Empowering Health Workers to Protect their Own Health: A Study of Enabling Factors and Barriers to Implementing HealthWISE in Mozambique, South Africa, and Zimbabwe
Abstract
1. Introduction
2. Materials and Methods
2.1. Country Contexts
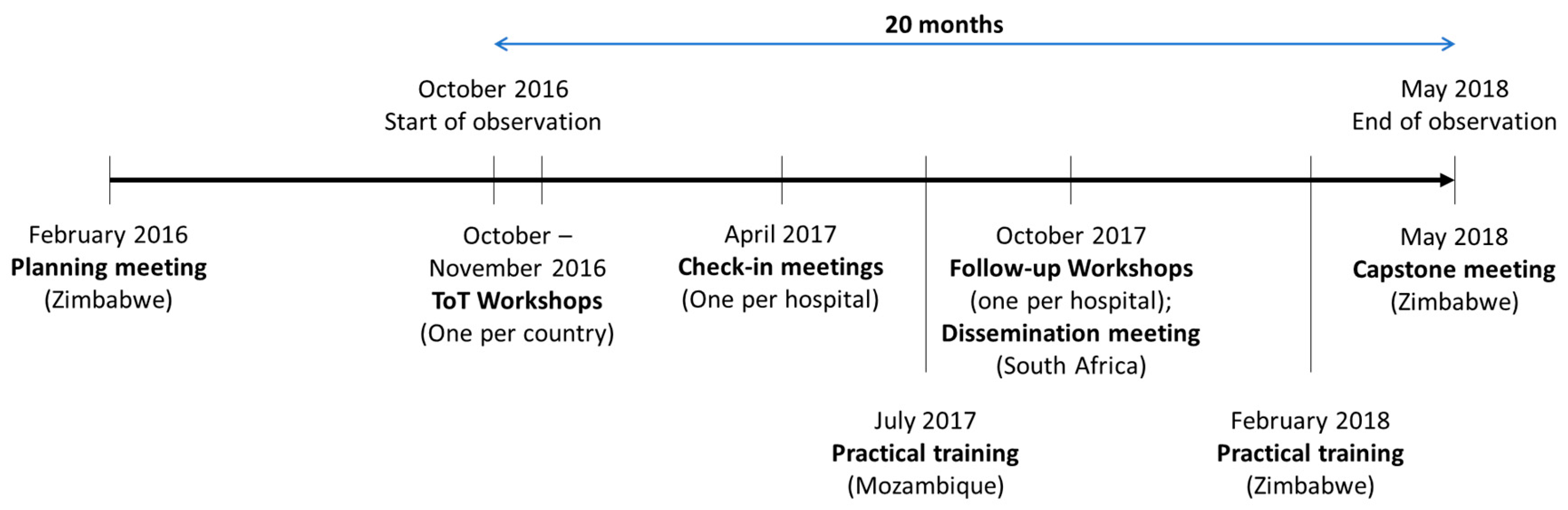
2.2. Implementation of HealthWISE
2.3. Research Methods
3. Results
3.1. Hospital Characteristics
3.2. Enabling Factors and Barriers
3.2.1. Innovation
3.2.2. Recipients
3.2.3. Context
3.2.4. Facilitation
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Campbell, J.; Buchan, J.; Cometto, G.; David, B.; Dussault, G.; Fogstad, H.; Fronteira, I.; Lozano, R.; Nyonator, F.; Pablos-Méndez, A.; et al. Human resources for health and universal health coverage: Fostering equity and effective coverage. Bull. World Health Organ. 2013, 91, 853–863. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The World Health Report 2006—Working Together for Health; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- HealthWISE—Work Improvement in Health Services. Available online: http://www.ilo.org/sector/Resources/training-materials/WCMS_250540/lang--en/index.htm (accessed on 10 April 2020).
- Madon, T.; Hofman, K.J.; Kupfer, L.; Glass, R.I. Implementation Science. Science 2007, 318, 1728–1729. [Google Scholar] [CrossRef] [PubMed]
- Yassi, A.; Zungu, M.; Spiegel, J.M.; Kistnasamy, B.; Lockhart, K.; Jones, D.; O’Hara, L.M.; Nophale, L.; Bryce, E.A.; Darwin, L. Protecting health workers from infectious disease transmission: An exploration of a Canadian-South African partnership of partnerships. Glob. Health 2016, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- The World Bank World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 8 October 2019).
