“We Don’t Assume That Everyone Has the Same Idea About Health, Do We?” Explorative Study of Citizens’ Perceptions of Health and Participation to Improve Their Health in a Low Socioeconomic City District
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Study Design
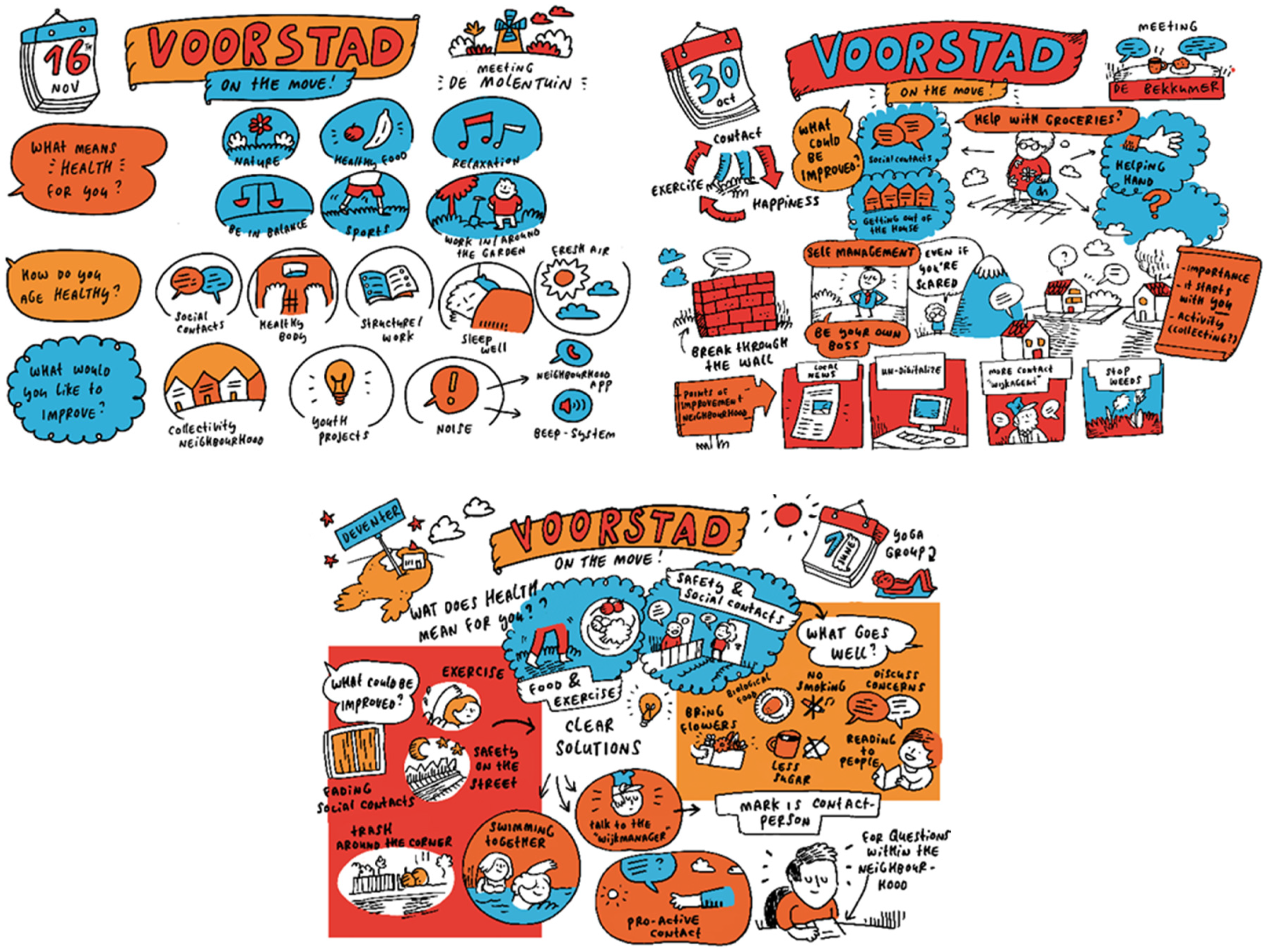
2.3. Participants: Recruitment and Response
2.4. Ethical Approval
2.5. Procedure: Concept Mapping
2.6. Overall Data Analysis
3. Results
3.1. Perceptions of Health
3.2. Needs and Barriers to Improving Health
3.3. Actions to Improve Health
- The language group and the yoga group participants went swimming;
- Two people got a biking buddy;
- Some language group participants took guitar lessons;
- The resident group participants made appointments to meet more regularly;
- One group organized a high tea to meet (new) neighbors.
