Risk Factors related to Late Failure of Dental Implant—A Systematic Review of Recent Studies
Abstract
:1. Introduction
2. Methodology
2.1. Protocol and Key Question
2.2. Eligibility Criteria
2.3. Literature Resource and Search Strategy
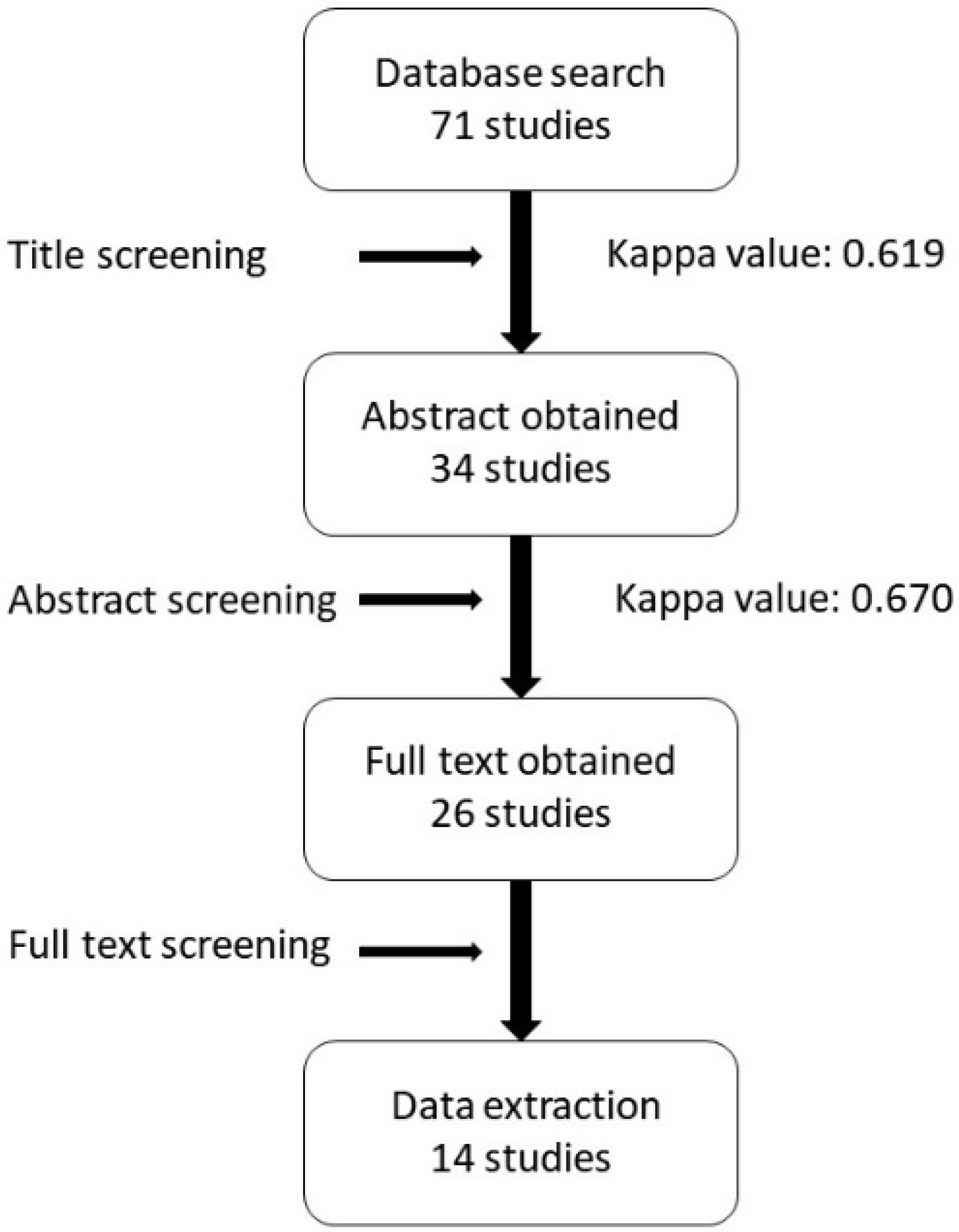
2.4. Article Review Process
3. Results
3.1. Study Selection
3.2. Data Extraction
3.2.1. Age and Sex
3.2.2. Systemic Factors
Radiation Therapy
Diabetes
Other Medical Problems
3.2.3. Oral History
3.2.4. Smoking
3.2.5. Implant Location
3.2.6. Bone Condition
3.2.7. Type of Implant
3.2.8. Implant Length and Diameter
3.2.9. Surgery-Related Factors
3.2.10. Other Factors
4. Discussion
4.1. Factors Related to Patient History
4.1.1. Patient Demographics and Medical History
4.1.2. Habits
4.2. Factors Related to Clinical Parameters
4.2.1. Implant Location
4.2.2. Bone Condition
4.2.3. Adjacent Dentition
4.3. Factors Related to Decisions Made by the Doctor
4.3.1. Implant Selection
4.3.2. Surgical Procedure
4.3.3. Prosthesis Design
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Branemark, P.-I. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand. J. Plast. Reconstr. Surg. Suppl. 1977, 16, 1–132. [Google Scholar] [PubMed]
- Romeo, E.; Chiapasco, M.; Ghisolfi, M.; Vogel, G. Long-term clinical effectiveness of oral implants in the treatment of partial edentulism: Seven-year life table analysis of a prospective study with ITI® Dental Implants System used for single-tooth restorations. Clin. Oral Implant. Res. 2002, 13, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Adell, R.; Lekholm, U.; Rockler, B.; Brånemark, P.-I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef]
- Esposito, M.; Hirsch, J.M.; Lekholm, U.; Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants,(I). Success criteria and epidemiology. Eur. J. Oral Sci. 1998, 106, 527–551. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Schmid, J. Pathogenesis of implant failures. Periodontol. 2000 1994, 4, 127–138. [Google Scholar] [CrossRef]
- Elaskary, A. Fundamentals of Esthetic Implant Dentistry; John Wiley & Sons: Hoboken, NJ, USA, 2008. [Google Scholar]
- Manor, Y.; Oubaid, S.; Mardinger, O.; Chaushu, G.; Nissan, J. Characteristics of early versus late implant failure: A retrospective study. J. Oral Maxillofac. Surg. 2009, 67, 2649–2652. [Google Scholar] [CrossRef]
- Sakka, S.; Baroudi, K.; Nassani, M.Z. Factors associated with early and late failure of dental implants. J. Investig. Clin. Dent. 2012, 3, 258–261. [Google Scholar] [CrossRef]
- Clark, D.; Levin, L. Dental implant management and maintenance: How to improve long-term implant success? Quintessence Int. 2016, 47, 417–423. [Google Scholar]
- van Steenberghe, D.; Lekholm, U.; Bolender, C.; Folmer, T.; Henry, P.; Herrmann, I.; Higuchi, K.; Laney, W.; Lindén, U.; Åstrand, P. The Applicability of Osseointegrated Oral Implants in the Rehabilitation of Partial Edentulism: A Prospective Multicenter Study on 558 Fixtures. Int. J. Oral Maxillofac. Implant. 1990, 5, 119–136. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. BMJ 2009, 339. [Google Scholar] [CrossRef] [Green Version]
