Effectiveness of Family-Based Behavior Change Interventions on Obesity-Related Behavior Change in Children: A Realist Synthesis
Abstract
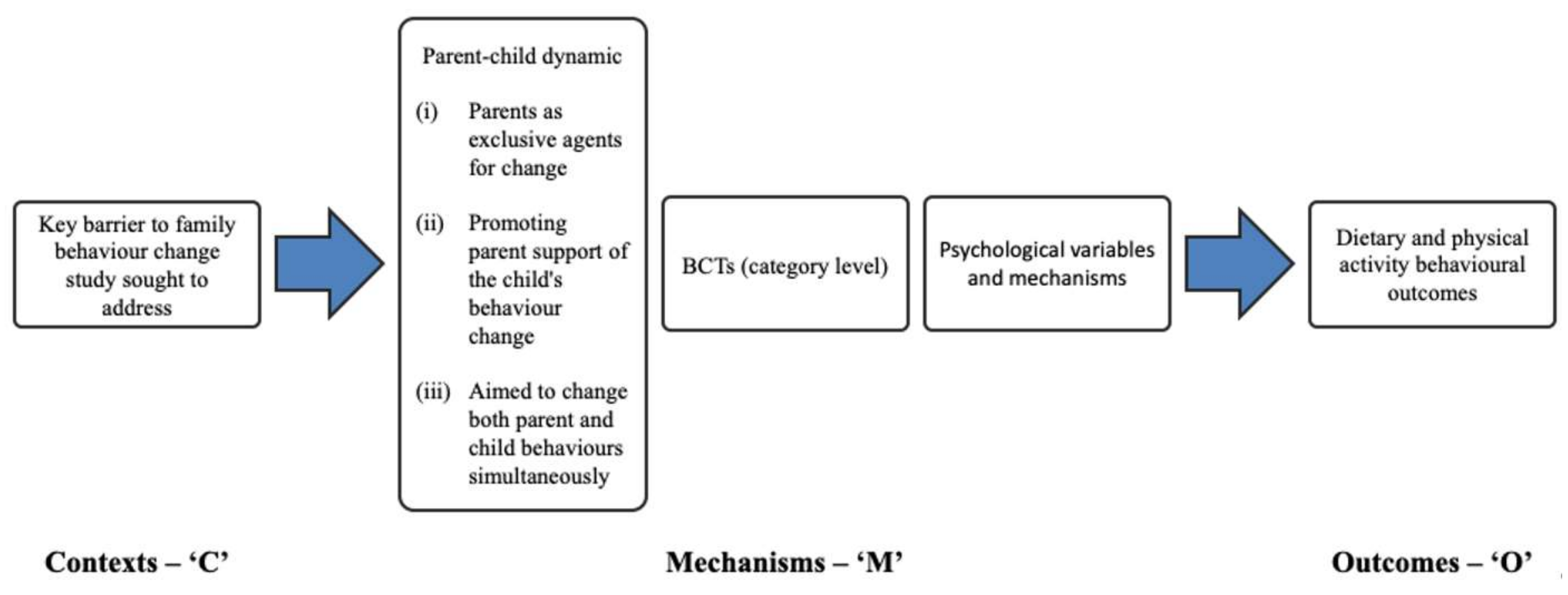
1. Introduction
- What are the diet and physical activity behavioral outcomes of family-based behavioral treatment strategies?
- What are the key mechanisms by which family-based behavioral treatment strategies result in their outcomes? Specifically, how does theoretical grounding, targeted psychological variables, and behavior change techniques relate to one another and result in diet and/physical activity behavior change?
- What influence does the type of parental involvement have on the ways different mechanisms produce behavioral outcomes?
2. Materials and Methods
2.1. Literature Search