4. Discussion
4.1. Health is a Multidimensional Concept
4.2. Perceptions on Health and the Social and Natural Environment as Important Assets
4.3. Citizens and Professionals Working Together to Build a Health Promotion Programme
4.4. Methodological Considerations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- de Jong, M.A.J.G.; Wagemakers, A.; Koelen, M.A. Study protocol: Evaluation of a community health promotion program in a socioeconomically deprived city district in the Netherlands using mixed methods and guided by action research. BMC Public Heal. 2019, 19, 72. [Google Scholar] [CrossRef] [PubMed]
- VTV 2018. A healthy Prospective. Available online: https://www.vtv2018.nl/2018 (accessed on 23 September 2018).
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.; Taylor, S. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- MacKenbach, J.P. Persistence of social inequalities in modern welfare states: Explanation of a paradox. Scand. J. Public Heal. 2016, 45, 113–120. [Google Scholar] [CrossRef] [PubMed]
- MacKenbach, J.P. Can we reduce health inequalities? An analysis of the English strategy (1997–2010). J. Epidemiol. Community Heal. 2011, 65, 568–575. [Google Scholar] [CrossRef]
- Borrell, C.; Artazcoz, L.; Pasarin, M.I.; Pasarín, M.I.; Diez, E. Social inequalities in health and closing the gap in a generation. J. Public Heal. Policy 2009, 30, 189–194. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. Ecological models of human development. In The International Encyclopedia of Education, 2nd ed.; Elsevier: Oxford, UK, 1994; Volume 3, pp. 1643–1647. [Google Scholar]
- Sallis, J.F.; Owen, N.; Fotheringham, M.J. Behavioral epidemiology: A systematic framework to classify phases of research on health promotion and disease prevention. Ann. Behav. Med. 2000, 22, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Stokols, D. Translating Social Ecological Theory into Guidelines for Community Health Promotion. Am. J. Heal. Promot. 1996, 10, 282–298. [Google Scholar] [CrossRef]
- Kandt, J. Social practice, plural lifestyles, and health inequalities in the United Kingdom. Sociol. Heal. Illn. 2018, 40, 1294–1311. [Google Scholar] [CrossRef]
- Stephens, C. Participation in Different Fields of Practice: Using Social Theory to Understand Participation in Community Health Promotion. J. Heal. Psychol. 2007, 12, 949–960. [Google Scholar] [CrossRef]
- Baum, F.; Fisher, M. Why Behavioural Health Promotion Endures Despite Its Failure to Reduce Health Inequities. In From Health Behaviours to Health Practices; John Wiley & Sons, Ltd.: Oxford, UK, 2014; pp. 57–68. [Google Scholar] [CrossRef]
- Veenstra, G.; Burnett, P.J. A Relational Approach to Health Practices: Towards Transcending the Agency-Structure Divide. In From Health Behaviours to Health Practices; Wiley: Hoboken, NJ, USA, 2014; pp. 31–42. [Google Scholar]
- Broeders, D.; Das, D.; Jennissen, R.; Tiemeijer, W.; de Visser, M. From Diffence to Potential; A Realistic Perspective on Socio-Economic Health Differences; WRR: The Hague, The Netherlands, 2018; p. 46. [Google Scholar]
- Herens, M.; Wagemakers, A.; Vaandrager, L.; van Ophem, J.; Koelen, M.; Baranowski, T.; Booth, A. Evaluation Design for Community-Based Physical Activity Programs for Socially Disadvantaged Groups: Communities on the Move. JMIR Res. Protoc. 2013, 2, e20. [Google Scholar] [CrossRef]
