Psychometric Properties of the Condom Use Self-Efficacy Scale among Young Colombians
Abstract
1. Introduction
2. Method
2.1. Sample
2.2. Instruments
2.3. Procedure
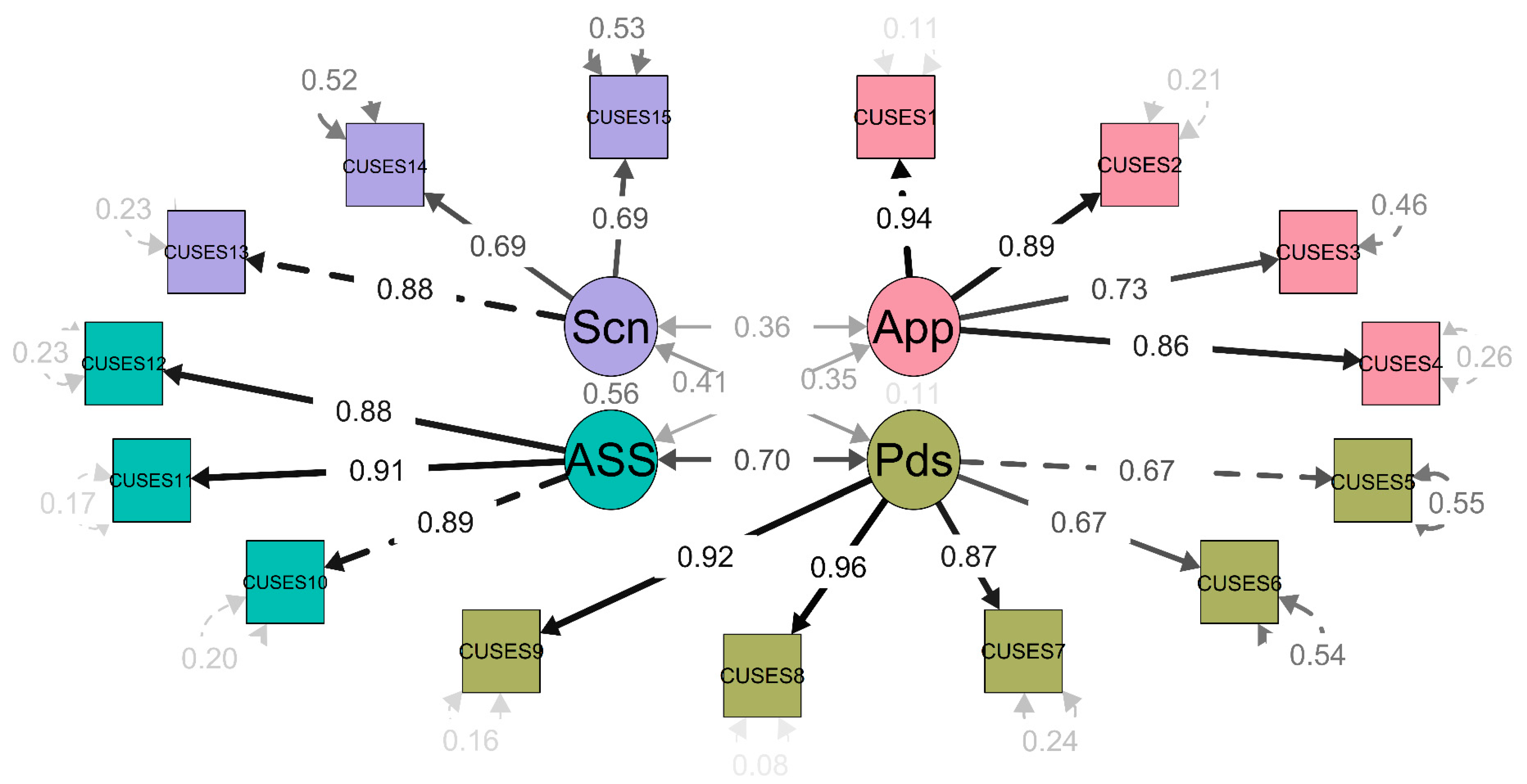
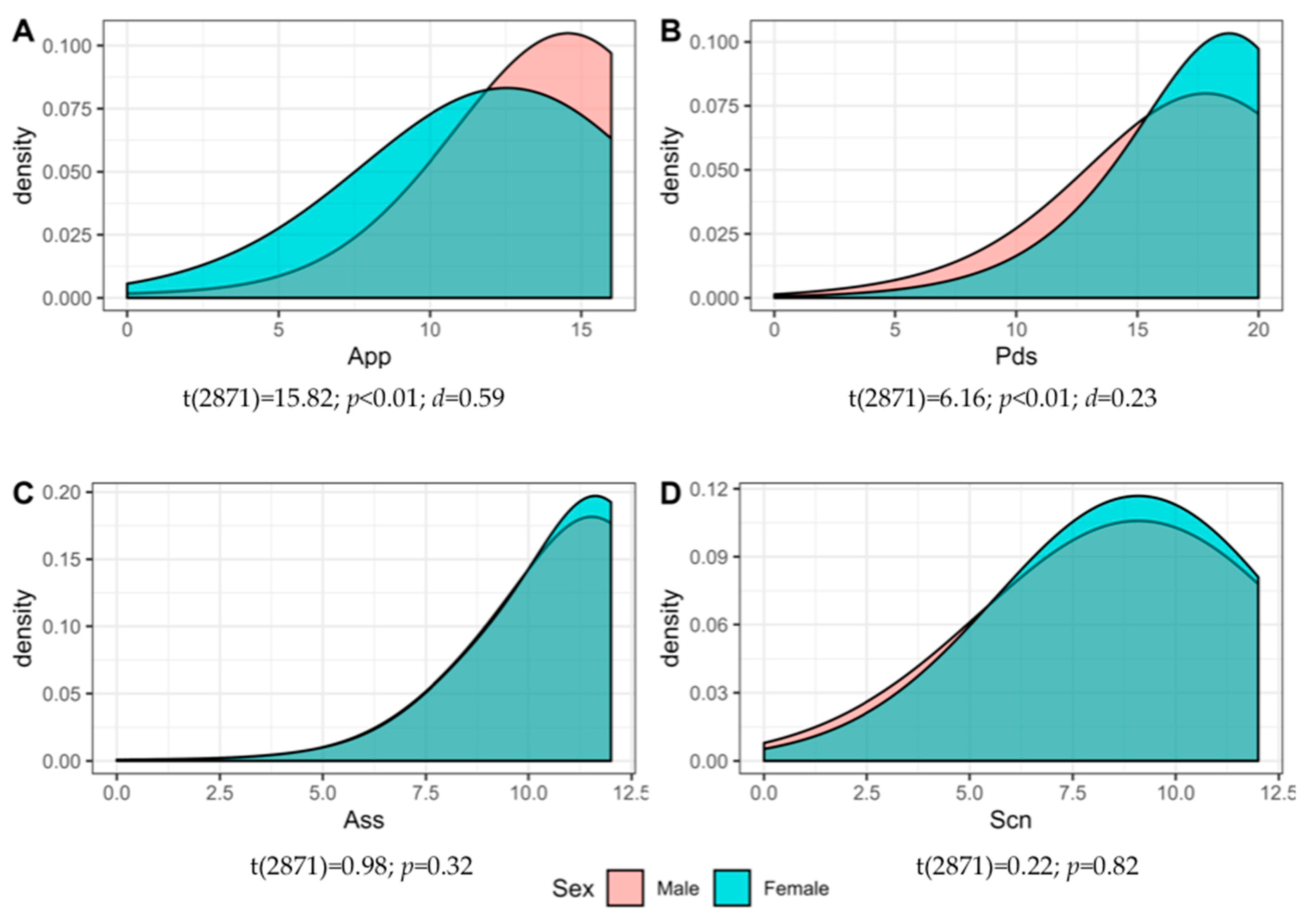
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- CONPES 3918. Estrategia Para la Implementación de Los Objetivos de Desarrollo Sostenible (ODS) en Colombia; Departamento Nacional de Planeación: Bogotá, Colombia, 2018. Available online: https://colaboracion.dnp.gov.co/CDT/Conpes/Econ%C3%B3micos/3918.pdf (accessed on 20 February 2020).
- Ministerio de Salud y Protección Social. Plan Decenal de Salud Pública; Ministerio de Salud y Protección Social: Bogotá. Colombia, 2012. Available online: https://www.minsalud.gov.co/plandecenal/Paginas/home2013.aspx (accessed on 20 February 2020).
- UNAIDS. Communities at the Centre. Global AIDS Update 2019; Joint United Nations Programme on HIV/AIDS (UNAIDS): Geneva, Switzerland, 2019. [Google Scholar]
- Instituto Nacional de Salud. Informe de Evento VIH/SIDA. Periodo Epidemiológico XIII Colombia; Ministerio de Salud: Bogotá, Colombia, 2019. Available online: https://www.ins.gov.co/buscador-eventos/Informesdeevento/VIH-SIDA%20PE%20XIII%202019.pdf (accessed on 20 February 2020).
- Rowley, J.; Vander Hoorn, S.; Korenromp, E.; Low, N.; Unemo, M.; AbuRaddad, L.; Chico, R.M.; Smolak, A.; Newman, L.; Gottlieb, S.; et al. Chlamydia, gonorrhea, trichomoniasis and syphilis: Global prevalence and incidence estimates, 2016. Bull. World Health Organ. 2019, 97, 548–562. [Google Scholar] [CrossRef] [PubMed]
- WHO. Report on Global Sexually TRANSMITTED Infection Surveillance. 2018. Available online: https://www.who.int/reproductivehealth/publications/stis-surveillance-2018/en/ (accessed on 20 February 2020).