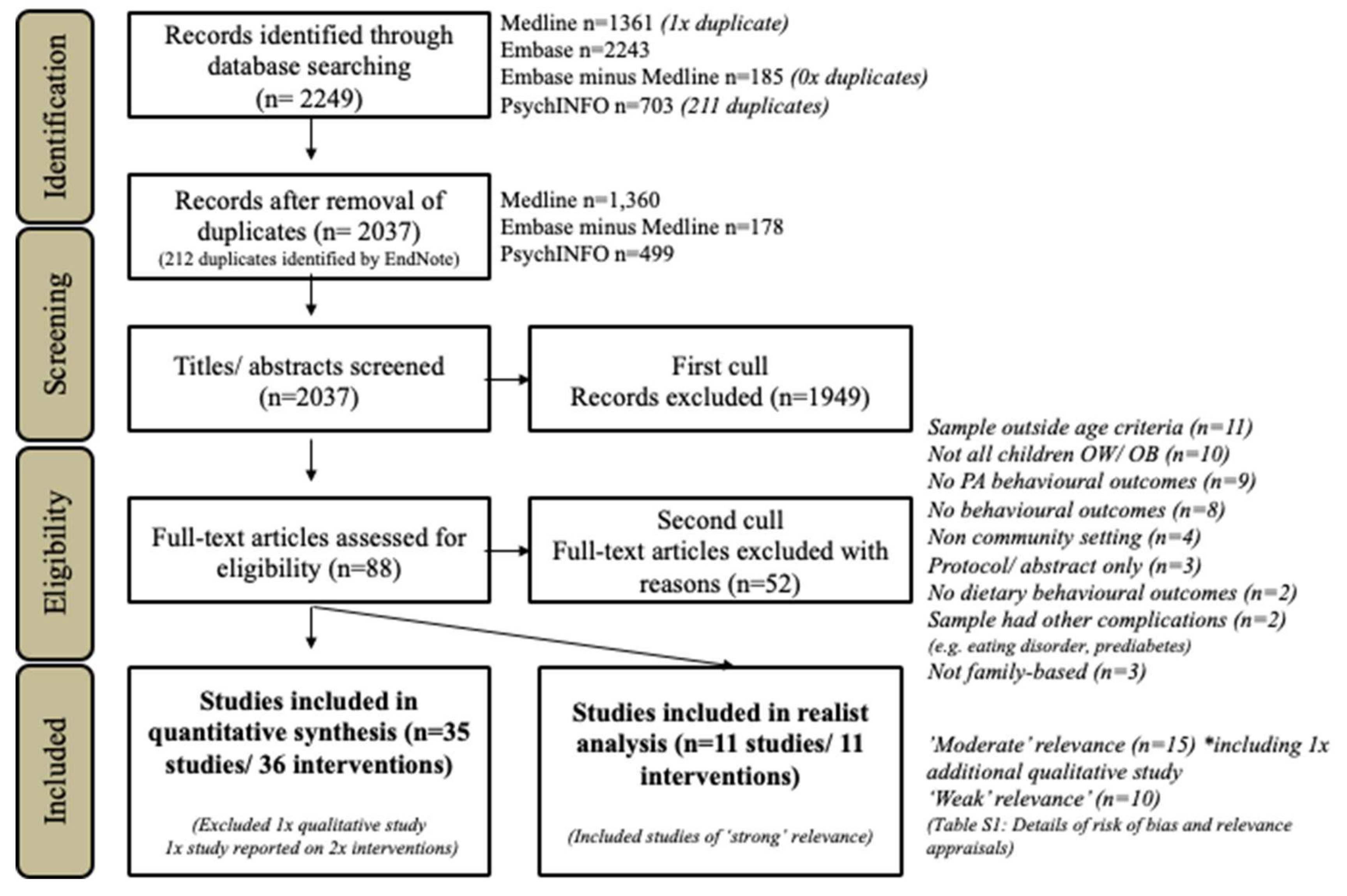
2.2. Selection of Full Texts and Further Refinement
2.3. Extracting and Organizing Data—Systematic Review
2.4. Development of a ‘Program Theory’ Framework
2.5. Extracting and Organizing Data—Realist Analysis
2.6. Refining Program Theory
2.7. Appraisal of Study Quality
3. Results
3.1. Study Selection
3.2. Risk of Bias Assessment
3.3. Study Characteristics
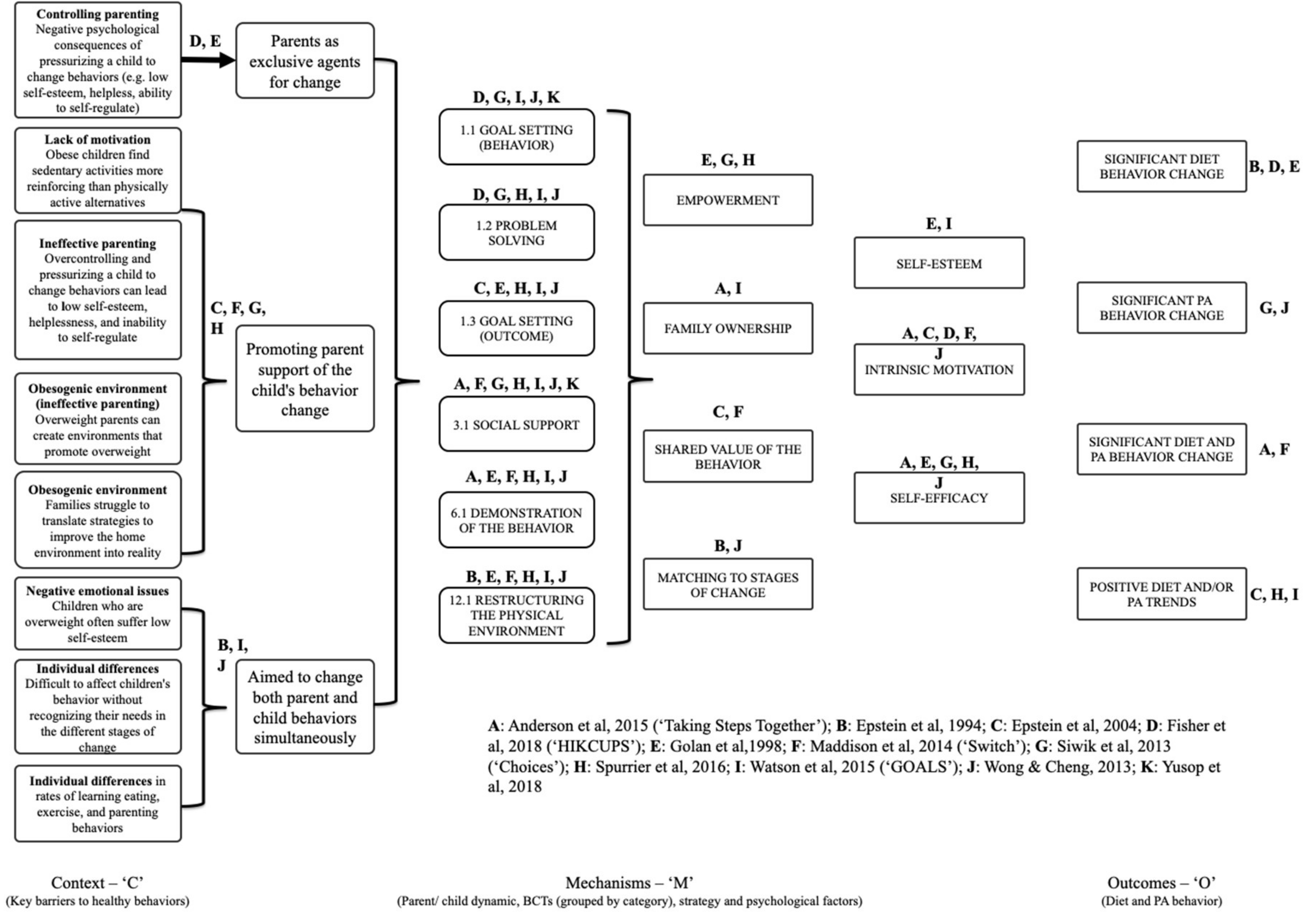
3.4. Realist Analysis
Study Quality
4. Parents as Exclusive Agents for Change
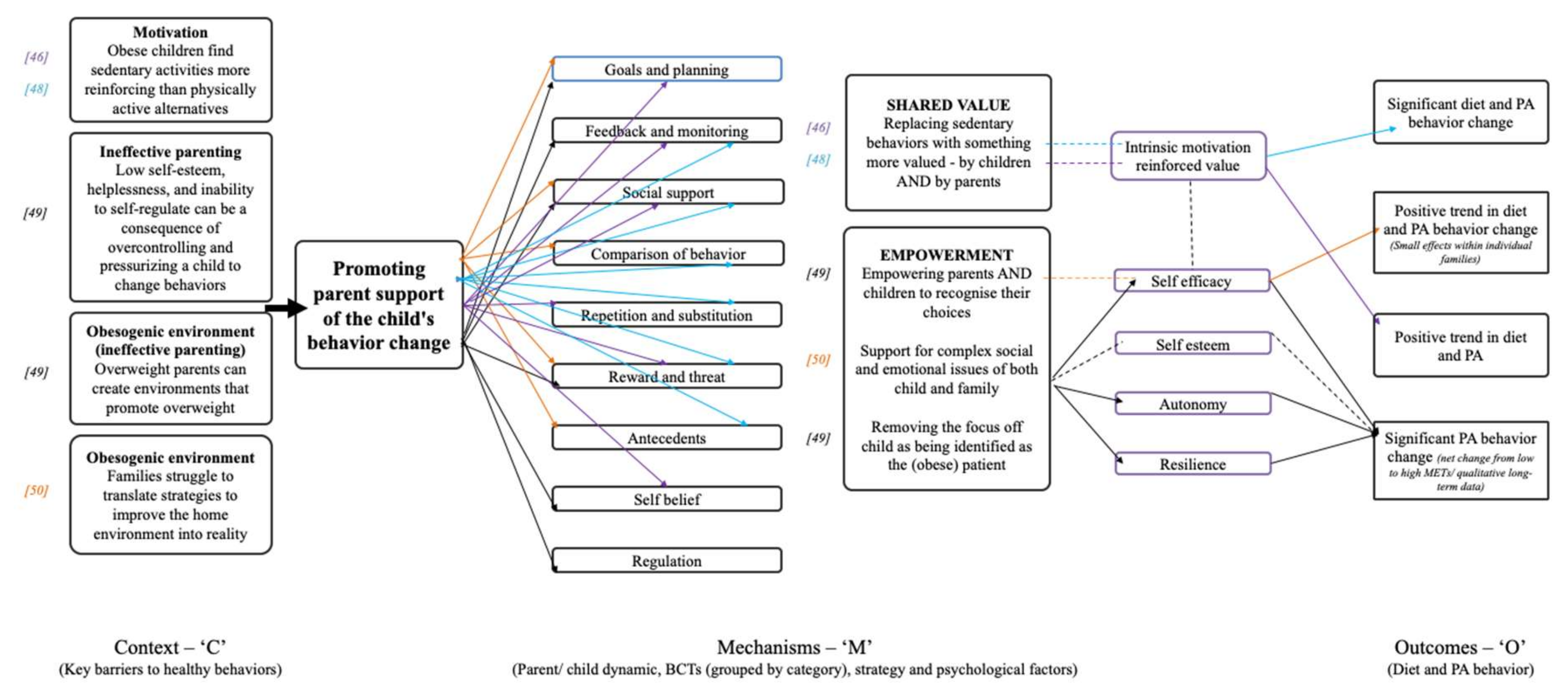
5. Promoting Parent Support of the Child’s Behavior Change
- (i)
- Shared value: Reinforcing intrinsic motivation by replacing an undesired behavior with something more valued by both children and parents.