- Storm, I.; van Koperen, M.; van der Lucht, F.; van Oers, H.; Schuit, J. Monitoren en evalueren van integraal gezondheidsbeleid. Beleidsonderzoek Online 2014. [Google Scholar] [CrossRef]
- Stronks, K.; Arah, O.A.; Plochg, T. Learning from Policy Failure and Failing to Learn from Policy. Eur. J. Public Heal. 2006, 16, 343–344. [Google Scholar] [CrossRef] [PubMed]
- MacKenbach, J.P. Has the English strategy to reduce health inequalities failed? Soc. Sci. Med. 2010, 71, 1249–1253. [Google Scholar] [CrossRef] [PubMed]
- Naaldenberg, J.; Vaandrager, L.; Koelen, M.A.; Leeuwis, C. Aging Population’s Everyday Life Perspectives on Healthy Aging. J. Appl. Gerontol. 2011, 31, 711–733. [Google Scholar] [CrossRef]
- Koelen, M.A.; Ban, A.W.V.D. Health Education, and Health Promotion; Wageningen Academic Publishers: Wageningen, The Netherlands, 2004. [Google Scholar]
- Wagemakers, A.; Vaandrager, L.; Koelen, M.A.; Saan, H.; Leeuwis, C. Community health promotion: A framework to facilitate and evaluate supportive social environments for health. Eval. Program Plan. 2010, 33, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Laverack, G. Using a ‘domains’ approach to build community empowerment. Community Dev. J. 2005, 41, 4–12. [Google Scholar] [CrossRef]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef]
- Peerson, A.; Saunders, M. Health literacy revisited: What do we mean and why does it matter? Heal. Promot. Int. 2009, 24, 285–296. [Google Scholar] [CrossRef]
- Frohlich, K.L.; Potvin, L. Transcending the Known in Public Health Practice. Am. J. Public Heal. 2008, 98, 216–221. [Google Scholar] [CrossRef]
- Cyril, S.; Smith, B.J.; Possamai-Inesedy, A.; Renzaho, A.M. Exploring the role of community engagement in improving the health of disadvantaged populations: A systematic review. Glob. Heal. Action 2015, 8, 29842. [Google Scholar] [CrossRef]
- Morgan, A.; Ziglio, E. Revitalising the evidence base for public health: An assets model. Promot. Educ. 2007, 14, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Stronks, K.; Hoeymans, N.; Haverkamp, B.; Hertog, F.R.J.D.; van Bon-Martens, M.J.H.; Galenkamp, H.; Verweij, M.; van Oers, H. Do conceptualisations of health differ across social strata? A concept mapping study among lay people. BMJ Open 2018, 8, e020210. [Google Scholar] [CrossRef] [PubMed]
- Haverkamp, B.; Verweij, M.; Stronks, K. ‘Gezondheid’: Voor iedere context een passend begrip? TSG 2017, 95, 258–263. [Google Scholar] [CrossRef]
- Bukman, A.J.; Teuscher, D.; Feskens, E.; van Baak, M.; Meershoek, A.; Renes, R.J. Perceptions on healthy eating, physical activity, and lifestyle advice: Opportunities for adapting lifestyle interventions to individuals with low socioeconomic status. BMC Public Heal. 2014, 14, 1036. [Google Scholar] [CrossRef] [PubMed]
- Coveney, J. A qualitative study exploring socio-economic differences in parental lay knowledge of food and health: Implications for public health nutrition. Public Heal. Nutr. 2005, 8, 290–297. [Google Scholar] [CrossRef]
- Ballering, C.; Schreurs, H.; Renders, C.; Kooiker, S.; van Ameijden, E. A glimpse in stories about lifestyle habits. Tijdschr Gezondheidswetenschappen 2013, 5, 263–269. [Google Scholar] [CrossRef]
- Haverkamp, B.; Bovenkerk, B.; Verweij, M.F. A Practice-Oriented Review of Health Concepts. J. Med. Philos. 2018, 43, 381–401. [Google Scholar] [CrossRef]
