A System Dynamics and Participatory Action Research Approach to Promote Healthy Living and a Healthy Weight among 10–14-Year-Old Adolescents in Amsterdam: The LIKE Programme
Abstract
1. Background
Aims & Objectives
2. Theoretical Perspective
2.1. Transition from Ten to Teenager
2.2. Epistemological Pluralism
2.3. Complexity Thinking
2.4. Participatory Action Research
3. Programme Development
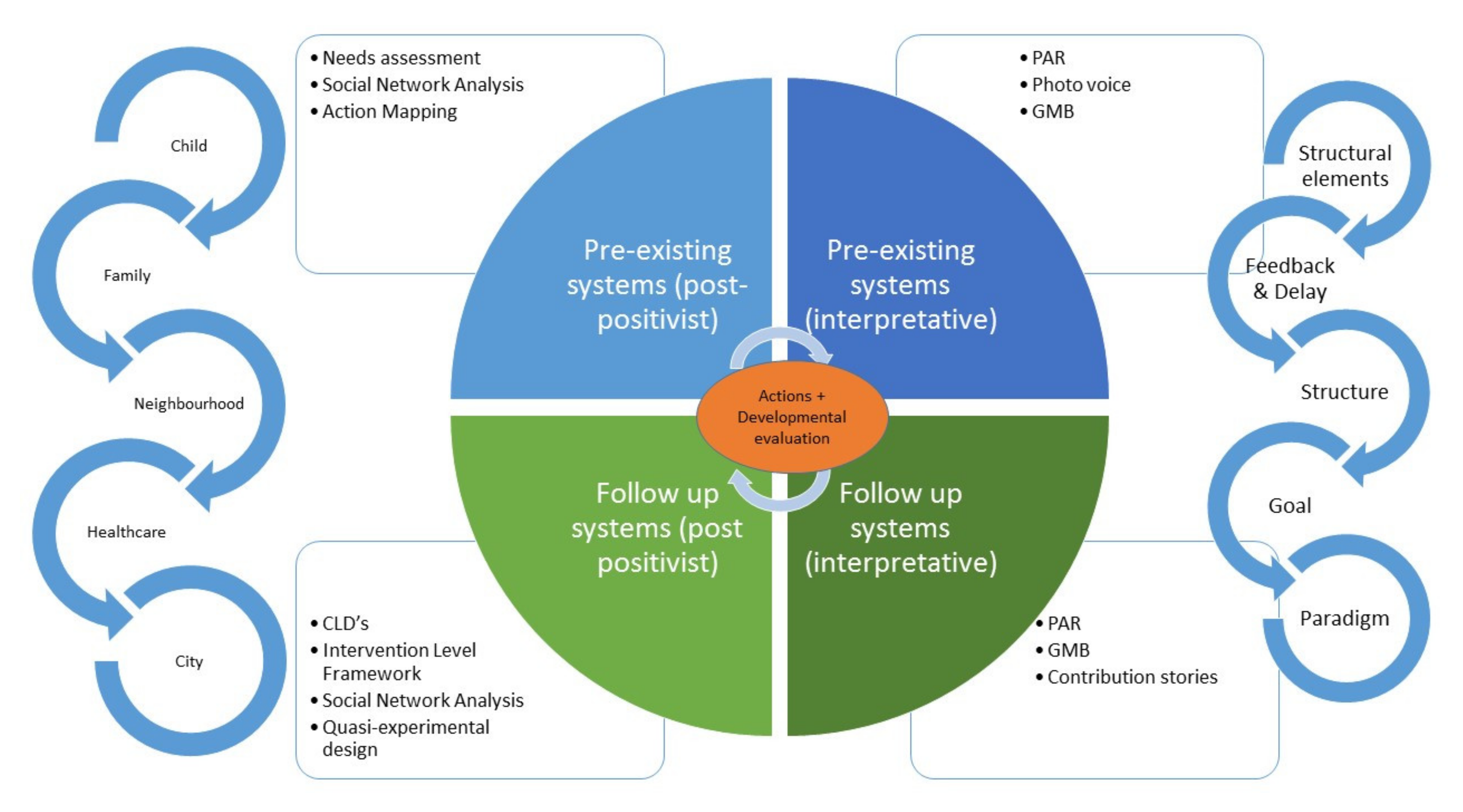
3.1. Overall Design
3.2. Understanding Pre-Existing Systems (Needs Assessment)
3.2.1. 10–14-Year-Old Adolescents and Their Families
3.2.2. Societal Stakeholders
3.3. Developing Quick and Disruptive Actions
3.3.1. Quick Actions Targeting System Elements
3.3.2. Disruptive Actions
4. Evaluation
4.1. Developmental Systems Evaluation
4.2. Evaluation to Support Action Development
4.3. Evaluation to Examine Systems Changes
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hammond, R.A. Complex systems modeling for obesity research. Prev. Chronic Dis. 2009, 6, A97. [Google Scholar]
- Signal, L.N.; Walton, M.D.; Ni Mhurchu, C.; Maddison, R.; Bowers, S.G.; Carter, K.N.; Gorton, D.; Heta, C.; Lanumata, T.S.; McKerchar, C.W.; et al. Tackling ‘wicked’ health promotion problems: A New Zealand case study. Health Promot. Int. 2013, 28, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Klijn, E.H.; Koppenjan, J. Governance Networks in the Public Sector; Routledge: New York, NY, USA, 2016. [Google Scholar]
- Hendriks, A.M.; Jansen, M.W.J.; Gubbels, J.S.; De Vries, N.K.; Molleman, G.; Kremers, S.P.J. Local government officials’ views on intersectoral collaboration within their organization-A qualitative exploration. Health Policy Technol. 2015, 4, 47–57. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.L.; Gortmaker, S.L. Obesity 1 The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- Sniehotta, F.F.; Araujo-Soares, V.; Brown, J.; Kelly, M.P.; Michie, S.; West, R. Complex systems and individual-level approaches to population health: A false dichotomy? Lancet Public Health 2017, 2, e396–e397. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. Lancet 2019, 393, 791–846. [Google Scholar] [CrossRef]
- Lloyd, J.; Creanor, S.; Logan, S.; Green, C.; Dean, S.G.; Hillsdon, M.; Abraham, C.; Tomlinson, R.; Pearson, V.; Taylor, R.S.; et al. Effectiveness of the Healthy Lifestyles Programme (HeLP) to prevent obesity in UK primary-school children: A cluster randomised controlled trial. Lancet Child Adolesc. Health 2018, 2, 35–45. [Google Scholar] [CrossRef]
- Durlak, J.A.; DuPre, E.P. Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am. J. Community Psychol. 2008, 41, 327–350. [Google Scholar] [CrossRef]
- Scheirer, M.A. Is sustainability possible? A review and commentary on empirical studies of program sustainability. Am. J. Eval. 2005, 26, 320–347. [Google Scholar] [CrossRef]
- Hawe, P.; Shiell, A.; Riley, T. Theorising Interventions as Events in Systems. Am. J. Community Psychol. 2009, 43, 267–276. [Google Scholar] [CrossRef]
- O’Mara-Eves, A.; Brunton, G.; Oliver, S.; Kavanagh, J.; Jamal, F.; Thomas, J. The effectiveness of community engagement in public health interventions for disadvantaged groups: A meta-analysis. BMC Public Health 2015, 15, 129. [Google Scholar] [CrossRef]