- (ii)
- Empowerment: Empowering parents and children to recognize their choices
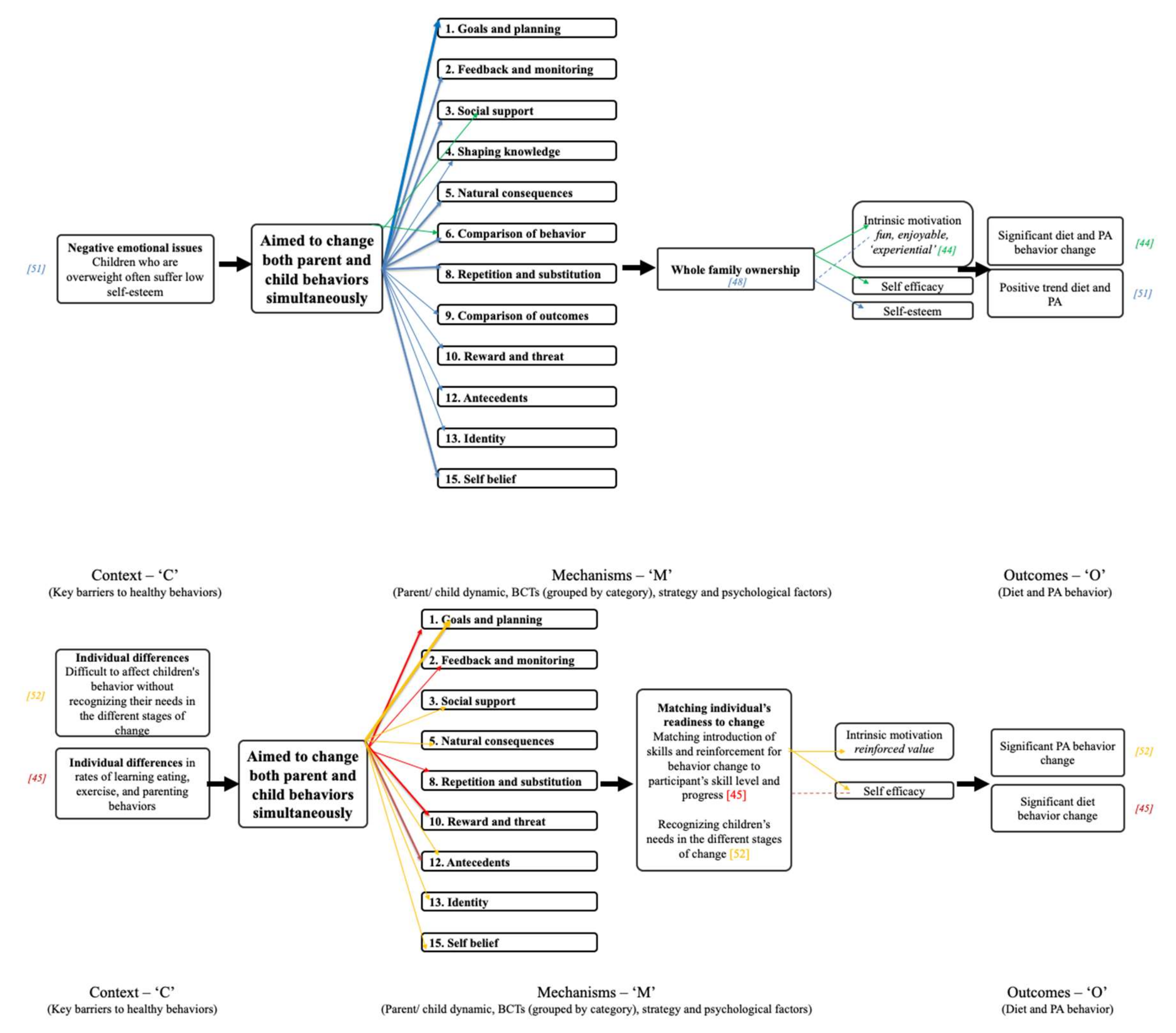
6. Aimed to Change Both Parent and Child Behaviors Simultaneously
7. Discussion
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Obesity and Overweight: Fact Sheet No 311. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/index.html (accessed on 11 August 2017).