- Ministerio de Salud y Protección Social. Situación de las Infecciones de Transmisión Sexual Diferentes al VIH. Colombia 2009–2011; Ministerio de Salud y Protección Social: Bogotá, Colombia, 2011. Available online: https://www.minsalud.gov.co/salud/Documents/observatorio_vih/documentos/monitoreo_evaluacion/1_vigilancia_salud_publica/a_situacion_epidimiologica/SITUACION%20DE%20LAS%20INFECCIONES%20DE%20TRANSMISION1.pdf (accessed on 20 February 2020).
- Tsevat, D.G.; Wiesenfeld, H.C.; Parks, C.; Peipert, J.F. Sexually transmitted diseases and infertility. Am. J. Obstet. Gynecol. 2017, 216, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.M.; Seth, P.; DiClemente, R.J.; Lin, A. Association of depressive symptoms and substance use with risky sexual behavior and sexually transmitted infections among African American female adolescents seeking sexual health care. Am. J. Public Health 2015, 105, 2137–2142. [Google Scholar] [CrossRef] [PubMed]
- Unemo, M.; Bradshaw, C.S.; Hocking, J.S.; de Vries, H.J.; Francis, S.C.; Mabey, D.; Peeling, R.W. Sexually transmitted infections: Challenges ahead. Lancet Infect. Dis. 2017, 17, e235–e279. [Google Scholar] [CrossRef]
- Sedgh, G.; Singh, S.; Hussain, R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud. Fam. Plan. 2014, 45, 301–314. [Google Scholar] [CrossRef]
- ENDS. Componente de Salud Sexual y Reproductiva; Profamilia: Bogotá, Colombia, 2015; Available online: https://dhsprogram.com/pubs/pdf/FR334/FR334.2.pdf (accessed on 20 February 2020).
- Morales, A.; Vallejo-Medina, P.; Abello-Luque, D.; Saavedra-Roa, A.; García-Roncallo, P.; Gomez-Lugo, M.; Espada, J.P. Sexual risk among Colombian adolescents: Knowledge, attitudes, normative beliefs, perceived control, intention, and sexual behavior. BMC Public Health 2018, 18, 1377. [Google Scholar] [CrossRef]
- González-Hernández, A.M.; Escobar-Estupiñan, J.; Vallejo-Medina, P. Condom use errors and problems in a simple of Young Colombian. J. Sex Res. 2020. [Google Scholar] [CrossRef]
- Albarracin, D.; Johnson, B.; Fishbein, M.; Muellerleile, P. Theories of reasoned action and planned behavior as models of condom use: A meta-analysis. Psychol. Bull. 2001, 127, 142–161. [Google Scholar] [CrossRef]
- Sheeran, P.; Abraham, C.; Orbell, S. Psychosocial correlates of heterosexual condom use: A meta-analysis. Psychol. Bull. 1999, 125, 90–132. [Google Scholar] [CrossRef]
- Armitage, C.J.; Conner, M. Social cognition models and health behaviour: A structured review. Psychol. Health 2000, 15, 173–189. [Google Scholar] [CrossRef]
- Ellis, E.M.; Homish, G.G.; Parks, K.A.; Collins, R.L.; Kiviniemi, M.T. Increasing condom use by changing people’s feelings about them: An experimental study. Health Psychol. 2015, 34, 941–950. [Google Scholar] [CrossRef] [PubMed]
- Vincent, W.; Gordon, D.M.; Campbell, C.; Ward, N.L.; Albritton, T.; Kershaw, T. Adherence to traditionally masculine norms and condom-related beliefs: Emphasis on African American and Hispanic men. Psychol. Men Masc. 2016, 17, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.Q.; Zhang, R.; Schwarzer, R.; Hagger, M.S. A meta-analysis of the health action process approach. Health Psychol. 2019, 38, 623–637. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioural change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Perceived self-efficacy in the exercise of control over AIDS infection. Eval. Program Plan. 1990, 13, 9–17. [Google Scholar] [CrossRef]
- Barkley, T.W., Jr.; Burns, J.L. Factor analysis of the Condom Use Self-Efficacy Scale among multicultural college students. Health Educ. Res. 2000, 15, 485–489. [Google Scholar] [CrossRef]
- Shaweno, D.; Tekletsadik, E. Validation of the condom use self-efficacy scale in Ethiopia. BMC Int. Health Hum. Rights 2013, 13, 22. [Google Scholar] [CrossRef]
- Brafford, L.; Beck, K. Development and Validation of a condom self-efficacy scale for college students. J. Am. Coll. Health 1991, 39, 219–225. [Google Scholar] [CrossRef]
- Brien, T.M.; Thombs, D.L.; Mahoney, C.A.; Wallnau, L. Dimensions of self-efficacy among three distinct groups of condom users. J. Am. Coll. Health 1994, 42, 167–174. [Google Scholar] [CrossRef]