- Matheson, A.; Walton, M.; Gray, R.; Lindberg, K.; Shantakumar, M.; Fyfe, C.; Wehipeihana, N.; Borman, B. Evaluating a community-based public health intervention using a complex systems approach. J. Public Health 2018, 40, 606–613. [Google Scholar] [CrossRef]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ-Brit. Med. J. 2015, 350. [Google Scholar] [CrossRef]
- Rutter, H.; Savona, N.; Glonti, K.; Bibby, J.; Cummins, S.; Finegood, D.T.; Greaves, F.; Harper, L.; Hawe, P.; Moore, L.; et al. The need for a complex systems model of evidence for public health. Lancet 2017, 390, 2602–2604. [Google Scholar] [CrossRef]
- Moore, G.F.; Evans, R.E.; Hawkins, J.; Littlecott, H.; Melendez-Torres, G.J.; Bonell, C.; Murphy, S. From complex social interventions to interventions in complex social systems: Future directions and unresolved questions for intervention development and evaluation. Evaluation-US 2019, 25, 23–45. [Google Scholar] [CrossRef] [PubMed]
- Allender, S.; Brown, A.D.; Bolton, K.A.; Fraser, P.; Lowe, J.; Hovmand, P. Translating systems thinking into practice for community action on childhood obesity. Obes. Rev. 2019, 20, 179–184. [Google Scholar] [CrossRef]
- Carey, G.; Malbon, E.; Carey, N.; Joyce, A.; Crammond, B.; Carey, A. Systems science and systems thinking for public health: A systematic review of the field. BMJ Open 2015, 5, e009002. [Google Scholar] [CrossRef] [PubMed]
- Bagnall, A.M.; Radley, D.; Jones, R.; Gately, P.; Nobles, J.; Van Dijk, M.; Blackshaw, J.; Montel, S.; Sahota, P. Whole systems approaches to obesity and other complex public health challenges: A systematic review. BMC Public Health 2019, 19, 8. [Google Scholar] [CrossRef] [PubMed]
- South, J.; Button, D.; Quick, A.; Bagnall, A.M.; Trigwell, J.; Woodward, J.; Coan, S.; Southby, K. Complexity and Community Context: Learning from the Evaluation Design of a National Community Empowerment Programme. Int. J. Environ. Res. Public Health 2019, 17, 91. [Google Scholar] [CrossRef]
- Allender, S.; Millar, L.; Hovmand, P.; Bell, C.; Moodie, M.; Carter, R.; Swinburn, B.; Strugnell, C.; Lowe, J.; de la Haye, K.; et al. Whole of Systems Trial of Prevention Strategies for Childhood Obesity: WHO STOPS Childhood Obesity. Int. J. Environ. Res. Public Health 2016, 13, 1143. [Google Scholar] [CrossRef]
- Karacabeyli, D.; Allender, S.; Pinkney, S.; Amed, S. Evaluation of complex community-based childhood obesity prevention interventions. Obes. Rev. 2018, 19, 1080–1092. [Google Scholar] [CrossRef] [PubMed]
- City of Amsterdam. Amsterdam Healthy Weight Programme. 2019. Available online: https://www.amsterdam.nl/sociaaldomein/blijven-wij-gezond/amsterdam-healthy/ (accessed on 1 December 2019).
- Patton, G.C.; Sawyer, S.M.; Santelli, J.S.; Ross, D.A.; Afifi, R.; Allen, N.B.; Arora, M.; Azzopardi, P.; Baldwin, W.; Bonell, C.; et al. Our future: A Lancet commission on adolescent health and wellbeing. Lancet 2016, 387, 2423–2478. [Google Scholar] [CrossRef]
- Seidell, J.C.; Halberstadt, J.; Noordam, H.; Niemer, S. An integrated health care standard for the management and prevention of obesity in The Netherlands. Fam. Pract. 2012, 29, i153–i156. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jones, M.; Verity, F.; Warin, M.; Ratcliffe, J.; Cobiac, L.; Swinburn, B.; Cargo, M. OPALesence: Epistemological pluralism in the evaluation of a systems-wide childhood obesity prevention program. Evaluation-US 2016, 22, 29–48. [Google Scholar] [CrossRef]