- Singh, A.S.; Mulder, C.; Twisk, J.W.R.; Van Mechelen, W.; Chinapaw, M.J.M. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes. Rev. 2008, 9, 74–488. [Google Scholar] [CrossRef]
- Daniels, S.R. The consequences of childhood overweight and obesity. Future Child. 2006, 16, 47–67. [Google Scholar] [CrossRef] [PubMed]
- Biro, F.M.; Wien, M. Childhood obesity and adult morbidities. Am. J. Clin. Nutr. 2010, 91, 1499s–1505s. [Google Scholar] [CrossRef] [PubMed]
- Janicke, D.M.; Steele, R.G.; Gayes, L.A.; Lim, C.S.; Clifford, L.M.; Schneider, E.M.; Carmody, J.K.; Westen, S. Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. J. Pediatr. Psychol. 2014, 39, 809–825. [Google Scholar] [CrossRef] [PubMed]
- Ash, T.; Agaronov, A.; Young, T.; Aftosmes-Tobio, A.; Davison, K.K. Family-based childhood obesity prevention interventions: A systematic review and quantitative content analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 113. [Google Scholar] [CrossRef]
- De Miguel-Etayo, P.; Bueno, G.; Garagorri, J.M.; Moreno, L.A. Interventions for treating obesity in children. World Rev. Nutr. Diet. 2013, 108, 98–106. [Google Scholar] [CrossRef]
- Campbell, K.J.; Hesketh, K.D. Strategies which aim to positively impact on weight, physical activity, diet and sedentary behaviours in children from zero to five years. A systematic review of the literature. Obes. Rev. 2007, 8, 327–338. [Google Scholar] [CrossRef] [PubMed]
- Luttikhuis, H.O.; Baur, L.; Jansen, H.; Shrewsbury, V.A.; O’Malley, C.; Stolk, R.P.; Summerbell, C.D. Interventions for treating obesity in children. Cochrane Database Syst. Rev. 2009, 1, CD001872. [Google Scholar] [CrossRef]
- Van de Kolk, I.; Verjans-Janssen, S.R.B.; Gubbels, J.S.; Kremers, S.P.J.; Gerards, S.M.P.L. Systematic review of interventions in the childcare setting with direct parental involvement: Effectiveness on child weight status and energy balance-related behaviours. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 110. [Google Scholar] [CrossRef]
- Reilly, K.C.; Tucker, P.; Irwin, J.D.; Johnson, A.M.; Pearson, E.S.; Bock, D.E.; Burke, S.M. “C.H.A.M.P. Families”: Description and theoretical foundations of a paediatric overweight and obesity intervention targeting parents—A single-centre non-randomised feasibility study. Int. J. Environ. Res. Public Health 2018, 15, 2858. [Google Scholar] [CrossRef]
- Altman, M.; Wilfley, D.E. Evidence update on the treatment of overweight and obesity in children and adolescents. J. Clin. Child Adolesc. Psychol. 2015, 44, 521–537. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.H.; Wrotniak, B.H. Future directions for pediatric obesity treatment. Obesity 2010, 18 (Suppl. 1), S8–S12. [Google Scholar] [CrossRef] [PubMed]
- Schalkwijk, A.; Bot, S.; de Vries, L.; Westerman, M.J.; Nijpels, G.; Elders, P.J.M. Perspectives of obese children and their parents on lifestyle behavior change: A qualitative study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 102. [Google Scholar] [CrossRef] [PubMed]
- Golan, M.; Fainaru, M.; Weizman, A. Role of behaviour modification in the treatment of childhood obesity with the parents as the exclusive agents of change. Int. J. Obes. 1998, 22, 1217–1224. [Google Scholar] [CrossRef]
- Golley, R.K.; Magarey, A.M.; Baur, L.A.; Steinbeck, K.S.; Daniels, L.A. Twelve-month effectiveness of a parent-led, family-focused weight-management program for pre-pubertal children: A randomized, controlled trial. Pediatrics 2007, 119, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Sacher, P.M.; Kolotourou, M.; Chadwick, P.; Cole, T.J.; Lawson, M.S.; Lucas, A.; Singhal, A. Randomized controlled trial of the MEND program: A family-based community intervention for childhood obesity. Obesity 2010, 18 (Suppl. 1), S62–S68. [Google Scholar] [CrossRef]
- Goldfield, G.S.; Epstein, L.H.; Kilanowski, C.K.; Paluch, R.A.; Kogut-Bossier, B. Cost-effectiveness of group and mixed family-based treatment for childhood obesity. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 1843–1849. [Google Scholar] [CrossRef]
- Berry, D.; Melkus, G.; Savoye, M.; Grey, M. An intervention for multi-ethnic obese parents and overweight children. Appl. Nurs. Res. 2007, 20, 63–71. [Google Scholar] [CrossRef]
- Mead, E.; Brown, T.; Rees, K.; Azevedo, L.B.; Whittaker, V.; Jones, D.; Olajide, J.; Mainardi, G.M.; Corpeleijn, E.; O’Malley, C.; et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst. Rev. 2017, 6, CD012651. [Google Scholar] [CrossRef]
- Spear, B.A.; Barlow, S.E.; Ervin, C.; Ludwig, D.S.; Saelens, B.E.; Schetzina, K.E.; Taveras, E.M. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics 2007, 120, S254–S288. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Emmons, K.M. How can we increase translation of research into practice? Types of evidence needed. Annu. Rev. Public Health 2007, 28, 413–433. [Google Scholar] [CrossRef] [PubMed]
- Watson, P.M.; Dugdill, L.; Murphy, R.; Knowles, Z.; Cable, N.T. Moving forward in childhood obesity treatment: A call for translational research. Health Educ. J. 2013, 72, 230–239. [Google Scholar] [CrossRef]
- Brown, T.; Moore, T.H.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019, 23, 7. [Google Scholar] [CrossRef] [PubMed]
- Coyne, J.C.; Thombs, B.D.; Hagedoorn, M. Ain’t necessarily so: Review and critique of recent meta-analyses of behavioral medicine interventions in Health Psychology. Health Psychol. 2010, 29, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Gopalakrishnan, S.; Ganeshkumar, P. Systematic Reviews and Meta-Analysis: Understanding the Best Evidence in Primary Healthcare. J. Family Med. Prim. Care. 2013, 2, 9–14. [Google Scholar] [CrossRef]
- Pawson, R. Evidence-Based Policy: A Realist Perspective; Sage: London, UK, 2006. [Google Scholar]
- Pawson, R.; Greenhalgh, T.; Harvey, G.; Walshe, K. Realist Synthesis: An Introduction; ESRC Research Methods Programme Manchester, University of Manchester: Manchester, UK, 2004. [Google Scholar]
- Wong, G.; Greenhalgh, T.; Westhorp, G.; Buckingham, J.; Pawson, R. RAMESES publication standards: Realist syntheses. BMC Med. 2013, 11, 21. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Guo, H.; Zeng, X.; Zhuang, Q.; Zheng, Y.; Chen, S. Intervention of childhood and adolescents obesity in Shantou city. Obes. Res. Clin. Pract. 2015, 9, 357–364. [Google Scholar] [CrossRef]
- Boff, R.d.M.; Liboni, R.P.A.; Batista, I.P.d.A.; de Souza, L.H.; Oliveira, M.d.S. Weight loss interventions for overweight and obese adolescents: A systematic review. Eat. Weight. Disord. 2017, 22, 211–229. [Google Scholar] [CrossRef]
- Pearson, N.; Griffiths, P.; Biddle, S.J.H.; Johnston, J.P.; Haycraft, E. Individual, behavioral and home environmental factors associated with eating behaviours in young adolescents. Appetite 2017, 112, 35–43. [Google Scholar] [CrossRef]
- Lipsky, L.M.; Haynie, D.L.; Liu, D.; Chaurasia, A.; Gee, B.; Li, K.; Iannotti, R.J.; Simons-Morton, B. Trajectories of eating behaviors in a nationally representative cohort of U.S. adolescents during the transition to young adulthood. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 138. [Google Scholar] [CrossRef] [PubMed]
- Geserick, M.; Vogel, M.; Gausche, R.; Lipek, T.; Spielau, U.; Keller, E.; Pfäffle, R.; Kiess, W.; Körner, A. Acceleration of BMI in early childhood and risk of sustained obesity. N. Engl. J. Med. 2018, 379, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Brown, H.E.; Atkin, A.J.; Panter, J.; Wong, G.; Chinapaw, M.J.M.; van Sluijs, E.M.F. Family-based interventions to increase physical activity in children: A systematic review, meta-analysis and realist synthesis. Obes. Rev. 2016, 17, 345–360. [Google Scholar] [CrossRef] [PubMed]
- Funnell, S.; Rogers, P. Purposeful Program Theory: Effective Use of Theories of Change and Logic Models; John Wiley & Sons: San Francisco, CA, USA, 2016. [Google Scholar]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Wong, G.; Westhorp, G.; Pawson, R. Protocol-realist and meta-narrative evidence synthesis: Evolving standards (RAMESES). BMC Med. Res. Methodol. 2011, 11, 115. [Google Scholar] [CrossRef]
- Popay, J.; Roberts, H.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: Final Report; ESRC Methods Programme: Swindon, Wiltshire, UK, 2006. [Google Scholar]
- Pawson, R.; Greenhalgh, T.; Harvey, G.; Walshe, K. Realist review-a new method of systematic review designed for complex policy interventions. J. Health Serv. Res. Policy 2005, 10 (Suppl. 1), 21–34. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- The Joanna Briggs Institute. Checklist for Quasi-Experimental Studies (Non-Randomized Experimental Studies). Available online: http://joannabriggs.org/assets/docs/critical-appraisal-tools/JBI_Quasi-Experimental_Appraisal_Tool2017.pdf (accessed on 22 August 2017).