- Forsyth, A.D.; Carey, M.P.; Fuqua, R.W. Evaluation of the validity of the Condom Use Self-Efficacy Scale (CUSES) in young men using two behavioral simulations. Health Psychol. 1997, 16, 175–178. [Google Scholar] [CrossRef]
- Asante, K.; Doku, P. Cultural adaptation of the Condom Use Self-Efficacy Scale (CUSES) in Ghana. BMC Public Health 2010, 10, 227. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Mendoza, V.; Soriano-Ayala, E.; Vallejo-Medina, P. A visual way to represent content validity and item properties. 2020; Manuscript under review. [Google Scholar]
- Vallejo-Medina, P.; Gómez-Lugo, M.; Marchal-Bertrand, L.; Saavedra-Roa, A.; Soler, F.; Morales, A. Desarrollo de Guías para Adaptar Cuestionarios Dentro de una Misma Lengua en Otra Cultura. Ter. Psicológica 2017, 35, 159–172. [Google Scholar] [CrossRef]
- Crosby, R.A.; Graham, C.A.; Milhausen, R.R.; Sanders, S.A.; Yarber, W.L. Condom use errors/problems survey. In Handbook of Sexuality-Related Measures; Fisher, T.D., Davis, C.M., Yarber, W.L., Eds.; Routledge: London, UK, 2010; pp. 153–159. [Google Scholar]
- Morokoff, P.J.; Quina, K.; Harlow, L.L.; Whitmire, L.; Grimley, D.M.; Gibson, P.R.; Burkholder, G.J. Sexual Assertiveness Scale (SAS) for women: Development and validation. J. Personal. Soc. Psychol. 1997, 73, 790–804. [Google Scholar] [CrossRef]
- Plaza-Vidal, R.; Ibagón-Parra, M.; Vallejo-Medina, P. Translation, adaptation and validation of the Spanish version of the multidimensional condom attitudes scale for Colombian young. Manuscr. Rev. 2020. under review. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing Vienna: R Foundation for Statistical Computing [Computer Software]. 2017. Available online: https://www.R-project.org/ (accessed on 24 February 2020).
- RStudio Team. RStudio: Integrated Development for R; RStudio, Inc. [Computer Software]: Boston, MA, USA, 2016; Available online: http://www.rstudio.com/ (accessed on 24 February 2020).
- Browne, M.W.; Cudeck, R. Alternative ways of assessing model fit. In Testing Structural Equation Models; Bollen, K.A., Long, J.S., Eds.; Sage: Newbury Park, CA, USA, 1993; pp. 136–162. [Google Scholar]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef]
- Tucker, L.R.; Lewis, C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika 1973, 38, 1–10. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cut-off criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Chen, F.F. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Modeling 2007, 14, 464–504. [Google Scholar] [CrossRef]
- Satorra, A. Scaled and adjusted restricted tests in multi-sample analysis of moment structures. In Innovations in Multivariate Statistical Analysis: A Festschrift for Heinz Neudecker; Heijmans, D.D.H., Pollock, D.S.G., Satorra, A., Eds.; Kluwer Academic: Dordrecht, The Netherlands, 2000; pp. 233–247. [Google Scholar]
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis [Computer Software]; Springer: New York, NY, USA, 2009; Available online: https://cran.r-project.org/web/packages/ggplot2/index.html (accessed on 20 February 2020).
- Revelle, W. Psych: Procedures for Personality and Psychological Research, [Computer Software]; Northwestern University: Evanston, IL, USA, 2018; Available online: https://CRAN.R-project.org/package=psych (accessed on 24 February 2020).
- Fletcher, T.D. Psychometric: Applied Psychometric Theory. R package version 2.2. 2010. Available online: https://CRAN.R-project.org/package=psychometric (accessed on 24 February 2020).
- Rosseel, Y. lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. Available online: http://www.jstatsoft.org/v48/i02/ (accessed on 24 February 2020). [CrossRef]
- Makowski, D. The Psycho Package: An Efficient and Publishing-Oriented Workflow for Psychological Science. J. Open Source Softw. 2018, 3, 470. Available online: https://github.com/neuropsychology/psycho.R (accessed on 24 February 2020). [CrossRef]
- Epskamp, S. SemPlot: Path Diagrams and Visual Analysis of Various SEM Packages’ Output. R package Version 1.1.2. 2019. Available online: https://CRAN.R-project.org/package=semPlot (accessed on 24 February 2020).
