Big Data-Driven Determinants of Length of Stay for Patients with Hip Fracture
Abstract
1. Introduction
2. Subjects and Methods
3. Results
4. Discussion
5. Conclusions
Funding
Conflicts of Interest
References
- Castelli, A.; Daidone, S.; Jacobs, R.; Kasteridis, P.; Street, A.D. The determinants of costs and length of stay for hip fracture patients. PLoS ONE 2015, 10, e0133545. [Google Scholar] [CrossRef] [PubMed]
- Ström, O.; Borgström, F.; Kanis, J.A.; Compston, J.; Cooper, C.; McCloskey, E.V.; Jönsson, B. Osteoporosis: Burden, health care provision and opportunities in the EU. Arch. Osteoporos. 2011, 6, 59–155. [Google Scholar] [CrossRef] [PubMed]
- Haentjens, P.; Lamraski, G.; Boonen, S. Costs and consequences of hip fracture occurrence in old age: An economic perspective. Disabil. Rehabil. 2005, 27, 1129–1141. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsen, B.; Van Staa, T.; Ariely, R.; Olson, M.; Cooper, C. Excess mortality following hip fracture: A systematic epidemiological review. Osteoporos. Int. 2009, 20, 1633–1650. [Google Scholar] [CrossRef] [PubMed]
- Panula, J.; Pihlajamäki, H.; Mattila, V.M.; Jaatinen, P.; Vahlberg, T.; Aarnio, P.; Kivelä, S.L. Mortality and cause of death in hip fracture patients aged 65 or older-a population-based study. BMC Musculoskelet. Disord. 2011, 12, 105. [Google Scholar] [CrossRef]
- Richmond, J.; Aharonoff, G.B.; Zuckerman, J.D.; Koval, K.J. Mortality risk after hip fracture. J. Orthop. Trauma 2003, 17, S2–S5. [Google Scholar] [CrossRef]
- Hung, W.W.; Egol, K.A.; Zuckerman, J.D.; Siu, A.L. Hip fracture management: Tailoring care for the older patient. JAMA 2012, 307, 2185–2194. [Google Scholar] [CrossRef]
- Boockvar, K.S.; Litke, A.; Penrod, J.D.; Halm, E.A.; Morrison, R.S.; Silberzweig, S.B.; Magaziner, J.; Koval, K.; Siu, A.L. Patient relocation in the 6 months after hip fracture: Risk factors for fragmented care. J. Am. Geriatr. Soc. 2004, 52, 1826–1831. [Google Scholar] [CrossRef]
- Ftouh, S.; Morga, A.; Swift, C. Management of hip fracture in adults: Summary of NICE guidance. BMJ 2011, 342, d3304. [Google Scholar] [CrossRef]
- Moore, L.; Cisse, B.; Kuimi, B.L.B.; Stelfox, H.T.; Turgeon, A.F.; Lauzier, F.; Clèment, J.; Bourgeois, G. Impact of socio-economic status on hospital length of stay following injury: A multicenter cohort study. BMC Health Serv. Res. 2015, 15, 285. [Google Scholar] [CrossRef]
- Youn, K.I. Comparison of Health Care Utilization Patterns and Length of Stay Determinants between Fracture Patients with Workers’ Compensation Insurance and National Health Insurance. Korean J. Health Serv. Manage. 2015, 9, 131–144. [Google Scholar] [CrossRef][Green Version]
- Kwon, C.I.; Kim, J.H.; Kim, J.H.; Lee, S.H. Social-economic effects of integrating insurance review system: National Health Insurance, automobile insurance and work accident insurance. Health Soc. Sci. 2007, 20, 105–125. [Google Scholar]
- Caminiti, C.; Meschi, T.; Braglia, L.; Diodati, F.; Iezzi, E.; Marcomini, B.; Nouvenne, A.; Palermo, E.; Prati, B.; Schianchi, T.; et al. Reducing unnecessary hospital days to improve quality of care through physician accountability: A cluster randomised trial. BMC Health Serv. Res. 2013, 13, 14. [Google Scholar] [CrossRef] [PubMed]
- Covinsky, K.E.; Palmer, R.M.; Fortinsky, R.H.; Counsell, S.R.; Stewart, A.L.; Kresevic, D.; Burant, C.J.; Landefeld, C.S. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. J. Am. Geriatr. Soc. 2003, 51, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Shojania, K.G.; Duncan, B.W.; McDonald, K.M.; Wachter, R.M. Safe but sound: Patient safety meets evidence-based medicine. JAMA 2002, 288, 508–513. [Google Scholar] [CrossRef]
- WHO. Estimates of unit costs for patient services for Canada. Available online: http://www.int/choice/country/can/cost/en/index.html (accessed on 26 April 2014).