- The World Bank World Bank Open Data. Available online: https://data.worldbank.org/ (accessed on 14 June 2019).
- Kanabus, A. Information about Tuberculosis. Available online: https://tbfacts.org/high-burden-tb/ (accessed on 3 May 2020).
- Yassi, A.; Mabhele, S.; Wilcox, E.S.; Tsang, V.W.L.; Lockhart, K. An embodied exercise to address HIV- and tuberculosisrelated stigma of healthcare workers in Southern Africa. J. Appl. Arts Health 2019, 10, 73–85. [Google Scholar] [CrossRef]
- Yin, R.K. Case Study Research and Applications: Design and Methods, 6th ed.; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2018; ISBN 978-1-5063-3616-9. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Harvey, G.; Kitson, A. PARIHS revisited: From heuristic to integrated framework for the successful implementation of knowledge into practice. Implement. Sci. 2016, 11, 33. [Google Scholar] [CrossRef]
- Kitson, A.; Harvey, G.; McCormack, B. Enabling the implementation of evidence based practice: A conceptual framework. Qual. Health Care QHC 1998, 7, 149–158. [Google Scholar] [CrossRef]
- Moullin, J.C.; Sabater-Hernández, D.; Fernandez-Llimos, F.; Benrimoj, S.I. A systematic review of implementation frameworks of innovations in healthcare and resulting generic implementation framework. Health Res. Policy Syst. 2015, 13, 16. [Google Scholar] [CrossRef]
- Rycroft-Malone, J.; Bucknall, T. Models and Frameworks for Implementing Evidence-Based Practice: Linking Evidence to Action; John Wiley & Sons: Chichester, West Sussex, 2010; ISBN 978-1-4051-7594-4. [Google Scholar]
- Bergström, A.; Dinh, H.; Duong, D.; Pervin, J.; Rahman, A.; Skeen, S.; Tomlinson, M.; Waiswa, P.; Zelaya, E.; Wallin, L. The Context Assessment for Community Health tool-investigating why what works where in low- and middle-income settings. BMC Health Serv. Res. 2014, 14, P8. [Google Scholar] [CrossRef][Green Version]
- Halligan, M.; Zecevic, A. Safety culture in healthcare: A review of concepts, dimensions, measures and progress. BMJ Qual. Saf. 2011, 20, 338–343. [Google Scholar] [CrossRef]
- Morello, R.T.; Lowthian, J.A.; Barker, A.L.; McGinnes, R.; Dunt, D.; Brand, C. Strategies for improving patient safety culture in hospitals: A systematic review. BMJ Qual. Saf. 2013, 22, 11–18. [Google Scholar] [CrossRef]
- Yassi, A.; Bryce, E.A.; Breilh, J.; Lavoie, M.-C.; Ndelu, L.; Lockhart, K.; Spiegel, J. Collaboration between infection control and occupational health in three continents: A success story with international impact. BMC Int. Health Hum. Rights 2011, 11, S8. [Google Scholar] [CrossRef] [PubMed]
- Cadena, J.; Prigmore, T.; Bowling, J.; Ayala, B.A.; Kirkman, L.; Parekh, A.; Scepanski, T.; Patterson, J.E. Improving Influenza Vaccination of Healthcare Workers by Means of Quality Improvement Tools. Infect. Control Hosp. Epidemiol. 2011, 32, 616–618. [Google Scholar] [CrossRef] [PubMed]
- Center for Global Health, Old Dominion University. Center for Global Health Newsletter. 4. 2016. Available online: https://digitalcommons.odu.edu/globalhealth_newsletter/4 (accessed on 26 May 2020).
- International Commission on Occupational Health Newsletter, Volume 16, Number 3, 2018. Available online: http://www.icohweb.org/site/multimedia/newsletter/pdf/icoh_newsletter_vol16_no3.pdf (accessed on 26 May 2020).
