Development and Validation of a Questionnaire Evaluating the Impact of Prosthetic Dental Treatments on Patients’ Oral Health Quality of Life: A Prospective Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Novel Questionnaire Development
Literature Review and Meta-Synthesis
2.2. PICO Defined for the Current Study
2.2.1. The Study Population
- Over 18 years of age and under 75 years.
- Patients at the School of Dentistry at Tel Aviv University.
- Good general health, no medical risks, including past or present chemotherapy or radiation.
- Ability to understand, respond, and complete the questionnaire.
- At least one tooth in need of prosthetic treatment: fixed partial denture (FPD), implant-supported, full or partial removable restorations, full or partial removable restorations supported by implants.
- Systemic illnesses that will prevent research participation.
- Oral disease that directly or indirectly affects rehabilitation.
- Oral disease that directly or indirectly affects OHRQoL.
- Failure to complete prosthetic treatments.
2.2.2. Intervention
2.2.3. Outcome
Documentation and information collection
Statistical analysis
3. Results
3.1. Questionnaire Reliability
3.2. Type of Rehabilitation
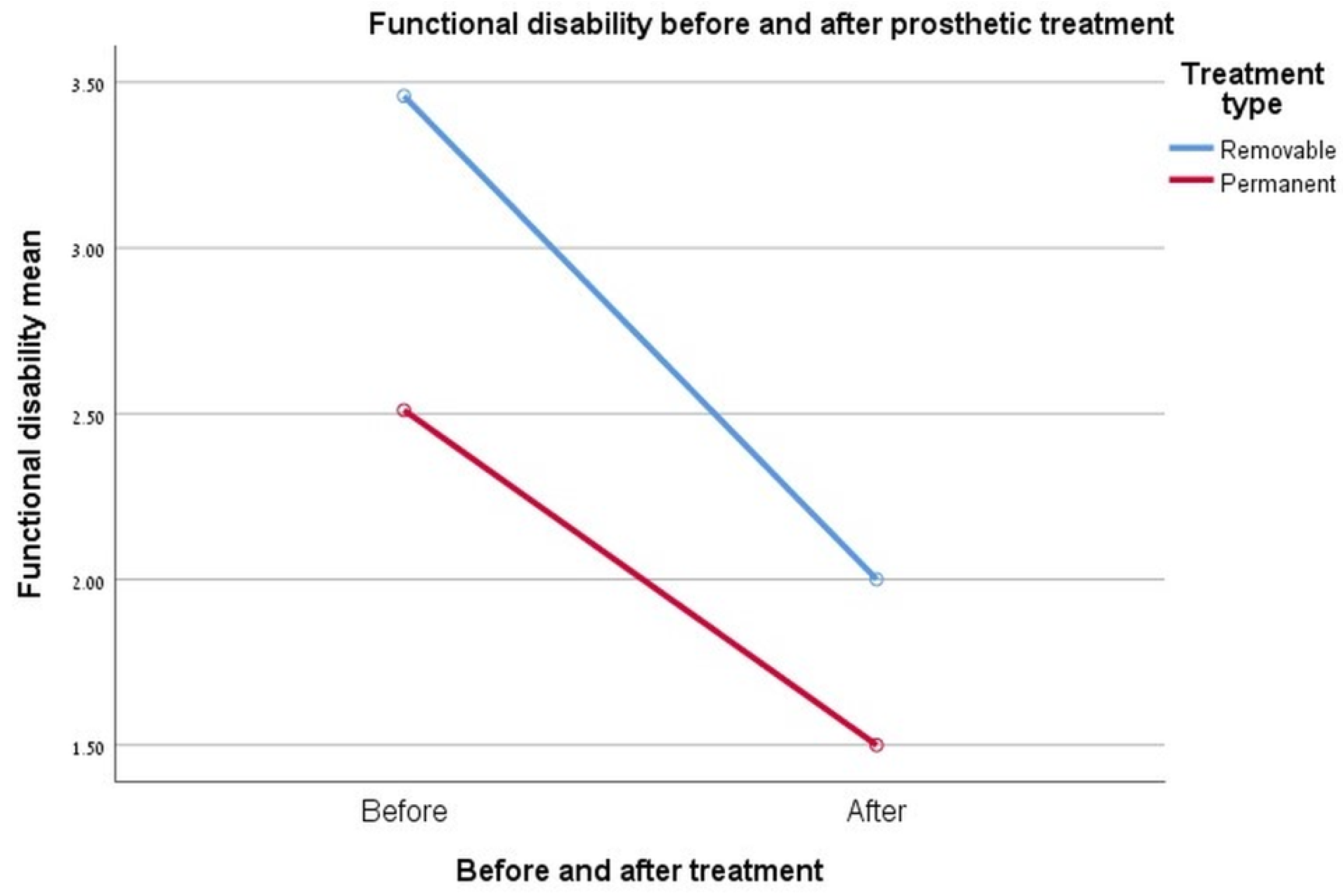
3.3. Functional Disability
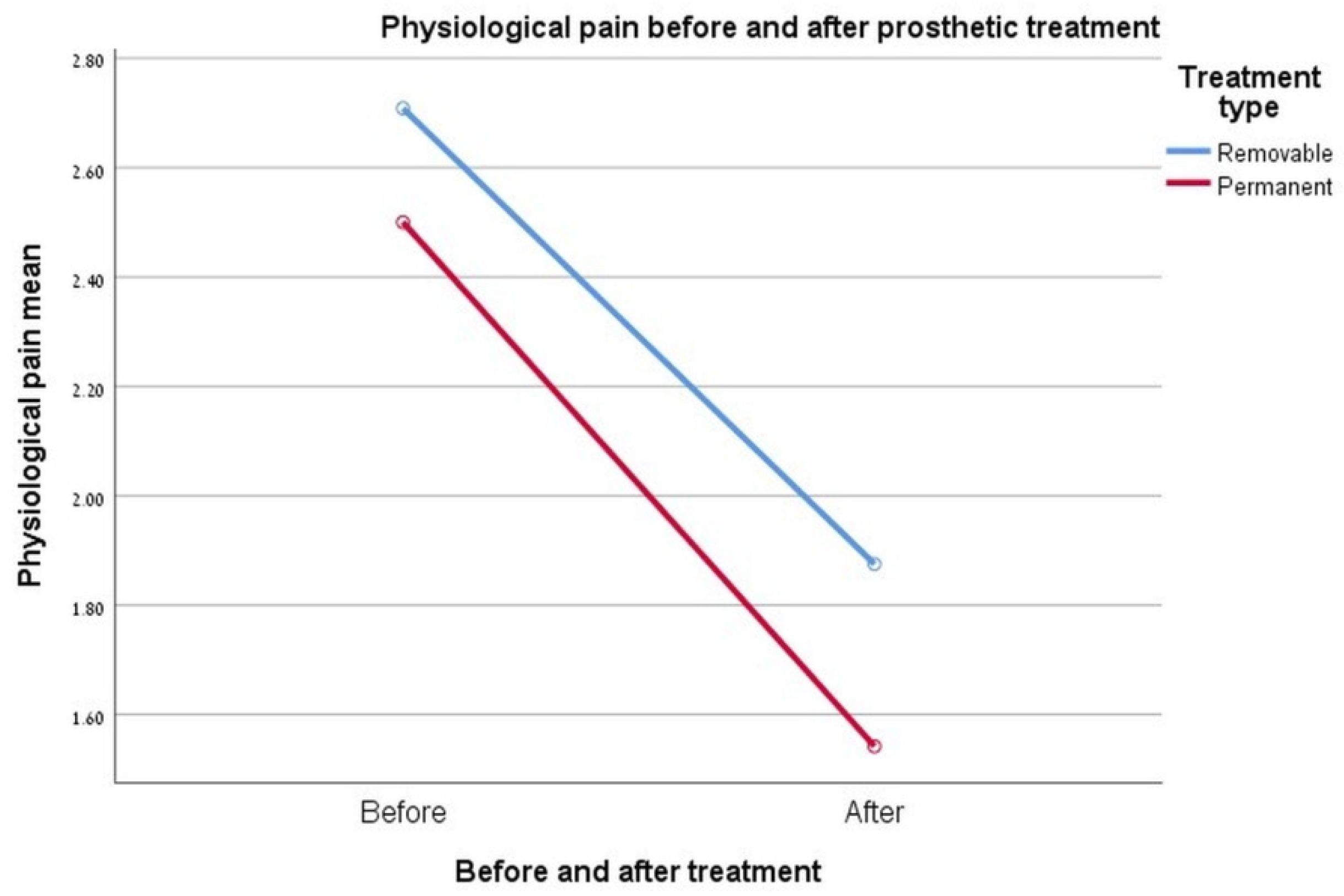
3.4. Physiological Pain
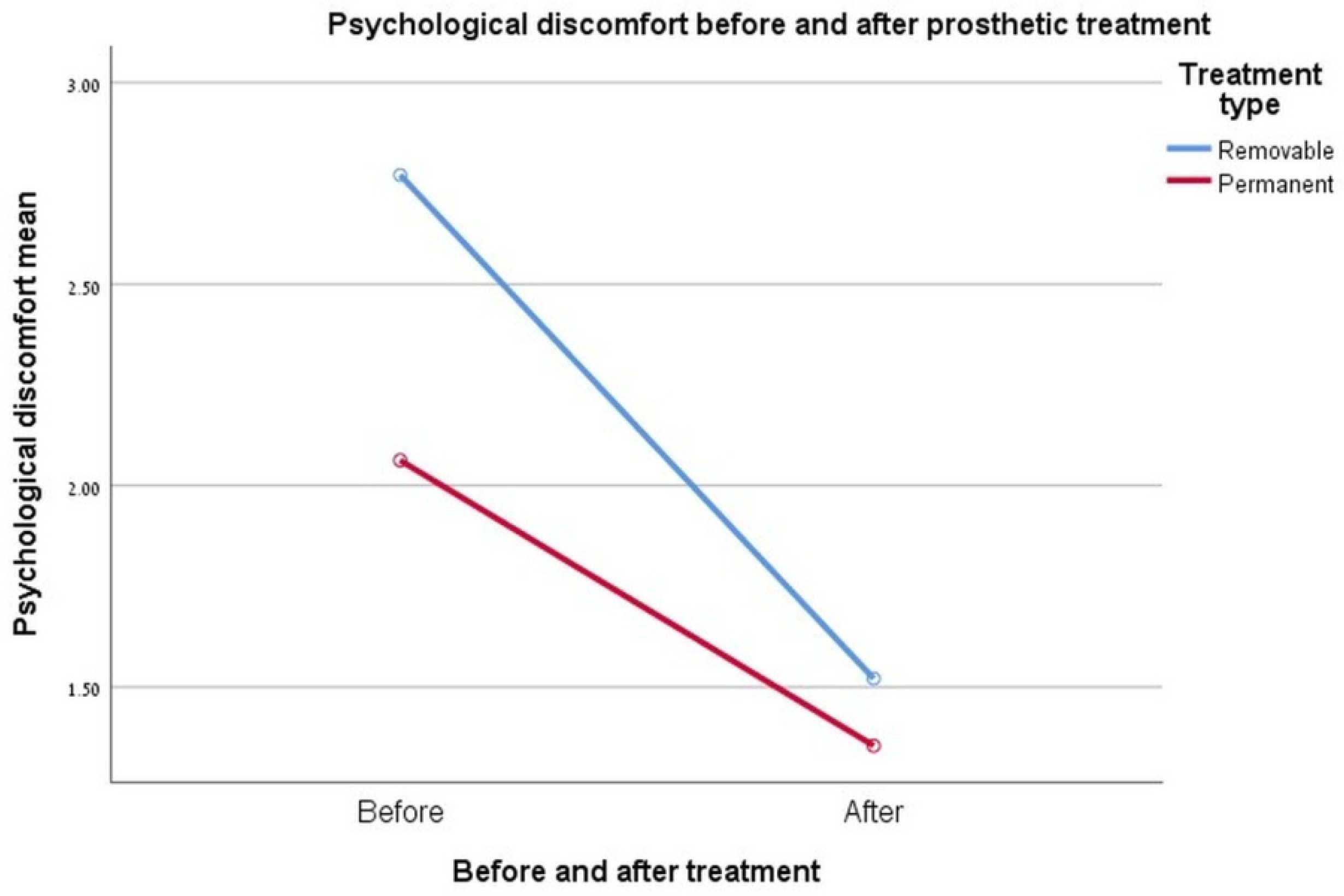
3.5. Psychological Discomfort
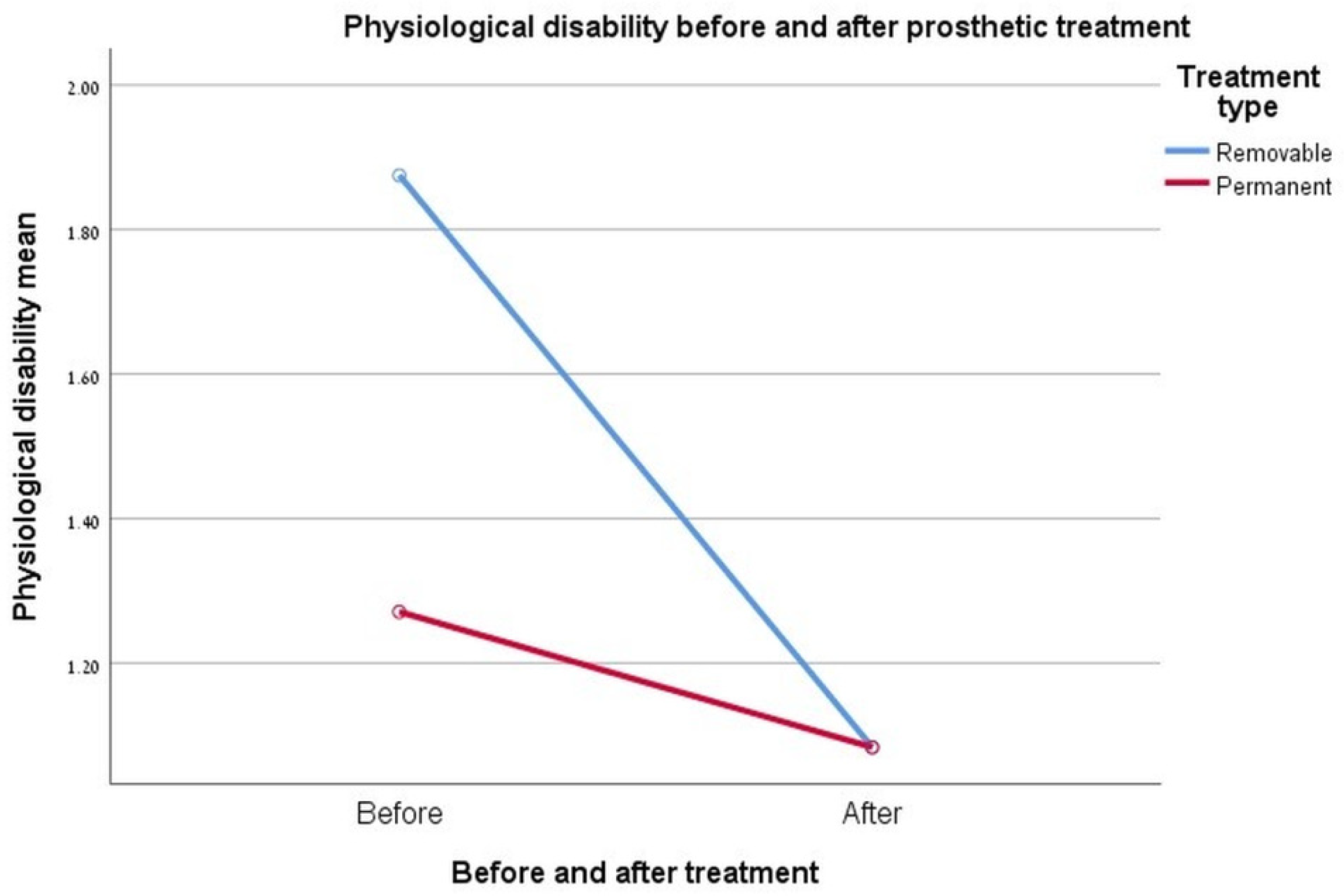
3.6. Physiological Disability
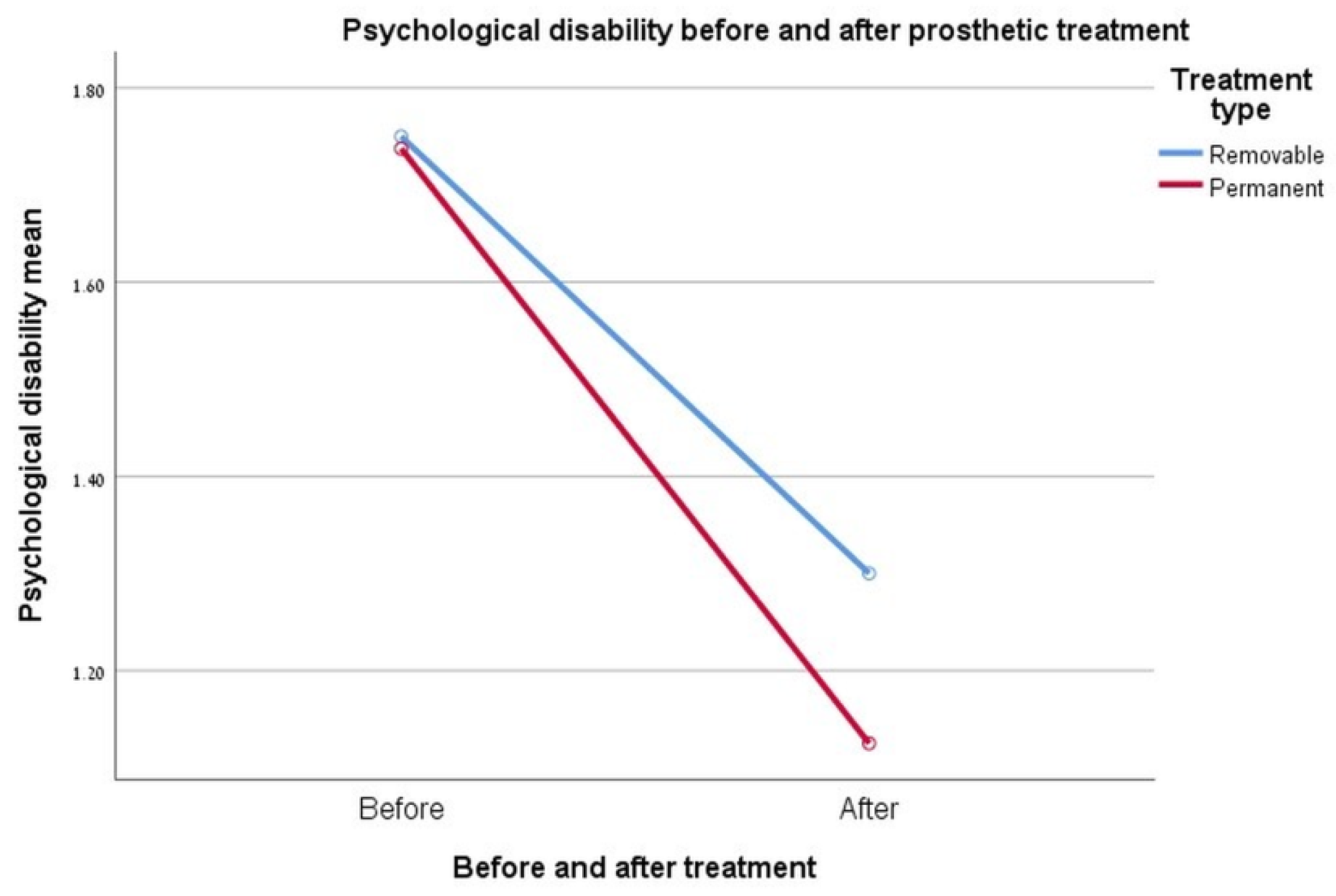
3.7. Psychological Disability
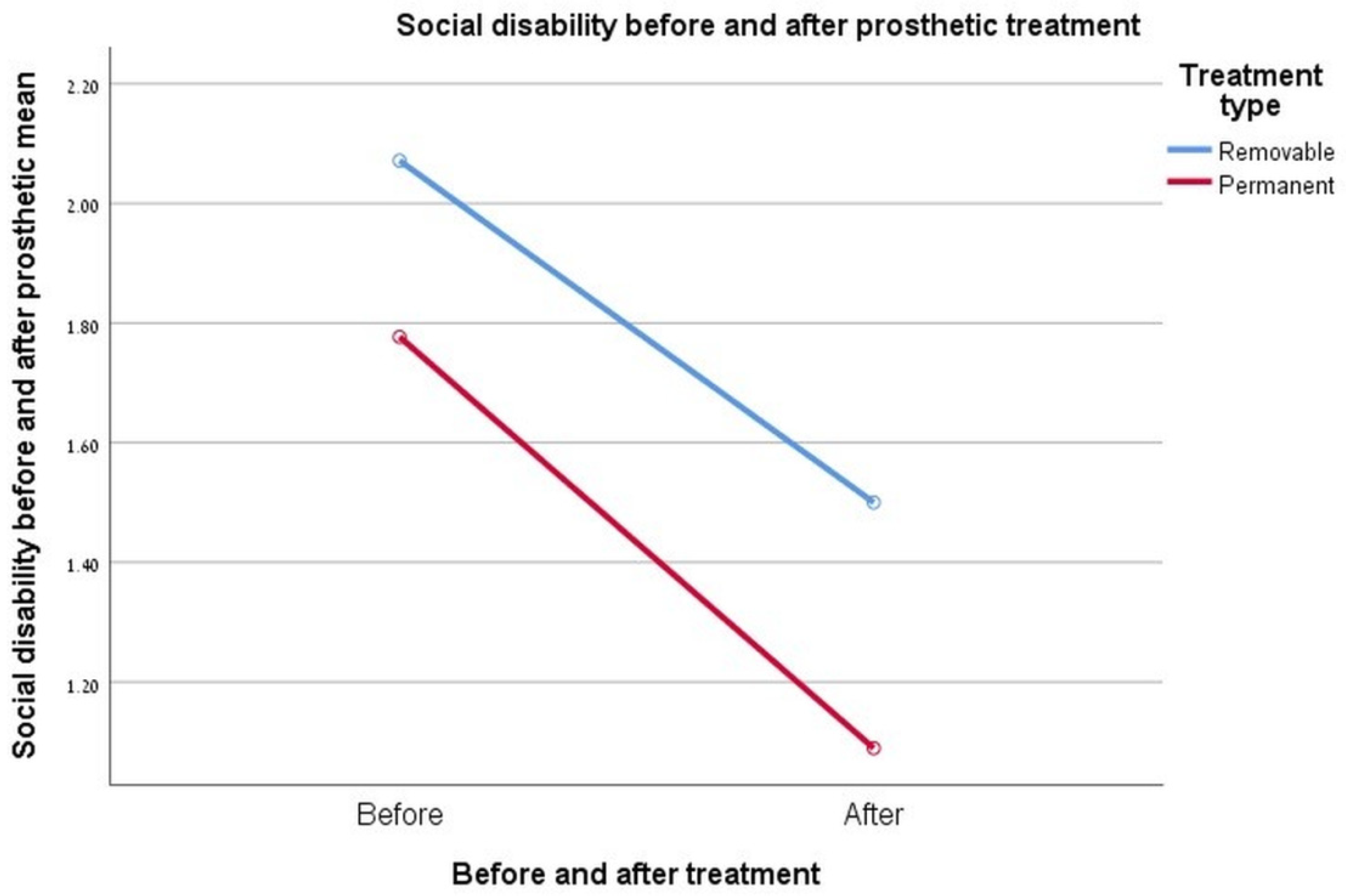
3.8. Social Disability
3.9. The Physician
3.10. Gender
3.11. Rehabilitation Times
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
- One tooth missing
- I am missing a few teeth