- Li, P.; Kim, M.M.; Doshi, J.A. Comparison of the performance of the CMS Hierarchical Condition Category (CMS-HCC) risk adjuster with the Charlson and Elixhauser comorbidity measures in predicting mortality. BMC Health Serv. Res. 2010, 10, 245. [Google Scholar] [CrossRef]
- Won, J.W. Workers’ Compensation and Moral Hazard. Available online: http://inochong.org/index.php?mid=ebook1&page=6&document_srl=1626 (accessed on 11 June 2016).
- Mun, S.H.; Park, E.J. A study of factors influencing claim duration of injured workers. Korean Soc. Secur. Stud. 2010, 26, 215–237. [Google Scholar]
- Nikkel, L.E.; Fox, E.J.; Black, K.P.; Davis, C.; Andersen, L.; Hollenbeak, C.S. Impact of comorbidities on hospitalization costs following hip fracture. JBJS 2012, 94, 9–17. [Google Scholar] [CrossRef]
- Sund, R.; Riihimäki, J.; Mäkelä, M.; Vehtari, A.; Lüthje, P.; Huusko, T.; Häkkinen, U. Modeling the length of the care episode after hip fracture: Does the type of fracture matter? Scand. J. Surg. 2009, 98, 169–174. [Google Scholar] [CrossRef]
- Ruestow, P.S.; Friedman, L.S. Characterizing the relationship between in-hospital measures and workers’ compensation outcomes among severely injured construction workers using a data linkage strategy. Am. J. Ind. Med. 2013, 56, 1149–1156. [Google Scholar] [CrossRef]
- Schmidt, A.H.; Asnis, S.E.; Gi, H.; Koval, K.J.; Thorngren, K.G. Femoral neck fractures. Instr. Course Lect. 2005, 54, 417–445. [Google Scholar] [CrossRef]
- Choi, H.J. Effect of surgery on mortality after hip fracture in elderly: Focused on timing of surgery. Unpublished doctoral dissertation. Hanyang University, Seoul, Koera, 2012. [Google Scholar]
- Shin, C.S.; Choi, H.J.; Kim, M.J.; Kim, J.T.; Yu, S.H.; Koo, B.K.; Cho, H.Y.; Cho, S.W.; Kim, S.W.; Park, Y.J.; et al. Prevalence and risk factors of osteoporosis in Korea: A community-based cohort study with lumbar spine and hip bone mineral density. Bone 2010, 47, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Ha, Y.C.; Jang, S.; Jang, S.; Yoon, H.K.; Lee, Y.K. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J. Bone Miner. Metab. 2011, 29, 744–751. [Google Scholar] [CrossRef]
- Hagino, H.; Furukawa, K.; Fujiwara, S.; Okano, T.; Katagiri, H.; Yamamoto, K.; Teshima, R. Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos. Int. 2009, 20, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Ireland, A.W.; Kelly, P.J.; Cumming, R.G. Total hospital stay for hip fracture: Measuring the variations due to pre-fracture residence, rehabilitation, complications and comorbidities. BMC Health Serv. Res. 2015, 15, 17. [Google Scholar] [CrossRef] [PubMed]
