Complications of Fixed Full-Arch Implant-Supported Metal-Ceramic Prostheses
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection of Patients and Implants
2.2. Prosthetic Protocol and Follow-Up Examinations
2.3. Assessment Criteria
2.4. Statistical Analysis
3. Results
3.1. Distribution of Patients, Implants and Prostheses
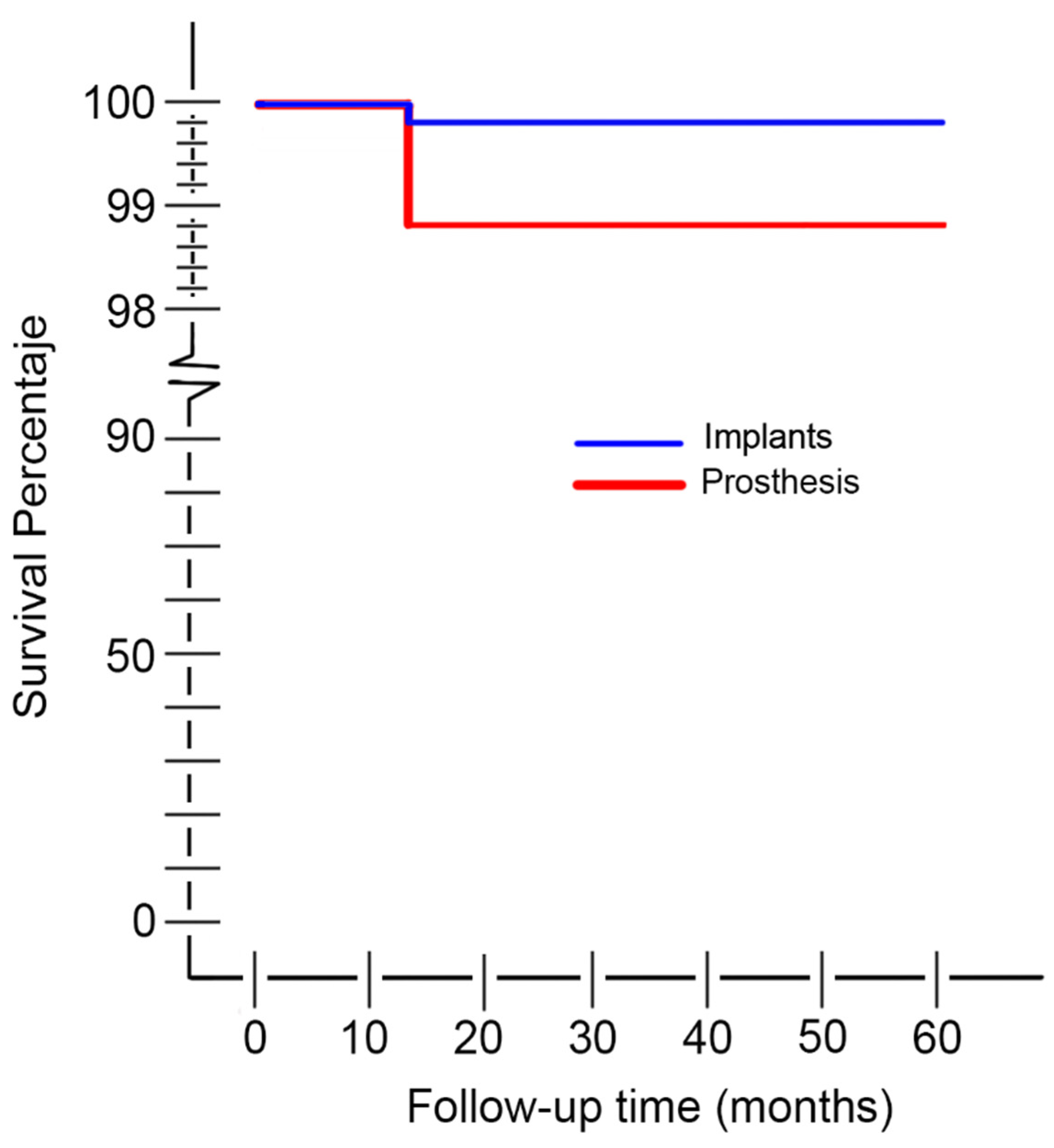
3.2. Cumulative Survival Rate of the Implants
3.3. Biological Complications
3.4. Mechanical-Technical or Prosthetic Complications
3.5. Survival of Restorations and Repair Time
4. Discussion
4.1. Implant and Restoration Survival Rates
4.2. Biological Complications
4.3. Mechanical-Technical Complications
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fueki, K.; Kimoto, K.; Ogawa, T.; Garrett, N.R. Effect of implant-supported or retained dentures on masticatory performance: A systematic review. J. Prosthet. Dent. 2007, 98, 470–477. [Google Scholar] [CrossRef]
- Pjetursson, B.E. Implant supported dentures and masticatory performance. Evid. Based Dent. 2008, 9, 22. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Turkyilmaz, I.; Company, A.M.; McGlumphy, E.A. Should edentulous patients be constrained to removable complete dentures? The use of dental implants to improve the quality of life for edentulous patients. Gerodontology 2010, 27, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Brennan, M.; Houston, F.; O’Sullivan, M.; O’Connell, B. Patient satisfaction and oral health-related quality of life outcomes of implant overdentures and fixed complete dentures. Int. J. Oral Maxillofac. Implant. 2010, 25, 791–800. [Google Scholar]
- Babbush, C.A. Posttreatment quantification of patient experiences with full-arch implant treatment using a modification of the OHIP-14 questionnaire. J. Oral. Implantol. 2012, 38, 251–260. [Google Scholar] [CrossRef]
- Testori, T.; Galli, F.; Fumagalli, L.; Capelli, M.; Zuffetti, F.; Deflorian, M.; Parenti, A.; Del Fabbro, M. Assessment of long-term survival of immediately loaded tilted Implants supporting a maxillary full-arch fixed prosthesis. Int. J. Oral Maxillofac. Implant. 2017, 32, 904–911. [Google Scholar] [CrossRef]
- Ortorp, A.; Jemt, T. Early laser-welded titanium frameworks supported by implants in the edentulous mandible: A 15-year comparative follow-up study. Clin. Implant Dent. Relat. Res. 2009, 11, 311–322. [Google Scholar] [CrossRef]
- Priest, G.; Smith, J.; Wilson, M.G. Implant survival and prosthetic complications of mandibular metal-acrylic resin implant complete fixed dental prostheses. J. Prosthe. Dent. 2014, 111, 466–475. [Google Scholar] [CrossRef]
- Heydecke, G.; Zwahlen, M.; Nicol, A.; Nisand, D.; Payer, M.; Renouard, F.; Grohmann, P.; Mühlemann, S.; Joda, T. What is the optimal number of implants for fixed reconstructions: A systematic review. Clin. Oral Implant. Res. 2012, 23, 217–228. [Google Scholar] [CrossRef]
- Mertens, C.; Steveling, H.G.; Stucke, K.; Pretzl, B.; Meyer-Bäumer, A. Fixed implant-retained rehabilitation of the edentulous maxilla: 11-year results of a prospective study. Clin. Implant Dent. Relat. Res. 2012, 14, 816–827. [Google Scholar] [CrossRef]
- Gallucci, G.O.; Doughtie, C.B.; Hwang, J.W.; Fiorellini, J.P.; Weber, H.P. Five-year results of fixed implant-supported rehabilitations with distal cantilevers for the edentulous mandible. Clin. Oral Implant. Res. 2009, 20, 601–607. [Google Scholar] [CrossRef]
- Maló, P.; Araújo Nobre, M.D.; Lopes, A.; Rodrigues, R. Double full-arch versus single full-arch, four implant-supported rehabilitations: A retrospective, 5-year cohort study. J. Prosthodont. 2015, 24, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Fischer, K.; Stenberg, T. Prospective 10-year cohort study based on a randomized, controlled trial (RCT) on implant-supported full-arch maxillary prostheses. Part II: Prosthetic outcomes and maintenance. Clin. Implant Dent. Relat. Res. 2013, 15, 498–508. [Google Scholar] [CrossRef] [PubMed]