- Hudson, L.A.; Ozanne, J.L. Alternative Ways of Seeking Knowledge in Consumer Research. J. Consum. Res. 1988, 14, 508–521. [Google Scholar] [CrossRef]
- Stame, N. What doesn’t work? Three failures, many answers. Evaluation-US 2010, 16, 371–387. [Google Scholar] [CrossRef]
- Patton, M.Q. Developmental Evaluation: Applying Complexity Concepts to Enhance Innovation and Use; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Johnston, L.M.; Matteson, C.L.; Finegood, D.T. Systems Science and Obesity Policy: A Novel Framework for Analyzing and Rethinking Population-Level Planning. Am. J. Public Health 2014, 104, 1270–1278. [Google Scholar] [CrossRef] [PubMed]
- Hart, R.A. The Theory and Practice of Involving Children in Communities; Earthscan: London, UK, 1997. [Google Scholar]
- Baum, F.; MacDougall, C.; Smith, D. Participatory action research. J. Epidemiol. Community Health 2006, 60, 854–857. [Google Scholar] [CrossRef]
- Cammarota, J.; Romero, A. Participatory Action Research for High School Students: Transforming Policy, Practice, and the Personal With Social Justice Education. Educ. Policy 2011, 25, 488–506. [Google Scholar] [CrossRef]
- Rodriguez, L.F.; Brown, T.M. From voice to agency: Guiding principles for participatory action research with youth. New Dir. Youth Dev. 2009, 2009, 19–34. [Google Scholar] [CrossRef]
- Niermann, C.Y.N.; Gerards, S.M.P.L.; Kremers, S.P.J. Conceptualizing Family Influences on Children’s Energy Balance-Related Behaviors: Levels of Interacting Family Environmental Subsystems (The LIFES Framework). Int. J. Environ. Res. Public Health 2018, 15, 2714. [Google Scholar] [CrossRef] [PubMed]
- Golan, M.; Crow, S. Parents are key players in the prevention and treatment of weight-related problems. Nutr. Rev. 2004, 62, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Gesell, S.B.; Barkin, S.L.; Valente, T.W. Social network diagnostics: A tool for monitoring group interventions. Implement. Sci. 2013, 8, 116. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed, A.M.; Galea, S. Systems Science and Population Health; Oxford University Press: Oxford, UK, 2017; pp. 113–126. [Google Scholar]
- Leonard, R.; Horsfall, D.; Rosenberg, J.; Noonan, K. Carer experience of end-of-life service provision: A social network analysis. BMJ Supportive Palliat. Care 2018, 10, e20. [Google Scholar] [CrossRef]
- Parnell, J.M.; Robinson, J.C. Social Network Analysis: Presenting an Underutilised Method for Nursing Research. J. Adv. Nurs. 2018, 74, 1310–1318. [Google Scholar] [CrossRef] [PubMed]
- Luke, D.A.; Harris, J.K. Network analysis in public health: History, methods, and applications. Annu. Rev. Public Health 2007, 28, 69–93. [Google Scholar] [CrossRef]
- Prevo, L.; Mercken, L.; Jansen, M.; Kremers, S. With whom are you dealing? Using social network analysis as a tool to strengthen service delivery structures for low socioeconomic status populations. J. Public Health Res. 2018, 7, 1369. [Google Scholar] [CrossRef]
- Valente, T.W.; Palinkas, L.A.; Czaja, S.; Chu, K.H.; Brown, C.H. Social network analysis for program implementation. PLoS ONE 2015, 10, e0131712. [Google Scholar] [CrossRef]
- Meadows, D. Leverage points to intervene in a system. In Thinking in Systems; Earthscan: London, UK, 2008. [Google Scholar]
- Rouwette, E.A.J.A.; Vennix, J.A.M.; van Mullekom, T. Group model building effectiveness: A review of assessment studies. Syst. Dynam. Rev. 2002, 18, 5–45. [Google Scholar] [CrossRef]