| Variables | National Health | Medicare | Others | Total |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | |
| Gender | ||||
| Male | 528 (28.6) | 72 (27.9) | 99 (72.8) | 699 (31.2) |
| Female | 1316 (71.4) | 186 (72.1) | 37 (27.2) | 1539 (68.8) |
| Age | ||||
| ≤44 | 57 (3.1) | 6 (2.3) | 27 (19.9) | 90 (4.0) |
| 45–64 | 188 (10.2) | 42 (16.3) | 47 (34.6) | 277 (12.4) |
| ≥65 | 1599 (86.7) | 210 (81.4) | 62 (45.6) | 1871 (83.6) |
| Admission route | ||||
| Emergency | 1525 (82.7) | 211 (81.8) | 115 (84.6) | 1851 (82.7) |
| Outpatient | 319 (17.3) | 47 (18.2) | 21 (15.4) | 387 (17.3) |
| Result of treatment | ||||
| Improved | 1690 (91.6) | 236 (91.5) | 130 (95.6) | 2056 (91.9) |
| Not improved | 154 (8.4) | 22 (8.5) | 6 (4.4) | 182 (8.1) |
| Operation | ||||
| No | 341 (18.5) | 53 (20.5) | 31 (22.8) | 425 (19.0) |
| Yes | 1503 (81.5) | 205 (79.5) | 105 (77.2) | 1813 (81.0) |
| Hospital beds | ||||
| 100–299 | 694 (37.6) | 131 (50.8) | 52 (38.2) | 877 (39.2) |
| 300–499 | 160 (8.7) | 28 (10.9) | 19 (14.0) | 207 (9.2) |
| 500–999 | 815 (44.2) | 85 (32.9) | 54 (39.7) | 954 (42.6) |
| ≥1000 | 175 (9.5) | 14 (5.4) | 11 (8.1) | 200 (8.9) |
| Comorbidity | Number of Patients, (%) | Mean LOS, SD | t | p | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Congestive heart failure | 41 (1.8) | 26.63 ± 21.04 | 24.05 ± 22.17 | −0.74 | 0.46 |
| Cardiac arrhythmia | 60 (2.7) | 23.12 ± 18.28 | 24.13 ± 22.25 | 0.35 | 0.73 |
| Valvular disease | 24 (1.1) | 24.50 ± 20.30 | 24.10 ± 22.18 | −0.09 | 0.93 |
| Pulmonary circulation disease | 20 (0.9) | 23.55 ± 13.94 | 24.11 ± 22.21 | 0.11 | 0.91 |
| Peripheral vascular disease | 18 (0.8) | 29.61 ± 20.89 | 24.06 ± 22.16 | −1.06 | 0.29 |
| Hypertension | 594 (26.5) | 25.64 ± 23.60 | 23.55 ± 21.59 | −1.97 | <0.05 |
| Hypertension, complicated | 13 (0.6) | 26.69 ± 19.77 | 24.09 ± 22.17 | −0.42 | 0.67 |
| Paralysis | 9 (0.4) | 45.00 ± 44.14 | 24.02 ± 21.20 | −1.43 | 0.19 |
| Neurological disorder | 46 (2.1) | 27.41 ± 20.43 | 24.03 ± 22.19 | −1.03 | 0.31 |
| Chronic pulmonary disease | 60 (2.7) | 28.83 ± 20.13 | 23.97 ± 22.20 | −1.68 | 0.94 |
| Diabetes | 345 (15.4) | 25.70 ± 25.77 | 23.81 ± 21.42 | −1.46 | 0.15 |