- Bukman, A.J.; Teuscher, D.; Ben Meftah, J.; Groenenberg, I.; Crone, M.; van Dijk, S.; Bos, M.B.; Feskens, E. Exploring strategies to reach individuals of Turkish and Moroccan origin for health checks and lifestyle advice: A mixed-methods study. BMC Fam. Pr. 2016, 17, 85. [Google Scholar] [CrossRef]
- Bonevski, B.; Randell, M.; Paul, C.; Chapman, K.; Twyman, L.; Bryant, J.; Brozek, I.; Hughes, C. Reaching the hard-to-reach: A systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res. Methodol. 2014, 14, 42. [Google Scholar] [CrossRef]
- Broeder, L.D.; Devilee, J.; van Oers, H.; Schuit, J.; Wagemakers, A. Citizen Science for public health. Heal. Promot. Int. 2018, 33, 505–514. [Google Scholar] [CrossRef]
- Bisogni, C.A.; Jastran, M.; Seligson, M.; Thompson, A. How People Interpret Healthy Eating: Contributions of Qualitative Research. J. Nutr. Educ. Behav. 2012, 44, 282–301. [Google Scholar] [CrossRef] [PubMed]
- Ministery of Health, Welfare and Sports. National Health Policy 2016–2019; Ministery of Health, Welfare and Sports: The Hague, The Netherlands, 2015.
- de Jong, M. Voorstad on the Move, Projectplan. 2016. Available online: https://www.fnozorgvoorkansen.nl/project/gezond-in-voorstad/ (accessed on 20 September 2018).
- Neigbourhoodsmonitor Deventer. Available online: http://www.staatvandeventer.nl/svd/wijkenmonitor-in/4/3 (accessed on 12 June 2017).
- Harting, J.; Kunst, A.; Kwan, A.; Stronks, K. A ’health broker’ role as a catalyst of change to promote health: An experiment in deprived Dutch neighbourhoods. Heal. Promot. Int. 2010, 26, 65–81. [Google Scholar] [CrossRef] [PubMed]
- van Rinsum, C.E.; Gerards, S.M.P.L.; Rutten, G.M.; van de Goor, I.A.M.; Kremers, S.P.J. Health Brokers: How Can They Help Deal with the Wickedness of Public Health Problems? BioMed. Res. Int. 2017, 2017, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Laverack, G.; la Bonte, R. A planning framework for community empowerment goals within health promotion. Heal. Policy Plan. 2000, 15, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Baum, F.; MacDougall, C.; Smith, D. Participatory action research. J. Epidemiol. Community Heal. 2006, 60, 854–857. [Google Scholar] [CrossRef]
- Laverack, G.; Mohammadi, N.K. What remains for the future: Strengthening community actions to become an integral part of health promotion practice? Heal. Promot. Int. 2011, 26, 2. [Google Scholar] [CrossRef][Green Version]
- Glanz, K.; Rimer, B.K. Theory Briefly: A Guide for Health Promotion Practice; U.S. Department of Health and Human Services; National Institutes of Health: San Francisco, CA, USA, 2005; p. 52. [CrossRef]
- Saan, H.; de Haes, W. Promoting Healthy Effects; Organising Effective Health Promotion; NIGZ: Woerden, The Netherlands, 2005. [Google Scholar]
- Rice, M.; Franceschini, M.C. Lessons learned from the application of a participatory evaluation methodology to healthy municipalities, cities, and communities’ initiatives in selected countries of the Americas. Promot. Educ. 2007, 14, 68–73. [Google Scholar] [CrossRef]
- Risisky, D.; Hogan, V.K.; Kane, M.; Burt, B.; Dove, C.; Payton, M. Concept mapping as a tool to engage a community in health disparity identification. Ethn. Dis. 2008, 18, 77–83. [Google Scholar]
- van Bon-Martens, M.; van de Goor, L.; Holsappel, J.; Kuunders, T.; der Bruggen, M.J.-V.; Brake, J.T.; van Oers, H. Concept mapping as a promising method to bring practice into science. Public Heal. 2014, 128, 504–514. [Google Scholar] [CrossRef]