- Purcell, B.A.; McGlumphy, E.A.; Holloway, J.A.; Beck, F.M. Prosthetic complications in mandibular metal-resin implant-fixed complete dental prostheses: A 5-to 9-year analysis. Int. J. Oral. Maxillofac. Implant. 2008, 23, 847–857. [Google Scholar]
- Bozini, T.; Petridis, H.; Garefis, K.; Garefis, P. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5 years. Int. J. Oral. Maxillofac. Implant. 2011, 26, 304–318. [Google Scholar]
- Papaspyridakos, P.; Chen, C.J.; Chuang, S.K.; Weber, H.P.; Gallucci, G.O. A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. Int. J. Oral Maxillofac. Implant. 2012, 27, 102–110. [Google Scholar]
- Sbordone, C.; Toti, P.; Martuscelli, R.; Guidetti, F.; Sbordone, L.; Ramaglia, L. A 5-year implant follow-up in maxillary and mandibular horizontal osseous onlay grafts and native bone. J. Oral Implantol. 2015, 41, 570–578. [Google Scholar] [CrossRef]
- Fouad, W.; Osman, A.; Atef, M.; Hakam, M. Guided maxillary sinus floor elevation using deproteinized bovine bone versus graftless Schneiderian membrane elevation with simultaneous implant placement: Randomized clinical trial. Clin. Implant Dent. Relat. Res. 2018, 20, 424–433. [Google Scholar] [CrossRef]
- Jung, R.E.; Al-Nawas, B.; Araujo, M.; Avila-Ortiz, G.; Barter, S.; Brodala, N.; Chappuis, V.; Chen, B.; De Souza, A.; Almeida, R.F.; et al. Group 1 ITI Consensus Report: The influence of implant length and design and medications on clinical and patient-reported outcomes. Clin. Oral Implant. Res. 2018, 29, 69–77. [Google Scholar] [CrossRef]
- Mangano, F.; Macchi, A.; Caprioglio, A.; Sammons, R.L.; Piattelli, A.; Mangano, C. Survival and complication rates of fixed restorations supported by locking-taper implants: A prospective study with 1 to 10 years of follow-up. J. Prosthodont. 2014, 23, 434–444. [Google Scholar] [CrossRef]
- Bechara, S.; Lukosiunas, A.; Dolcini, G.A.; Kubilius, R. Fixed full arches supported by tapered implants with knife-edge thread design and nanostructured, calcium-incorporated surface: A short-term prospective clinical study. Biomed. Res. Int. 2017, 2017, 4170537. [Google Scholar] [CrossRef] [PubMed]
- Papaspyridakos, P.; Barizan-Bordin, T.; Kim, Y.J.; DeFuria, C.; Pagni, S.E.; Choclidakis, K.; Rolim-Teixeria, E.; Weber, H.P. Implant survival rates and biologic complications with implant-supported fixed complete dental prostheses: A retrospective study with up to 12-year follow-up. Clin. Oral Implant. Res. 2018, 29, 881–893. [Google Scholar] [CrossRef] [PubMed]
- Van Steenberghe, D. Outcomes and their measurement in clinical trials of endosseous oral implants. Ann. Periodontol. 1997, 2, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Lindhe, J.; Meyle, J.; Berglunh, T. Peri-implant diseases: Consensus report of the sixth european workshop on periodontology. J. Clin. Periodontol. 2008, 35, 282–285. [Google Scholar] [CrossRef] [PubMed]
- Heitz-Mayfield, L.J.; Aaboe, M.; Araujo, M.; Carrión, J.B.; Cavalcanti, R.; Cionca, N.; Cochran, D.; Darby, I.; Funakoshi, E.; Gierthmuehlen, P.C.; et al. Group 4 ITI Consensus report: Risks and biologic complications associated with implant dentistry. Clin. Oral Implant. Res. 2018, 29, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Hirooka, H.; Polyzois, I.; Kelekis-Cholakis, A.; Wang, H.L.; Working Group 3. Diagnosis and non-surgical treatment of peri-implant diseases and maintenance care of patients with dental implants-Consensus report of working group 3. Int. Dent. J. 2019, 69, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Anusavice, K.J. Standardizing failure, success, and survival decisions in clinical studies of ceramic and metal-ceramic fixed dental prostheses. Dent. Mater. 2012, 28, 102–111. [Google Scholar] [CrossRef]