- Jorgensen, T.D.; Pornprasertmanit, S.; Schoemann, A.M.; Rosseel, Y. SemTools: Useful tools for Structural Equation Modeling. R Package Version 0.5–2. 2019. Available online: https://CRAN.R-project.org/package=semTools (accessed on 24 February 2020).
- Dimitrov, D.M. Testing for factorial invariance in the context of construct validation. Meas. Eval. Couns. Dev. 2010, 43, 121–149. [Google Scholar] [CrossRef]
- Sakaluk, J.K. Expanding statistical frontiers in sexual science: Taxometric, invariance, and equivalence testing. J. Sex Res. 2019, 56, 475–510. [Google Scholar] [CrossRef] [PubMed]
- Guillemin, F. Cross-cultural adaptation and validation of health status measures. Scand. J. Rheumatol. 1995, 24, 61–63. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.P. Applied Multivariate Statistics for the Social Sciences, 5th ed.; Taylor & Francis Group: New York, NY, USA, 2009. [Google Scholar]
- Carretero-Dios, H.; Pérez, C. Standards for the development and review of instrumental studies: Considerations about test selection in psychological research. Int. J. Clin. Health Psychol. 2007, 7, 863–882. [Google Scholar]
- Ritchwood, T.D.; Penn, D.; Peasant, C.; Albritton, T.; Corbie-Smith, G. Condom Use Self-Efficacy among younger rural adolescents: The influence of parent-teen communication, and knowledge of and attitudes toward condoms. J. Early Adolesc. 2017, 37, 267–283. [Google Scholar] [CrossRef]
- Logie, C.; Lys, C.; Okumu, M.; Fujioka, J. Exploring factors associated with condom use self-efficacy and condom use among Northern and Indigenous adolescent peer leaders in northern Canada. Vulnerable Child. Youth Stud. 2019, 14, 50–62. [Google Scholar] [CrossRef]
- Sanders, S.; Hill, B.; Crosby, R.; Janssen, E. Correlates of condom-associated erection problems in young, heterosexual men: Condom fit, self-efficacy, perceptions, and motivations. AIDS Behav. 2014, 18, 128–134. [Google Scholar] [CrossRef]
- Li, J.; Li, S.; Yan, H.; Xu, D.; Xiao, H.; Cao, Y.; Mao, Z. Early sex initiation and subsequent unsafe sexual behaviors and sex-related risks among female undergraduates in Wuhan, China. Asia Pac. J. Public Health 2015, 27, 21S–29S. [Google Scholar] [CrossRef]
- UNFPA. Análisis de Situación de Condones en Colombia. Ministerio de Salud y Protección Social; Fondo de población de las Naciones Unidas: Bogotá, Colombia, 2015; Available online: https://colombia.unfpa.org/sites/default/files/pub-pdf/analisiscondonesColombia_web.pdf (accessed on 20 February 2020).
- Albarracin, J.; Plambeck, C. Demographic factors and sexist beliefs as predictors of condom use among Latinos in the USA. AIDS Care 2010, 22, 1021–1028. [Google Scholar] [CrossRef]
- Unger, J.; Molina, G. Contraceptive use among Latina women: Social, cultural, and demographic correlates. Women’s Health Issues 1998, 8, 359–369. [Google Scholar] [CrossRef]
- Peasant, C.; Parra, G.; Okwumabua, T. Condom negotiation: Findings and future directions. J. Sex Res. 2015, 52, 470–483. [Google Scholar] [CrossRef] [PubMed]
| Males (n = 971) | Females (n = 1902) | Total (n = 2873) | |