- I am missing missing all teeth
- Replacement of defective permanent restoration
- Repairing a tooth’s aesthetic defect.
- Crown
- Front plating
- Bridge
- Crown supported implant
- Bridge supported implant
- Whole denture supported by implants
- Removable whole denture
- Removable partial denture
- Implant supported partial dentures/unknown.
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
- Never/rarely/sometimes/often/almost always
- Unknown/irrelevant
Appendix B
- I am proud of my teeth.
- I like to show my teeth when I smile.
- I am pleased when I see my teeth in the mirror.
- My teeth are attractive to others.
- I am satisfied with the appearance of my teeth.
- I find my tooth position to be very nice.
- I hold myself back when I smile so my teeth don’t show so much.
- If I don’t know people well I am sometimes concerned what they might think about my teeth.
- I’m afraid other people could make offensive remarks about my teeth.
- I am somewhat inhibited in social contacts because of my teeth.
- I sometimes catch myself holding my hand in front of my mouth to hide my teeth.
- Sometimes I think people are staring at my teeth.
- Remarks about my teeth irritate me even when they are meant jokingly.
- I sometimes worry about what members of the opposite sex think about my teeth.
- I envy the nice teeth of other people.
- I am somewhat distressed when I see other people’s teeth.
- Sometimes I am somewhat unhappy about the appearance of my teeth.
- I think most people I know have nicer teeth than I do.
- I feel bad when I think about what my teeth look like.
- I wish my teeth looked better.
- I don’t like to see my teeth in the mirror.
- I don’t like to see my teeth in photographs.
- I don’t like to see my teeth when I look at a video of myself.