- De Boever, A.L.; Keersmaekers, K.; Vanmaele, G.; Kerschbaum, T.; Theuniers, G.; De Boever, J.A. Prosthetic complications in fixed endosseous implant-borne reconstructions after an observations period of at least 40 months. J. Oral Rehabil. 2006, 33, 833–839. [Google Scholar] [CrossRef]
- Gallucci, G.O.; Bernard, J.P.; Belser, U.C. Treatment of completely edentulous patients with fixed implant-supported restorations: Three consecutive cases of simultaneous immediate loading in both maxilla and mandible. Int. J. Periodontics Restor. Dent. 2005, 25, 27–37. [Google Scholar]
- Lambert, F.E.; Weber, H.P.; Susarla, S.M.; Belser, U.C.; Gallucci, G.O. Descriptive analysis of implant and prosthodontic survival rates with fixed implant-supported rehabilitations in the edentulous maxilla. J. Periodontol. 2009, 80, 1220–1230. [Google Scholar] [CrossRef]
- Zhang, X.X.; Shi, J.Y.; Gu, Y.X.; Lai, H.C. Long-term outcomes of early loading of straumann implant-supported fixed segmented bridgeworks in edentulous maxillae: A 10-year prospective study. Clin. Implant Dent. Relat. Res. 2016, 18, 1227–1237. [Google Scholar] [CrossRef] [PubMed]
- Ravald, N.; Dahlgren, S.; Teiwik, A.; Gröndahl, K. Long-term evaluation of Astra Tech and Brånemark implants in patients treated with full-arch bridges. Results after 12–15 years. Clin. Oral Implant. Res. 2013, 24, 1144–1151. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Francischone, C.; Rigolizzo, M. “All-on-4” immediate-function concept for completely edentulous maxillae: A clinical report on the medium (3 years) and long-term (5 years) outcomes. Clin. Implant Dent. Relat. Res. 2012, 14, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Drago, C. Ratios of cantilever lengths and anterior-posterior spreads of definitive hibrid full-arch, screw-retained prostheses: Results of a clinical study. J. Prosthodont. 2018, 27, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. A retrospective study on clinical and radiological outcomes of oral implants in patients followed up for a minimum of 20 years. Clin. Implant Dent. Relat. Res. 2018, 20, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Jemt, T. Implant survival in the edentulous jaw: 30 years of experience. part II: A retro-prospective multivariate regression analysis related to treated arch and implant surface roughness. Int. J. Prosthodont. 2018, 31, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Derks, J.; Tomasi, C. Peri-implant health and disease. A systematic review of current epidemiology. J. Clin. Periodontol. 2015, 42, S158–S171. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Chapple, I.L.C.; Jepsen, S.; Sanz, M. Primary and secondary prevention of periodontal and peri-implant diseases-Introduction to, and objectives of the 11th European workshop on periodontology consensus conference. J. Clin. Periodontol. 2015, 42, S1–S4. [Google Scholar] [CrossRef]
- Francetti, L.; Cavalli, N.; Taschieri, S.; Corbella, S. Ten years follow-up retrospective study on implant survival rates and prevalence of peri-implantitis in implant-supported full-arch rehabilitations. Clin. Oral Implant. Res. 2019, 30, 252–260. [Google Scholar] [CrossRef]
- Cavalli, N.; Corbella, S.; Taschieri, S.; Francetti, L. Prevalence of peri-implant mucositis and peri-implantitis in patients treated with a combination of axial and tilted implants supporting a complete fixed denture. Sci. World J. 2015, 2015, 874842. [Google Scholar] [CrossRef]