| Diabetes, complicated | 38 (1.7) | 30.92 ± 18.29 | 23.98 ± 22.19 | −1.92 | 0.06 |
| Hypothyroidism | 20 (0.9) | 27.90 ± 22.48 | 24.07 ± 22.15 | −0.77 | 0.44 |
| Renal failure | 90 (4.0) | 25.04 ± 19.53 | 24.06 ± 22.26 | −0.41 | 0.68 |
| Liver disease | 30 (1.3) | 30.80 ± 21.70 | 24.01 ± 22.15 | −1.67 | 0.10 |
| Peptic ulcer disease | 6 (0.3) | 45.83 ± 19.22 | 24.04 ± 22.14 | −2.41 | <0.05 |
| Lymphoma | 2 (0.1) | 13.00 ± 5.66 | 24.11 ± 22.16 | 0.71 | 0.48 |
| Metastatic cancer | 4 (0.2) | 26.00 ± 14.17 | 24.10 ± 22.17 | −0.17 | 0.86 |
| Solid tumor | 19 (0.8) | 34.00 ± 29.67 | 24.02 ± 22.07 | −1.46 | 0.16 |
| Rheumatoid arthritis | 9 (0.4) | 21.33 ± 13.71 | 24.11 ± 22.18 | 0.38 | 0.71 |
| Coagulopathy | 9 (0.4) | 40.89 ± 26.72 | 24.03 ± 22.11 | −2.28 | <0.05 |
| Weight loss | 3 (0.1) | 21.67 ± 0.58 | 24.10 ± 22.17 | 0.19 | 0.85 |
| Electrolyte disorder | 34 (1.5) | 29.53 ± 23.80 | 24.02 ± 22.12 | −1.44 | 0.15 |
| Deficiency anemia | 22 (1.0) | 27.91 ± 25.45 | 24.06 ± 22.12 | −0.81 | 0.42 |
| Alcohol abuse | 12 (0.5) | 40.75 ± 26.84 | 24.01 ± 22.10 | −2.61 | <0.05 |
| Psychosis | 13 (0.6) | 48.00 ± 57.47 | 23.96 ± 21.74 | −1.51 | 0.16 |
| Depression | 32 (1.4) | 34.13 ± 58.19 | 23.96 ± 21.18 | −0.99 | 0.33 |
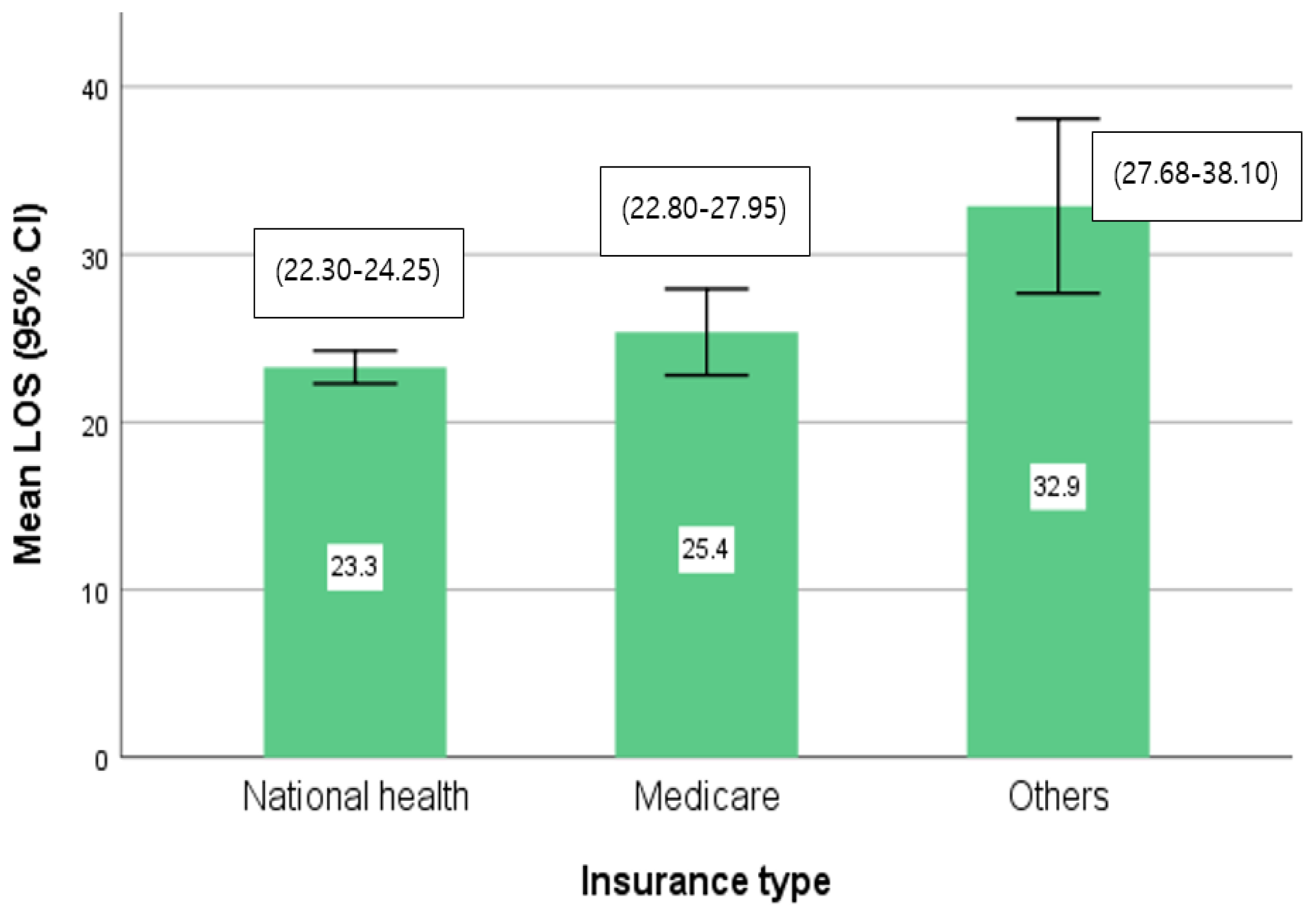
| Variables | National Health | Medicare | Others | |||
|---|---|---|---|---|---|---|
| Mean, SD | p | Mean, SD | p | Mean, SD | p | |
| Gender | ||||||
| Male | 23.93 ± 25.27 | 0.45 | 24.85 ± 16.36 | 0.80 | 35.08 ± 33.92 | 0.18 |
| Female | 23.01 ± 19.65 | 25.58 ± 22.60 | 27.03 ± 18.97 | |||
| Age | ||||||
| ≤44 | 25.95 ± 47.35 | 0.26 | 32.33 ± 20.21 | 0.33 | 26.41 ± 20.54 | <0.05 |
| 45–64 | 21.23 ± 18.73 | 28.88 ± 31.04 | 43.77 ± 44.06 | |||
| ≥65 | 23.42 ± 20.20 | 24.47 ± 18.43 | 27.47 ± 17.48 | |||
| Admission route | ||||||
| Emergency | 23.12 ± 19.72 | 0.49 | 24.80 ± 18.99 | 0.35 | 32.34 ± 26.36 | 0.63 |
| Outpatient | 24.03 ± 28.15 | 27.96 ± 28.52 | 35.90 ± 48.99 | |||
| Result of treatment | ||||||
| Improved | 24.50 ± 21.54 | <0.01 | 26.08 ± 19.91 | 0.22 | 34.30 ± 30.70 | <0.05 |
| Not improved | 9.89 ± 14.22 | 17.77 ± 30.05 | 2.33 ± 3.01 | |||
| Operation | ||||||
| No | 16.43 ± 31.90 | <0.01 | 17.53 ± 19.47 | <0.01 | 36.68 ± 51.40 | 0.61 |
| Yes | 24.83 ± 17.86 | 27.40 ± 20.97 | 31.77 ± 21.40 | |||
| Hospital beds | ||||||
| 100–299 | 25.67 ± 23.78 | <0.01 | 27.77 ± 23.37 | <0.05 | 38.31 ± 36.63 | <0.05 |
| 300–499 | 28.67 ± 21.15 | 30.46 ± 29.62 | 45.58 ± 27.32 | |||