|---|---|---|---|
| N % | N % | N % | |
| Age | |||
| 18 | 81 (8.3) | 230 (12.1) | 311 (10.8) |
| 19 | 109 (11.2) | 267 (14) | 376 (13.1) |
| 20 | 134 (13.8) | 282 (14.8) | 416 (14.5) |
| 21 | 131 (13.5) | 287 (15.1) | 418 (15.5) |
| 22 | 123 (12.7) | 236 (12.4) | 359 (12.5) |
| 23 | 127 (13.1) | 239 (12.6) | 366 (12.7) |
| 24 | 128 (13.2) | 154 (8.1) | 282 (9.8) |
| 25 | 107 (11) | 163 (8.6) | 270 (9.6) |
| 26 | 31 (3.2) | 44 (2.3) | 75 (2.6) |
| Schooling level N (%) | |||
| Basic Elementary | 1 (0.1) | 1 (0.0) | |
| Secondary | 52 (5.4) | 101 (5.3) | 153 (5.3) |
| First Technical level | 59 (6.1) | 142 (7.5) | 201 (7) |
| Second Technical level | 51 (5.3) | 85 (4.5) | 136 (4.7) |
| College undergraduate | 573 (59) | 1159 (60.9) | 1732 (60.3) |
| College graduate | 183 (18.8) | 323 (17) | 506 (17.6) |
| Postgraduate candidate | 41 (4.2) | 48 (2.5) | 89 (3.1) |
| Postgraduate | 11 (1.1) | 44 (2.3) | 55 (1.9) |
| Marital Status N (%) | |||
| Married | 14 (1.4) | 26 (1.4) | 40 (1.4) |
| Single | 867 (89.5) | 1659 (87.5) | 2526 (88.1) |
| Widowed | 1 (0.1) | 1 (0.0) | |
| Co-habiting | 81 (8.4) | 206 (10.9) | 287 (10) |
| Separated/Divorced | 6 (0.6) | 6 (0.3) | 12 (0.4) |
| Sexual orientation N (%) | |||
| Exclusively heterosexual | 738 (76.2) | 1431 (75.4) | 2169 (75.6) |
| Predominantly heterosexual, only incidentally homosexual | 66 (6.8) | 297 (15.6) | 363 (12.7) |
| Predominantly heterosexual, but more than incidentally homosexual | 10 (1) | 60 (3.2) | 70 (2.4) |
| Equally heterosexual and homosexual | 15 (1.5) | 66 (3.5) | 81 (2.8) |
| Predominantly homosexual, but more than incidentally heterosexual | 10 (1) | 9 (0.5) | 19 (0.7) |
| Predominantly homosexual, only incidentally heterosexual | 28 (2.9) | 12 (0.6) | 40 (1.4) |
| Exclusively homosexual | 98 (10.1) | 13 (0.7) | 111 (3.9) |
| Asexual | 4 (0.4) | 11 (0.6) | 15 (0.5) |
| Do you have a partner that you have been seeing for more than 6 months? | |||
| Yes | 491 (50.7) | 1179 (62.1) | 1670 (58.1) |
| No | 477 (49.3) | 719 (37.9) | 1196 (41.6) |
| How often do you use condoms during sexual intercourse? | |||
| Every time | 271 (28) | 334 (17.6) | 605 (21.1) |
| Usually | 248 (22.6) | 345 (18.2) | 593 (20.7) |
| Frequently | 105 (10.8) | 184 (9.7) | 289 (10.1) |
| Sometimes | 55 (5.7) | 125 (6.6) | 180 (6.3) |
| Occasionally | 92 (9.5) | 253 (13.3) | 345 (12) |
| Rarely | 105 (10.8) | 321 (16.9) | 426 (14.9) |
| Never | 93 (9.6) | 336 (17.7) | 429 (15) |
| 3 Dimensions | 4 Dimensions | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| D3 | D2 | D1 | h2 | u2 | com | D2 | D3 | D1 | D4 | h2 | u2 | com | ||
| CUSES8 | 0.92 | 0.89 | 0.10 | 10.1 | CUSES8 | 0.93 | 0.89 | 0.11 | 1.1 | |||||
| CUSES9 | 0.90 | 0.88 | 0.12 | 10.2 | CUSES9 | 0.91 | 0.88 | 0.11 | 1.1 | |||||
| CUSES7 | 0.84 | 0.78 | 0.21 | 10.2 | CUSES7 | 0.85 | 0.78 | 0.21 | 1.1 | |||||
| CUSES5 | 0.42 | 0.26 | 0.73 | 10.8 | CUSES5 | 0.44 | 0.26 | 0.74 | 1.7 | |||||
| CUSES6 | 0.41 | 0.32 | 0.27 | 0.72 | 10.9 | CUSES6 | 0.43 | 0.27 | 0.73 | 1.9 | ||||