- John, G.; Becker, J.; Schwarz, F. Modified implant surface with slower and less initial biofilm formation. Clin. Implant Dent. Rel. Res. 2015, 17, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Galindo-Moreno, P.; León-Cano, A.; Ortega-Oller, I.; Monje, A.; Suárez, F.; ÓValle, F.; Spinato, S.; Catena, A. Prosthetic abutment height is a key factor in peri-implant marginal bone loss. J. Dent. Res. 2014, 93, S80–S85. [Google Scholar] [CrossRef] [PubMed]
- Sasada, Y.; Cochran, D.L. Implant-abutment connections: A review of biologic consequences and peri-implantitis implications. Int. J. Oral Maxillofac. Implant. 2017, 32, 1296–1307. [Google Scholar] [CrossRef] [PubMed]
- Mouhyi, J.; Dohan-Ehrenfest, D.M.; Albrektsson, T. The peri-implantitis: Implant surfaces, microstructure, and physicochemical aspects. Clin. Implant Dent. Relat. Res. 2012, 14, 170–183. [Google Scholar] [CrossRef]
- Jordana, F.; Susbielles, L.; Colat-Parros, J. Periimplantitis and implant body roughness: A systematic review of literature. Implant Dent. 2018, 27, 672–681. [Google Scholar] [CrossRef]
- Kotsovilis, S.; Fourmousis, I.; Karoussis, I.K.; Bamia, C. A systematic review and meta-analysis on the effect of implant length on the survival of rough-surface dental implants. J. Periodontol. 2009, 80, 1700–1718. [Google Scholar] [CrossRef]
- Pommer, B.; Frantal, S.; Willer, J.; Posch, M.; Watzek, G.; Tepper, G. Impact of dental implant length on early failure rates: A meta-analysis of observational studies. J. Clin. Periodontol. 2011, 38, 856–863. [Google Scholar] [CrossRef]
- Monje, A.; Chan, H.L.; Fu, J.H.; Suarez, F.; Galindo-Moreno, P.; Wang, H.L. Are short dental implants (< 10 mm) effective? a meta-analysis on prospective clinical trials. J. Periodontol. 2013, 84, 895–904. [Google Scholar]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Reasons for failures of oral implants. J. Oral Rehabil. 2014, 41, 443–476. [Google Scholar] [CrossRef]
- Telleman, G.; Raghoebar, G.M.; Vissink, A.; den Hartog, L.; Huddleston Slater, J.J.; Meijer, H.J. A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patient. J. Clin. Periodontol. 2011, 38, 667–676. [Google Scholar]
- Papaspyridakos, P.; De Souza, A.; Vazouras, K.; Gholami, H.; Pagni, S.; Weber, H.P. Survival rates of short dental implants (≤6 mm) compared with implants longer than 6 mm in posterior jaw areas: A meta-analysis. Clin. Oral Implant. Res. 2018, 29, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Jemt, T. Implant survival in the edentulous jaw-30 years of experience. part I: A retro-prospective multivariate regression analysis of overall implant failure in 4585 consecutively treated arches. Int. J. Prosthodont. 2018, 31, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Saffi, S.H.; Palmer, R.M.; Wilson, R.F. Risk of implant failure and marginal bone loss in subjects with a history of periodontitis: A systematic review and meta-analysis. Clin. Implant Dent. Relat. Res. 2010, 12, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Staubli, N.; Walter, C.; Schmidt, J.C.; Weiger, R.; Zitzmann, N.U. Excess cement and the risk of peri-implant disease-a systematic review. Clin. Oral Implant. Res. 2017, 28, 1278–1290. [Google Scholar] [CrossRef] [PubMed]
- Kourtis, S.; Damanaki, M.; Kaitatzidou, S.; Kaitatzidou, A.; Roussou, V. Loosening of the fixing screw in single implant crowns: Predisposing factors, prevention and treatment options. J. Esthet. Restor. Dent. 2017, 29, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Gracis, S.; Michalakis, K.; Vigolo, P.; von Steyern, V.P.; Zwahlen, M.; Sailer, I. Internal vs. external connections for abutments/reconstructions: A systematic review. Clin. Oral Implant. Res. 2012, 23, 202–216. [Google Scholar] [CrossRef] [PubMed]