- Derks, J.; Håkansson, J.; Wennström, J.; Tomasi, C.; Larsson, M.; Berglundh, T. Effectiveness of implant therapy analyzed in a Swedish population: Early and late implant loss. J. Dent. Res. 2015, 94, 44S–51S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noda, T. A longitudinal retrospective study of the analysis of the risk factors of implant failure by the application of generalized estimating equations. J. Prosthodont. Res. 2015, 59, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Kermalli, J.Y.; Deporter, D.A.; Atenafu, E.G.; Lam, E.W. A retrospective report on three implant devices used to restore posterior partial edentulism: Overall performance and changes in crestal bone levels. Int. J. Periodontics Restor. Dent. 2014, 34, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Doll, C.; Nack, C.; Raguse, J.-D.; Stricker, A.; Duttenhoefer, F.; Nelson, K.; Nahles, S. Survival analysis of dental implants and implant-retained prostheses in oral cancer patients up to 20 years. Clin. Oral Investig. 2015, 19, 1347–1352. [Google Scholar] [CrossRef] [PubMed]
- Dvorak, G.; Arnhart, C.; Heuberer, S.; Huber, C.D.; Watzek, G.; Gruber, R. Peri-implantitis and late implant failures in postmenopausal women: A cross-sectional study. J. Clin. Periodontol. 2011, 38, 950–955. [Google Scholar] [CrossRef]
- Strietzel, F.P.; Karmon, B.; Lorean, A.; Fischer, P.P. Implant-prosthetic rehabilitation of the edentulous maxilla and mandible with immediately loaded implants: Preliminary data from a retrospective study, considering time of implantation. Int. J. Oral Maxillofac. Implant. 2011, 26, 139–147. [Google Scholar]
- Levin, L.; Ofec, R.; Grossmann, Y.; Anner, R. Periodontal disease as a risk for dental implant failure over time: A long-term historical cohort study. J. Clin. Periodontol. 2011, 38, 732–737. [Google Scholar] [CrossRef]
- Le, B.T.; Follmar, T.; Borzabadi-Farahani, A. Assessment of short dental implants restored with single-unit nonsplinted restorations. Implant Dent. 2013, 22, 499–502. [Google Scholar] [CrossRef] [Green Version]
- Vercruyssen, M.; Marcelis, K.; Coucke, W.; Naert, I.; Quirynen, M. Long-term, retrospective evaluation (implant and patient-centred outcome) of the two-implants-supported overdenture in the mandible. Part 1: Survival rate. Clin. Oral Implant. Res. 2010, 21, 357–365. [Google Scholar] [CrossRef]
- Alsaadi, G.; Quirynen, M.; Komárek, A.; Van Steenberghe, D. Impact of local and systemic factors on the incidence of late oral implant loss. Clin. Oral Implant. Res. 2008, 19, 670–676. [Google Scholar]