| 500–999 | 21.39 ± 19.84 | 20.61 ± 11.09 | 26.78 ± 25.77 | |||
| ≥1000 | 17.66 ± 15.96 | 21.64 ± 19.35 | 15.36 ± 6.50 | |||
| Variables | National Health Insurance | Medicare | Others | ||||||
|---|---|---|---|---|---|---|---|---|---|
| ß | t | p | ß | t | p | ß | t | p | |
| Gender | |||||||||
| Male (ref.) | |||||||||
| Female | −1.896 | −1.701 | 0.089 | 3.814 | 1.232 | 0.219 | −7.674 | −1.297 | 0.197 |
| Age | 0.018 | 0.453 | 0.650 | −0.230 | −2.220 | <0.05 | −0.016 | −0.111 | 0.912 |
| Admission route | |||||||||
| Emergency (ref.) | |||||||||
| Outpatient | −0.205 | −0.157 | 0.875 | 3.136 | 0.905 | 0.366 | −1.488 | −0.206 | 0.837 |
| Result of treatment | |||||||||
| Improved (ref.) | |||||||||
| Not improved | −13.44 | −7.119 | <0.001 | −2.056 | −0.416 | 0.678 | −37.57 | −2.876 | <0.01 |
| Operation | |||||||||
| No (ref.) | |||||||||
| Yes | 6.507 | 4.766 | <0.001 | 11.276 | 3.184 | <0.01 | −9.228 | −1.379 | 0.170 |
| Comorbidity count | 2.337 | 5.019 | <0.001 | 2.642 | 2.293 | <0.05 | 4.869 | 1.469 | 0.144 |
| Hospital beds | |||||||||
| 100–299 (ref.) | |||||||||
| 300–499 | 2.089 | 1.148 | 0.251 | 1.223 | 0.285 | 0.776 | 8.559 | 1.034 | 0.303 |
| 500–999 | −6.448 | −5.817 | <0.001 | −9.754 | −3.325 | <0.01 | −12.28 | −2.063 | <0.05 |
| ≥1000 | −10.83 | −6.117 | <0.001 | −5.567 | −0.969 | 0.333 | −23.73 | −2.401 | <0.05 |
| Adj. R2 F (p) Durbin–Watson | 0.084 19.839 (0.000) 1.864 | 0.089 3.798 (0.000) 1.958 | 0.114 2.924 (0.004) 2.034 | ||||||
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, J. Big Data-Driven Determinants of Length of Stay for Patients with Hip Fracture. Int. J. Environ. Res. Public Health 2020, 17, 4949. https://doi.org/10.3390/ijerph17144949
Lim J. Big Data-Driven Determinants of Length of Stay for Patients with Hip Fracture. International Journal of Environmental Research and Public Health. 2020; 17(14):4949. https://doi.org/10.3390/ijerph17144949
Chicago/Turabian StyleLim, Jihye. 2020. "Big Data-Driven Determinants of Length of Stay for Patients with Hip Fracture" International Journal of Environmental Research and Public Health 17, no. 14: 4949. https://doi.org/10.3390/ijerph17144949
APA StyleLim, J. (2020). Big Data-Driven Determinants of Length of Stay for Patients with Hip Fracture. International Journal of Environmental Research and Public Health, 17(14), 4949. https://doi.org/10.3390/ijerph17144949