- Larrucea Verdugo, C.; Jaramillo Núñez, G.; Acevedo Avila, A.; Larrucea San Martín, C. Microleakage of the prosthetic abutment/implant interface with internal and external connection: In vitro study. Clin. Oral Implant. Res. 2014, 25, 1078–1083. [Google Scholar] [CrossRef]
- Pieri, F.; Forlivesi, C.; Caselli, E.; Corinaldesi, G. Narrow-(3.0 mm) versus standard-diameter (4.0 and 4.5 mm) implants for splinted partial fixed restoration of posterior mandibular and maxillary jaws: A 5-year retrospective cohort study. J. Periodontol. 2017, 88, 338–347. [Google Scholar] [CrossRef]
- Sailer, I.; Mühlemann, S.; Zwahlen, M.; Hämmerle, C.H.; Schneider, D. Cemented and screw-retained implant reconstructions: A systematic review of the survival and complication rates. Clin. Oral Implant. Res. 2012, 23, 163–201. [Google Scholar] [CrossRef]
- Nissan, J.; Narobai, D.; Gross, O.; Ghelfan, O.; Chaushu, G. Long-term outcome of cemented versus screw-retained implant-supported partial restorations. Int. J. Oral Maxillofac. Implant. 2011, 26, 1102–1107. [Google Scholar]
- Nedir, R.; Bischof, M.; Szmukler-Moncler, S.; Belser, U.C.; Samson, J. Prosthetic complications with dental implants: From an up-to-8-year experience in private practice. Int. J. Oral Maxillofac. Implant. 2006, 21, 919–928. [Google Scholar]
- Milen, C.; Brägger, U.; Wittneben, J.G. Influence of prosthesis type and retention mechanism on complications with fixed implant-supported prostheses: A systematic review applying multivariate analyses. Int. J. Oral Maxillofac. Implant. 2015, 30, 110–124. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Thoma, D.; Jung, R.; Zwahlen, M.; Zembic, A. systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin. Oral Implant. Res. 2012, 23, 22–38. [Google Scholar] [CrossRef] [PubMed]
- Zembic, A.; Kim, S.; Zwahlen, M.; Kelly, J.R. Systematic review of the survival rate and incidence of biologic, technical, and esthetic complications of single implant abutments supporting fixed prostheses. Int. J. Oral Maxillofac. Implant. 2014, 29, 99–116. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Philipp, A.; Zembic, A.; Pjetrusson, B.E.; Hämmerle, C.H.; Zahlen, M. A systematic review of the performance of ceramic and metal implant abutments supporting fixed implant reconstructions. Clin. Oral Implant. Res. 2009, 20, 4–31. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Zembic, A.; Pjetursson, B.E.; Zwahlen, M.; Thoma, D.S. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin. Oral Implant. Res. 2012, 23, 2–21. [Google Scholar] [CrossRef]
- Wittneben, J.G.; Buser, D.; Salvi, G.E.; Bürgin, W.; Hicklin, S.; Brägger, U. Complication and failure rates with implant-supported fixed dental prostheses and single crowns: A 10-year retrospective study. Clin. Implant Dent. Relat. Res. 2014, 16, 356–364. [Google Scholar] [CrossRef]
| Patients (n = 65) (42/65) | |||
|---|---|---|---|
| Variable | OR | (ORCI) | p |
| Sex | 0.91 | (0.30–2.78) | 0.875 |
| Female (30/46) * | |||
| Male (12/19) | |||
| Age Year Group | |||
| <51 (8/12) * | |||
| 51–60 (17/28)) | 0.77 | (0.19–2.19) | 0.727 |
| 61–70 (10/15) | 1.00 | (0.20–5.00) | 1.00 |
| 71–80 (7/10) | 1.16 | (0.19–7.11) | 0.367 |
| Previous Periodontitis | 1.75 | (0.36–10.55) | 0.823 |
| No (3/5) * | |||
| Yes (39/60) | |||
| Bruxism | 1.32 | (0.47–3.65) | 0.593 |
| No (19/31) * | |||
| Yes (23/34) | |||
| Smoker > 10 Cigarettes/Day | 3.07 | (0.80–11.70) | 0.100 |
| No (34/49) * | |||
| Yes (8/16) | |||
| Bone Regeneration | 2.62 | (0.76–0.85) | 0.127 |
| No (6/13) * | |||
| Yes (36/52) | |||
| Prosthesis (n = 80) (54/80) | |||
|---|---|---|---|
| Variable | OR | (ORCI) | p |
| Site | 0.62 | (0.19–1.94) | 0.411 |