- Anderson, J.D.; Newby, R.; Kehm, R.; Barland, P.; Hearst, M.O. Taking steps together: A family-and community-based obesity intervention for urban, multiethnic children. Health Educ. Behav. 2015, 42, 194–201. [Google Scholar] [CrossRef]
- Epstein, L.H.; McKenzie, S.J.; Valoski, A.; Klein, K.R.; Wing, R.R. Effects of mastery criteria and contingent reinforcement for family-based child weight control. Addict. Behav. 1994, 19, 135–145. [Google Scholar] [CrossRef]
- Epstein, L.H.; Paluch, R.A.; Kilanowski, C.K.; Raynor, H.A. The effect of reinforcement or stimulus control to reduce sedentary behavior in the treatment of pediatric obesity. Health Psychol. 2004, 23, 371–380. [Google Scholar] [CrossRef]
- Fisher, A.; Hammersley, M.L.; Jones, R.A.; Morgan, P.J.; Collins, C.E.; Okely, A. Goal setting for weight-related behavior change in children: An exploratory study. Nutr. Health 2018, 24, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Maddison, R.; Marsh, S.; Foley, L.; Epstein, L.H.; Olds, T.; Dewes, O.; Heke, I.; Carter, K.; Jiang, Y.; Ni Mhurchu, C. Screen-time weight-loss intervention targeting children at home (SWITCH): A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 111. [Google Scholar] [CrossRef] [PubMed]
- Siwik, V.; Kutob, R.; Ritenbaugh, C.; Cruz, L.; Senf, J.; Aickin, M.; Going, S.; Shatte, A. Intervention in overweight children improves body mass index (BMI) and physical activity. J. Am. Board. Fam. Med. 2013, 26, 126–137. [Google Scholar] [CrossRef] [PubMed]
- Spurrier, N.J.; Bell, L.; Wilson, A.; Lowe, E.; Golley, R.; Magarey, A.A. Minimal change in children’s lifestyle behaviours and adiposity following a home-based obesity intervention: Results from a pilot study. BMC Res. Notes 2016, 9, 26. [Google Scholar] [CrossRef]
- Watson, P.M.; Dugdill, L.; Owen, S.; Hargreaves, J.; Staniford, L.J.; Murphy, R.C.; Knowles, Z.; Cable, N.T. Service evaluation of the GOALS family-based childhood obesity treatment intervention during the first 3 years of implementation. BMJ Open 2015, 5, e006519. [Google Scholar] [CrossRef]
- Wong, E.M.; Cheng, M.M. Effects of motivational interviewing to promote weight loss in obese children. J. Clin. Nurs. 2013, 22, 2519–2530. [Google Scholar] [CrossRef]
- Yusop, N.B.M.; Mohd, N.B.; Shariff, Z.M.; Hwu, T.T.; Talib, R.A.; Spurrier, N. The effectiveness of a stage-based lifestyle modification intervention for obese children. BMC Public Health 2018, 18, 299. [Google Scholar] [CrossRef]
- Arauz Boudreau, A.D.; Kurowski, D.S.; Gonzalez, W.I.; Dimond, M.A.; Oreskovic, N.M. Latino families, primary care, and childhood obesity: A randomized controlled trial. Am. J. Prev. Med. 2013, 44 (Suppl. 3), S247–S257. [Google Scholar] [CrossRef]
- Brennan, L.; Walkley, J.; Lukeis, S.; Risteska, A. A cognitive behavioural intervention for overweight and obese adolescents illustrated by four case studies. Behav. Chang. 2009, 26, 190–213. [Google Scholar] [CrossRef]
- Cason-Wilkerson, R.; Goldberg, S.; Albright, K.; Allison, M.; Haemer, M. Factors influencing healthy lifestyle changes: A qualitative look at low-income families engaged in treatment for overweight children. Child. Obes. 2015, 11, 170–176. [Google Scholar] [CrossRef]
- Davis, A.M.; Daldalian, M.C.; Mayfield, C.A.; Dean, K.; Black, W.R.; Sampilo, M.L.; Gonzalez-Mijares, M.; Suminski, R. Outcomes from an urban pediatric obesity program targeting minority youth: The Healthy Hawks program. Child. Obes. 2013, 9, 492–500. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.M.; Sampilo, M.; Gallagher, K.S.; Landrum, Y.; Malone, B. Treating rural pediatric obesity through telemedicine: Outcomes from a small randomized controlled trial. J. Pediatr. Psychol. 2013, 38, 932–943. [Google Scholar] [CrossRef] [PubMed]
- Delamater, A.M.; Pulgaron, E.R.; Rarback, S.; Hernandez, J.; Carillo, A.; Christiansen, S.; Severson, H.H. Web-based family intervention for overweight children: A pilot study. Child. Obes. 2013, 9, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.H.; Roemmich, J.N.; Stein, R.I.; Paluch, R.A.; Kilanowski, C.K. The challenge of identifying behavioral alternatives to food: Clinic and field studies. Ann. Behav. Med. 2005, 30, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Janicke, D.M. Treatment of pediatric obesity using a parent-only approach: A case example. Health Psychol. 2013, 32, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Ho, M.; Keung, V.M.; Kwong, A.C. Childhood obesity management shifting from health care system to school system: Intervention study of school-based weight management programme. BMC Public Health 2014, 14, 1128. [Google Scholar] [CrossRef] [PubMed]
- Reinehr, T.; Schaefer, A.; Winkel, K.; Finne, E.; Toschke, A.M.; Kolip, P. An effective lifestyle intervention in overweight children: Findings from a randomized controlled trial on “Obeldicks light”. Clin. Nutr. 2010, 29, 331–336. [Google Scholar] [CrossRef]
- Robertson, W.; Fleming, J.; Kamal, A.; Hamborg, T.; Khan, K.A.; Griffiths, F.; Stewart-Brown, S.; Stallard, N.; Petrou, S.; Simkiss, D.; et al. Randomised controlled trial and economic evaluation of the ‘Families for Health’ programme to reduce obesity in children. Arch. Dis. Child. 2017, 102, 416–426. [Google Scholar] [CrossRef]
- Semke, C.A. Examining the Efficacy of Conjoint Behavioral Consultation for Health Behaviors of Children with Obesity. Ph.D. Thesis, University of Nebraska-Lincoln, Lincoln, NE, USA, 2011. Available online: digitalcommons.unl.edu/dissertations/AAI3461355 (accessed on 24 April 2020). ETD collection.