Appendix C
| OHIP-14 | |||||
|---|---|---|---|---|---|
| In the Last Six Months | Never | Hardly ever | Occasionally | Fairly Often | Very Often |
| (1) Have you had trouble pronouncing any words because of problem with your teeth, mouth or dentures? | |||||
| (2) Have you felt that your sense of taste has worsened because of problems with your teeth, mouth or dentures? | |||||
| (3) Have you had painful aching in your mouth? | |||||
| (4) Have you found it uncomfortable to eat any foods because of problems with your teeth, mouth or dentures? | |||||
| (5) Have you been worried by dental problems? | |||||
| (6) Have you felt tense because of problems with teeth, mouth or dentures? | |||||
| (7) Has your diet been unsatisfactory because of problems with teeth, mouth or dentures? | |||||
| (8) Have you had to interrupt meals because of problems with teeth, mouth or dentures? | |||||
| (9) Have you found it difficult to relax because of problems with teeth, mouth or dentures? | |||||
| (10) Have you been a bit embarrassed because of problems with teeth, mouth or dentures? | |||||
| (11) Have you been a bit irritable with other people because of problems with teeth, mouth or dentures? | |||||
| (12) Have you had difficulty doing you usual jobs because of problems with teeth, mouth or dentures? | |||||
| (13) Have you felt that life in general was less satisfying because of problems with teeth, mouth or dentures? | |||||
| (14) Have you been totally unable to function because of problems with teeth, mouth or dentures? | |||||
References
- Nordenram, G.; Davidson, T.; Gynther, G.; Helgesson, G.; Hultin, M.; Jemt, T.; Lekholm, U.; Nilner, K.; Norlund, A.; Rohlin, M.; et al. Qualitative studies of patients’ perceptions of loss of teeth, the edentulous state and prosthetic rehabilitation: A systematic review with meta-synthesis. Acta Odontol. Scand. 2013, 71, 937–951. [Google Scholar] [CrossRef]
- Klages, U.; Claus, N.; Wehrbein, H.; Zentner, A. Development of a questionnaire for assessment of the psychosocial impact of dental aesthetics in young adults. Eur. J. Orthod. 2006, 28, 103–111. [Google Scholar] [CrossRef]
- Thomason, J.M.; Heydecke, G.; Feine, J.S.; Ellis, J.S. How do patients perceive the benefit of reconstructive dentistry with regard to oral health-related quality of life and patient satisfaction? A systematic review. Clin. Oral Implant. Res. 2008, 19, 326–328. [Google Scholar] [CrossRef] [PubMed]
- Bassi, F.; Carr, A.; Chang, T.-L.; Estafanous, E.; Garrett, N.; Happonen, R.-P.; Koka, S.; Laine, J.; Osswald, M.; Reintsema, H.; et al. Psychologic Outcomes in Implant Prosthodontics. Int. J. Prosthodont. 2013, 26, 429–4345. [Google Scholar] [CrossRef][Green Version]
- Slade, G.D. The oral health impact profile. In Measuring Oral Health and Quality of Life, 1st ed.; Slade, G.D., Ed.; University of North Carolina: Chapell Hill, NC, USA, 1997; pp. 57–64. [Google Scholar]
- Van Der Geld, P.; Oosterveld, P.; Van Heck, G.; Kuijpers-Jagtman, A.M. Smile attractiveness: Self-perception and influence on personality. Angle Orthod. 2007, 77, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Gates, W.D.; Cooper, L.F.; Sanders, A.E.; Reside, G.J.; De Kok, I.J. The effect of implant-supported removable partial dentures on oral health quality of life. Clin. Oral Implant. Res. 2014, 25, 207–213. [Google Scholar] [CrossRef]
- Trulsson, U.; Engstrand, P.; Berggren, U.; Nannmark, U.; Brånemark, P.I. Edentulousness and oral rehabilitation: Experiences from the patients’ perspective. Eur. J. Oral Sci. 2002, 110, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef]
- Locker, D. Measuring oral health: A conceptual framework. Community Dent. Health 1988, 5, 3–18. [Google Scholar] [PubMed]
- Klages, U.; Bruckner, A.; Zentner, A. Dental aesthetics, self-awareness, and oral health-related quality of life in young adults. Eur. J. Orthod. 2004, 26, 507–514. [Google Scholar] [CrossRef]
- Patrick, D.L.; Bergner, M. Measurement of health status in the 1990s. Annu. Rev. Public Health 1990, 11, 165–183. [Google Scholar] [CrossRef] [PubMed]
- Locker, D.; Allen, F. What do measures of “oral health-related quality of life” measure? Community Dent. Oral Epidemiol. 2007, 35, 401–411. [Google Scholar] [CrossRef]
- Bramanti, E.; Matacena, G.; Cecchetti, F.; Arcuri, C.; Cicciù, M. Oral health-related quality of life in partially edentulous patients before and after implant therapy: A 2-year longitudinal study. Oral Implant. 2013, 6, 37–42. [Google Scholar] [CrossRef]
- Kuoppala, R.; Näpänkangas, R.; Raustia, A. Quality of Life of Patients Treated With Implant-Supported Mandibular Overdentures Evaluated With the Oral Health Impact Profile (OHIP-14): A Survey of 58 Patients. J. Oral Maxillofac. Res. 2013, 4, e4. [Google Scholar] [CrossRef]