| Mandible (15/20) * | |||
| 5 implants (7) | |||
| 6 implants (9) | |||
| 7 implants (1) | |||
| 8 implants (3) | |||
| Maxilla (39/60) | |||
| 6 implants (21) | |||
| 7 implants (2) | |||
| 8 implants (36) | |||
| 10 implants (1) | |||
| Sections | |||
| One (30/47) * | |||
| Two (16/21) | 1.81 | (0.56–5.82) | 0.32 |
| Three (8/12) | 1.13 | (0.29–4.38) | 0.85 |
| Without Cantilevers (40/63) | 1.92 | (0.56–6.56) | 0.275 |
| Maxilla (13/52) * | |||
| Mandible (2/11) | |||
| Retention | 0.98 | (0.38–2.54) | 0.981 |
| Cemented (23/34) * | |||
| Maxilla (29) | |||
| Mandible (5) | |||
| Screwed (31/46) | |||
| Maxilla (31) | |||
| Mandible (15) | |||
| Crown/Implant Ratio | |||
| < 1 (10/18) * | |||
| Maxilla (17) | |||
| Mandible (1) | |||
| 1 (34/49) | 1.81 | (0.59–5.50) | 0.29 |
| Maxilla (35) | |||
| Mandible (14) | |||
| > 1 (10/13) | 2.66 | (0.54–13.98) | 0.22 |
| Maxilla (8) | |||
| Mandible (5) | |||
| Opposing Dentition | 1.11 | (0.74–1.66) | 0.626 |
| Natural Teeth (27/30) * | |||
| Acrylic/Resin (1/2) | |||
| Metal-Porcelain and Teeth (9/18) | |||
| Metal-Porcelain (17/30) | |||
| Implants (n = 558) (54/558) | |||
|---|---|---|---|
| Variable | OR | (ORCI) | p |
| Site | 0.57 | (0.36–0.91) | 0.019 |
| Mandible (15/120) * | |||
| Maxilla (39/438) | |||
| Implant area | |||
| Incisal (32/150) | |||
| Maxilla (119) | |||
| Mandible (31) | |||
| Canine (5/101) | 0.98 | (0.58–1.68) | 0.957 |
| Maxilla (77) | |||
| Mandible (24) | |||
| Premolar (8/167) | 1.07 | (0.64–1.62) | 0.94 |
| Maxilla (126) | |||
| Mandible (41) | |||
| Molar (9/140) | 1.02 | (0.63–1.66) | 0.93 |
| Maxilla (116) | |||
| Mandible (24) | |||
| Implant Diameter | |||
| Narrow (< 4 mm) (19/82) * | |||
| Standard (4–4.1 mm) (25/422) | 0.84 | (0.50–1.41) | 0.516 |
| Width (> 4.1 mm) (10/54) | 0.60 | (0.29–1.23) | 0.168 |
| Length | 0.45 | (0.20–0.99) | 0.048 |
| < 10 mm (20/42) * | |||
| > 10 mm (34/516) | |||
| Connection | 0.92 | (0.32–2.22) | 0.86 |
| Internal (49/543) * | |||
| External (5/15) | |||
| Implant Brand | 1.76 | (1.14–2.72) | 0.011 |
| Straumann SLA Tissue Level (47/410) * | |||
| Others (7/148) | |||
| Astra Osseospeed (133) | |||
| Biomet 3i Osseotite (15) | |||
| Patients (n = 65) (10/65) | |||
|---|---|---|---|
| Variable | OR | (ORCI) | p |
| Sex | 0.22 | (0.026–1.94) | 0.177 |
| Female (9/46) * | |||
| Male (1/19) | |||
| Age Year Group | |||
| < 51 (2/12) * | |||
| 51–60 (5/28) | 1.08 | (0.18–6.58) | 0.93 |
| 61–70 (2/15) | 0.77 | (0.092–6.44) | 0.809 |
| 71–80 (1/10) | 0.55 | (0.042–7.21) | 0.653 |
| Previous Periodontitis | 0.9 | (0.09–8.63) | 0.93 |
| No (0/5) * | |||
| Yes (10/60) | |||
| Bruxism | 1.44 | (0.36–5.69) | 0.568 |
| No (4/31) * | |||
| Yes (6/34) | |||
| Smoker > 10 Cigarettes/Day | 0.70 | (0.134–5.451) | 0.674 |
| No (9/49) * | |||
| Yes (1/16) | |||
| Bone Regeneration | 0.51 | (0.11–2.36) | 0.396 |
| No (3/13) * | |||
| Yes (7/52) | |||
| Prosthesis (n = 80) (11/80) | |||
|---|---|---|---|
| Variable | OR | (ORCI) | p |
| Site | 3.80 | (0.45–31.73) | 0.218 |
| Mandible (1/20) * | |||
| 5 implants (7) | |||
| 6 implants (9) | |||
| 7 implants (1) | |||
| 8 implants (3) | |||
| Maxilla (10/60) | |||
| 6 implants (21) | |||
| 7 implants (2) | |||
| 8 implants (36) | |||
| 10 implants (1) | |||
| Sections | |||
| One (6/47) * | |||
| Two (4/21) | 1.60 | (0.40–6.42) | 0.50 |
| Three (1/12) | 0.44 | (0.10–1.79) | 0.254 |
| Without cantilevers | 0.30 | (0.03–2.56) | 0.275 |
| Maxilla (0/52) * | |||
| Mandible (0/11) | |||
| Retention | 0.36 | (0.09–1.37) | 0.137 |
| Cemented (7/34) * | |||
| Maxilla (29) | |||
| Mandible (5) | |||
| Screwed (4/46) | |||
| Maxilla (31) | |||
| Mandible (15) | |||
| Crown/Implant Ratio | |||
| < 1 (2/18) * | |||
| Maxilla (17) | |||