- Conceição, S.C.O.; Samuel, A.; Biniecki, S.M.Y. Using concept mapping as a tool for conducting research: An analysis of three approaches. Cogent Soc. Sci. 2017, 3, 3. [Google Scholar] [CrossRef]
- Burke, J.G.; O’Campo, P.; Peak, G.L.; Gielen, A.C.; McDonnell, K.A.; Trochim, W.M.K. An Introduction to Concept Mapping as a Participatory Public Health Research Method. Qual. Heal. Res. 2005, 15, 1392–1410. [Google Scholar] [CrossRef] [PubMed]
- Trochim, W.M. An introduction to concept mapping for planning and evaluation. Eval. Program Plan. 1989, 12, 1–16. [Google Scholar] [CrossRef]
- Vaughn, L.M.; Jacquez, F.; Marschner, D.; McLinden, D. See what we say: Using concept mapping to visualize Latino immigrant’s strategies for health interventions. Int. J. Public Heal. 2016, 61, 837–845. [Google Scholar] [CrossRef] [PubMed]
- van Bon-Martens, M.J.; van de Goor, I.A.; van Oers, H. Concept mapping as a method to enhance evidence-based public health. Eval. Program Plan. 2017, 60, 213–228. [Google Scholar] [CrossRef]
- Trochim, W.; Kane, M. Concept mapping: An introduction to structured conceptualization in health care. Int. J. Qual. Heal. Care 2005, 17, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Wordclouds. Available online: www.wordclouds.com (accessed on 5 June 2017).
- Bushnell, F.K.L.; Cook, T.H.; Wells, N.; Johnson, R. The meaning of health to the low-income patients in a primary care center. J. Heal. Care Poor Underser. 2000, 11, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Nagelhout, G.E.; Verhagen, D.; Loos, V.; de Vries, H. Belangrijke randvoorwaarden bij de ontwikkeling van leefstijlinterventies voor mensen met een lage sociaaleconomische status. TSG 2018, 96, 37–45. [Google Scholar] [CrossRef]
- Broeder, L.D.; Chung, K.Y.; Geelen, L.; Scholtes, M.; Schuit, J.; Wagemakers, A. We are all experts! Does stakeholder engagement in health impact scoping lead to consensus? A Dutch case studies. Impact Assess. Proj. Apprais. 2016, 34, 294–305. [Google Scholar] [CrossRef]
- Flinterman, F.; Bisscheroux, P.; Dijkema, P.; Hertog, F.D.; de Jong, M.; Vermeer, A.; Vosjan, M. Positieve Gezondheid en gezondheidspercepties van mensen met een lage SES. TSG 2019, 97, 96–105. [Google Scholar] [CrossRef]
- Hughner, R.S.; Kleine, S.S. Views of health in the lay sector: A compilation and review of how individuals think about health. Heal. Interdiscip. J. Soc. Study Heal. Illn. Med. 2004, 8, 395–422. [Google Scholar] [CrossRef]
- Teuscher, D.; Bukman, A.J.; van Baak, M.; Feskens, E.; Renes, R.J.; Meershoek, A. Challenges of a healthy lifestyle for socially disadvantaged people of Dutch, Moroccan and Turkish origin in the Netherlands: A focus group study. Crit. Public Heal. 2014, 25, 615–626. [Google Scholar] [CrossRef] [PubMed]
- Wagemakers, A. Community Health Promotion; Facilitating and Evaluating Coordinated Action to Create Supportive Social Environments; Thesis Wageningen University: Wageningen, The Netherlands, 2010; p. 192. ISBN 978-90-8585-630-6. [Google Scholar]
- Broeder, L.D.; Uiters, E.; Hofland, A.; Wagemakers, A.; Schuit, J. Local professional’s perceptions of health assets in a low-SES Dutch neighbourhood: A qualitative study. BMC Public Heal. 2017, 18, 12. [Google Scholar] [CrossRef]