- Puchalski Ritchie, L.M.; Khan, S.; Moore, J.E.; Timmings, C.; van Lettow, M.; Vogel, J.P.; Khan, D.N.; Mbaruku, G.; Mrisho, M.; Mugerwa, K.; et al. Low- and middle-income countries face many common barriers to implementation of maternal health evidence products. J. Clin. Epidemiol. 2016, 76, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Somech, A.; Drach-Zahavy, A. Translating Team Creativity to Innovation Implementation: The Role of Team Composition and Climate for Innovation. J. Manag. 2013, 39, 684–708. [Google Scholar] [CrossRef]
- Valente, T.W.; Pumpuang, P. Identifying Opinion Leaders to Promote Behavior Change. Health Educ. Behav. 2007, 34, 881–896. [Google Scholar] [CrossRef] [PubMed]
- Borbas, C.; Morris, N.; McLaughlin, B.; Asinger, R.; Gobel, F. The Role of Clinical Opinion Leaders in Guideline Implementation and Quality Improvement. Chest 2000, 118, 24S–32S. [Google Scholar] [CrossRef]
- Shoveller, J.; Viehbeck, S.; Ruggiero, E.D.; Greyson, D.; Thomson, K.; Knight, R. A critical examination of representations of context within research on population health interventions. Crit. Public Health 2016, 26, 487–500. [Google Scholar] [CrossRef]
- Birken, S.A.; Lee, S.-Y.D.; Weiner, B.J. Uncovering middle managers’ role in healthcare innovation implementation. Implement. Sci. 2012, 7, 28. [Google Scholar] [CrossRef] [PubMed]
- Engle, R.L.; Lopez, E.R.; Gormley, K.E.; Chan, J.A.; Charns, M.P.; Lukas, C.V. What roles do middle managers play in implementation of innovative practices? Health Care Manag. Rev. 2017, 42, 14–27. [Google Scholar] [CrossRef]
- Bergström, A.; Peterson, S.; Namusoko, S.; Waiswa, P.; Wallin, L. Knowledge translation in Uganda: A qualitative study of Ugandan midwives’ and managers’ perceived relevance of the sub-elements of the context cornerstone in the PARIHS framework. Implement. Sci. 2012, 7, 117. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Dou, L.; Zhang, H.; Sun, Y.; Yuan, B. Analysis of context factors in compulsory and incentive strategies for improving attraction and retention of health workers in rural and remote areas: A systematic review. Hum. Resour. Health 2015, 13, 61. [Google Scholar] [CrossRef] [PubMed]
- Harvey, G.; Loftus-Hills, A.; Rycroft-Malone, J.; Titchen, A.; Kitson, A.; McCormack, B.; Seers, K. Getting evidence into practice: The role and function of facilitation. J. Adv. Nurs. 2002, 37, 577–588. [Google Scholar] [CrossRef] [PubMed]
- Ellis, I.; Howard, P.; Larson, A.; Robertson, J. From Workshop to Work Practice: An Exploration of Context and Facilitation in the Development of Evidence-Based Practice. Worldviews Evid. Based Nurs. 2005, 2, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Landau, L.B. Communities of Knowledge or Tyrannies of Partnership: Reflections on North–South Research Networks and the Dual Imperative. J. Refug. Stud. 2012, 25, 555–570. [Google Scholar] [CrossRef]


| Hospital Characteristics | A | B | C | D | E | F | G |
|---|---|---|---|---|---|---|---|
| Country | MZ | MZ | MZ | SA | SA | ZI | ZI |
| Number of patient beds | 260 | 272 | 36 | 1652 | 720 | 1179 | 160 |
| Number of workers | 257 | 656 | 139 | 4407 | 1930 | 2843 | 213 |
| • Male | 84 | 205 | 32 | 1146 | 457 | 567 | 78 |
| • Female | 173 | 451 | 107 | 3261 | 1473 | 2276 | 135 |
| Characteristics | A/C | B | D | E | F | G |
|---|---|---|---|---|---|---|
| Clarity | EF | - | - | EF | EF | EF |
| • Lack of clarity | B | B | - | B | - | - |
| Relative advantage | EF | - | EF | - | - | - |