- Siokou, C.; Morgan, R.; Shiell, A. Group model building: A participatory approach to understanding and acting on systems. Public Health Res. Pract. 2014, 25, e2511404. [Google Scholar] [CrossRef]
- Gerritsen, S.; Harre, S.; Rees, D.; Renker-Darby, A.; Bartos, A.E.; Waterlander, W.E.; Swinburn, B. Community Group Model Building as a Method for Engaging Participants and Mobilising Action in Public Health. Int. J. Environ. Res. Public Health 2020, 17, 3457. [Google Scholar] [CrossRef] [PubMed]
- Knai, C.; Petticrew, M.; Mays, N.; Capewell, S.; Cassidy, R.; Cummins, S.; Eastmure, E.; Fafard, P.; Hawkins, B.; Jensen, J.D.; et al. Systems Thinking as a Framework for Analyzing Commercial Determinants of Health. Milbank Q 2018, 96, 472–498. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. Whole Systems Approach to Obesity: A Guide to Support Local Approaches to Promoting a Healthy Weight; Public Health England: London, UK, 2019. [Google Scholar]
- Simmons, A.; Mavoa, H.M.; Bell, A.C.; De Courten, M.; Schaaf, D.; Schultz, J.; Swinburn, B.A. Creating community action plans for obesity prevention using the ANGELO (Analysis Grid for Elements Linked to Obesity) Framework. Health Promot. Int. 2009, 24, 311–324. [Google Scholar] [CrossRef]
- The Health Foundation. Evaluation: What to Consider; The Health Foundation: London, UK, 2015. [Google Scholar]
- Fagen, M.C.; Redman, S.D.; Stacks, J.; Barrett, V.; Thullen, B.; Altenor, S.; Neiger, B.L. Developmental evaluation: Building innovations in complex environments. Health Promot. Pract. 2011, 12, 645–650. [Google Scholar] [CrossRef]
- Walton, M. Applying complexity theory: A review to inform evaluation design. Eval. Program Plan. 2014, 45, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Egan, M.; McGill, E.; Penney, T.; Anderson de Cuevas, R.; Er, V.; Orton, L.; White, M.; Lock, K.; Cummins, S.; Savona, N.; et al. NIHR SPHR Guidance on Systems Approaches to Local Public Health Evaluation. Part 2: What to Consider When Planning a Systems Evaluation; National Institute for Health Research School for Public Health Research: London, UK, 2019. [Google Scholar]
- Ling, T. Evaluating complex and unfolding interventions in real time. Evaluation-US 2012, 18, 79–91. [Google Scholar] [CrossRef]
- Gerritsen, S.; Harre, S.; Swinburn, B.; Rees, D.; Renker-Darby, A.; Bartos, A.E.; Waterlander, W.E. Systemic Barriers and Equitable Interventions to Improve Vegetable and Fruit Intake in Children: Interviews with National Food System Actors. Int. J. Environ. Res. Public Health 2019, 16, 1387. [Google Scholar] [CrossRef]
- Van Koperen, M.; van Wietmarschen, M.; Seidell, J.C.; Hageraats, R. Amsterdamse Aanpak Gezond Gewicht Kansrijk? (Amsterdam Healthy Weight Approach Full of Potential?); Dutch Youth Institute: Utrecht, The Netherlands, 2018. [Google Scholar]
- Swinburn, B.; Gill, T.; Kumanyika, S. Obesity prevention: A proposed framework for translating evidence into action. Obes. Rev. 2005, 6, 23–33. [Google Scholar] [CrossRef]
- Maitland, N.; Williams, M.; Jalaludin, B.; Allender, S.; Strugnell, C.; Brown, A.; Hayward, J.; Crooks, N.; Tredoux, J.; Li, V.; et al. Campbelltown-Changing our Future: Study protocol for a whole of system approach to childhood obesity in South Western Sydney. BMC Public Health 2019, 19, 1699. [Google Scholar] [CrossRef]
