | 0.4529 | ||||
| H2: HP | 0.0682 | 0.2525 | 0.6501 | 16.40% | ||
| H4: NHP | 0.0096 | 0.0856 | 0.5457 | 4.70% | ||
| H6: FET | 0.0041 | 0.0595 | 0.5656 | 3.40% | ||
| H7: EFI | 0.1932 | 0.455 | 0.7197 | 32.70% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barrios-Ipenza, F.; Calvo-Mora, A.; Velicia-Martín, F.; Criado-García, F.; Leal-Millán, A. Patient Satisfaction in the Peruvian Health Services: Validation and Application of the HEALTHQUAL Scale. Int. J. Environ. Res. Public Health 2020, 17, 5111. https://doi.org/10.3390/ijerph17145111
Barrios-Ipenza F, Calvo-Mora A, Velicia-Martín F, Criado-García F, Leal-Millán A. Patient Satisfaction in the Peruvian Health Services: Validation and Application of the HEALTHQUAL Scale. International Journal of Environmental Research and Public Health. 2020; 17(14):5111. https://doi.org/10.3390/ijerph17145111
Chicago/Turabian StyleBarrios-Ipenza, Fernando, Arturo Calvo-Mora, Félix Velicia-Martín, Fernando Criado-García, and Antonio Leal-Millán. 2020. "Patient Satisfaction in the Peruvian Health Services: Validation and Application of the HEALTHQUAL Scale" International Journal of Environmental Research and Public Health 17, no. 14: 5111. https://doi.org/10.3390/ijerph17145111
APA StyleBarrios-Ipenza, F., Calvo-Mora, A., Velicia-Martín, F., Criado-García, F., & Leal-Millán, A. (2020). Patient Satisfaction in the Peruvian Health Services: Validation and Application of the HEALTHQUAL Scale. International Journal of Environmental Research and Public Health, 17(14), 5111. https://doi.org/10.3390/ijerph17145111