- Teder, M.; Mörelius, E.; Nordwall, M.; Bolme, P.; Ekberg, J.; Wilhelm, E.; Timpka, T. Family-based behavioural intervention program for obese children: An observational study of child and parent lifestyle interpretations. PLoS ONE 2013, 8, e71482. [Google Scholar] [CrossRef]
- West, F.; Sanders, M.R.; Cleghorn, G.J.; Davies, P.S. Randomised clinical trial of a family-based lifestyle intervention for childhood obesity involving parents as the exclusive agents of change. Behav. Res. Ther. 2010, 48, 1170–1179. [Google Scholar] [CrossRef]
- Wright, J.A.; Phillips, B.D.; Watson, B.L.; Newby, P.K.; Norman, G.J.; Adams, W.G. Randomized trial of a family-based, automated, conversational obesity treatment program for underserved populations. Obesity (Silver Spring) 2013, 21, E369–E378. [Google Scholar] [CrossRef] [PubMed]
- Chaiopanant, S. A 3-Years-Follow-Up study of the effect of the weight control program on KAP and behavior among overweight and obese school children in nonthaburi province. J. Med. Assoc. Thai. 2016, 99, 853–860. [Google Scholar] [PubMed]
- Cohen, T.R.; Hazell, T.J.; Vanstone, C.A.; Rodd, C.; Weiler, H.A. Changes in eating behavior and plasma leptin in children with obesity participating in a family-centered lifestyle intervention. Appetite 2018, 125, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.M.; Sampilo, M.; Gallagher, K.S.; Dean, K.; Saroja, M.B.; Yu, Q.; He, J.; Sporn, N. Treating rural paediatric obesity through telemedicine vs. telephone: Outcomes from a cluster randomized controlled trial. J. Telemed. Telecare 2016, 22, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Elizondo-Montemayor, L.; Gutierrez, N.G.; Moreno, D.M.; Martinez, U.; Tamargo, D.; Treviño, M. School-based individualised lifestyle intervention decreases obesity and the metabolic syndrome in Mexican children. J. Hum. Nutr. Diet. 2013, 26 (Suppl. 1), 82–89. [Google Scholar] [CrossRef] [PubMed]
- Joosse, L.; Steams, M.; Anderson, H.; Hartlaub, P.; Euclide, J. Fit Kids/Fit Families: A report on a countywide effort to promote healthy behaviors. WMJ 2008, 107, 231–236. [Google Scholar] [PubMed]
- Nemet, D.; Barkan, S.; Epstein, Y.; Friedland, O.; Kowen, G.; Eliakim, A. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics 2005, 115, e4439. [Google Scholar] [CrossRef]
- Schwartz, R.P.; Vitolins, M.Z.; Case, L.D.; Armstrong, S.C.; Perrin, E.M.; Cialone, J.; Bell, R.A. The YMCA healthy, fit, and strong program: A community-based, family-centered, low-cost obesity prevention/treatment pilot study. Child. Obes. 2012, 8, 577–582. [Google Scholar] [CrossRef]
- Van Middlekoop, M.; Ligthart, K.A.M.; Paulis, W.D.; van Teeffelen, J.; Kornelisse, K.; Koes, B.W. A multidisciplinary intervention programme for overweight and obese children in deprived areas. Fam. Pract. 2017, 34, 702707. [Google Scholar] [CrossRef]
- Williams, D.P. The Effectiveness of a Structured, Long-Term, Multi-Component, Family-Based Weight Management Program in Reducing Body Mass Index Z-Scores and Improving Lifestyle Habits in Overweight/Obese Children and Adolescents. Ph.D. Thesis, Utah State University, Logan, UT, USA, 2011. [Google Scholar]
- Bandura, A. Social Foundations of thought and Action: A Social Cognitive Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Hursh, S.R. Behavioral economics. J. Exp. Anal. Behav. 1987, 42, 435–452. [Google Scholar] [CrossRef]
- Janz, N.K.; Becker, M.H. The health belief model: A decade later. Health Educ. Behav. 1984, 11, 1–47. [Google Scholar] [CrossRef] [PubMed]
- Harter, S. Effectance motivation reconsidered. Hum. Dev. 1978, 21, 34–64. [Google Scholar] [CrossRef]
- Cullen, K.W.; Baranowski, T.; Smith, S.P. Using goal setting as a strategy for dietary behavior change. J. Am. Diet. Assoc. 2001, 101, 562–566. [Google Scholar] [CrossRef]
- Locke, E.A.; Latham, G.P. Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. Am. Psychol. 2002, 57, 705–717. [Google Scholar] [CrossRef] [PubMed]
- Sebire, S.J.; Standage, M.; Vansteenkiste, M. Examining instrinsic versus extrinsic exercise goals: Cognitive, affective and behavioral outcomes. J. Sport. Exerc. Psychol. 2009, 31, 189–210. [Google Scholar] [CrossRef] [PubMed]
- Shilts, M.K.; Horowitz, M.; Townsend, M.S. Goal setting as a strategy for dietary and physical activity behavior change: A review of the literature. Am. J. Health. Promot. 2004, 19, 81–93. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; LeBlanc, A.G.; Kho, M.E.; Saunders, T.J.; Larouche, R.; Colley, R.C.; Goldfield, G.; Gorber, S.C. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int. J. Behav. Nutr. Phys. 2011, 8, 98. [Google Scholar] [CrossRef]
- Schmidt, M.E.; Haines, J.; O’Brien, A.; McDonald, J.; Price, S.; Sherry, B.; Taveras, E.M. Systematic review of effective strategies for reducing screen time among young children. Obesity 2012, 20, 1338–1354. [Google Scholar] [CrossRef]
- Van Grieken, A.; Ezendam, N.P.; Paulis, W.D.; van der Wouden, J.C.; Raat, H. Primary prevention of overweight in children and adolescents: A meta-analysis of the effectiveness of interventions aiming to decrease sedentary behaviour. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 61. [Google Scholar] [CrossRef]
- Epstein, L.H.; Saelens, B.E.; Myers, M.D.; Vito, D. Effects of decreasing sedentary behaviors on activity choice in obese children. Health Psychol. 1997, 16, 107–113. [Google Scholar] [CrossRef]
- Timperio, A.; Salmon, J.; Ball, K. Evidence-based strategies to promote physical activity among children, adolescents and young adults: Review and update. J. Sci. Med. Sport. 2004, 7 (Suppl. 1), 20–29. [Google Scholar] [CrossRef]
- Reivich, K.; Shatte, A. The Resilience Factor; Broadway Books: New York, NY, USA, 2002. [Google Scholar]