- Maller, C. Understanding health through social practices: Performance and materiality in everyday life. Sociol. Heal. Illn. 2015, 37, 52–66. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.; Diez, J.; Gullón, P.; Margolles, M.; Cofiño, R.; Pasarín, M.; Borrell, C. Towards a policy relevant neighborhoods and health agenda: Engaging citizens, researchers, policy makers and public health professionals. SESPAS Report 2018. Gac. Sanit. 2018, 32, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Wagemakers, A.; Corstjens, R.; Koelen, M.; Vaandrager, L.; Riet, H.V.; Dijkshoorn, H. Participatory approaches to promote healthy lifestyles among Turkish and Moroccan women in Amsterdam. Promot. Educ. 2008, 15, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Golden, S.D.; Earp, J.A.L. Social Ecological Approaches to Individuals and Their Contexts. Heal. Educ. Behav. 2012, 39, 364–372. [Google Scholar] [CrossRef]
- Baum, F. Cracking the nut of health equity: Top down and bottom up pressure for action on the social determinants of health. Promot. Educ. 2007, 14, 90–95. [Google Scholar] [CrossRef]
- Herens, M.; Wagemakers, A. Assessing participant’s perceptions on group-based principles for action in community-based health enhancing physical activity programmes: The APEF tool. Eval. Program Plan. 2017, 65, 54–68. [Google Scholar] [CrossRef]
- McNaught, C.; Lam, P. Using wordle as a supplementary research tool. Qual Rep. 2010, 15, 630–643. Available online: https://nsuworks.nova.edu/tqr/vol15/iss3/8 (accessed on 5 June 2020).
- Herens, M.; Wagemakers, A.; Vaandrager, L.; Koelen, M.A. Exploring participant appreciation of group-based principles for action in community-based physical activity programs for socially vulnerable groups in the Netherlands. BMC Public Heal. 2015, 15, 1173. [Google Scholar] [CrossRef]

| Name | Participants Total Session * 1 2 | Sex | Mean Age | Ethnic Background | Occupational Status | Educational Status | |||
|---|---|---|---|---|---|---|---|---|---|
| 1 | Adolescents’ group AG | 11 | 11 | - ** | Male: 5 Female: 6 | 17 (14–30) | Dutch: 11 | Student: 10 Employed: 1 | Low: 4 Medium: 5 High: 2 |
| 2 | Language group LG | 10 | 8 | 7 | Male: 2 Female: 8 | 40 (27–66) | Dutch: 2 Turkish: 4 Syrian: 2 Other: 3 | Employed: 1 Unemployed: 8 Retired: 1 | Low: 6 Medium: 2 High: 2 |
| 3 | Yoga group YG | 8 | 7 | 5 | Male: 0 Female: 8 | 71 (57–79) | Dutch: 8 | Employed: 2 Unemployed: 1 Retired: 5 | Low: 4 Medium: 1 High: 3 |
| 4 | Knitting group KG | 9 | 8 | 9 | Male: 0 Female: 9 | 73 (53–92) | Dutch: 9 | Employed: 3 Retired: 6 | Low: 6 Medium: 1 High: 2 |
| 5 | Walking group WG | 7 | 7 | 4 | Male: 4 Female: 3 | 69 (64–77) | Dutch: 7 | Unemployed: 1 Retired: 6 | Low: 4 Medium: 1 High: 2 |
| 6 | Residents’ group A RA | 7 | 6 | 4 | Male: 1 Female: 6 | 61 (22–77) | Dutch: 3 Turkish: 3 Indonesia: 1 | Employed: 1 Unemployed: 2 Retired: 4 | Low: 6 Medium: 1 |
| 7 | Residents’ group B RB | 10 | 10 | - ** | Male: 3 Female: 7 | 72 (57–82) | Dutch: 10 | Employed: 1 Unemployed: 1 Retired: 8 | Low: 8 High: 2 |
| 8 | Residents’ group M RM | 8 | 4 | 8 | Male: 5 Female: 3 | 47 (16–69) | Dutch: 8 | Employed: 2 Unemployed: 2 Retired: 2 Student: 2 | Low: 3 Medium: 3 High: 2 |
| 9 | Volunteers’ community centre VD | 4 | 4 | - ** | Male: 3 Female: 1 | 69 (66–71) | Dutch: 4 | Retired: 4 | Medium: 2 Unknown: 2 |
| 10 | Volunteers’ play garden VS | 6 | 6 | 6 | Female: 6 | 37 (31–47) | Dutch: 5 East Europe: 1 | Unemployed: 6 | Low: 6 |