- Jemt, T.; Karouni, M.; Abitbol, J.; Zouiten, O.; Antoun, H. A retrospective study on 1592 consecutively performed operations in one private referral clinic. Part II: Peri-implantitis and implant failures. Clin. Implant Dent. Relat. Res. 2017, 19, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Jemt, T. A retro-prospective effectiveness study on 3448 implant operations at one referral clinic: A multifactorial analysis. Part II: Clinical factors associated to peri-implantitis surgery and late implant failures. Clin. Implant Dent. Relat. Res. 2017, 19, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Bruxism and dental implant treatment complications: A retrospective comparative study of 98 bruxer patients and a matched group. Clin. Oral Implant. Res. 2017, 28, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Gómez-de Diego, R. Indications and contraindications of dental implants in medically compromised patients: Update. Med. Oral Patol. Oral Cir. Bucal 2014, 19, e483. [Google Scholar] [CrossRef]
- Heitz-Mayfield, L.J. Peri-implant diseases: Diagnosis and risk indicators. J. Clin. Periodontol. 2008, 35, 292–304. [Google Scholar] [CrossRef]
- Karoussis, I.K.; Kotsovilis, S.; Fourmousis, I. A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients. Clin. Oral Implant. Res. 2007, 18, 669–679. [Google Scholar] [CrossRef]
- Koldsland, O.C.; Scheie, A.A.; Aass, A.M. Prevalence of implant loss and the influence of associated factors. J. Periodontol. 2009, 80, 1069–1075. [Google Scholar] [CrossRef]
- Porter, S.E.; Hanley, E.N. The musculoskeletal effects of smoking. JAAOS J. Am. Acad. Orthop. Surg. 2001, 9, 9–17. [Google Scholar] [CrossRef]
- Manzano, G.; Montero, J.; Martín-Vallejo, J.; Del Fabbro, M.; Bravo, M.; Testori, T. Risk factors in early implant failure: A meta-analysis. Implant Dent. 2016, 25, 272–280. [Google Scholar] [CrossRef] [Green Version]
- De Angelis, F.; Papi, P.; Mencio, F.; Rosella, D.; Di Carlo, S.; Pompa, G. Implant survival and success rates in patients with risk factors: Results from a long-term retrospective study with a 10 to 18 years follow-up. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 433–437. [Google Scholar]
- Mohl, N.D. A Textbook of Occlusion; Quintessence Pub Co.: Chicago, IL, USA, 1988. [Google Scholar]
- Yadav, K.; Nagpal, A.; Agarwal, S.; Kochhar, A. Intricate Assessment and Evaluation of Effect of Bruxism on Long-term Survival and Failure of Dental Implants: A Comparative Study. J. Contemp. Dent. Pract. 2016, 17, 670–674. [Google Scholar] [PubMed]
- Ji, T.-J.; Kan, J.Y.; Rungcharassaeng, K.; Roe, P.; Lozada, J.L. Immediate loading of maxillary and mandibular implant-supported fixed complete dentures: A 1-to 10-year retrospective study. J. Oral Implantol. 2012, 38, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Glauser, R.; Ree, A.; Lundgren, A.; Gottlow, J.; Hammerle, C.H.; Scharer, P. Immediate occlusal loading of Brånemark implants applied in various jawbone regions: A prospective, 1-year clinical study. Clin. Implant Dent. Relat. Res. 2001, 3, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Bruxism and dental implants: A meta-analysis. Implant Dent. 2015, 24, 505–516. [Google Scholar] [CrossRef]
- Helkimo, E.; Carlsson, G.E.; Helkimo, M. Bite force and state of dentition. Acta Odontol. Scand. 1977, 35, 297–303. [Google Scholar] [CrossRef]
- Sreenivasan, P.K.; Prasad, K.V. Distribution of dental plaque and gingivitis within the dental arches. J. Int. Med. Res. 2017, 45, 1585–1596. [Google Scholar] [CrossRef] [Green Version]