- Bronfenbrenner, U. Ecological Models of Human Development. In International Encyclopedia of Education, 2nd ed.; Gauvain, M., Cole, M., Eds.; Freeman: New York, NY, USA, 1993; Volume 3, pp. 37–43. [Google Scholar]
- Ludwig, D.S. Weight loss strategies for adolescents. JAMA 2012, 37, 498–508. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.H.; Voloski, A.; Wing, R.R.; McCurley, I. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol. 1994, 13, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Swinburn, B.A. Obesity prevention: The role of policies, laws and regulations. Aust. N. Z. Health Policy 2008, 5, 12. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.M.; Deci, E.L. Self-Determination Theory: Basic Psychological Needs in Motivation, Development, and Wellness; Guilford Publishing: New York, NY, USA, 2017. [Google Scholar]
- Alulis, S.; Grabowski, D. Theoretical frameworks informing family-based child and adolescent obesity interventions: A qualitative meta-synthesis. Obes. Res. Clin. Pract. 2017, 11, 627–639. [Google Scholar] [CrossRef]
- Staiano, A.E.; Beyl, R.A.; Hsia, D.S.; Jarrell, A.R.; Katzmarzyk, P.T.; Mantzor, S.; NewtonJr, R.L.; Tyson, P. Step tracking with goals increases children’s weight loss in behavioral intervention. Child. Obes. 2017, 13. [Google Scholar] [CrossRef]
- Wilfley, D.E.; Saelens, B.E.; Stein, R.I.; Best, J.R.; Kolko, R.P.; Schechtman, K.B.; Wallendorf, M.; Welch, R.R.; Perri, M.G.; Epstein, L.H. Dose, content, and mediators of family-based treatment for childhood obesity: A multisite randomized clinical trial. JAMA Pediatr. 2017, 171, 1151–1159. [Google Scholar] [CrossRef]
- Aires, L.; Silva, G.; Martins, C.; Marques, E.; Lagoa, M.J.; Ribeiro, J.C.; Rêgo, C.; Nascimento, H.; Pereira, P.R.; Santos-Silva, A.; et al. Exercise intervention and cardiovascular risk factors in obese children. Comparison between obese youngsters taking part in a physical activity school-based programme with and without individualised diet counselling: The ACORDA project. Ann. Hum. Biol. 2016, 43, 183–190. [Google Scholar] [CrossRef]
- Lasecki, K.; Olympia, D.; Clark, E.; Jenson, W.; Heathfield, L.T. Using behavioral interventions to assist children with type 1 diabetes manage blood glucose levels. Sch. Psychol. Q. 2008, 23, 389–406. [Google Scholar] [CrossRef]
- Fenner, A.A.; Straker, L.M.; Davis, M.C.; Hagger, M.A. Theoretical underpinnings of a need-supportive intervention to address sustained healthy lifestyle changes in overweight and obese adolescents. Psychol. Sport Exerc. 2013, 14, 819–829. [Google Scholar] [CrossRef]
- Girelli, L.; Luccidi, F. A self-determination theory based intervention to promote healthy eating and physical activity in school-aged children. Cuad. Psicol. Del Deporte 2016, 16, 13–20. Available online: https://revistas.um.es/cpd/article/view/278391 (accessed on 24 April 2020).
- Di Noia, J.; Thompson, D. Processes of change for increasing fruit and vegetable consumption among economically disadvantaged African American adolescents. Eat. Behav. 2012, 1, 58–61. [Google Scholar] [CrossRef] [PubMed]
- Romain, A.J.; Chevance, G.; Caudroit, J.; Bernard, P. Le modèle transthéorique: Description, intérêts et application dans la motivation à l’activité physique auprès de populations en surcharge pondérale. Obesite 2016, 11, 47–55. [Google Scholar] [CrossRef]
- Sokel, R.L.; Qin, B.; Poti, J. Parenting styles and body mass index: A systematic review of prospective studies among children. Obes. Rev. 2017, 18, 281–292. [Google Scholar] [CrossRef]
- Zubatsky, M.; Berge, J.; Neumark-Sztainer, D. Longitudinal associations between parenting style and adolescent disordered eating behaviors. Eat. Weight Disord. 2015, 20, 187–194. [Google Scholar] [CrossRef]
- Tai-Seale, T.; Chandler, C. Nutrition and Overweight Concerns in Rural Areas: A Literature Review. Rural Healthy People 2010: A Companion Document to Healthy People 2010; The Texas A & M University System Health Science Center: College Station, TX, USA, 2003; Volume 2. [Google Scholar]
- Papoutsi, C.; Mattick, K.; Pearson, M.; Brennan, N.; Briscoe, S.; Wong, G. Interventions to Improve Antimicrobial Prescribing of Doctors in Training (IMPACT): A Realist Review; Health Services and Delivery Research: Southampton, UK, 2018; Volume 6. [Google Scholar]

| Study Characteristic | Inclusion Criteria |
|---|---|
| Country and language | Any country or language. |
| Status | Published peer-reviewed and grey literature. |
| Dates | No date restriction. |
| Design | RCTs, cluster RCTs, all quasi-experimental and observational designs (including cohort, cross sectional, longitudinal, case control studies), case series and case reports, and qualitative studies. |
| Setting | All community-, school-, and home-based interventions, including initiatives trialed within existing weight-management programs. Remote interventions (i.e., delivered via telephone or other technology) were also included. Articles were excluded if based on interventions carried out in hospital or research-based institutions. |
| Intervention duration and follow-up | Any intervention or follow-up duration. |
| Population | Children aged 7–13 years classified as overweight or obese, (including but not restricted to the definition of Centre’s for Diseases Control and Prevention, where body mass index (BMI) must be greater than the 85th percentile for age and sex). Articles were excluded if the primary focus was adolescent or adult obesity. |
| Intervention | Child obesity-focused, family-based interventions. All eligible articles were ‘multicomponent’ and included (i) education, (ii) behavior change strategies as either stand-alone or multicomponent intervention, and (iii) parental involvement. |