- Public Health England. Whole Systems Approach to Obesity Programme: Learning from Co-Producing and Testing the Guide and Resources; Public Health England: London, UK, 2019. [Google Scholar]
- Hennessy, E.; Economos, C.D.; Hammond, R.A. Integrating Complex Systems Methods to Advance Obesity Prevention Intervention Research. Health Educ. Behav. 2020. [Google Scholar] [CrossRef]
- Kania, A.; Patel, A.B.; Roy, A.; Yelland, G.S.; Nguyen, D.T.K.; Verhoef, M.J. Capturing the complexity of evaluations of health promotion interventions—A scoping review. Can. J. Program Eval. 2012, 65–91. [Google Scholar]
| Evaluation Question | Population | Epistemology | Outcome Measures | Data Collection | Systems Principles (Based on [24,25]) | |
|---|---|---|---|---|---|---|
| Post-Positivist | Inter-Pretative | |||||
| 1. Understanding the pre-existing system in relation to health-related behaviours 1.1 Which factors and processes in the pre-existing system in Amsterdam East shape unhealthy behaviours? | Adolescents and their families | V | Pre-existing system of relevant health behaviours and determinants and how they are connected |
| Developing an understanding of the system, information from different agents, participatory methods. Question provides input for programme development | |
| Stakeholders | V | Baseline SNA | Social network analysis (baseline): mapping all the local actors who are involved with the target behaviour and are in touch with the target group and the connection between them | Information from different agents Relationship between agents | ||
| Adolescents with obesity and their families | V | V | Barriers and facilitators of support and empowerment towards sustainable healthy habits |
| Information from different agents, participatory methods. | |
| 1.2 From the perspective of adolescents/families/societal stakeholders, which factors and processes in the pre-existing system in Amsterdam East shape unhealthy behaviours? | Adolescents and their families | V | Pre-existing system/CLD from target group perspective |
| Developing an understanding of the system Participatory methods Question provides input for programme development | |
| Societal stakeholders | V | Pre-existing system/CLD from stakeholder perspective | Group Model Building with local stakeholders | Developing an understanding of the system | ||
| Adolescents with obesity and their families | V | Needs for lifestyle behaviour change by adolescents with obesity and their parents | PAR groups with adolescents with obesity and/or their parents | Developing an understanding of the system Participatory methods | ||
| 2. Developmental evaluation (process) 2.1 How does the action-programme evolve and of which action elements does it consist? | Adolescents and their families | V | Overview of activities listed by Intervention Level Framework Barriers & Facilitators |
| Developmental evaluation Dynamic Adaptation Feedback | |
| 2.2 How successful is the approach we follow in our LIKE programme in creating a sustainable programme and how can this be optimized? | Adolescents and their families | V | V | Process evaluation |
| Developmental evaluation Dynamic Adaptation Feedback |