| CUSES1 | 0.93 | 0.91 | 0.09 | 10.1 | CUSES1 | 0.94 | 0.91 | 0.09 | 1.1 | |||||
| CUSES2 | 0.89 | 0.85 | 0.15 | 10.2 | CUSES2 | 0.89 | 0.85 | 0.15 | 1.1 | |||||
| CUSES4 | 0.85 | 0.78 | 0.22 | 10.1 | CUSES4 | 0.86 | 0.78 | 0.22 | 1.1 | |||||
| CUSES3 | 0.76 | 0.65 | 0.35 | 10.2 | CUSES3 | 0.77 | 0.65 | 0.35 | 1.2 | |||||
| CUSES11 | 0.40 | 0.80 | 0.85 | 0.15 | 10.7 | CUSES13 | 0.96 | 0.98 | 0.02 | 1.1 | ||||
| CUSES10 | 0.35 | 0.77 | 0.77 | 0.23 | 10.6 | CUSES14 | 0.66 | 0.47 | 0.53 | 1.1 | ||||
| CUSES12 | 0.39 | 0.71 | 0.70 | 0.30 | 10.8 | CUSES15 | 0.43 | 0.31 | 0.68 | 2.5 | ||||
| CUSES13 | 0.48 | 0.28 | 0.72 | 10.4 | CUSES11 | 0.44 | 0.75 | 0.88 | 0.11 | 2.2 | ||||
| CUSES15 | 0.41 | 0.23 | 0.76 | 10.8 | CUSES10 | 0.40 | 0.71 | 0.77 | 0.22 | 2.1 | ||||
| CUSES14 | 0.35 | 0.15 | 0.85 | 10.4 | CUSES12 | 0.43 | 0.60 | 0.69 | 0.31 | 2.7 | ||||
| Variance | 0.22 | 0.21 | 0.19 | M = 10.4 | Variance | 0.23 | 0.22 | 0.12 | 0.12 | M = 1.5 * | ||||
| Models | χ2 | df | p | CFI | TLI | RMSEA | 90% CI RMSEA |
|---|---|---|---|---|---|---|---|
| D-1 | 4284.53 | 90 | <0.01 | 0.81 | 0.78 | 0.216 | 0.211–0.222 |
| D-3 I | 4146.70 | 90 | <0.01 | 0.82 | 0.79 | 0.212 | 0.207–0.218 |
| D-3 R | 920.65 | 87 | <0.01 | 0.96 | 0.95 | 0.098 | 0.092–0.104 |
| D-4 I | 4242.12 | 90 | <0.01 | 0.81 | 0.78 | 0.215 | 0.209–0.220 |
| D-4 R | 432.33 | 84 | <0.01 | 0.98 | 0.98 | 0.064 | 0.058–0.071 * |
| Models | χ2 | p > χ2 | df | p | CFI | ΔCFI | RMSEA | ΔRMSEA |
|---|---|---|---|---|---|---|---|---|
| Conf | 295.57 | - | 168 | <0.01 | 0.939 | - | 0.039 | - |
| Metric | 322.49 | 0.012 * | 179 | <0.01 | 0.932 | −0.007 | 0.040 | 0.001 |
| Scalar | 332.95 | 0.561 | 190 | <0.01 | 0.932 | 0 | 0.039 | −0.001 |
| Strict | 354.49 | 0.054 | 205 | <0.01 | 0.929 | −0.003 | 0.038 | −0.001 * |
| Dim | Item | M | SD | Skew | Kurtosis | Ci-tc | α-Item | α |
|---|---|---|---|---|---|---|---|---|
| App | 1 | 3.18 | 0.99 | −1.23 | 1.08 | 0.88 | 0.88 | 0.92 |
| 2 | 3.31 | 0.88 | −1.48 | 2.30 | 0.86 | 0.89 | ||
| 3 | 3.25 | 0.92 | −1.30 | 1.54 | 0.73 | 0.93 | ||
| 4 | 2.80 | 1.09 | −0.68 | −0.30 | 0.82 | 0.90 | ||
| Pds | 5 | 3.40 | 0.94 | −1.75 | 2.60 | 0.61 | 0.89 | 0.89 |
| 6 | 3.25 | 0.97 | −1.30 | 1.09 | 0.59 | 0.89 | ||
| 7 | 3.58 | 0.84 | −2.49 | 6.24 | 0.82 | 0.84 | ||
| 8 | 3.62 | 0.77 | −2.57 | 7.13 | 0.83 | 0.84 | ||
| 9 | 3.57 | 0.84 | −2.30 | 5.14 | 0.81 | 0.84 | ||
| Ass | 10 | 3.60 | 0.69 | −2.18 | 5.95 | 0.84 | 0.88 | 0.92 |
| 11 | 3.67 | 0.60 | −2.25 | 6.87 | 0.87 | 0.85 | ||
| 12 | 3.58 | 0.71 | −2.11 | 5.47 | 0.80 | 0.91 | ||
| Scn | 13 | 2.99 | 0.96 | −0.70 | −0.01 | 0.89 | 0.51 | 0.76 * |
| 14 | 2.71 | 1.13 | −0.55 | −0.34 | 0.82 | 0.69 | ||
| 15 | 3.09 | 0.99 | −0.96 | 0.35 | 0.76 | 0.81 |
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. App | 12.53 | 3.35 | |||||||||||
| 2. Pds | 17.42 | 3.23 | 0.08 ** | ||||||||||
| [0.04, 0.12] | |||||||||||||
| 3. Ass | 10.85 | 1.75 | 0.27 ** | 0.48 ** | |||||||||
| [0.24, 0.31] | [0.45, 0.51] | ||||||||||||
| 4. Scn | 8.79 | 2.43 | 0.27 ** | 0.24 ** | 0.36 ** | ||||||||