| Outcomes | Primary (essential): Behavioral outcomes relating to both dietary and physical activity behavior change, including subjective or objective measures of increases or decreases in healthy eating or an increase or decrease in physical activity or sedentary behavior. Secondary (not essential): Social cognitive variables (e.g., self-esteem, physical activity enjoyment, self-efficacy, intrinsic motivation) and qualitative outcomes such as barriers and facilitators to implementing new behaviors. |
| Study Characteristic | Proportion % (n = 36 Interventions) | % Favored Intervention (Diet and PA) | % Favored Intervention (Diet) | % Favored Intervention (PA) |
|---|---|---|---|---|
| Study Design | ||||
| RCTs/cRCTs | 31 (11) | 9 (1) | 27 (3) | 18 (2) |
| Quasi-experimental (non-randomized)/observational studies | 42 (15) | 27 (4) | 27 (4) | 7 (1) |
| Case reports/case series | 8 (3) | 67 (2) | ||
| Pilot/feasibility studies | 19 (7) | 29 (2) | 29 (2) | |
| Qualitative component | 8 (3) | 33 (1) | ||
| Year of Publication | ||||
| 2018–2019 | 8 (3) | 67 (2) | 33 (1) | |
| 2016–2017 | 14 (5) | 20 (1) | ||
| 2010–2015 | 56 (20) | 35 (7) | 10 (2) | 15 (3) |
| 1994–2009 | 22 (8) | 25 (2) | 25 (2) | 13 (1) |
| Study Location | ||||
| USA | 47 (17) | 35 (6) | 12 (2) | 6 (1) |
| UK | 6 (2) | |||
| Europe (excl. UK) | 8 (3) | 33 (1) | ||
| Australia | 11 (4) | 25 (1) | 25 (1) | |
| Other locations* | (28 (10) | 20 (2) | 30 (3) | 40 (4) |
| Sample Size | ||||
| <50 | 42 (15) | 27 (4) | 7 (1) | 20 (3) |
| 51–200 | 53 (19) | 26 (5) | 26 (5) | 11 (2) |
| ≥200 | 6 (2) | 50 (1) | ||
| Priority Population (low socioeconomic status) | ||||
| >50% Hispanic/Latino | 11 (4) | 50 (2) | 25 (1) | |
| Other priority populations** | 14 (5) | 20 (1) | 20 (1) | |
| Intervention Duration | ||||
| ≤1 month (up to 4 weeks) | 3 (1) | 100 (1) | ||
| 1–2 months (up to 8 weeks) | 6 (2) | 50 (1) | ||
| >2–3 months (up to 12 weeks) | 28 (10 | 10 (1) | 20 (2) | 20 (2) |
| >3 months (12 weeks+) | 58 (21) | 29 (6) | 19 (4) | 14 (3) |
| ≥12 months | 6 (2) | |||
| Follow-up (Post-Intervention) Periods Reported Sustained effects shown | ||||
| Short term: up to 6 months | 11 (4) | 50 (2) | 25 (1) | |
| Medium-term: 7–12 months | 22 (8) | 13 (1) | ||
| Long term: >12 months | 14 (5) | 20 (1) | ||
| No follow-up | 53 (19) | na | na | na |
| Intervention Deliverer*** | ||||
| Community registered dietitians/exercise physiologists | 42 (15) | 27 (4) | 27 (4) | 20 (3) |
| Medical/health care staff | 25 (9) | 11 (1) | 22 (2) | 22 (2) |
| Other clinicians | 33 (12) | 25 (3) | 8 (1) | |
| Local community experts on nutrition and exercise | 36 (13) | 15 (2) | 15 (2) | 23 (3) |
| Research team/research assistant | 11 (4) | 50 (2) | ||
| Automated component | 3 (1) | 100 (1) | ||
| Unspecified | 14 (5) | 20 (1) | 40 (2) | |
| Group or Individual Intervention | ||||
| Predominantly group-based sessions | 15 (27) | 19 (5) | 26 (7) | 11 (3) |
| Exclusively individual | 25 (9) | 44 (4) | 22 (2) | |
| Setting | ||||
| Predominantly school | 14 (5) | 40 (2) | 20 (1) | 40 (2) |
| Predominantly community center | 58 (21) | 19 (4) | 29 (6) | 10 (2) |
| Predominantly home | 8 (3) | |||
| Collaborative | 6 (2) | 50 (1) | 50 (1) | |
| Remote delivery component | 22 (8) | 50 (4) | 50 (1) | |
| PA Outcome Measure✢ | ||||
| Subjective | 86 (31) | 26 (8) | 16 (5) | 16 (5) |
| Objective | 36 (13) | 31 (4) | 15 (2) | |
| Diet Outcome Measure✢ | ||||
| Subjective | 100 (36) | 25 (9) | 19 (7) | 14 (5) |
| Objective | 6 (2) | 50 (1) | ||
General notes—
| ||||
| Study Characteristic | Proportion % (n = 36 Interventions) | % Favored Intervention (Diet and PA) | % Favored Intervention (Diet) | % Favored Intervention (PA) |
|---|---|---|---|---|
| Outcome Measures | ||||
| Diet- and PA-related only | 56 (20) | 30 (6) | 30 (6) | 20 (4) |
| Additional behavioral/psychosocial variables* | 44 (16) | 19 (3) | 6 (1) | 6 (1) |
| Theoretical Grounding (in relation to BCTs/mechanisms) | ||||
| Theory identified | 44 (16) | 25 (4) | 19 (3) | 19 (3) |
| No theory identified | 56 (20) | 25 (5) | 20 (4) | 10 (2) |
| Type of Parental Involvement | ||||
| Exclusive agents for change | 14 (5) | 40 (2) | ||
| Promoting support of child’s behavior change | 31 (11) | 45 (5) | 9 (1) | |
| Aimed to change both parent and child behavior | 17 (6) | 17 (1) | 17 (1) | 17 (1) |
| Parent acknowledged as influential** | 39 (14) | 21 (3) | 29 (4) | 21 (3) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Enright, G.; Allman-Farinelli, M.; Redfern, J. Effectiveness of Family-Based Behavior Change Interventions on Obesity-Related Behavior Change in Children: A Realist Synthesis. Int. J. Environ. Res. Public Health 2020, 17, 4099. https://doi.org/10.3390/ijerph17114099
Enright G, Allman-Farinelli M, Redfern J. Effectiveness of Family-Based Behavior Change Interventions on Obesity-Related Behavior Change in Children: A Realist Synthesis. International Journal of Environmental Research and Public Health. 2020; 17(11):4099. https://doi.org/10.3390/ijerph17114099
Chicago/Turabian StyleEnright, Gemma, Margaret Allman-Farinelli, and Julie Redfern. 2020. "Effectiveness of Family-Based Behavior Change Interventions on Obesity-Related Behavior Change in Children: A Realist Synthesis" International Journal of Environmental Research and Public Health 17, no. 11: 4099. https://doi.org/10.3390/ijerph17114099
APA StyleEnright, G., Allman-Farinelli, M., & Redfern, J. (2020). Effectiveness of Family-Based Behavior Change Interventions on Obesity-Related Behavior Change in Children: A Realist Synthesis. International Journal of Environmental Research and Public Health, 17(11), 4099. https://doi.org/10.3390/ijerph17114099