| Observable results | EF | - | - | EF | - | EF |
| Characteristics | A/C | B | D | E | F | G |
|---|---|---|---|---|---|---|
| Motivation | EF | - | - | - | EF/B | B |
| Goals and expectations | B | B | EF | EF | - | EF |
| Skills and knowledge | B | EF | - | - | - | - |
| Project funding | EF/B | - | B | B | EF/B | B |
| Human resources | - | B | B | B | B | EF/B |
| Material resources | B | EF/B | EF | EF | EF | B |
| Personal protective equipment (PPE) | B | B | - | EF | - | EF |
| Local opinion leaders | - | - | EF | EF | B | EF |
| Collaboration and teamwork | EF/B | EF | - | - | - | - |
| Existing networks | EF | EF | B | EF | - | EF |
| Power and authority | EF | - | - | B | - | EF |
| Characteristics | A/C | B | D | E | F | G |
|---|---|---|---|---|---|---|
| Local and organizational | ||||||
| Senior leadership and management support | EF | EF | EF/B | EF/B | EF/B | EF |
| • Senior leadership | EF | EF | EF | EF | EF | EF |
| • Middle management | - | - | B | B | B | - |
| Culture | B | EF/B | EF/B | B | EF | EF/B |
| • Commitment to work | - | EF | EF | - | EF | EF |
| • Knowledge application | - | B | B | B | - | EF |
| • Worker attitudes/ Resistance to change | B | B | B | B | - | B |
| Organizational priorities | EF | - | B | - | B | B |
| Structure and systems | B | B | B | B | B | B |
| History of innovation and change | B | B | - | B | - | B |
| Evaluation and feedback processes | EF | B | B | B | - | - |
| External health system | ||||||
| Regulatory frameworks | - | - | EF | EF | - | - |
| Environmental (in)stability | - | - | - | - | B | - |
| Inter-organizational networks/relationships | - | - | EF | EF/B | - | - |
| Characteristics | A/C | B | D | E | F | G |
|---|---|---|---|---|---|---|
| HealthWISE trainings | EF/B | B | EF | - | - | EF |
| Communication with research team | EF | - | EF | EF | EF | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilcox, E.S.; Chimedza, I.T.; Mabhele, S.; Romao, P.; Spiegel, J.M.; Zungu, M.; Yassi, A. Empowering Health Workers to Protect their Own Health: A Study of Enabling Factors and Barriers to Implementing HealthWISE in Mozambique, South Africa, and Zimbabwe. Int. J. Environ. Res. Public Health 2020, 17, 4519. https://doi.org/10.3390/ijerph17124519
Wilcox ES, Chimedza IT, Mabhele S, Romao P, Spiegel JM, Zungu M, Yassi A. Empowering Health Workers to Protect their Own Health: A Study of Enabling Factors and Barriers to Implementing HealthWISE in Mozambique, South Africa, and Zimbabwe. International Journal of Environmental Research and Public Health. 2020; 17(12):4519. https://doi.org/10.3390/ijerph17124519
Chicago/Turabian StyleWilcox, Elizabeth S., Ida Tsitsi Chimedza, Simphiwe Mabhele, Paulo Romao, Jerry M. Spiegel, Muzimkhulu Zungu, and Annalee Yassi. 2020. "Empowering Health Workers to Protect their Own Health: A Study of Enabling Factors and Barriers to Implementing HealthWISE in Mozambique, South Africa, and Zimbabwe" International Journal of Environmental Research and Public Health 17, no. 12: 4519. https://doi.org/10.3390/ijerph17124519
APA StyleWilcox, E. S., Chimedza, I. T., Mabhele, S., Romao, P., Spiegel, J. M., Zungu, M., & Yassi, A. (2020). Empowering Health Workers to Protect their Own Health: A Study of Enabling Factors and Barriers to Implementing HealthWISE in Mozambique, South Africa, and Zimbabwe. International Journal of Environmental Research and Public Health, 17(12), 4519. https://doi.org/10.3390/ijerph17124519