| Mandible (1) | |||
| 1 (7/49) | 1.33 | (0.25–7.10) | 0.73 |
| Maxilla (35) | |||
| Mandible (14) | |||
| > 1 (2/13) | 1.45 | (0.17–11.93) | 0.72 |
| Maxilla (8) | |||
| Mandible (5) | |||
| Opposing Dentition | 0.94 | (0.551–1.617) | 0.834 |
| Natural Teeth (9/30) * | |||
| Acrylic/Resin (1/2) | |||
| Metal-Porcelain and Teeth (0/18) | |||
| Metal-Porcelain (1/30) | |||
| Implants (n = 558) (11/558) | |||
|---|---|---|---|
| Variable | OR | (ORCI) | p |
| Site | 2.78 | (0.35–21.93) | 0.332 |
| Mandible (1/120) * | |||
| Maxilla (10/438) | |||
| Implant area | |||
| Incisal (11/150) | |||
| Maxilla (10/119) | |||
| Mandible (1/31) | |||
| Canine (0/101) | 0.24 | (0.28–2.03) | 0.191 |
| Maxilla (77) | |||
| Mandible (24) | |||
| Premolar (0/167) | 0.44 | (0.10–1.79) | 0.254 |
| Maxilla (126) | |||
| Mandible (41) | |||
| Molar (0/140) | 0.16 | (0.01–1.40) | 0.099 |
| Maxilla (116) | |||
| Mandible (24) | |||
| Implant Diameter | |||
| Narrow (< 4 mm) (5/82) * | |||
| Standard (4–4.1 mm) (6/422) | 0.77 | (0.16–3.70) | 0.747 |
| Width (> 4.1 mm) (0/54) | 0.75 | (0.60–8.53) | 0.820 |
| Length | 0.13 | (0.36–0.46) | 0.002 |
| < 10 mm (4/42) * | |||
| > 10 mm (7/516) | |||
| Connection | 2.38 | (0.29–19.47) | 0.417 |
| Internal (11/543) * | |||
| External (0/15) | |||
| Implant Brand | 0.65 | (0.14–3.08) | 0.59 |
| Straumann SLA Tissue Level (8/410) * | |||
| Others (3/148) | |||
| Astra Osseospeed (133) | |||
| Biomet 3i Osseotite (15) | |||
| Patients (n = 65) (29/65) | |||
|---|---|---|---|
| Variable | OR | (ORCI) | p |
| Sex | 0.86 | (0.29–2.54) | 0.794 |
| Female (21/46) * | |||
| Male (8/19) | |||
| Age Year Group | |||
| <51 (5/12) * | |||
| 51–60 (12/28) | 1.05 | (0.26–4.13) | 0.944 |
| 61–70 (8/15) | 1.6 | (0.34–7.40) | 0.548 |
| 71–80 (4/10) | 0.93 | (0.17–5.15) | 0.937 |
| Previous Periodontitis | 1.13 | (0.01–1.24) | 0.078 |
| No (5/5) * | |||
| Yes (24/60) | |||
| Bruxism | 0.95 | (0.36–2.55) | 0.933 |
| No (14/31) * | |||
| Yes (15/34) | |||
| Smoker > 10 Cigarettes/Day | 0.196 | (0.049–0.78) | 0.021 |
| No (26/49) * | |||
| Yes (3/16) | |||
| Bone Regeneration | 0.628 | (0.18–2.13) | 0.456 |
| No (7/13) * | |||
| Yes (22/52) | |||
| Prosthesis (n = 80) (31/80) | |||
|---|---|---|---|
| Variable | OR | (ORCI) | p |
| Site | 1.00 | (0.36–2.76) | 1.00 |
| Mandible (7/20) * | |||
| 5 implants (7) | |||
| 6 implants (9) | |||
| 7 implants (1) | |||
| 8 implants (3) | |||
| Maxilla (24/60) | |||
| 6 implants (21) | |||
| 7 implants (2) | |||
| 8 implants (36) | |||
| 10 implants (1) | |||
| Sections | |||
| One (21/47) * | |||
| Two (6/21) | 0.47 | (0.16–1.40) | 0.179 |
| Three (4/12) | 0.68 | (0.19–2.46) | 0.560 |
| Without Cantilevers | 1.50 | (0.51–4.39) | 0.460 |
| Maxilla (15/52) * | |||
| Mandible (1/11) | |||
| Retention | 5.05 | (1.88–13.59) | 0.001 |
| Cemented (7/34) * | |||
| Maxilla (29) | |||
| Mandible (5) | |||
| Screwed (24/46) | |||
| Maxilla (31) | |||
| Mandible (15) | |||
| Crown/Implant Ratio | |||
| <1 (8/18) * | |||
| Maxilla (17) | |||
| Mandible (1) | |||
| 1 (18/49) | 0.55 | (0.16–1.64) | 0.285 |
| Maxilla (35) | |||
| Mandible (14) | |||
| > 1 (5/13)) | 0.68 | (0.17–2.87) | 0.606 |
| Maxilla (8) | |||
| Mandible (5) | |||
| Opposing Dentition | 0.82 | (0.55–1.21) | 0.32 |
| Natural Teeth (30) * | |||
| Acrylic/resin (2) | |||
| Metal-Porcelain and Teeth (18) | |||
| Metal-Porcelain (30) | |||
| Implants (n = 558) (31/558) | |||
|---|---|---|---|
| Variable | OR | (ORCI) | p |
| Site | 1.04 | (0.69–1.57) | 0.828 |
| Mandible (120) * | |||
| Maxilla (438) | |||
| Implant Area | |||
| Incisal (150) | |||
| Maxilla (119) | |||
| Mandible (31) | |||
| Canine (101) | 0.99 | (0.60–1.65) | 0.986 |
| Maxilla (77) | |||
| Mandible (24) | |||