- Sun, X.; Zhai, J.J.; Liao, J.; Teng, M.H.; Tian, A.; Liang, X. Masticatory efficiency and oral health-related quality of life with implant-retained mandibular overdentures. Saudi Med. J. 2014, 35, 1195–1202. [Google Scholar]
- Özhayat, E.B.; Gotfredsen, K. Effect of treatment with fixed and removable dental prostheses. An oral health-related quality of life study. J. Oral Rehabilit. 2012, 39, 28–36. [Google Scholar]
- Brennan, M.; Houston, F.; O’Sullivan, M.O.B. Patient satisfaction and oral health-related quality of life outcomes of implant overdentures and fixed complete dentures. Int. J. Oral Maxillofac. Implant. 2010, 25, 791–800. [Google Scholar]
- Swelem, A.A.; Gurevich, K.F.K. Oral health-related quality of life in partially edentulous patients treated with removable, fixed, fixed-removable, and implant-supported prostheses. Int. J. Prosthodont. 2014, 24, 338–347. [Google Scholar]
- Smith, P.A.; Entwistle, V.A.; Nuttall, N. Patients’ experiences with partial dentures: A qualitative study. Gerodontology 2005, 22, 187–192. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Allen, P.F. Assessment of oral health related quality of life. Health Qual. Life Outcomes 2003, 1, 40. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the Oral Health Impact Profile. Community Dent. Health 1994, 11, 3–11. [Google Scholar] [PubMed]
- Zembic, A.; Wismeijer, D. Patient-reported outcomes of maxillary implant-supported overdentures compared with conventional dentures. Clin. Oral Implant. Res. 2014, 25, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Preciado, A.; Del Río, J.; Suárez-García, M.J.; Montero, J.; Lynch, C.D.; Castillo-Oyagüe, R. Differences in impact of patient and prosthetic characteristics on oral health-related quality of life among implant-retained overdenture wearers. J. Dent. 2012, 40, 857–865. [Google Scholar] [CrossRef] [PubMed]
- Wickert, M.; John, M.T.; Schierz, O.; Hirsch, C.; Aarabi, G.; Reissmann, D.R. Sensitivity to change of oral and general health-related quality of life during prosthodontic treatment. Eur. J. Oral Sci. 2014, 122, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Peršić, S.; Čelebić, A. Influence of different prosthodontic rehabilitation options on oral health-related quality of life, orofacial esthetics and chewing function based on patient-reported outcomes. Qual. Life Res. 2015, 24, 919–926. [Google Scholar] [CrossRef]

| Domain | Functional Disability | Physiological Pain | Psychological Discomfort | Physiological Disability | Psychological Disability | Social Disability |
|---|---|---|---|---|---|---|
| Items number | Items #1–6 | Items #7–10 | Items #11–16 | Items #17–19 | Items #20–24 | Items #25–31 |
| Domain | Functional Disability | Physiological Pain | Psychological Discomfort | Physiological Disability | Psychological Disability | Social Disability |
|---|---|---|---|---|---|---|
| Cronbach’s alpha | α = 0.67 | α = 0.77 | α = 0.76 | α = 0.7 | α = 0.7 | α = 0.868 |
| ICC (95% confidence interval; p) | 0.56 (0.31–0.76; <0.001) | 0.71 (0.5–0.85; <0.001) | 0.69 (0.49–0.84; <0.001) | 0.67 (0.42–0.83; <0.001) | 0.67 (0.45–0.83; <0.001) | 0.84 (0.73–0.92; <0.001) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mijiritsky, E.; Lerman, Y.; Mijiritsky, O.; Shely, A.; Meyerson, J.; Shacham, M. Development and Validation of a Questionnaire Evaluating the Impact of Prosthetic Dental Treatments on Patients’ Oral Health Quality of Life: A Prospective Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 5037. https://doi.org/10.3390/ijerph17145037
Mijiritsky E, Lerman Y, Mijiritsky O, Shely A, Meyerson J, Shacham M. Development and Validation of a Questionnaire Evaluating the Impact of Prosthetic Dental Treatments on Patients’ Oral Health Quality of Life: A Prospective Pilot Study. International Journal of Environmental Research and Public Health. 2020; 17(14):5037. https://doi.org/10.3390/ijerph17145037
Chicago/Turabian StyleMijiritsky, Eitan, Yael Lerman, Ori Mijiritsky, Asaf Shely, Joseph Meyerson, and Maayan Shacham. 2020. "Development and Validation of a Questionnaire Evaluating the Impact of Prosthetic Dental Treatments on Patients’ Oral Health Quality of Life: A Prospective Pilot Study" International Journal of Environmental Research and Public Health 17, no. 14: 5037. https://doi.org/10.3390/ijerph17145037
APA StyleMijiritsky, E., Lerman, Y., Mijiritsky, O., Shely, A., Meyerson, J., & Shacham, M. (2020). Development and Validation of a Questionnaire Evaluating the Impact of Prosthetic Dental Treatments on Patients’ Oral Health Quality of Life: A Prospective Pilot Study. International Journal of Environmental Research and Public Health, 17(14), 5037. https://doi.org/10.3390/ijerph17145037