| 3. Developmental evaluation (effect) 3.1 What type of (emergent, adaptive, reinforcing) changes occurred in the living context, what were potential unintended consequences, and how can these be related to the LIKE programme? | Adolescents and their families | V | Adapted CLDs Extent to which the adapted system is “healthier” | Actions that were implemented during the programme and plotting these on the baseline system maps (CLDs) and against Intervention Level Framework. Feedback in the baseline systems following these actions. This includes:
| Adaptation Emergence Non-linearity Case study design Multiple and mixed methods | |
| Societal stakeholders | V | Follow up SNA | Social network analysis (follow up): mapping all local actors who are involved with the target behaviour and are in touch with the target group and the connection between them | Information from different agentsRelationship between agents | ||
| 3.2 How do the target group and stakeholders perceive changes in the system and how do they perceive the contribution of activities within the LIKE programme to these changes? | V | Perceived changes Contribution (how reasonable is it to believe that the programme contributed to the observed changes?) |
| Information from different agents Contribution Participatory methods | ||
| 4. To what extent do adolescents’ behaviours and weight status improve as a result of changes in the system? | Adolescents and their families | V | Routinely collected data on BMI; diet, sleep, PA, screen time | Quasi-experimental design | Time (delay) Emergence | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Waterlander, W.E.; Luna Pinzon, A.; Verhoeff, A.; den Hertog, K.; Altenburg, T.; Dijkstra, C.; Halberstadt, J.; Hermans, R.; Renders, C.; Seidell, J.; et al. A System Dynamics and Participatory Action Research Approach to Promote Healthy Living and a Healthy Weight among 10–14-Year-Old Adolescents in Amsterdam: The LIKE Programme. Int. J. Environ. Res. Public Health 2020, 17, 4928. https://doi.org/10.3390/ijerph17144928
Waterlander WE, Luna Pinzon A, Verhoeff A, den Hertog K, Altenburg T, Dijkstra C, Halberstadt J, Hermans R, Renders C, Seidell J, et al. A System Dynamics and Participatory Action Research Approach to Promote Healthy Living and a Healthy Weight among 10–14-Year-Old Adolescents in Amsterdam: The LIKE Programme. International Journal of Environmental Research and Public Health. 2020; 17(14):4928. https://doi.org/10.3390/ijerph17144928
Chicago/Turabian StyleWaterlander, Wilma E., Angie Luna Pinzon, Arnoud Verhoeff, Karen den Hertog, Teatske Altenburg, Coosje Dijkstra, Jutka Halberstadt, Roel Hermans, Carry Renders, Jacob Seidell, and et al. 2020. "A System Dynamics and Participatory Action Research Approach to Promote Healthy Living and a Healthy Weight among 10–14-Year-Old Adolescents in Amsterdam: The LIKE Programme" International Journal of Environmental Research and Public Health 17, no. 14: 4928. https://doi.org/10.3390/ijerph17144928
APA StyleWaterlander, W. E., Luna Pinzon, A., Verhoeff, A., den Hertog, K., Altenburg, T., Dijkstra, C., Halberstadt, J., Hermans, R., Renders, C., Seidell, J., Singh, A., Anselma, M., Busch, V., Emke, H., van den Eynde, E., van Houtum, L., Nusselder, W. J., Overman, M., van de Vlasakker, S., ... Stronks, K. (2020). A System Dynamics and Participatory Action Research Approach to Promote Healthy Living and a Healthy Weight among 10–14-Year-Old Adolescents in Amsterdam: The LIKE Programme. International Journal of Environmental Research and Public Health, 17(14), 4928. https://doi.org/10.3390/ijerph17144928