| [0.24, 0.31] | [0.20, 0.27] | [0.33, 0.40] | |||||||||||
| 5. Neg | 9.18 | 4.56 | 0.25 ** | 0.54 ** | 0.54 ** | 0.30 ** | |||||||
| [0.28, 0.21] | [0.57, 0.52] | [0.57, 0.52] | [0.33, 0.26] | ||||||||||
| 6. Reli | 11.87 | 5.11 | 0.20 ** | 0.11 ** | 0.15 ** | 0.14 ** | 0.20 ** | ||||||
| [0.23, 0.16] | [0.14, 0.07] | [0.19, 0.11] | [0.18, 0.10] | [0.16, 0.24] | |||||||||
| 7. Plea | 16.85 | 6.08 | 0.14 ** | 0.23 ** | 0.20 ** | 0.29 ** | 0.25 ** | 0.21 ** | |||||
| [0.17, 0.10] | [0.26, 0.19] | [0.24, 0.16] | [0.32, 0.25] | [0.22, 0.29] | [0.17, 0.24] | ||||||||
| 8. Sham | 13.72 | 7.32 | 0.28 ** | 0.19 ** | 0.26 ** | 0.21 ** | 0.32 ** | 0.15 ** | 0.17 ** | ||||
| [0.32, 0.25] | [0.23, 0.15] | [0.29, 0.22] | [0.25, 0.17] | [0.29, 0.36] | [0.11, 0.18] | [0.13, 0.20] | |||||||
| 9. Stig | 7.43 | 3.30 | 0.07 ** | 0.48 ** | 0.38 ** | 0.20 ** | 0.48 ** | 0.15 ** | 0.26 ** | 0.21 ** | |||
| [0.11, 0.03] | [0.51, 0.45] | [0.41, 0.34] | [0.24, 0.17] | [0.45, 0.51] | [0.12, 0.19] | [0.23, 0.30] | [0.17, 0.25] | ||||||
| 10. CUEP | 9.67 | 4.46 | −0.15 ** | −0.19 ** | −0.11 ** | −0.16 ** | 0.24 ** | 0.15 ** | 0.44 ** | 0.12 ** | 0.18 ** | ||
| [−0.21, −0.09] | [−0.25, −0.13] | [−0.17, −0.04] | [−0.22, −0.10] | [0.18, 0.30] | [0.09, 0.21] | [0.39, 0.49] | [0.06, 0.19] | [0.12, 0.24] | |||||
| 11. Init | 7.86 | 3.13 | 0.15 ** | 0.19 ** | 0.19 ** | 0.11 ** | −0.23 ** | −0.07 ** | −0.07 ** | −0.15 ** | −0.17 ** | 0.04 | |
| [0.12, 0.19] | [0.15, 0.23] | [0.15, 0.22] | [0.07, 0.14] | [−0.26, −0.19] | [−0.11, −0.03] | [−0.10, −0.03] | [−0.19, −0.11] | [−0.21, −0.13] | [−0.03, 0.10] | ||||
| 12. STI−P | 6.37 | 4.11 | 0.06 ** | 0.22 ** | 0.20 ** | 0.24 ** | −0.24 ** | −0.16 ** | −0.39 ** | −0.04 | −0.18 ** | −0.32 ** | −0.02 ** |
| [0.02, 0.10] | [0.18, 0.26] | [0.17, 0.24] | [0.20, 0.28] | [−0.28, −0.21] | [−0.20, −0.12] | [−0.42, −0.35] | [−0.08, 0.00] | [−0.21, −0.14] | [−0.37, −0.26] | [−0.06, 0.02] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanchez-Mendoza, V.; Soriano-Ayala, E.; Vallejo-Medina, P. Psychometric Properties of the Condom Use Self-Efficacy Scale among Young Colombians. Int. J. Environ. Res. Public Health 2020, 17, 3762. https://doi.org/10.3390/ijerph17113762
Sanchez-Mendoza V, Soriano-Ayala E, Vallejo-Medina P. Psychometric Properties of the Condom Use Self-Efficacy Scale among Young Colombians. International Journal of Environmental Research and Public Health. 2020; 17(11):3762. https://doi.org/10.3390/ijerph17113762
Chicago/Turabian StyleSanchez-Mendoza, Vanessa, Encarnacion Soriano-Ayala, and Pablo Vallejo-Medina. 2020. "Psychometric Properties of the Condom Use Self-Efficacy Scale among Young Colombians" International Journal of Environmental Research and Public Health 17, no. 11: 3762. https://doi.org/10.3390/ijerph17113762
APA StyleSanchez-Mendoza, V., Soriano-Ayala, E., & Vallejo-Medina, P. (2020). Psychometric Properties of the Condom Use Self-Efficacy Scale among Young Colombians. International Journal of Environmental Research and Public Health, 17(11), 3762. https://doi.org/10.3390/ijerph17113762