| 11 | Women’s group VC | 9 | 9 | - ** | Male: 1 Female: 8 | 67 (44–87) | Dutch: 8 Polish: 1 | Employed: 4 Unemployed: 1 Retired: 4 | Low: 8 High: 1 |
| TOTAL | 89 | Male: 24 Female: 65 | Employed: 15 Unemployed: 22 Retired: 40 Student: 10 | Low: 55 Medium: 16 High: 16 Unknown: 2 | |||||
| 1. Preparation | Recruiting participants and defining questions and focus of group sessions. | |
| First group session ‘What does feeling healthy mean to you?’ | 2. Idea generation | Participants individually wrote words or statements that they associated with health on separate cards. |
| 3. Structuring the ideas | With all cards collected, the group composed clusters of words/statements that belonged together and assigned a name to each cluster. | |
| 4. Representation | Participants individually selected the three most important clusters. The rankings resulted in a group rating from 1 (most important) to 10 (least important). | |
| Second group session ‘What do you need to retain/improve health?’ | 5. Interpretation | The results of the first focus group session, clusters as well as ranking, were fed back in a second session. Needs and wishes for improving health were inventoried and discussed. |
| 6. Utilization | Resources, facilitators, barriers, and ideas about health-improving actions were explored. A visual representation of the results of this session was made by a cartoonist. All the results of both sessions were brought together and used as inputs for the VoM health promotion program. |
| Perceptions | # Number of Groups Mentioned | Quotes | Actions to Improve Health |
|---|---|---|---|
| Social relations | 10 | “Relations, I think, are very important, with other people. Has to do with health as well.” (WG) “Look, as soon as one doesn’t have social relations, you are getting lonely and loneliness is bad for your health.” (VD) | Participate in one of the community or activity groups Activities in neighborhood centers |
| Physical activity | 10 | “If you keep on moving, you experience; I feel healthy.” (YG) “When I’ve been swimming; I feel relaxed and then afterwards I can pay attention to my child and be fully present.” (VS) | Swimming lessons Biking buddy Walking, yoga, Zumba |
| Positive life attitude | 9 | “Just always putting the focus on positive things.” (AG) “Seize the day, that’s what I always say.” (YG) “To stay healthy, you need to think positively about all problems.” (LG) | No specific actions |
| Healthy eating | 8 | “Food and eating have different aspects, like enjoying it, but also you simply need it.” (RB) “Healthy eating, making tasty soup and … don’t eat too much.” (LG) | Cooking workshops (adolescents, Turkish women) |
| Being in control/empowered | 7 | “That I can decide about what to do and what not.” (YG) “Being able to do everything by yourself; self-dependence.” (RA) | Course “Looking for sense” |
| Relaxation/mental rest | 7 | “It’s a way of relaxing and taking time for myself.” (RM) “No duties, everything is allowed, well... everything …. Ha ha.” (LG) | No specific actions |
| Natural environment | 6 | “Spending time outside is relaxing, a kind of rest.” (YG) “Being outdoors is a piece of happiness.” (YG) “Fresh air also has something to do with it, with health.” (RB) | No specific actions |
| Supportive of Health | Barriers to Improving Health |
|---|---|