- Park, H.-S.; Lee, Y.-J.; Jeong, S.-H.; Kwon, T.-G. Density of the alveolar and basal bones of the maxilla and the mandible. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 30–37. [Google Scholar] [CrossRef]
- Chugh, T.; Ganeshkar, S.V.; Revankar, A.V.; Jain, A.K. Quantitative assessment of interradicular bone density in the maxilla and mandible: Implications in clinical orthodontics. Prog. Orthod. 2013, 14, 38. [Google Scholar] [CrossRef] [Green Version]
- Turkyilmaz, I.; McGlumphy, E.A. Influence of bone density on implant stability parameters and implant success: A retrospective clinical study. BMC Oral Health 2008, 8, 32. [Google Scholar] [CrossRef] [Green Version]
- Sakka, S.; Coulthard, P. Bone quality: A reality for the process of osseointegration. Implant Dent. 2009, 18, 480–485. [Google Scholar] [CrossRef]
- Chung, D.M.; Oh, T.-J.; Lee, J.; Misch, C.E.; Wang, H.-L. Factors affecting late implant bone loss: A retrospective analysis. Int. J. Oral Maxillofac. Implant. 2007, 22, 117–126. [Google Scholar]
- Yong, L.T.; Moy, P.K. Complications of Computer-Aided-Design/Computer-Aided-Machining-Guided (NobelGuide™) Surgical Implant Placement: An Evaluation of Early Clinical Results. Clin. Implant Dent. Relat. Res. 2008, 10, 123–127. [Google Scholar] [CrossRef] [PubMed]
| Author & Year | No Implants Placed | No Late Failure of Implants Loss | Risk Factors Associated with Late Failure of Dental Implant (Medical History Related) | ||||
|---|---|---|---|---|---|---|---|
| Age & Sex | Systemic History | Oral History | Smoking | Bruxism | |||
| Manor et al., 2009 [7] | Age (−) | Medical problem (+) | |||||
| Derks et al., 2015 [12] | 2367 | 46 (2%) | Initial diagnosis of periodontitis (−) | (−) | |||
| Noda et al., 2015 [13] | 710 | 10 (1.4%) | Sex (−) Age (−) | (−) | |||
| Doll et al., 2015 [15] | 830 | 20 (2.4%) | Sex (−) Age (−) | RCTx (+) | |||
| Dvorak et al., 2011 [16] | 828 | 69 (8.3%) | Age (−) | Diabetes (−) Thyro (−) | (−) | ||
| Strietzel et al., 2011 [17] | 283 | 5 (1.8%) | (−) | ||||
| Levin et al., 2011 [18] | 2259 | 50 (2.2%) | Severe periodontitis (+) | (−) | |||
| Le et al., 2013 [19] | 221 | 1 (0.4%) | Diabetes (−) | (−) | |||
| Vercruyss-en et al., 2010 [20] | 1051 | 37 (3.5%) | Diabetes (−) | Periodontitis (+) | (−) | ||
| Alsaadi et al., 2008 [21] | 1514 | 101 (6.7%) | Diabetes (−) Medical problem (−) RTx (+) | (−) | |||
| Chrcanovic et al., 2017 [24] | 854 | (+) | |||||
| Author & Year | No Implants Placed | No Late Failure of Implants Loss | Risk Factors Associated with Late Failure of Dental Implant (Implant Treatment Related) | |||||
|---|---|---|---|---|---|---|---|---|
| Implant Location | Bone Condition | Type of Implant | Implant Size | Surgical Related | Others | |||
| Manor et al., 2009 [7] | Posterior (+) | |||||||
| Derks et al., 2015 [12] | 2367 | 46 (2%) | Implant brand (+) | |||||
| Noda et al., 2015 [13] | 710 | 10 (1.4%) | Maxilla (+) Posterior (+) | L (−) D (−) | Bone graft (−) | ≥20 teeth remaining (+) RD opposing (+) ISO-conus type connection (+) | ||