| Premolar (167) | 0.94 | (0.60–1.46) | 0.78 |
| Maxilla (126) | |||
| Mandible (41) | |||
| Molar (140) | 0.87 | (0.55–1.39) | 0.578 |
| Maxilla (116) | |||
| Mandible (24) | |||
| Implant Diameter | |||
| Narrow (< 4 mm) (5/82) * | |||
| Standard (4–4.1 mm) (24/422) | 0.98 | (0.60–1.58) | 0.937 |
| Width (> 4.1 mm) (2/54) | 0.44 | (0.20–0.97) | 0.043 |
| Length | 0.74 | (0.39–1.40) | 0.369 |
| <10 mm (3/42) * | |||
| > 10 mm (28/516) | |||
| Connection | 2.54 | (1.06–6.10) | 0.036 |
| Internal (21/543) * | |||
| External (10/15) | |||
| Implant Brand | 1.87 | (1.27–2.75) | 0.001 |
| Straumann SLA Tissue Level (6/410) * | |||
| Others (25/148) | |||
| Astra Osseospeed (133) | |||
| Biomet 3i Osseotite (15) | |||
| Year Interval of Follow–Up | No. of Implants Follow–Up | No. of Failures | Survival Rate per Year Interval (%) | Cumulative Survival Rate (%) |
|---|---|---|---|---|
| 0–1 | 558 | 0 | 100 | 100 |
| 1–2 | 558 | 1 | 99.8 | 99.8 |
| 2–3 | 557 | 0 | 100 | 99.8 |
| 3–4 | 557 | 0 | 100 | 99.8 |
| 4–5 | 557 | 0 | 100 | 99.8 |
| Year Interval of Follow–Up | No. of Prosthesis Follow–Up | No. of Failures | Survival Rate per Year Interval (%) | Cumulative Survival Rate (%) |
|---|---|---|---|---|
| 0–1 | 80 | 0 | 100 | 100 |
| 1–2 | 80 | 1 | 98.8 | 98.8 |
| 2–3 | 79 | 0 | 100 | 98.8 |
| 3–4 | 79 | 0 | 100 | 98.8 |
| 4–5 | 79 | 0 | 100 | 98.8 |
| Kind of Complication | Restoration Based | Patient Based | Screwed Prostheses N = 46 | Cemented Prostheses N = 34 | p |
|---|---|---|---|---|---|
| All Complications | 31/80 (38.75%) | 31/65 (47.69%) | 26/46 (60.86%) | 5/34 (14.71%) | 0.001 |
| Loss of the Access Plug | 13/80 (16.25%) | 13/65 (20.00%) | 13/46 (34.78%) | 0/34 0.00% | |
| Porcelain Fracture | 10/80 (12.50%) | 10/65 (15.38%) | 7/46 (15.22%) | 3/34 (8.82%) | 0.396 |
| Screw Loosening | 4/80 (5.00%) | 4/65 (6.15%) | 3/46 (6.52%) | 1/34 (2.94%) | 0.467 |
| Screw Fracture | 1/80 (1.25%) | 1/65 (1.54%) | 1/46 (2.17%) | 0/34 (0.00%) | |
| Implant Fracture | 1/80 (1.25%) | 1/65 (1.54%) | 1/46 (2.17%) | 0/34 (0.00%) | |
| Framework Fracture | 1/80 (1.25%) | 1/65 (1.54%) | 1/46 (2.17%) | 0/34 (0.00%) | |
| De-cementation | 1/80 (1.25%) | 1/65 (1.54%) | 0/46 (0.00%) | 1/34 (2.94%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonzalez-Gonzalez, I.; deLlanos-Lanchares, H.; Brizuela-Velasco, A.; Alvarez-Riesgo, J.-A.; Llorente-Pendas, S.; Herrero-Climent, M.; Alvarez-Arenal, A. Complications of Fixed Full-Arch Implant-Supported Metal-Ceramic Prostheses. Int. J. Environ. Res. Public Health 2020, 17, 4250. https://doi.org/10.3390/ijerph17124250
Gonzalez-Gonzalez I, deLlanos-Lanchares H, Brizuela-Velasco A, Alvarez-Riesgo J-A, Llorente-Pendas S, Herrero-Climent M, Alvarez-Arenal A. Complications of Fixed Full-Arch Implant-Supported Metal-Ceramic Prostheses. International Journal of Environmental Research and Public Health. 2020; 17(12):4250. https://doi.org/10.3390/ijerph17124250
Chicago/Turabian StyleGonzalez-Gonzalez, Ignacio, Hector deLlanos-Lanchares, Aritza Brizuela-Velasco, Jose-Antonio Alvarez-Riesgo, Santiago Llorente-Pendas, Mariano Herrero-Climent, and Angel Alvarez-Arenal. 2020. "Complications of Fixed Full-Arch Implant-Supported Metal-Ceramic Prostheses" International Journal of Environmental Research and Public Health 17, no. 12: 4250. https://doi.org/10.3390/ijerph17124250
APA StyleGonzalez-Gonzalez, I., deLlanos-Lanchares, H., Brizuela-Velasco, A., Alvarez-Riesgo, J.-A., Llorente-Pendas, S., Herrero-Climent, M., & Alvarez-Arenal, A. (2020). Complications of Fixed Full-Arch Implant-Supported Metal-Ceramic Prostheses. International Journal of Environmental Research and Public Health, 17(12), 4250. https://doi.org/10.3390/ijerph17124250