| Social environment, friends “….. because you are in contact, you matter again.” (YG) Doing things together, collaboration, giving and asking for help “… but there are people surrounding you, that care and want to give help.” (RB) “If you get started together, I mean having social interactions with other people, then it becomes easier to accept yourself as well.” (RM) Acceptance, openness about the situation “It does not work, or it works with some extra effort. That doesn’t matter. It’s all part of getting older, I always say.” (RB) Self-confidence, focus on possibilities “It is just that you should better not complain but just hop on your bike and go.” (KG) Character traits like perseverance, courage, being strong, and taking the initiative “With a strong character, one does everything with perseverance and confidence. A strong character is what you need.” (VS) A dog (pat) “With a dog, you get enough physical activity.” (KG) Bike, e-bike “A special low step through bike; very nice and now I can use it more.” (KG) | Cultural aspects “It depends on, I think, the family and culture you grow up with. What the habits are.” (KG) Beliefs, convictions “Your own thoughts can hinder you, you know.” (RB) Physical impediments “I have a lot of physical impediments. Still, I would feel like being the same as before; a very competitive person I am. And because of that, I’ve lost my quality of life.” (RM) “I really find it difficult not to be able to open a jar of marmalade for example.” (RB) (Chronic) Diseases and illness “I only have 50% lung capacity, so I am permanently, when doing something, I am always out of breath.” (RM) Financial aspects, money “A lot of things just cost a lot, for me too. I have four children and I am getting older and it all becomes very expensive.” (VS) Language “Often, things go wrong because of the talking and the language barrier that one has.” (RA) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Jong, M.A.J.G.; Wagemakers, A.; Koelen, M.A. “We Don’t Assume That Everyone Has the Same Idea About Health, Do We?” Explorative Study of Citizens’ Perceptions of Health and Participation to Improve Their Health in a Low Socioeconomic City District. Int. J. Environ. Res. Public Health 2020, 17, 4958. https://doi.org/10.3390/ijerph17144958
de Jong MAJG, Wagemakers A, Koelen MA. “We Don’t Assume That Everyone Has the Same Idea About Health, Do We?” Explorative Study of Citizens’ Perceptions of Health and Participation to Improve Their Health in a Low Socioeconomic City District. International Journal of Environmental Research and Public Health. 2020; 17(14):4958. https://doi.org/10.3390/ijerph17144958
Chicago/Turabian Stylede Jong, Marja A. J. G., Annemarie Wagemakers, and Maria A. Koelen. 2020. "“We Don’t Assume That Everyone Has the Same Idea About Health, Do We?” Explorative Study of Citizens’ Perceptions of Health and Participation to Improve Their Health in a Low Socioeconomic City District" International Journal of Environmental Research and Public Health 17, no. 14: 4958. https://doi.org/10.3390/ijerph17144958
APA Stylede Jong, M. A. J. G., Wagemakers, A., & Koelen, M. A. (2020). “We Don’t Assume That Everyone Has the Same Idea About Health, Do We?” Explorative Study of Citizens’ Perceptions of Health and Participation to Improve Their Health in a Low Socioeconomic City District. International Journal of Environmental Research and Public Health, 17(14), 4958. https://doi.org/10.3390/ijerph17144958