| Kermalli et al., 2014 [14] | 799 | 19 (2.4%) | Press-fit SPS (+) | |||||
| Doll et al., 2015 [15] | 830 | 20 (2.4%) | Jaw (−) | |||||
| Dvorak et al., 2011 [16] | 828 | 69 (8.3%) | Jaw (−) Posterior (−) | Bone status (−) | Surface treatment (−) | Bone graft (−) | ||
| Strietzel et al., 2011 [17] | 283 | 5 (1.8%) | Jaw (−) Posterior (−) | Surface treatment (−) | Short (+) D (−) | Bone graft (−) Time of implantation (−) | ||
| Le et al., 2013 [19] | 221 | 1 (0.4%) | Bone graft (−) | |||||
| Vercruyss-en et al., 2010 [20] | 1051 | 37 (3.5%) | L (−) | |||||
| Alsaadi et al., 2008 [21] | 1514 | 101 (6.7%) | Maxilla (+) Posterior (+) | Bone status (−) Bone quality (+) | Surface treatment (−) | L (−) Wide D (+) | High PTVs (+) | |
| Jemt et al., 2017 [22] | 3082 | 70 (2.3%) | Mandible (+) | 2-stages (+) | Inflammation at implant site during 1st year (+) | |||
| Jemt et al., 2017 [23] | 9582 | 82 (0.9%) | Mandible (+) | Bone quality (+) | D (−) | No installed implant at surgery (+) | ||
| Patient History Related | Clinical Parameter-Related | Doctor’s Decision-Related | ||||||
|---|---|---|---|---|---|---|---|---|
| Medical History | Habit | Implant Location | Bone Condition | Surgical Procedure | Prosthesis Design | |||
| Radiation Therapy | Periodontitis | Early Implant Loss | Bruxism | Posterior | Bone Grade 4 | Low Initial Stability | More than 1 Implant Placed at Surgery | Overdenture with Conus-Type Connection |
| Doll et al. [13] | Levin et al. [16] | Jemt et al. [20] | Manor et al. [5] | Manor et al. [5] | Alsaadi et al. [19] | Alsaadi et al. [19] | Jemt et al. [21] | Noda et al. [11] |
| Alsaadi et al. [19] | Vercruyssen et al. [18] | Chrcanovic et al. [22] | Noda et al. [11] | Jemt et al. [21] | ||||
| Derks et al. [10] | Alsaadi et al. [19] | |||||||
| Dvorak et al. [14] | ||||||||
| Strietzel et al. [15] | ||||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Do, T.A.; Le, H.S.; Shen, Y.-W.; Huang, H.-L.; Fuh, L.-J. Risk Factors related to Late Failure of Dental Implant—A Systematic Review of Recent Studies. Int. J. Environ. Res. Public Health 2020, 17, 3931. https://doi.org/10.3390/ijerph17113931
Do TA, Le HS, Shen Y-W, Huang H-L, Fuh L-J. Risk Factors related to Late Failure of Dental Implant—A Systematic Review of Recent Studies. International Journal of Environmental Research and Public Health. 2020; 17(11):3931. https://doi.org/10.3390/ijerph17113931
Chicago/Turabian StyleDo, Thanh An, Hoang Son Le, Yen-Wen Shen, Heng-Li Huang, and Lih-Jyh Fuh. 2020. "Risk Factors related to Late Failure of Dental Implant—A Systematic Review of Recent Studies" International Journal of Environmental Research and Public Health 17, no. 11: 3931. https://doi.org/10.3390/ijerph17113931
APA StyleDo, T. A., Le, H. S., Shen, Y.-W., Huang, H.-L., & Fuh, L.-J. (2020). Risk Factors related to Late Failure of Dental Implant—A Systematic Review of Recent Studies. International Journal of Environmental Research and Public Health, 17(11), 3931. https://doi.org/10.3390/ijerph17113931





